Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Association of Pain with Plasma C5a in Patients with Neuromyelitis Optica Spectrum Disorders During Remission
Authors Tong Y, Liu J, Yang T, Wang J, Zhao T, Kang Y, Fan Y
Received 23 January 2022
Accepted for publication 6 May 2022
Published 17 May 2022 Volume 2022:18 Pages 1039—1046
DOI https://doi.org/10.2147/NDT.S359620
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Yanping Tong,1,2 Jie Liu,3 Tao Yang,1,2 Jingwen Wang,4 Tianyou Zhao,4 Yuezhi Kang,1,2 Yongping Fan1,2
1Department of Traditional Chinese Medicine, Beijing Tiantan Hospital, Capital Medical University, Beijing, 100070, People’s Republic of China; 2Beijing Integrative Medicine on Encephalopathy Research Institution, Beijing Tiantan Hospital, Capital Medical University, Beijing, 100070, People’s Republic of China; 3Department of Respiratory Medicine, Beijing First Hospital of Integrated Chinese and Western Medicine, Beijing, 100026, People’s Republic of China; 4Department of Neurology, Beijing Miyun District Hospital of Traditional Chinese Medicine, Beijing, 101599, People’s Republic of China
Correspondence: Yongping Fan, Email [email protected]
Objective: To investigate the association of pain with plasma C5a levels and other related inflammatory cytokines in neuromyelitis optica spectrum disorders (NMOSD) patients during remission.
Participants and Methods: NMOSD patients (n = 87) and healthy controls (HC; n = 44) were consecutively recruited between January 2017 and April 2018. Plasma complement 5 (C5), C5a, interleukin (IL)-6, tumor necrosis factor (TNF)-α, and IL-1β levels were detected. Visual Analogue Scale (VAS), ID pain scale, 24-item Hamilton Depression Scale (HAMD), Multiple Sclerosis Impact Scale (MSIS-29), and Kurtzke Expanded Disability Status Scale (EDSS) were used to evaluate the degree and types of pain, the existence of depression and anxiety, and the life quality and disability status of patients. Binary logistic regression equation was used to assess the association of pain with plasma C5a levels.
Results: Among the 87 NMOSD patients, 40 complained of pain that in 67.5% (27/40) of cases had a neuropathic component (ID pain ≥ 2). Plasma C5a, IL-6, TNF-α, and IL-1β levels were significantly elevated in NMOSD patients than in HC. Plasma C5 levels were negatively correlated with the time from sampling to the last relapse or disease onset. NMOSD patients with pain had higher plasma C5a levels, and they suffered from a higher disability, more anxiety, and worse life quality compared to those patients without pain. In NMOSD patients with pain, there were not significant differences between plasma levels of C5, C5a, IL-6, TNF-α, or IL-1β, regardless of neuropathic pain or not. Binary logistic regression showed that the OR of plasma C5a level was 1.002, with gender and EDSS score were identified as independent factors associated with pain in NMOSD.
Conclusion: NMOSD patients during remission had elevated C5a and related inflammatory cytokines levels in peripheral blood. Elevated C5a may have a unique role in the pathogenesis of pain in NMOSD patients.
Keywords: neuromyelitis optica spectrum disorders, remission, pain, C5a
Introduction
Neuromyelitis optica spectrum disorders (NMOSD) is a rare autoimmune inflammatory demyelinating disease of the central nervous system (CNS) characterized by recurrent inflammation of the optic nerve, spinal cord, and specific brain areas.1 Compared to multiple sclerosis (MS) that primarily targets myelin, NMOSD induces irreparable neuronal cell death which leads to more severe disability and a poorer prognosis.2 The clinical presentation of NMOSD includes severe episodes of optic neuritis that may lead to loss of vision, transverse myelitis causing paraplegia or paralysis, and sometimes brainstem encephalitis causing intractable vomiting or hiccups. In addition, NMOSD causes severe, persistent pain which is more prevalent (83.8%−91%) than in MS (~47%) and most other neurological diseases.3–5 Many NMOSD patients experience pain that severely affects their quality of life and is often refractory to treatment.6
Aquaporin-4 antibody (AQP4- immunoglobulin [IgG]) is a highly specific antibody involved in the disease pathogenesis of NMOSD, which can be used to distinguish NMOSD from MS.7 Animal experiments showed that immunoglobulin G from aquaporin-4-autoantibody-positive neuromyelitis optica (NMO) patients did not activate mouse complement and was not pathogenic when injected into mouse brain. However, co-injection of immunoglobulin G from NMO patients with human complement produced NMO-like lesions in mice, suggesting that human complement plays a key role in the pathogenesis of NMOSD.8 Complement 5 (C5) is an activated complement protein common to all complement activation pathways. One of its cleavage products, C5a, is the most effective complement-derived inflammatory mediator. Several lines of evidence have shown that C5a plays a pivotal role in neuropathic pain mechanisms;9–13 however, its association with pain in NMOSD remains unclear. Therefore, in this study, we investigated the association of pain with plasma levels of C5a and other related inflammatory factors in patients with NMOSD during remission.
