Back to Journals » Nature and Science of Sleep » Volume 14
Associations Between Childhood Stressors, COVID-19-Related Anxiety, and Sleep Quality of Adults During the Third Wave of the COVID-19 Pandemic in Israel
Authors Haimov I, Szepsenwol O, Cohen A
Received 12 June 2022
Accepted for publication 30 August 2022
Published 20 September 2022 Volume 2022:14 Pages 1665—1675
DOI https://doi.org/10.2147/NSS.S378271
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Sarah L Appleton
Iris Haimov,1 Ohad Szepsenwol,2,* Ami Cohen1,*
1The Center for Psychobiological Research and The Department of Psychology, The Max Stern Yezreel Valley College, Yezreel Valley, Israel; 2The Center for Psychobiological Research and The Department of Education and Educational Counseling, The Max Stern Yezreel Valley College, Yezreel Valley, Israel
*These authors contributed equally to this work
Correspondence: Iris Haimov, The Center for Psychobiological Research and The Department of Psychology, The Max Stern Yezreel Valley College, Yezreel Valley, Israel, Email [email protected]
Purpose: Studies point to a persistent effect of the COVID-19 pandemic on sleep quality and mental health, including anxiety. Exposure to stressors during childhood increases the susceptibility to anxiety in later life. Given the negative effects of anxiety on sleep quality, the present study aimed to examine the associations between various childhood stressors and poor sleep quality of adults during the COVID-19 pandemic, and whether these associations are mediated by COVID-19-related anxiety.
Participants and Methods: A total of 586 participants aged 18– 40 (mean age 27.53± 6.48 years, 301 females) were recruited to take part in an online survey conducted in Israel between February 7 and 15, 2021, during the third wave of the COVID-19 pandemic. Participants completed questionnaires assessing retrospectively adverse childhood experiences (ACEs), childhood harshness (indexed separately by exposure to morbidity and mortality and low socioeconomic status, SES), and childhood unpredictability. COVID-19-related anxiety was assessed using two items. Sleep quality was measured using the Pittsburgh Sleep Quality Index (PSQI), and insomnia symptoms with the Insomnia Severity Index (ISI). Participants were asked to complete the ISI concerning two time points: (a) retrospectively, before the COVID-19 outbreak, and (b) currently, during the pandemic.
Results: Path analysis indicated that poor sleep quality (PSQI) was directly and indirectly (through COVID-19-related anxiety) predicted by the number of ACEs and childhood morbidity-mortality exposure, directly predicted by childhood low SES, and indirectly predicted by childhood unpredictability. Insomnia symptoms increase (ISI) was indirectly predicted by the number of ACEs, childhood morbidity-mortality exposure, and childhood unpredictability.
Conclusion: ACEs as well as harsh and unpredictable childhood environments are predictive of poorer sleep during the COVID-19 pandemic. COVID-19-related anxiety mediates the effects of childhood stressors (other than low SES) on sleep. These findings may have clinical implications relevant to stressful periods in general.
Keywords: childhood environments, harshness, unpredictability, stressful periods, sleep efficiency
Introduction
The COVID-19 pandemic exposed the population worldwide to severe psychological distress caused by health concerns, loss of income, and uncertainty about the future, in addition to the social isolation and other negative factors associated with imposed lockdowns.1 The stressors associated with epidemics and lockdowns are likely to induce deterioration in measures of psychological health.2–4 Large-scale studies conducted in various countries since the onset of the COVID-19 pandemic have shown a significant increase in the levels and prevalence of symptoms of depression and anxiety, eg.1,5,6 as well as in the rates of poor sleep quality and sleep disturbances, most common being insomnia (difficulty falling asleep, maintaining sleep, or nonrestorative sleep, with impairment of daytime functioning7).5,8–11 Given the association of insomnia and other forms of reduced sleep quality with a host of adverse psychological and physiological consequences, such as cardiovascular and metabolic diseases,12–14 depression, and anxiety,15,16 this increase raises serious concerns. Studies conducted during the COVID-19 pandemic showed an association of insomnia and other forms of poor sleep quality with poorer perceived physical health,17 greater involvement in unhealthy behaviors, such as consumption of cigarettes and alcoholic beverages,18 low subjective wellbeing,19 and higher levels of emotional distress, including depression, psychological stress, and anxiety.10,17,20–22
The relationship between sleep quality and emotional distress is complex and bidirectional.15 Insomnia may increase the risk for depression and anxiety,16 and prospective studies have shown a negative effect of anxiety disorders and symptoms of anxiety on sleep.23,24 Individuals with higher levels of stress during the COVID-19 pandemic tended to report that their sleep quality was worse than it had been before the pandemic.25
Interpersonal differences in the effects of the COVID-19 pandemic on anxiety and sleep quality may be explained by various factors that influence resilience to negative stressors.26 One factor that may hinder such resilience in adults is a history of adverse childhood experiences (ACEs). ACEs refer to experiences involving childhood abuse, neglect, and/or household dysfunction that occurred within the first 18 years of life.27 ACEs are associated with mental health difficulties, including anxiety and depression, throughout life,27–29 and with poorer self-reported sleep quality and insomnia in later life.30–32
It has been suggested that ACEs compromise the development of capabilities that are essential for resilience, such as emotional regulation and executive functioning, increasing the risk for negative consequences following exposure to environmental stressors,28 such as the ones elicited by the COVID-19 pandemic. Several studies examining the possible effect of ACEs on mental health during the pandemic have shown an association between ACEs and symptoms of depression, anxiety, and COVID-19-related stress and fear in both young adults33 and adolescents.34,35 Yet, the relationship between ACEs, COVID-19-related anxiety, and sleep quality remains unclear.
