Back to Journals » Nature and Science of Sleep » Volume 15
Association of Objective Sleep Characteristics and Incident Angina Pectoris: A Longitudinal Analysis from the Sleep Heart Health Study
Authors Liu J, Zhu Y , Chang Y, Xu Z , Wang C, Zhang P , Li S, Yang W, An R, Wen D, Xu J, Zheng M
Received 6 July 2023
Accepted for publication 14 November 2023
Published 22 November 2023 Volume 2023:15 Pages 955—965
DOI https://doi.org/10.2147/NSS.S429231
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Valentina Alfonsi
Jiali Liu,1,* Yuanqiang Zhu,1,* Yingjuan Chang,1,* Ziliang Xu,1 Chen Wang,1 Pengpeng Zhang,1 Shuangxin Li,1 Wenxuan Yang,1 Rui An,1,2 Didi Wen,1 Jian Xu,1,2 Minwen Zheng1
1Department of Radiology, Xijing Hospital, Air Force Medical University, Xi’an, Shaanxi, People’s Republic of China; 2Department of Interventional Surgery Center, Xijing Hospital, Air Force Medical University, Xi’an, Shaanxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Minwen Zheng, Department of Radiology, Xijing Hospital, Air Force Medical University, 127# Changle West Road, Xi’an, Shaanxi, 710032, People’s Republic of China, Tel +86-29-84775421, Fax +86-29-84773732, Email [email protected] Jian Xu, Department of Interventional Surgery Center, Xijing Hospital, Air Force Medical University, 127# Changle West Road, Xi’an, Shaanxi, 710032, People’s Republic of China, Tel +86-29-84775299, Fax +86-29-84775299, Email [email protected]
Purpose: While prior research has highlighted a significant association between sleep characteristics and angina pectoris (AP) incidence, the link between sleep efficiency (SE) and angina remains unexplored. This study seeks to elucidate the relationship between AP and objectively quantified SE.
Patients and Methods: We examined a cohort of 2990 participants (1320 males and 1670 females; mean age 63.69 ± 13.2 years) from the Sleep Heart Health Study. The main exposure variable was SE, as determined by baseline home polysomnography, while the primary outcome was the first incidence of angina pectoris (AP) during the period between the baseline polysomnography and the end of follow-up. A multivariate Cox regression model was utilized, controlling for factors such as age, gender, BMI, smoking and alcohol consumption habits, diabetes, hypertension, sleep duration, triglycerides, cholesterol, high-density lipoprotein, apnea-hypopnea index, nocturnal oxygen saturation, to analyze the relationship between SE and AP.
Results: During an average follow-up of 11 years, 284 patients developed AP. The unadjusted Kaplan-Meier analysis identified the 2nd quartile of SE as having the lowest AP risk. The multivariate Cox proportional hazards model demonstrated a higher risk of AP in quartile 1 (HR, 1.679; 95% CI, 1.109– 2.542; P < 0.014) and quartile 3 (HR, 1.503; 95% CI, 1.037– 2.179; P < 0.031), compared to quartile 2 of SE. Upon stratified analysis, this relationship was particularly pronounced in hypertensive individuals.
Conclusion: Our results highlight the critical role of optimal sleep efficiency in mitigating the risk of angina pectoris, especially among hypertensive individuals.
Keywords: sleep efficiency, angina pectoris, polysomnography, cardiovascular risk, sleep heart health study, hypertension
Introduction
Angina pectoris (AP), characterized by chest discomfort typically induced by physical exertion or emotional distress due to myocardial ischemia, remains a substantial global health concern, affecting millions of individuals each year.1 Beyond the immediate pain and discomfort, AP often signals an underlying, substantial risk of cardiovascular disease (CVD).2 Therefore, identifying contributing factors to AP, and by extension CVD, carries profound public health implications.