Participants and Methods
Participants
Patients with NMOSD and healthy controls (HC) were consecutively recruited from the Beijing Tiantan Hospital between January 2017 and April 2018. The diagnosis of NMOSD was confirmed according to the 2015 revised international criteria.1 All patients were in remission (had remained relapse-free for over a 1-month period) and had no other autoimmune comorbidities at the time of blood collection. In NMOSD patients, clinical relapses were defined as new neurologic symptoms lasting at least 24 hours and accompanied by new neurologic findings, occurring 30 days after the previous attack.14 Acute phase was defined as within one month of onset or relapse of NMOSD.15 Age- and sex-matched volunteers without immune disorders were recruited as HC. Infections were ruled out based on complete blood count testing in all participants. Clinical records of participants were collected, including sex, age at sampling, disease duration since the first onset, and relapse times; the mean annualized relapse rate (ARR, times/year) was calculated accordingly.
Measurement Instruments and Evaluation
Visual analogue scale (VAS) and ID pain scale16,17 were used for evaluating the degree of pain and screening of neuropathic pain (ID pain score ≥ 2). In addition, 24-item Hamilton Depression Scale (HAMD) and 14-item Hamilton Anxiety Scale (HAMA) were used to evaluate the existence of depression and anxiety; a total score of HAMD ≥ 8 indicated depression and HAMA ≥ 7 indicated anxiety. Also, Multiple Sclerosis Impact Scale (MSIS-29) was used to evaluate the impact of disease on the life quality of patients. The total score of MSIS-29 ranged between 29 and 145, with a higher score indicating lower life quality. Kurtzke Expanded Disability Status Scale (EDSS) was used to evaluate the disability status of patients.
Assay for Plasma C5, C5a, IL-6, TNF-α, and IL-1β Levels
Peripheral blood was obtained from each participant. All blood samples were collected at 9:00 a.m. After collection into a 4-mL disposable BD Vacutainer® containing ethylene diamine tetraacetic acid, plasma samples were separated at 2000 × g for 10 min within 3 h and stored in aliquots at −80°C until further analysis. All testing was performed in a blinded manner with respect to diagnosis or clinical presentations. Plasma C5, C5a, interleukin (IL) −6, tumor necrosis factor (TNF) -α, and IL-1β levels were assayed using MILLIPLEX® map human High Sensitivity Cytokine/Chemokine Panels (Cat. HCMP1MAG, HCYTOMAG) (Merck KGaA, Darmstadt, Germany) according to the manufacturer’s instructions.
Statistical Analysis
Statistical analysis was conducted using SPSS 22.0 (International Business Machines Corporation, Chicago, IL, USA). After normality test, data with non-Gaussian distributions were analyzed using the Mann–Whitney U-test for two groups. Normally distributed data were processed using Student’s t-test or analysis of variance. Demographic features of NMOSD patients with and without pain, including gender, age, age at disease onset, disease duration, ARR, relapse times, etc., were compared. To clarify whether plasma C5a was correlated with pain risk in NMOSD, binary logistic regression was conducted after adjusting for the above demographic features. Odds ratios (ORs) and 95% confidence intervals (CIs) for pain and plasma C5a were also estimated. A P-value of <0.05 was considered to be statistically significant.