A recent study showed that ACEs were associated with reduced sleep quality during the COVID-19 pandemic,36 but it did not examine the possible mediating role of COVID-related anxiety in this relationship, and it was conducted on a unique sample of Native Americans, therefore, its generalizability to other populations is uncertain. Moreover, in that study, sleep quality was measured only by the Pittsburgh Sleep Quality Index (PSQI),37 which is widely used for the assessment of general sleep quality, a construct that is not well defined.38 Other measures, such as the Insomnia Severity Index (ISI),39 specifically designed for the assessment of insomnia, can add important information about the relationship between ACEs and sleep disturbances.
Less studied potential risk factors for anxiety and sleep disturbances are exposures to harsh and unpredictable childhood environments. Childhood unpredictability refers to frequent, stochastic changes in the local environment during childhood. It is frequently indexed by the number of economic, residential, and family transitions occurring during the first years of a child’s life.40 Childhood harshness refers to an abundance of sources of morbidity and mortality in the local environment during childhood. It is frequently indexed by socioeconomic status (SES) or exposure to morbidity and mortality in the first years of a child’s life.40,41 These distinct environmental parameters may have unique predictive associations with human psychology and physiology, above and beyond the effects of specific ACEs.42
According to life history theory, exposure to harsh or unpredictable childhood environments should lead to the development of a generally impulsive and dysregulated behavior, which could be evolutionarily adaptive in harsh and unpredictable adult environments, but may also hinder psychological resilience and emotional wellbeing.43 Prospective studies have shown that childhood unpredictability in particular predicts emotion regulation difficulties and externalizing problems later in life.44,45 These characteristics may play out mostly in stressful contexts, such as the COVID-19 pandemic,46 making individuals more susceptible to COVID-related distress and potentially greater sleep problems. No studies to date, however, have examined associations between childhood exposure to unpredictability and harshness and sleep quality during stressful periods.
Exposure to extreme stressors during childhood is known to increase the susceptibility to anxiety in later life.27 Given the negative effects of anxiety on sleep quality,15 the present study examined whether various childhood stressors were uniquely associated with poor sleep quality and symptoms of insomnia during the COVID-19 pandemic, and whether these associations were mediated by COVID-19-related anxiety. The study was conducted in Israel during the third wave of the COVID-19 pandemic. As in other countries, the COVID-19 pandemic in Israel led to excess mortality, particularly for people above 55 years of age.47 During the first two waves of the pandemic, the government mandated strict containment measures, including limiting public gatherings and celebrations, limited use of public transport, and the closing of schools. Lockdowns were imposed in April-May and September-October 2020, and some restrictions remained in effect longer. The third wave led to high excess mortality between December 2020-February 2021. Lockdown measures, including the closure of non-essential stores and services, closure of schools, and limiting travel to a 1000-meter radius from home, were imposed for five weeks starting on December 27 2021.47
To the best of our knowledge, this is the first study to examine the unique associations of the number of ACEs, childhood harshness, and childhood unpredictability with COVID-related anxiety and sleep quality. We hypothesized that a larger number of ACEs, greater unpredictability, and greater harshness (indexed separately by exposure to morbidity-mortality and low socioeconomic status) are uniquely associated with poor sleep quality and an increase in symptoms of insomnia relative to the period before the pandemic, and that these associations are mediated by greater COVID-19-related anxiety.
Materials and Methods
The study was carried out in accordance with the declaration of Helsinki, and was approved by the Institutional Ethics Review Board (IERB) of the Max Stern Yezreel Valley College (approval # 2021–10). All participants provided their informed consent online, after which they completed the survey posted on the iPanel online platform. The survey took approximately 25 minutes to complete. The survey was conducted in Hebrew, using validated translations where necessary.