Among various lifestyle factors, the role of sleep, including both its quantity and quality, has garnered significant attention in recent years due to its potential association with cardiovascular health. Adequate, high-quality sleep is increasingly recognized as a cornerstone of both physical and mental well-being.3,4 Emerging evidence shows that optimal sleep patterns could reduce the risk of CVD.5,6 Conversely, poor sleep quality has been implicated in a heightened occurrence of cardiovascular events.7,8 This relationship is further emphasized by studies establishing a connection between sleep characteristics—such as sleep duration, sleep quality, and sleep apnea—and the incidence of AP. Therefore, we postulate that sleep efficiency (SE), a quantifiable, objective metric of sleep quality, could significantly influence the risk of AP.9–11
Interestingly, the protective effect of high-sleep quality on cardiovascular events does not follow a linear relationship as traditionally believed. Rather, contemporary research proposes a U- or J-shaped association, where neither the highest proportion of slow-wave sleep nor the least arousal burden corresponds to the lowest cardiovascular risk. Rather, It appears that moderate sleep indices may offer the most significant protective effect.12,13
Despite these findings, a knowledge gap persists in the current literature concerning the association between objective SE, as determined by polysomnography, and AP. This association warrants further investigation, particularly considering the nuanced relationship between sleep quality and cardiovascular health. Therefore, in this study, we aim to elucidate the relationship between AP and objectively measured SE using data from the Sleep Heart Health Study (SHHS) database. We hypothesize that a non-linear relationship exists between SE and AP risk, akin to the U- or J-shaped association observed between other sleep indices and cardiovascular events. Our findings aim to enhance the understanding of sleep’s role in cardiovascular health and could potentially inform strategies to improve sleep health and mitigate AP and CVD risk.
Methods
Study Design and Population
The Sleep Heart Health Study (SHHS) is a multicenter, community-based, prospective cohort study aimed at exploring the relationship between sleep-disordered breathing and cardiovascular disease. Between 1995 and 1998, this study recruited 6441 men and women aged 40 years or older without prior cardiovascular disease. Baseline assessments were conducted, which included collecting information on cardiovascular health and wellness habits, administering a sleep habit questionnaire, recording anthropometric measurements, and conducting overnight polysomnography (PSG) at home. The cohort was then followed for an average of 11 years for cardiovascular events and other outcomes. The study design details have been previously reported.14,15 All the participants provided written informed consent, and the study was approved by the institutional review board of each participating institution. We received access to the SHHS database by completing a signed agreement with Brigham and Women’s Hospital. Our study followed definitely the guidelines outlined in the Declaration of Helsinki. For this study, inclusion criteria were: (1) Availability of complete PSG data and clinical records, and (2) No prior history of AP. Participants with prior AP history (n=212) and without time-to-AP outcome events (n=1840) were excluded. Due to sovereignty issues, the Strong Heart Study participants (n=637) were not included in the SHHS dataset. A total of 2990 participants who met the selection criteria were included in this study. Figure 1 illustrates a flowchart of the participant data selection process.
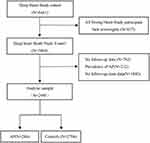 |
Figure 1 Eligibility criteria for the study population. |
Outcome Definition and Covariates
Angina pectoris was defined as “definitive angina pectoris” for the first onset during the SHHS, with a mean follow-up period of 11 years. Subjects were followed for cardiovascular events at least every 2 years. Cardiovascular events were identified through structured telephone or home interviews. In one of the SHHS cohorts (CHS cohort), potential events were identified by alternating telephone calls and clinic visits every 6 months. Inpatient and outpatient surgical records were obtained and extracted by trained personnel. In this study, criteria for ‘definite angina pectoris’ include an exercise stress test diagnostic for ischemia, coronary angiography demonstrating 70% narrowing of an epicardial coronary artery, or the occurrence of a surgical intervention. Only the ‘definite angina pectoris’ events will be utilized by the SHHS. ‘Possible angina pectoris’ was not considered an outcome.