Results
Demographics and Disease Characteristics
A total of 87 patients with NMOSD and 44 HC were enrolled in the current study. Among the 87 NMOSD patients, 40 complained of pain that in 67.5% (27/40) of cases had a neuropathic component (ID pain ≥2). The demographics and disease characteristics of the participants are presented in Table 1. NMOSD patients with pain showed significantly higher EDSS and MSIS-29 scores, as well as anxiety rates than those without pain (all P values < 0.01). There were no significant differences in proportions of depression in NMOSD patients with pain and without pain.
 |
Table 1 Demographic Characteristics of Participants in the Study |
Plasma C5, C5a, IL-6, TNF-α, and IL-1β Levels in NMOSD Patients and HC
There was no significant difference (P=0.10) between plasma C5 levels in patients with NMOSD and HC. However, plasma C5a levels in NMOSD patients was significantly higher than in HC (P=0.000) (Table 2).
 |
Table 2 Plasma Levels of C5a and IL-6, TNF-α, and IL-1β in Different Groups (Mean ± SE) |
Next, we examined the levels of plasma IL-6, TNF-α, and IL-1β, whose productions may be induced by C5a. The data showed that plasma levels of all the cytokines mentioned above were significantly elevated in NMOSD patients than in HC (P=0.035, 0.019, and 0.012, respectively) (Table 2).
Table 3 shows the Spearman correlations among plasma C5a and IL-6, TNF-α, and IL-1β in NMOSD patients during remission. Briefly, plasma IL-6 and IL-1β levels were positively correlated with plasma C5a levels.
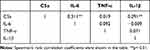 |
Table 3 Correlations Between Plasma C5a and IL-6, TNF-α, and IL-1β Among NMOSD Patients (n=87) |
Influences of the Time from Sampling to the Last Relapse or Disease Onset on Plasma Levels of C5, C5a, IL-6, TNF-α, and IL-1β in NMOSD Patients During Remission
The time from sampling to the last relapse or disease onset was calculated and the correlations of C5, C5a, and inflammatory cytokines with it were analyzed. The results showed that the time from sampling to the last relapse or disease onset of NMOSD patients was 198.75 ± 20.61 (days, mean ± SE), ranged from 31 to 1192 days. Spearman’s rank correlation analysis showed that plasma C5 levels were negatively correlated with the time interval (P=−0.016, r=−0.258). Plasma levels of C5a, IL-6, TNF-α, and IL-1β had no correlation with the time interval (P=0.729, 0.285, 0.188, and 0.913, respectively).
Plasma Levels of C5, C5a, IL-6, TNF-α, and IL-1β in NMOSD Patients with Pain and without Pain, and in Those with Different Type of Pain
There were no significant differences in plasma C5 levels between NMOSD patients with and without pain (P=0.698). Nevertheless, NNMOSD patients with pain had higher plasma C5a levels than those patients without pain (P=0.008). In addition, no significant differences were found between plasma levels of IL-6, TNF-α, or IL-1β in NMOSD patients with pain and without pain (P=0.190, 0.123, and 0.528, respectively) (Table 2).
In NMOSD patients with pain, there were not significant differences between plasma levels of C5, C5a, IL-6, TNF-α, or IL-1β, regardless of neuropathic pain or not (all P>0.05) (Table 2).
Association of C5a Level with Pain in Patients with NMOSD During Remission
Binary logistic regression analysis showed that the plasma C5a level was significantly correlated with pain risk in patients with NMOSD (P = 0.007). All models were adjusted for gender, age, disease duration, relapse times, and EDSS score, which were included in univariate analysis and clinical practice (Table 4). Gender and EDSS score were identified as independent factors associated with pain in NMOSD (P = 0.047 and 0.005, respectively).
 |
Table 4 Adjusted Odds Ratios (95% CI) for Pain According to Exposure for Plasma C5a Levels in the Logistic Regression Models |
Discussion
Severe episodes of painful optic neuritis and longitudinally extensive transverse myelitis are the most typical clinical syndromes of NMOSD. In addition, some limited forms of encephalic lesions and coexisting autoimmune disorders are encompassed in NMOSD. Pain, which is highly prevalent in patients with NMOSD, can greatly impair quality of life.18 In the present study, 46% of the patients with NMOSD during remission complained of current pain. They suffered from a higher disability, greater anxiety, and worse life quality.