Participants
The study was conducted between February 7-15, 2021, during the third wave of the COVID-19 pandemic in Israel (December 2020-March 2021). The study began one day after the termination of a 5-week lockdown. A total of 586 participants aged 18-40 (M = 27.53, SD = 6.48; 301 women, 285 men) were recruited from the Jewish-Israeli community to take part in an online study. They were members of iPanel (ipanel.co.il), a large online Israeli survey panel that has over 100,000 members from all walks of Israeli society. The sample was representative of the Hebrew-speaking, Jewish-Israeli population of the specified age range. Of the participants, 7.8% did not complete high school, 38.6% had a high school education, 14.7% had post-secondary non-academic education, and 38.9% had academic education (Bachelor’s degree or higher); 48.1% had full-time employment, 22.5% had part-time employment, 29.4% were not employed (31.7% of the sample indicated that they were students). Applicants were excluded if they reported suffering from sleep apnea syndrome (SAS) or periodic limb movement disorder during sleep (PLMD). Participants were compensated with points on the iPanel website that can be converted into gift certificates, worth approximately USD 27.
Measures
Demographics
All participants provided demographic information including age, gender, education level, and employment status.
Adverse Childhood Experiences
The number of adverse childhood experiences was assessed with the Adverse Childhood Experience Questionnaire,48 a widely used and well-validated self-report questionnaire examining childhood traumas. It includes 10 binary (yes/no) items relating to three general categories: childhood abuse, neglect, and household dysfunction (eg. “Did a parent or other adult in the household (1) often or very often swear at you, insult you, or put you down? (2) often or very often act in a way that made you afraid that you would be physically hurt?”). ACEs refer to experiences that occurred before the age of 18. The sum of item scores ranges from 0 to 10, higher scores indicating greater exposure to childhood adversity.
Childhood Harshness
Two aspects of childhood harshness were assessed: low SES, based on 5 items (eg. “My family struggled financially”) used in previous studies, eg.45 and exposure to morbidity and mortality, based on 5 items concerning the death and illness of close others (eg. “People close to me died before their time”), similarly to previous studies, eg.41 Participants indicated their agreement with each item on a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree) relating to the first 10 years of their lives. We computed low SES and morbidity-mortality exposure scores by averaging the respective items (Cronbach’s αs = 0.77 and 0.79, respectively), with higher values indicating harsher childhood environments.
Childhood Unpredictability
Early-life unpredictability was assessed with a 9-item expanded version of a 6-item scale used in previous research,45 rating the frequency of three types of events that signal unpredictability: changes in economic circumstances or resource availability, moving to a different environment (house, school, custody), and changes inside the family (people moving in and out of the house, parents becoming romantically involved with other people, losing or reestablishing contact with a first-degree family member). Participants indicated whether each of these events occurred in their first 10 years of life on a 4-point scale (0 = not at all; 1 = once; 2 = twice, 3 = three or more times). These ratings were summed to create an accumulated early-life unpredictability count score. Higher values indicate greater childhood unpredictability. The score of the 9-item version correlated highly with that of the 6-item version used in previous research (r = 0.96).
COVID-19-Related Anxiety
COVID-19-related anxiety was assessed with two items used in previous research:49 (a) “To what extent are you anxious these days?” and (b) “To what extent are you tense these days?”. Participants rated their degree of anxiety or tension specific to the current COVID-19 crisis on a 5-point scale ranging from 1 (not at all) to 5 (very much). The two items were averaged (Cronbach’s α = 0.87), higher scores indicating a higher level of COVID-19-related anxiety.
Insomnia Severity Index
The Insomnia Severity Index (ISI)39 is a seven-item self-report questionnaire assessing the nature, severity, and impact of insomnia based on a 5-point (0–4) scale. The sum score range is 0–28. Participants were asked to complete the ISI concerning two time points: (a) retrospectively, before the COVID-19 outbreak in Israel (Cronbach’s α = 0.88), and (b) currently, during the pandemic (Cronbach’s α = 0.91).
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI)37 is a widely used self-report questionnaire that assesses sleep quality in the preceding month. The PSQI consists of 19 items used to evaluate perceived sleep quality. The items are used to generate categorical scores representing 7 PSQI subscales, and a total score reflecting the sum of the subscales. The total PSQI score range is 0-21, with higher scores representing poorer sleep.