All SHHS participants received a family, single-night, unattended PSG (P-Series; Compumedics, Abbotsville, Australia)and the PSG graded at the Central Reading Center. SE was calculated as the total sleep time divided by the total time in bed and multiplied by 100%. SE was categorized into quartile 1 (≥90.5%), quartile 2 (90.5–85.3%), quartile 3 (78.0–85.3%) and quartile 4 (<78.0%). Wake after sleep onset (WASO) was defined as the total awake time from the first time the participant fell asleep to the time the participant was fully awake. WASO was categorized into quartile 1 (<30min), quartile 2 (30–49.5min), quartile 3 (49.5–81.5min) and quartile 4 (≥81.5min). Sleep fragmentation index (SFI) was defined as the number of awakenings and sleep-stage shifts per hour. SFI was categorized into quartile 1 (<6.6 events/h), quartile 2 (6.6–8.5 events/h), quartile 3 (8.5–10.7 events/h) and quartile 4 (≥10.7 events/h). Total arousal index (ArI-total) was defined as the number of arousals per hour. Arl-total was categorized into quartile 1 (<12.0 events/h), quartile 2 (12.0–16.7 events/h), quartile 3 (16.7–23.5 events/h) and quartile 4 (≥23.5 events/h). Non-rapid eye movement arousal index (ArI-NREM) and rapid eye movement arousal index (ArI-REM) were measured based on the number of arousals per hour during NREM and REM sleep, respectively. Slow-wave sleep (SWS) was described as the third stage of non-REM sleep. REM sleep % was defined as the percentage of REM sleep captured by PSG. REM was categorized into quartile 1 (<15.6%), quartile 2 (15.6–20.0%), quartile 3 (20.0–23.8%) and quartile 4 (≥23.8%). Sleep duration was defined as total time in bed. The apnea-hypopnea index (AHI) was defined as all apnea and hypopnea occurrences per hour of sleep accompanied by at least a 4% drop in oxygen saturation. The Epworth sleepiness score (ESS) score was assessed using an eight-item self-report questionnaire. Participants were considered sleepy if ESS scored 11 or higher.
Baseline demographic, lifestyle, and medical information were collected from the SHHS, including age, sex, ethnicity, smoking status, body mass index (BMI), alcohol consumption, diabetes status, hypertension status, sleep duration, AHI, triglycerides, total cholesterol, high-density lipoprotein (HDL) and ESS questionnaire scores. Based on the common classification methods, sleep duration (< 6 h vs 6 ~ 8 h vs > 8 h) and smoking state (current vs former vs never) were divided into three categories, and AHI (< 5, 5–15, 15–30, ≥30) was divided into four categories.
Statistical Analysis
Baseline characteristics differences between AP patients and controls were analyzed using an independent sample t-test for continuous variables and chi-square test for categorical variables. Continuous variables were expressed as mean ± standard deviation, and categorical variables as percentages. An unadjusted Kaplan-Meier plot was employed to evaluate the association between quartiles of SE, WASO, SFI, Arl, REM, SWS and the incidence of AP. Univariate and multivariate Cox regression analyses were used to explore the association between sleep characteristics and AP occurrence. Clinically relevant baseline variables or those showing a univariate relationship with the outcome were included in the multivariate Cox proportional-hazards regression model. In sleep efficiency, quartile 2 was chosen as the reference due to its lowest incidence of AP. Similarly, quartile 3 was chosen as the reference for SWS and REM. These results were expressed as hazard ratios (HR) with 95% confidence intervals (CIs). The potential interaction between SE and other variables was examined in multivariate Cox regression analysis. Restricted cubic splines were used to explore potential non-linear associations of continuous variables with the outcome. All statistical analyses and calculations were performed using SPSS 26.0 and R statistical software. Statistical significance was considered at two-sided P-values <0.05.
Results
Participant Characteristics
This study included a total of 2990 participants, with 284 AP patients and 2706 control participants. About 56% of the participants were female, 80% were white, and the mean age was 63.9 ± 13.2 years. The analysis revealed that the AP group consisted of significantly older participants with higher BMI, more likely to be female, and had a greater proportion of individuals with diabetes and hypertension. Furthermore, AP patients exhibited higher WASO, SFI, Arl, Arl-nrem, REM, ESS score, AHI, and SaO2 values than the control group. Conversely, their sleep efficiency and slow-wave sleep were lower than those in the control group. The participant characteristics, categorized by AP presence, are detailed in Tables 1 and 2.
 |
Table 1 Clinical Characteristics of Participants with or Without AP |
 |
Table 2 Sleep Characteristics of Participants with or Without AP |
Association of Sleep Characteristics with Incidence of AP
The unadjusted Kaplan-Meier analysis demonstrated the incidence of AP in the SE, WASO, SFI, ArI, REM and SWS (Figure 2). A significant association was found between the incidence of AP and the severity of sleep fragmentation, particularly in terms of SE and wake WASO (P<0.001). Participants with the lowest SE (<78.0%) had the highest incidence of AP, while those in quartile 2 (85.3% to 90.5%) had the lowest. Participants with the highest WASO (≥81.5 min) had the highest AP incidence, whereas those in quartile 1 (<30 min) had the lowest. In addition to this, participants with the lowest REM (<15.6%) had the highest incidence of AP, while participants with the 3 quartile (20.0% to 23.8%) had the lowest incidence.