Next, we investigated the association of pain with plasma levels of C5a and other related inflammatory factors in NMOSD patients during remission. These patients had significantly higher plasma C5a levels compared to HC. What’s more, the inflammatory cytokines IL-6 and IL-1β plasma levels were also elevated and positively correlated with the C5a level. Also, 46% of NMOSD patients in the current study experienced ongoing pain, and further binary logistic regression analysis showed that pain was positively correlated with the C5a level, with gender and EDSS score were identified as independent factors.
AQP4-IgGs are present in 65 to 88% of patients with NMOSD.19,20 AQP4-IgG triggers the complement cascade, which leads to inflammation and the formation of the membrane attack complex.8,21 Recent studies have suggested that the C5 inhibitor eculizumab, which inhibits its cleavage into C5a and C5b and the subsequent neurologic damage, significantly reduced relapse risk compared to placebo in patients with AQP4-IgG-positive NMOSD.22,23 As one of the C5 cleavage products, C5a is an efficient proinflammatory factor activated its cell membrane receptors, C5aR, mainly distributed in neutrophils, astrocytes, and microglia. Increased concentration of C5a had been found in the cerebrospinal fluid (CSF) of patients with active NMOSD, and the CSF-C5a levels were correlated with the severity of exacerbation.24 In CNS, C5a is associated with impaired BBB integrity in a neuroinflammatory setting where C5a affects both endothelial and astroglial cells.25 The inflammatory response induced by C5a can promote the production of C5a, form a positive feedback cycle, promote the expansion of NMO lesions, and prolong the inflammatory process. These humoral and cellular immune responses induced by C5a are consistent with the results of NMO neuropathology in human and animal models.8,26,27 C5a/C5aR signaling can also induce the production of proinflammatory cytokines (TNF, IL-1β, and IL-6) in vitro and in vivo.28 Higher levels of IL-6 were seen in CSF and serum of patients with NMO attack.29 Our results suggested that although NMOSD patients during remission seemed to be in a stable condition, there were still abnormally high levels of C5a and related inflammatory cytokines and disordered inflammatory environment in peripheral blood.
There are two types of pain being most characteristic in patients with NMOSD: evoked pain most often caused by painful tonic muscle spasms, and ongoing neuropathic pain.30 What’s more, pain due to excess loading and pain as a side effect of immunotherapy and in the context of comorbidities are also not rare in NMOSD patients.31 Neuropathic pain is defined by the International Association for the Study of Pain (IASP) as a chronic pain state initiated or caused by a lesion or disease of the central or peripheral somatosensory nervous system. It may result from different stimuli such as physical trauma, infection, inflammation, metabolic abnormalities, vascular abnormalities, neurotoxins (including chemotherapeutic agents), radiation, surgery procedures or autoimmune disease that induce pathological changes in the tissue and nerves.32 Long and centrally situated inflammatory lesions in the spinal cord provide a credible explanation for most pain incidence.33 In the present study, about 68% of NMOSD patients experiencing pain with a neuropathic component (ID pain ≥2). Previous studies suggested that C5a and its cell membrane receptor, C5aR, participate in acute and chronic pain pathophysiological mechanisms.
Emerging evidences suggest that C5a has potent nociceptive activity in several models of inflammatory and neuropathic pain.34 Inflammatory pain is mainly triggered by the interaction between inflammatory mediators in the damaged tissue, such as prostaglandins, sympathetic amines and kinins and their receptors expressed in the primary nociceptive neuron membranes, which leads to peripheral sensitization. The peripheral pro-nociceptive action of these cytokines (TNF, CXCL1/2 chemokines and IL-1β) during inflammatory pain partially dependent on neutrophil recruitment. C5a/ C5aR has been involved in the development of several inflammatory events, including edema, leukocyte recruitment and activation and production of proinflammatory cytokines, which drive inflammatory and neuropathic pain.13 C5a could also mediate peripheral sensitization during inflammatory pain through direct action on C5aR-expressing nociceptors.35,36 Glial cell activation is involved in the induction and maintenance of neuropathic pain, such as satellite glial cells in the dorsal root ganglions (DRGs) and spinal and supraspinal microglial cells and astrocytes.13 Upregulated levels of C5a and C5aR were found in spinal cord microglia in animals subjected to spared nerve injury (SNI), a model of neuropathic pain.12 The expression of C5aR and C5 also increased in the spinal cord after nerve injury, and intrathecal administration of C5a induces cold allodynia in a dose-dependent manner. Nerve injury-induced allodynia is ameliorated in C5-deficient mice and in mice intrathecally treated with C5aR antagonist (PMX-53), further supporting the role of C5a/Ca5R signaling in the genesis of neuropathic pain.12,13 Although it is clear that spinal C5a/C5aR signaling accounts for the genesis of the neuropathic pain process, the mechanisms involved are not fully understood.