Data Analysis
We computed correlations between all study variables. Next, we created an ISI difference score [Current ISI – pre-pandemic ISI] as an indicator of the amount of increase in insomnia symptoms during the pandemic (positive scores suggesting an increase). The main analysis was conducted in two stages. First, to examine the unique associations between specific childhood stressors and sleep quality variables (Model 1: Total Effects), we conducted a path analysis using Mplus version 8.3.50 The number of ACEs and the scores for childhood unpredictability, low SES, and morbidity-mortality exposure were specified as predictors. The PSQI score and the ISI difference score were specified as outcome variables. Second, to examine mediation by COVID-19-related anxiety (Model 2: Mediation), we added this variable to the path model as an outcome of the four childhood stressors and a predictor of the two sleep variables (Figure 1). We also included direct paths between the four childhood stressors and the two sleep variables. Both path models were estimated using Maximum Likelihood (ML) estimation. Indirect paths in Model 2 were estimated using 95% bias-corrected bootstrap confidence intervals (k = 5000). In this method, confidence intervals that do not include 0 indicate a statistically significant effect (p < 0.05). Model fit was not an issue because both models were saturated. There were no missing values in any of the variables in our dataset.
Results
Descriptive statistics and zero-order correlations between all study variables are reported in Table 1. Early childhood stressors were positively intercorrelated, and all were positively correlated with sleep and anxiety measures, with the one exception being a nonsignificant correlation between childhood exposure to morbidity and mortality and the ISI difference score. Sleep and anxiety measures were also positively intercorrelated, with the one exception being a small negative correlation between the ISI before score and the ISI difference score, suggesting that individuals who experienced more insomnia symptoms before the pandemic tended to experience a lower increase in insomnia over this period. In general, ISI scores were significantly higher during the pandemic than before it [t(584) = 9.99, p < 0.001], suggesting an increase in insomnia symptoms during this period. Standardized ML estimates and confidence intervals for Model 1 are provided in Table 2. The PSQI score was significantly associated with the number of ACEs and childhood exposure to morbidity-mortality, indicating that these childhood stressors were predictive of poor sleep quality during the COVID-19 pandemic. The ISI difference score was uniquely associated with the number of ACEs and childhood unpredictability, indicating that these childhood stressors were uniquely predictive of an increase in insomnia symptoms during the COVID-19 pandemic. Model 1 explained 14% of the variance in PSQI scores and 4.3% of the variance in ISI difference scores.
 |
Table 1 Descriptive Statistics and Zero-Order Correlations Between Study Variables |
 |
Table 2 Standardized Maximum Likelihood Estimates. Model 1 – Childhood Stressors Predicting Sleep Variables |
Standardized ML estimates and confidence intervals for Model 2 are provided in Table 3. A larger number of ACEs, greater childhood unpredictability, and greater childhood morbidity-mortality exposure were significantly associated with greater COVID-19-related anxiety, which in turn was associated with worse sleep quality on the PSQI and an increase in insomnia symptoms on the ISI. The resulting indirect paths were all significant, indicating significant mediation by COVID-19-related anxiety (Table 4). Some direct paths also emerged; regardless of COVID-19-related anxiety, poor sleep quality on the PSQI was directly predicted by a larger number of ACEs, greater morbidity-mortality exposure, and lower SES during childhood. No direct paths were found between childhood stressors and the ISI difference score (Figure 1). Model 2 explained 33% of the variance in PSQI scores, 13.4% of the variance in ISI difference scores, and 14.4% of the variance in COVID-19-related anxiety. We repeated all analyses using the 6-item version of the unpredictability score, with similar results.
 |
Table 3 Standardized Maximum Likelihood Estimates. Model 2 – Childhood Stressors Predicting Sleep Variables Mediated by COVID-19 Anxiety |
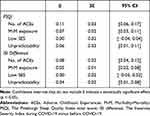 |
Table 4 Model 2 – Bias-Corrected 95% Bootstrap Confidence Intervals for Standardized Indirect Effects Through COVID-19 Anxiety |
In sum, poor sleep quality during the COVID-19 pandemic based on the PSQI was directly and indirectly (through COVID-19-related anxiety) associated with the number of ACEs and exposure to morbidity-mortality during childhood, directly associated with low SES during childhood, and indirectly associated with childhood unpredictability. An increase in insomnia symptoms based on the ISI was indirectly associated with the number of ACEs, exposure to morbidity-mortality, and unpredictability during childhood.
Discussion
The present study examined the associations of various childhood stressors (ACEs, harsh and unpredictable childhood environments) with sleep quality and symptoms of insomnia during the third wave of the COVID-19 pandemic in Israel, and whether these associations were mediated by COVID-19-related anxiety.