Association of Sleep Efficiency with Incidence of AP
Table 3 presents the associations between SE quartiles and incident AP, using quartile 2 as the reference. After adjusting for age, sex, BMI, smoking status, alcohol use, diabetes mellitus, hypertension, sleep duration, triglyceride, total cholesterol HDL, AHI, and percentage of sleep time with SaO2 <90%, quartile 1 and quartile 3 of SE was significantly associated with the incidence of AP. Furthermore, a statistically significant interaction, stratified by hypertension, was observed between SE (Pinteraction <0.05) and the incidence of AP, leading to further investigation of the association of SE with incident AP in participants with or without hypertension (Table 4).
 |
Table 3 Univariable and Multivariable Cox Regression Analysis for Sleep Characteristics Associated with AP |
 |
Table 4 Univariable and Multivariable Cox Regression Analysis for SE Associated with AP Stratified by Hypertension |
In univariate analysis, participants who with hypertension in quartile 1(HR, 1.714; 95% CI, 1.009–2.909; P =0.046), quartile 3(HR, 2.154; 95% CI, 1.340–3.462; P = 0.002), and quartile 4(HR, 1.753; 95% CI, 1.093–2.812; P = 0.020) all had significantly higher risk of AP compared to quartile 2. After multivariable Cox regression analysis, participants who with hypertension in quartile 1(HR, 2.019; 95% CI, 1.164–3.500; P =0.046) and quartile 3(HR, 1.770; 95% CI, 1.085–2.888; P = 0.022) still had significantly higher risk of AP compared with quartile 2 (Table 4). A U-shaped association between sleep efficiency and AP can be observed on restriction cube splines (Figure 3).
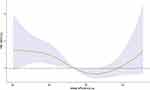 |
Figure 3 Restricted spline curve for association between estimated SE and AP. |
Correlation Between AP and WASO, SFI, Arl, SWS, REM, Arl-nrem, Arl-rem, or ESS
In the unvariate Cox regression analysis, AP were significantly associated with WASO, SFI, Arl, SWS, REM, Arl-nrem, Arl-rem, or ESS. However, in multivariate Cox regression analysis, only REM in quartile 1 (HR, 1.421; 95% CI, 1.002–2.016; P <0.049) and quartile 2 (HR, 1.445; 95% CI, 1.003–2.083; P =0.048) was associated with AP after adjusting for age and gender, and the association between the remaining sleep parameters and AP was not significant (Table 3).
Discussion
This study, to our knowledge, is the first longitudinal investigation utilizing PSG data to examine the relationship between objectively measured sleep efficiency and the risk of AP. Our findings indicate that sleep efficiency significantly influences the development of AP after accounting for age, sex, BMI, smoking status, alcohol use, diabetes, hypertension, sleep duration, triglycerides, and cholesterol and high-density lipoprotein levels. At present, sleep insufficient and poor sleep quality have shown to be strongly associated with AP,11,16 but little is known about the relationship between objectively measured sleep efficiency and AP. Furthermore, our results suggested a U-shaped association between sleep efficiency and AP risk, with the lowest risk observed in the second quartile.
Our study distinguishes itself from the recent work by Sobhan Salari Shahrbabaki et al, published in the European Heart Journal (2021),12 which primarily focused on the relationship between sleep wake burden and overall cardiovascular events. In contrast, our research delved into a statistical analysis of commonly used clinical measures reflecting sleep fragmentation, emphasizing sleep efficiency and its connection to angina pectoris specifically. Angina pectoris often serves as an initial, warning manifestation of cardiovascular disease, and its investigation can provide crucial early insights into cardiovascular health risks. Furthermore, the decision to concentrate on angina pectoris, instead of broader cardiovascular morbidity and mortality, was informed by previous reports linking sleep fragmentation to cardiometabolic factors. Given that angina pectoris is strongly associated with these cardiometabolic factors, we hypothesized that an objective measurement of sleep characteristics might reveal significant correlations with this condition. Our results support this hypothesis, highlighting the nuanced role of sleep efficiency in the onset of angina, and underscoring the importance of sleep quality in cardiovascular health.