However, to the best of our knowledge, no studies reported on the relationship between C5a levels in peripheral blood and pain in patients with NMOSD during remission. Direct administration of C5a elicits mechanical and thermal hypersensitivity in rodents, and both genetic deletion and pharmacologic antagonism of C5aR produce analgesia in murine models of inflammatory, arthritic, postsurgical, and neuropathic pain.11,37,38 In this study, plasma levels of C5a, IL-6, TNF-α, and IL-1β were significantly higher in NMOSD patients during remission than healthy controls; however, only plasma C5a level showed elevated in patients with pain, which suggested that C5a may play a unique role in the pathogenesis of pain in NMOSD, especially during remission. In addition, only plasma C5 levels were negatively correlated with the time interval. Since plasma C5 levels in patients with NMOSD showed no significant difference with that in HC, we believed that the inclusion time from the acute phase did not influence the results significantly in our study.
A few limitations to our study should be mentioned. Types of pain in NMOSD patients including painful tonic muscle spasms, neuropathic pain, and sometimes pain due to excess loading and pain as a side effect of immunotherapy and in the context of comorbidities. We did not conduct detailed subgroup analysis for pain types due to a small sample. Moreover, as this was only an observational study, a longitudinal study is needed to be performed to figure out the association of pain with plasma C5a level in patients with NMOSD during remission and attack.
Conclusion
Collectively, the findings of this study showed that NMOSD patients during remission may have unregulated C5a and related-inflammatory cytokines levels in peripheral blood; however, higher plasma C5a level in patients with pain suggesting that C5a may play a unique role in the pathogenesis of pain in NMOSD.
Abbreviations
NMOSD, neuromyelitis optica spectrum disorders; MS, multiple sclerosis; NMO, neuromyelitis optica; CNS, central nervous system; C5, complement 5; IL, interleukin; TNF, tumor necrosis factor; VAS, Visual Analogue Scale; HAMD, Hamilton Depression Scale; HAMA, Hamilton Anxiety Scale; MSIS, Multiple Sclerosis Impact Scale; EDSS, Kurtzke Expanded Disability Status Scale; AQP4, Aquaporin-4; HC, healthy controls; ARR, annualized relapse rate; OR, odds ratio; CI, confidence interval; SE, standard error; CSF, cerebrospinal fluid; C5aR, C5a receptor; DRG, dorsal root ganglions; SNI, spared nerve injury.
Ethics Approval and Informed Consent
The study was approved by the Ethics Committee of Beijing Tiantan Hospital, Capital Medical University, China. Prior to participation, all participants provided written informed consent.
Author Contributions
All authors contributed substantially to conception and design, data analysis, drafting or revising the article. All authors agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be responsible for all aspects of the work.
Funding
The present work was supported by the Capital’s Funds for Health Improvement and Research (CFH 2020-2-2043), Beijing municipal hospital scientific research and cultivation program (PZ2021006), National Natural Science Foundation of China (CN), China (81973599, 82074350).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Wingerchuk DM, Banwell B, Bennett JL, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85(2):177–189. doi:10.1212/WNL.0000000000001729
2. Popescu BF, Lucchinetti CF. Immunopathology: autoimmune glial diseases and differentiation from multiple sclerosis. Handb Clin Neurol. 2016;133:95–106.