Consistent with previous reports,8 participants reported an increase in symptoms of insomnia since the outbreak of the pandemic (mean ISI scores of 7.89 compared to 6.08 before the pandemic). General sleep quality, as measured by the PSQI (6.39), was also high in comparison to that demonstrated in studies conducted in Israel before the COVID-19 pandemic (eg. 4.4 in the study of Cohen et al).51 The mean global PSQI and ISI scores in the current study were within the range observed in England, Italy, the West Balkan, and the USA during the third wave of the COVID-19 pandemic (ISI= 6.9-8.1; PSQI = 5.77-7.62).52–55
In the present study, several childhood stressors were found to be associated with a reduction in sleep quality and with increased symptoms of insomnia. The most consistent predictor was the number of ACEs. A larger number of ACEs was associated with both poor sleep quality and an increase in symptoms of insomnia relative to the period before the pandemic. These findings are consistent with previous studies examining the association between ACEs and sleep quality in general30–32 and in the context of the COVID-19 pandemic in particular.36 Previous studies, however, examined the number of ACEs in isolation, without taking into account other aspects of the childhood environment.
Greater childhood harshness, as indexed by exposure to morbidity and mortality, was associated with poor sleep quality during the pandemic, and greater childhood unpredictability was associated with an increase in insomnia symptoms relative to the period before the pandemic. These associations were not strong but were present above and beyond the effect of the ACEs, indicating that they were distinct stressors with unique effects on sleep quality, and they should be considered in future studies. These findings are consistent with life history models that found a connection between early exposure to harshness and unpredictability and poor health outcomes later in life.56 Yet, the present study is the first to link childhood harshness and unpredictability to poor sleep quality in adulthood.
COVID-19 provides an important context for studying the health effects of childhood environments. Exposure to childhood unpredictability, for example, may influence individuals’ response to the pandemic both physiologically and psychologically.57 The present study identified COVID-19-related anxiety as a key pathway by which childhood stressors may lead to reduced sleep quality in adulthood. Specifically, the results revealed indirect effects of childhood unpredictability, morbidity-mortality exposure, and adverse experiences on sleep difficulties and worsening insomnia during COVID-19, mediated by greater anxiety surrounding COVID-19. These results are consistent with substantial evidence for a link between childhood stressors and anxiety disorders in adulthood. Childhood stressors may provoke increased activation of the HPA axis that can endure into adulthood, increasing the risk for anxiety disorders (for a review, see Juruena et al).58 A recent study showed that a history of early sexual abuse increased the risk for anxiety in health professionals caring for patients with COVID‐19.59 The results of the present study are also consistent with several studies showing levels of anxiety during the COVID-19 pandemic to be positively correlated with levels of insomnia and other indices of poor sleep quality.10,21,22 Nevertheless, we also found some direct effects, with greater morbidity-mortality exposure, financial difficulties, and adverse experiences in childhood uniquely predicting greater sleep difficulties during COVID-19, above and beyond general levels of anxiety surrounding the pandemic.
Exposure to ACEs, childhood harshness, and childhood unpredictability were more consistently associated with overall sleep quality, as measured by the PSQI, than with severity of insomnia symptoms, as measured by the ISI. This difference may reflect the fact that the PSQI assesses a broader aspect of sleep than the ISI. Furthermore, the PSQI was administered once, whereas the ISI was administered twice, with respect to insomnia symptoms before and during the pandemic. Thus, the PSQI scores reflected sleep quality during the pandemic, whereas the ISI-difference scores used in the analysis reflected the increase in insomnia symptoms following the outbreak of the pandemic.
The present study expands the literature on adverse childhood experiences by incorporating measures of harsh and unpredictable childhood environments as distinct childhood stressors. The results of the study demonstrate that various childhood stressors may uniquely contribute to a reduction in sleep quality during stressful periods, such as the COVID-19 pandemic, and that context-related anxiety may mediate these associations. Given that stress-inducing environmental events, such as the COVID-19 pandemic, are likely to recur, and given the grave medical and psychological consequences of low sleep quality and sleep disturbances,23,60 these findings have important clinical implications. It may be particularly important to train adults who were exposed to severe stressors in childhood to adopt effective strategies for managing anxiety and reducing stress reactivity to avoid deterioration of sleep quality in response to significant external stressors.
Limitations and Future Directions
The present study should be viewed in light of several limitations. First, the participants were all members of an online Israeli survey panel. Although they were representative of the various subgroups of Jewish-Israeli population of the specified age range (18-40), biases in sample composition may have occurred. For example, the sample may not represent individuals who do not have easy access to the Internet. Future studies should aim to include such individuals by distributing paper-and-pencil surveys to eligible participants. Future studies should also aim to include populations that did not take part in the current study, such as Israelis who are not Jewish (20% of the Israeli population) and different age groups. Second, the childhood stressors were measured based on retrospective self-reports, which may be subject to recall bias. For example, it was found that reports of childhood trauma decrease with age.23 Because of the cross-sectional study design, insomnia severity before COVID-19 was also based on retrospective self-reports, and was thus similarly subject to recall bias as well as other biases that may result from the use of self-reports. Future studies should rely on longitudinal methods and use multiple sources of information to assess childhood environments and sleep quality. Last, the present study did not assess the personal effect of the pandemic on participants (eg. having a loved one fall ill or die, having suffered from a severe form of COVID-19) and therefore the contribution of such experiences to the participants’ COVID-related anxiety could not be determined.