Several epidemiological studies have found that sleep insufficiency heightens the risk of cardiovascular disease,16 obesity,17,18 and diabetes,19 yet our understanding of the mechanisms underlying these associations is still incomplete. In order to study the protective effect of sleep on cardiovascular disease, Carras et al treated mice with sleep fragmentation and found that long-term SF induced the activation of NADPH oxidase and increased oxidative stress, inducing vascular endothelial dysfunction.20,21 McAlpine et al conducted similar experiments and found that mice treated with sleep fragmentation produced more Ly-6Chi monocytes and formed larger atherosclerotic lesions.22 These factors could lead to the formation of atherosclerotic plaque, luminal narrowing, or even vessel occlusion, triggering APor acute myocardial infarction.23
We observed a more pronounced U-shaped association between sleep efficiency and APin hypertensive individuals. This could be attributed to fragmented sleep reducing non-REM sleep duration, hyperactivating the hypothalamic-pituitary-adrenal axis, and escalating sympathetic tone.24 Increased sympathetic activity, an independent cardiovascular risk factor, may raise peripheral vascular resistance, thereby increasing blood pressure, heart rate, myocardial oxygen demand, and decreasing coronary blood flow, thereby predisposing to AP.25,26 While larger studies are required to assess the relationship between AP risk and sleep efficiency, the U-shaped association we observed echoes findings linking sleep duration with various cardiovascular outcomes and cardiometabolic risk factors.
Our study also demonstrated how the age of participants could influence the relationship between sleep efficiency and AP risk. Sleep efficiency was not associated with AP incidence in the univariate Cox analysis when sleep efficiency was ≥ 90.5%, however, after adjusting for age and sex, sleep efficiency significantly correlated with AP incidence. This observation might be attributable to the larger proportion of young people in the high sleep efficiency group. Conversely, in participants with sleep efficiency < 78.0%, after adjusting for age and sex, no association was found between sleep efficiency and AP, possibly due to older individuals constituting a higher proportion of this group and the age-related decrease in sleep needs.27–29
Our study provides a new perspective on the relationship between objectively measured sleep efficiency and the risk of AP. The results demonstrate a U-shaped association, indicating both higher and lower sleep efficiency than the optimal range can increase AP risk, especially in individuals with hypertension. The results, thus, emphasize the critical role of adequate sleep in cardiovascular health and the importance of screening and managing sleep disorders to potentially mitigate the risk of AP. The strengths of our study include the large, community-based prospective design, enhancing the generalizability of our results, and the use of PSG for standard, objective measurement of sleep parameters, which increases accuracy. However, our study has several limitations. Firstly, while we employed age as a covariate in our multivariate analyses to mitigate its influence, we acknowledge that an age-matched control group could offer a more isolated view of SE’s effects on AP incidence. However, this strategy would require the exclusion of a substantial portion of our diverse data, potentially constraining the breadth of our conclusions. Additionally, the multifaceted impacts of age on the cardiovascular system are challenging to disentangle from the cumulative events of a lifetime, encompassing various known and yet-to-be-discovered factors influencing the cardiovascular system. Secondly, the observational nature of our study presents complexities in definitively establishing a causal relationship between sleep efficiency (SE) and AP, notably, the U-shaped association we observed is nuanced, influenced by the older age and more frequent comorbidities in the AP group. Future studies could enrich understanding by employing an age-matched cohort and delving deeper into the potential confounders identified, including medication use and the “healthy user effect”. Additionally, all participants were middle-aged or elderly, and the majority were white, consequently, our findings may not be applicable to all ethnic groups or younger populations. Lastly, our use of a single night’s PSG data may limit the accuracy of sleep efficiency measurements, and multiple PSG recordings over an extended period could provide more precise information.
Conclusion
Our study based on polysomnography confirms the correlation of objective measures of SE with AP. The results showed a U-shaped relationship between SE and the risk of AP, highlighting the key role of optimal SE in reducing the risk of angina, especially in patients with hypertension.
Acknowledgments
The authors thank the investigators, the staff, and the participants of the SHHS study for their valuable contributions. The Sleep Heart Health Study (SHHS) was supported by National Heart, Lung, and Blood Institute cooperative agreements U01HL53916 (University of California, Davis), U01HL53931 (New York University), U01HL53934 (University of Minnesota), U01HL53937 and U01HL64360 (Johns Hopkins University), U01HL53938 (University of Arizona), U01HL53940 (University of Washington), U01HL53941 (Boston University), and U01HL63463 (Case Western Reserve University). The National Sleep Research Resource was supported by the National Heart, Lung, and Blood Institute (R24 HL114473, 75N92019R002).