3. Kanamori Y, Nakashima I, Takai Y, et al. Pain in neuromyelitis optica and its effect on quality of life: a cross-sectional study. Neurology. 2011;77(7):652–658. doi:10.1212/WNL.0b013e318229e694
4. Qian P, Lancia S, Alvarez E, Klawiter EC, Cross AH, Naismith RT. Association of neuromyelitis optica with severe and intractable pain. Arch Neurol. 2012;69(11):1482–1487. doi:10.1001/archneurol.2012.768
5. Mealy MA, Kozachik SL, Levy M. Review of treatment for central spinal neuropathic pain and its effect on quality of life: implications for neuromyelitis optica spectrum disorder. Pain Manag Nurs. 2019;20(6):580–591. doi:10.1016/j.pmn.2019.03.003
6. Hyun JW, Jang H, Yu J, et al. Comparison of neuropathic pain in neuromyelitis optica spectrum disorder and multiple sclerosis. J Clin Neurol. 2020;16(1):124–130. doi:10.3988/jcn.2020.16.1.124
7. Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005;202(4):473–477. doi:10.1084/jem.20050304
8. Saadoun S, Waters P, Bell BA, Vincent A, Verkman AS, Papadopoulos MC. Intra-cerebral injection of neuromyelitis optica immunoglobulin G and human complement produces neuromyelitis optica lesions in mice. Brain. 2010;133(Pt 2):349–361. doi:10.1093/brain/awp309
9. Moriconi A, Cunha TM, Souza GR, et al. Targeting the minor pocket of C5aR for the rational design of an oral allosteric inhibitor for inflammatory and neuropathic pain relief. Proc Natl Acad Sci U S A. 2014;111(47):16937–16942. doi:10.1073/pnas.1417365111
10. Shi X, Guo TZ, Li WW, et al. C5a complement and cytokine signaling mediate the pronociceptive effects of complex regional pain syndrome patient IgM in fracture mice. Pain. 2021;162(5):1400–1415. doi:10.1097/j.pain.0000000000002150
11. Shutov LP, Warwick CA, Shi X, et al. The complement system component C5a produces thermal hyperalgesia via macrophage-to-nociceptor signaling that requires NGF and TRPV1. J Neurosci. 2016;36(18):5055–5070. doi:10.1523/JNEUROSCI.3249-15.2016
12. Griffin RS, Costigan M, Brenner GJ, et al. Complement induction in spinal cord microglia results in anaphylatoxin C5a-mediated pain hypersensitivity. J Neurosci. 2007;27(32):8699–8708. doi:10.1523/JNEUROSCI.2018-07.2007
13. Quadros AU, Cunha TM. C5a and pain development: an old molecule, a new target. Pharmacol Res. 2016;112:58–67. doi:10.1016/j.phrs.2016.02.004
14. Sepulveda M, Delgado-García G, Blanco Y, et al. Late-onset neuromyelitis optica spectrum disorder: the importance of autoantibody serostatus. Neurol Neuroimmunol Neuroinflamm. 2019;6(6):e607. doi:10.1212/NXI.0000000000000607
15. Uzawa A, Mori M, Hayakawa S, Masuda S, Nomura F, Kuwabara S. Expression of chemokine receptors on peripheral blood lymphocytes in multiple sclerosis and neuromyelitis optica. BMC Neurol. 2010;10:113. doi:10.1186/1471-2377-10-113
16. Portenoy R. Development and testing of a neuropathic pain screening questionnaire: ID Pain. Curr Med Res Opin. 2006;22(8):1555–1565. doi:10.1185/030079906X115702
17. Li J, Feng Y, Han J, et al. Linguistic adaptation, validation and comparison of 3 routinely used neuropathic pain questionnaires. Pain Phy. 2012;15(2):179–186.