Conclusion
The present study demonstrated that the number of adverse experiences during childhood, as well as harsh and unpredictable childhood environments, predicted poorer sleep during the COVID-19 pandemic, and that anxiety related to the pandemic mediated the effects of these childhood stressors on sleep. These findings have important clinical implications that may be relevant to stressful periods in general.
Acknowledgments
We thank all the participants in this study.
Author Contributions
All authors made a significant contribution to the work reported, either in conceptualization, study design, execution, data acquisition, analysis and interpretation, or in all these areas. All authors took part in drafting, writing, revising, and critically reviewing the article; reviewed and gave final approval for the revision to be published; agreed on the journal to which the article has been submitted; and agreed to take responsibility and be accountable for all aspects of the manuscript.
Funding
This research received funding from the Israel Science Foundation (ISF) grant number 1497/17.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Santomauro DF, Mantilla Herrera AM, Shadid J.; COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi:10.1016/S0140-6736(21)02143-7
2. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/S0140-6736(20)30460-8
3. Alimoradi Z, Ohayon MM, Griffiths MD, Lin CY, Pakpour AH. Fear of COVID-19 and its association with mental health-related factors: systematic review and meta-analysis. B J Psych Open. 2022;8(2):e73. doi:10.1192/bjo.2022.26
4. Olashore AA, Akanni OO, Fela-Thomas AL, Khutsafalo K. The psychological impact of COVID-19 on healthcare workers in African Countries: a systematic review. Asian J Soc Health Behav. 2021;4:85–97. doi:10.4103/shb.shb_32_21
5. Morin CM, Bjorvatn B, Chung F, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. 2021;87:38–45. doi:10.1016/j.sleep.2021.07.035
6. Andersen AJ, Mary-Krause M, Bustamante JJH. Symptoms of anxiety/depression during the COVID-19 pandemic and associated lockdown in the community: longitudinal data from the TEMPO cohort in France. BMC Psychiatry. 2021;21(1):381. doi:10.1186/s12888-021-03383-z
7. Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 Suppl):S7–10.
8. Jahrami H, BaHammam AS, Bragazzi NL. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. doi:10.5664/jcsm.8930
9. Morin CM, Vézina-Im LA, Ivers H, et al. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020). Sleep. 2021:zsab258. doi:10.1093/sleep/zsab258
10. Alimoradi Z, Broström A, Tsang H, et al. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: a systematic review and meta-analysis. EClinical Med. 2021;36:100916. doi:10.1016/j.eclinm.2021.100916
11. Alimoradi Z, Gozal D, Tsang HWH, et al. Gender-specific estimates of sleep problems during the COVID-19 pandemic: systematic review and meta-analysis. J Sleep Res. 2022;31(1):e13432. doi:10.1111/jsr.13432
12. Gangwisch JE, Heymsfield SB, Boden-Albala B. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47(5):833–839. doi:10.1161/01.HYP.0000217362.34748.e0
13. Huang T, Mariani S, Redline S. Sleep irregularity and risk of cardiovascular events: the multi-ethnic study of atherosclerosis. JACC. 2020;75(9):991–999. doi:10.1016/j.jacc.2019.12.054
14. Knutson K. Sociodemographic and cultural determinants of sleep deficiency: implications for cardiometabolic disease risk. Soc Sci Med. 2013;79:7–15. doi:10.1016/j.socscimed.2012.05.002
15. Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64(4):443–449. doi:10.1016/j.jpsychores.2007.10.016
16. Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? JAMA. 1989;262(11):1479–1484. doi:10.1001/jama.262.11.1479
17. Fan CW, Drumheller K, Chen IH, Huang HH. College students’ sleep difficulty during COVID-19 and correlated stressors: a large-scale cross-sessional survey study. Sleep Epidemiol. 2021;1:100004. doi:10.1016/j.sleepe.2021.100004