18. Valerio F, Apostolos-Pereira SL, Sato DK, et al. Characterization of pain syndromes in patients with neuromyelitis optica. Eur J Pain. 2020;24(8):1548–1568. doi:10.1002/ejp.1608
19. Jiao Y, Fryer JP, Lennon VA, et al. Updated estimate of AQP4-IgG serostatus and disability outcome in neuromyelitis optica. Neurology. 2013;81(14):1197–1204. doi:10.1212/WNL.0b013e3182a6cb5c
20. Waters P, Reindl M, Saiz A, et al. Multicentre comparison of a diagnostic assay: aquaporin-4 antibodies in neuromyelitis optica. J Neurol Neurosurg Psychiatry. 2016;87(9):1005–1015. doi:10.1136/jnnp-2015-312601
21. Hinson SR, Romero MF, Popescu BF, et al. Molecular outcomes of neuromyelitis optica (NMO)-IgG binding to aquaporin-4 in astrocytes. Proc Natl Acad Sci U S A. 2012;109(4):1245–1250. doi:10.1073/pnas.1109980108
22. Pittock SJ, Berthele A, Fujihara K, et al. Eculizumab in Aquaporin-4-positive neuromyelitis optica spectrum disorder. N Engl J Med. 2019;381(7):614–625. doi:10.1056/NEJMoa1900866
23. Singh P, Gao X, Kleijn HJ, Bellanti F, Pelto R. Eculizumab pharmacokinetics and pharmacodynamics in patients with neuromyelitis optica spectrum disorder. Front Neurol. 2021;12:696387. doi:10.3389/fneur.2021.696387
24. Kuroda H, Fujihara K, Takano R, et al. Increase of complement fragment C5a in cerebrospinal fluid during exacerbation of neuromyelitis optica. J Neuroimmunol. 2013;254(1–2):178–182. doi:10.1016/j.jneuroim.2012.09.002
25. Mahajan SD, Parikh NU, Woodruff TM, et al. C5a alters blood-brain barrier integrity in a human in vitro model of systemic lupus erythematosus. Immunology. 2015;146(1):130–143. doi:10.1111/imm.12489
26. Lucchinetti CF, Mandler RN, McGavern D, et al. A role for humoral mechanisms in the pathogenesis of Devic’s neuromyelitis optica. Brain. 2002;125(Pt 7):1450–1461. doi:10.1093/brain/awf151
27. Bradl M, Misu T, Takahashi T, et al. Neuromyelitis optica: pathogenicity of patient immunoglobulin in vivo. Ann Neurol. 2009;66(5):630–643. doi:10.1002/ana.21837
28. Ricklin D, Hajishengallis G, Yang K, Lambris JD. Complement: a key system for immune surveillance and homeostasis. Nat Immunol. 2010;11(9):785–797. doi:10.1038/ni.1923
29. Uzawa A, Mori M, Arai K, et al. Cytokine and chemokine profiles in neuromyelitis optica: significance of interleukin-6. Mult Scler. 2010;16(12):1443–1452. doi:10.1177/1352458510379247
30. Hisahara S, Iwahara N, Matsushita T, et al. SIRT1 decelerates morphological processing of oligodendrocyte cell lines and regulates the expression of cytoskeleton-related oligodendrocyte proteins. Biochem Biophys Res Commun. 2021;546:7–14. doi:10.1016/j.bbrc.2021.01.095
31. Pellkofer HL, Kümpfel T. [Pain in multiple sclerosis and neuromyelitis optica spectrum disorders]. Schmerz. 2021;35(3):211–222. German. doi:10.1007/s00482-021-00554-5
32. Baron R. Mechanisms of disease: neuropathic pain–a clinical perspective. Nat Clin Pract Neurol. 2006;2(2):95–106. doi:10.1038/ncpneuro0113
33. Zhao S, Mutch K, Elsone L, Nurmikko T, Jacob A. Neuropathic pain in neuromyelitis optica affects activities of daily living and quality of life. Mult Scler. 2014;20(12):1658–1661. doi:10.1177/1352458514522103
34. Giorgio C, Zippoli M, Cocchiaro P, et al. Emerging role of C5 complement pathway in peripheral neuropathies: current treatments and future perspectives. Biomedicines. 2021;9(4):399. doi:10.3390/biomedicines9040399
35. Li YH, Jin H, Xu JS, Guo GQ, Chen DL, Bo Y. Complement factor C5a and C5a receptor contribute to morphine tolerance and withdrawal-induced hyperalgesia in rats. Exp Ther Med. 2012;4(4):723–727. doi:10.3892/etm.2012.636
36. Jang JH, Clark DJ, Li X, Yorek MS, Usachev YM, Brennan TJ. Nociceptive sensitization by complement C5a and C3a in mouse. Pain. 2010;148(2):343–352. doi:10.1016/j.pain.2009.11.021
37. Warwick CA, Shutov LP, Shepherd AJ, Mohapatra DP, Usachev YM. Mechanisms underlying mechanical sensitization induced by complement C5a: the roles of macrophages, TRPV1, and calcitonin gene-related peptide receptors. Pain. 2019;160(3):702–711. doi:10.1097/j.pain.0000000000001449
38. Jang JH, Liang D, Kido K, Sun Y, Clark DJ, Brennan TJ. Increased local concentration of complement C5a contributes to incisional pain in mice. J Neuroinflammation. 2011;8:80. doi:10.1186/1742-2094-8-80
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