18. Bruno S, Bazzani A, Marantonio S, et al. Poor sleep quality and unhealthy lifestyle during the lockdown: an Italian study. Sleep Med. 2022;90:53–64. doi:10.1016/j.sleep.2022.01.002
19. Fares Z, Aljaberi MA, Gadelrab HF, Lin CY, Muhammed A. Mediated effects of insomnia in the association between problematic social media use and subjective well-being among university students during COVID-19 pandemic. Sleep Epidemiol. 2022;2:100030. doi:10.1016/j.sleepe.2022.100030
20. Varma P, Burge M, Meaklim H, Junge M, Jackson ML. Poor sleep quality and its relationship with individual characteristics, personal experiences and mental health during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(11):6030. doi:10.3390/ijerph18116030
21. Eleftheriou A, Rokou A, Arvaniti A, Nena E, Steiropoulos P. Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front Public Health. 2021;9:775374. doi:10.3389/fpubh.2021.775374
22. Diaz F, Cornelius T, Bramley S, et al. The association between sleep and psychological distress among New York City healthcare workers during the COVID-19 pandemic. J Affect Disord. 2022;298(PtA):618–624. doi:10.1016/j.jad.2021.10.033
23. Jansson M, Linton SJ. The role of anxiety and depression in the development of insomnia: cross-sectional and prospective analyses. Psychol Health. 2006;21:383–397. doi:10.1001/jama.262.11.1479
24. Taylor DJ, Lichstien KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–1464. doi:10.1093/sleep/28.11.1457
25. Tsang S, Avery AR, Seto EYW, Duncan GE. Is COVID-19 keeping us up at night? Stress, anxiety, and sleep among adult twins. Front Neurosci. 2021;15:665777. doi:10.3389/fnins.2021.665777
26. Vinkers CH, van Amelsvoort T, Bisson JI, et al. Stress resilience during the coronavirus pandemic. Eur Neuropsychopharmacol. 2020;35:12–16. doi:10.1016/j.euroneuro.2020.05.003
27. Merrick MT, Ports KA, Ford DC, et al. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse Negl. 2017;69:10–19. doi:10.1016/j.chiabu.2017.03.016
28. Kessler RC, McLaughlin KA, Greif Green J, et al. Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br J Psychiatry. 2010;197:378–385. doi:10.1192/bjp.bp.110.080499
29. Fritz J, de Graaff AM, Caisley H, van Harmelen A, Wilkinson PO. A systematic review of amenable resilience factors that moderate and/or mediate the relationship between childhood adversity and mental health in young people. Front Psychiatry. 2018;9:230. doi:10.3389/fpsyt.2018.00230
30. Sheehan CM, Li L, Friedman EM. Quantity, timing, and type of childhood adversity and sleep quality in adulthood. Sleep Health. 2020;6(2):246–252. doi:10.1016/j.sleh.2020.01.010
31. Wang Y, Raffeld MR, Slopen N, Hale L, Dunn EC. Childhood adversity and insomnia in adolescence. Sleep Med. 2016;21:12–18. doi:10.1016/j.sleep.2016.01.011
32. Chapman DP, Wheaton AG, Anda RF, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011;12(8):773–779. doi:10.1016/j.sleep.2011.03.013
33. Li X, Lv Q, Tang W. Psychological stresses among Chinese university students during the COVID-19 epidemic: the effect of early life adversity on emotional distress. J Affect Disord. 2021;282:33–38. doi:10.1016/j.jad.2020.12.126
34. Stinson EA, Sullivan RM, Peteet BJ, et al. Longitudinal impact of childhood adversity on early adolescent mental health during the COVID-19 pandemic in the ABCD study® cohort: does race or ethnicity moderate findings? Biol Psychiatry Glob Open Sci. 2021;1(4):324–335. doi:10.1016/j.bpsgos.2021.08.007
35. Guo J, Fu M, Liu D, Zhang B, Wang X, van IJzendoorn MH. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110(Pt2):104667. doi:10.1016/j.chiabu.2020.104667
36. John-Henderson NA. Childhood trauma as a predictor of changes in sleep quality in American Indian adults during the COVID-19 pandemic. Sleep Health. 2020;6(6):718–722. doi:10.1016/j.sleh.2020.09.001
37. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
38. Hartmann JA, Carney CE, Lachowski A, Edinger JD. Exploring the construct of subjective sleep quality in patients with insomnia. J Clin Psychiatry. 2015;76(6):e768–73. doi:10.4088/JCP.14m09066
39. Morin CM. Insomnia: Psychological Assessment and Management. Guilford Press; 1993.
40. Belsky J, Schlomer GL, Ellis BJ. Beyond cumulative risk: distinguishing harshness and unpredictability as determinants of parenting and early life history strategy. Dev Psychol. 2012;48(3):662–673. doi:10.1037/a0024454
41. Szepsenwol O, Shai D, Zamir O, Simpson JA. The effects of morbidity-mortality and economic unpredictability on parental distress: a life history approach. J Soc Pers Relat. 2021;38(1):189–209. doi:10.1177/0265407520959719
42. Ellis BJ, Figueredo AJ, Brumbach BH, Schlomer GL. Fundamental dimensions of environmental risk: the impact of harsh versus unpredictable environments on the evolution and development of life history strategies. Hum Nat. 2009;20(2):204–268. doi:10.1007/s12110-009-9063-7
43. Belsky J, Steinberg L, Draper P. Childhood experience, interpersonal development, and reproductive strategy: and evolutionary theory of socialization. Child Dev. 1991;62(4):647–670. doi:10.1111/j.1467-8624.1991.tb01558.x
44. Doom JR, Vanzomeren-Dohm AA, Simpson JA. Early unpredictability predicts increased adolescent externalizing behaviors and substance use: a life history perspective. Dev Psychopathol. 2016;28(4pt2):1505–1516. doi:10.1017/S0954579415001169
45. Szepsenwol O, Simpson JA, Griskevicius V, et al. The effects of childhood unpredictability and harshness on emotional control and relationship quality: a life history perspective. Dev Psychopathol. 2022;34(2):607–620. doi:10.1017/S0954579421001371
46. Ellis BJ, Bianchi J, Griskevicius V, Frankenhuis WE. Beyond risk and protective factors: an adaptation-based approach to resilience. Perspect Psychol Sci. 2017;12(4):561–587. doi:10.1177/1745691617693054
47. Haklai Z, Goldberger NF, Gordon ES. Mortality during the first four waves of COVID-19 pandemic in Israel: March 2020-October 2021. Israel Isr J Health Policy Res. 2022;11(1):24. doi:10.1186/s13584-022-00533-w
48. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi:10.1016/s0749-3797(98)00017-8
49. Zreik G, Asraf K, Haimov I, Tikotzky L. Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID-19) pandemic in Israel. J Sleep Res. 2021;30(1):e13201. doi:10.1111/jsr.13201
50. Muthén LK, Muthén BO. Mplus User’s Guide.
51. Cohen A, Asraf K, Saveliev I, Dan O, Haimov I. The effects of sleep deprivation on the processing of emotional facial expressions in young adults with and without ADHD. Sci Rep. 2021;11(1):14241. doi:10.1038/s41598-021-93641-7
52. Conte F, De Rosa O, Rescott ML, et al. High sleep fragmentation parallels poor subjective sleep quality during the third wave of the Covid-19 pandemic: an actigraphic study. J Sleep Res. 2022;31(3):e13519. doi:10.1111/jsr.13519
53. Šljivo A, Juginović A, Ivanović K, et al. Sleep quality and patterns of young West Balkan adults during the third wave of COVID-19 pandemic: a cross-sectional study. BMJ Open. 2022;12(5):e060381. doi:10.1136/bmjopen-2021-060381
54. Kantor J, Kantor BN, Fortgang RG, Pace-Schott EF. Sleep quality impairment is associated with pandemic attitudes during the coronavirus disease 2019 (COVID-19) circuit breaker lockdown in England: a cross-sectional study. Front Public Health. 2022;10:819231. doi:10.3389/fpubh.2022.819231
55. Alqahtani JS, AlRabeeah SM, Aldhahir AM, et al. Sleep quality, insomnia, anxiety, fatigue, stress, memory and active coping during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(9):4940. doi:10.3390/ijerph19094940
56. Maner JK, Dittmann A, Meltzer AL, McNulty JK. Implications of life-history strategies for obesity. Proc Natl Acad Sci U S A. 2017;114(32):8517–8522. doi:10.1073/pnas.1620482114
57. Liu S, Fisher PA. Early experience unpredictability in child development as a model for understanding the impact of the COVID-19 pandemic: a translational neuroscience perspective. Dev Cogn Neurosci. 2022;54:101091. doi:10.1016/j.dcn.2022.101091
58. Juruena M, Eror F, Cleare AJ, Young AH. The role of early life stress in HPA axis and anxiety. In: Kim YK, editor. Anxiety Disorders: Rethinking and Understanding Recent Discoveries. Singapore: Springer; 2020:141–153. doi:10.1007/978-981-32-9705-0_9
59. Fernández-Arana A, Olórtegui-Yzú A, Vega-Dienstmaier JM, Cuesta MJ. Depression and anxiety symptoms and perceived stress in health professionals in the context of COVID-19: do adverse childhood experiences have a modulating effect? Brain Behav. 2022;12(1):e2452. doi:10.1002/brb3.2452
60. Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Colten HR, Altevogt BM, editors. Washington (DC): National Academies Press (US); 2006. doi:10.17226/11617
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