Funding
This study has received funding by the Key R&D Program Projects of Shaanxi, China (2022JM-575 and 2021SF-287), Fast Response Program of Air Force Medical University (2023KXKT050), Boost Program of Xijing Hospital (JSYXM28, JSYXZ08 and XJZT21CM21), and Young Eagle Project of Air Force Medical University (2020CYJHFP).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–477. doi:10.1093/eurheartj/ehz425
2. Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254–e743. doi:10.1161/CIR.0000000000000950
3. Kim B, Branas CC, Rudolph KE, et al. Neighborhoods and sleep health among adults: a systematic review. Sleep Health. 2022;8(3):322–333. doi:10.1016/j.sleh.2022.03.005
4. Mp SO, Ma G, B D, et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation. 2016;134(18). doi:10.1161/CIR.0000000000000444
5. Fan M, Sun D, Zhou T, et al. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: a prospective study of 385 292 UK biobank participants. Eur Heart J. 2020;41(11):1182–1189. doi:10.1093/eurheartj/ehz849
6. Zhong Q, Qin Z, Wang X, et al. Healthy sleep pattern reduce the risk of cardiovascular disease: a 10-year prospective cohort study. Sleep Med. 2023;105:53–60. doi:10.1016/j.sleep.2023.03.003
7. Wang C, Bangdiwala SI, Rangarajan S, et al. Association of estimated sleep duration and naps with mortality and cardiovascular events: a study of 116 632 people from 21 countries. Eur Heart J. 2019;40(20):1620–1629. doi:10.1093/eurheartj/ehy695
8. Kwok CS, Kontopantelis E, Kuligowski G, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response meta-analysis. J Am Heart Assoc. 2018;7(15):e008552. doi:10.1161/JAHA.118.008552
9. Aggarwal S, Loomba RS, Arora RR, Molnar J. Associations between sleep duration and prevalence of cardiovascular events. Clin Cardiol. 2013;36(11):671–676. doi:10.1002/clc.22160
10. Chan HS, Chiu HF, Tse LK, Woo KS. Obstructive sleep apnea presenting with nocturnal angina, heart failure, and near-miss sudden death. Chest. 1991;99(4):1023–1025. doi:10.1378/chest.99.4.1023
11. Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the national health interview survey. Sleep. 2010;33(8):1037–1042. doi:10.1093/sleep/33.8.1037
12. Shahrbabaki SS, Linz D, Hartmann S, Redline S, Baumert M. Sleep arousal burden is associated with long-term all-cause and cardiovascular mortality in 8001 community-dwelling older men and women. Eur Heart J. 2021;42(21):2088–2099. doi:10.1093/eurheartj/ehab151
13. Javaheri S, Zhao YY, Punjabi NM, Quan SF, Gottlieb DJ, Redline S. Slow-wave sleep is associated with incident hypertension: the Sleep Heart Health Study. Sleep. 2018;41(1):zsx179. doi:10.1093/sleep/zsx179
14. Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. Sleep. 1997;20(12):1077–1085.
15. Zhang GQ, Cui L, Mueller R, et al. The national sleep research resource: towards a sleep data commons. J Am Med Inform Assoc. 2018;25(10):1351–1358. doi:10.1093/jamia/ocy064
16. Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484–1492. doi:10.1093/eurheartj/ehr007
17. Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. doi:10.1093/sleep/31.5.619
18. Zhao B, Sun S, He X, Yang J, Ma X, Yan B. Sleep fragmentation and the risk of obesity: the Sleep Heart Health Study. Obesity. 2021;29(8):1387–1393. doi:10.1002/oby.23193
19. Shan Z, Ma H, Xie M, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529–537. doi:10.2337/dc14-2073
20. Zhang SXL, Khalyfa A, Wang Y, et al. Sleep fragmentation promotes NADPH oxidase 2-mediated adipose tissue inflammation leading to insulin resistance in mice. Int J Obes. 2014;38(4):619–624. doi:10.1038/ijo.2013.139
21. Carreras A, Zhang SX, Peris E, et al. Chronic sleep fragmentation induces endothelial dysfunction and structural vascular changes in mice. Sleep. 2014;37(11):1817–1824. doi:10.5665/sleep.4178
22. McAlpine CS, Kiss MG, Rattik S, et al. Sleep modulates haematopoiesis and protects against atherosclerosis. Nature. 2019;566(7744):383–387. doi:10.1038/s41586-019-0948-2
23. Boudoulas KD, Triposciadis F, Geleris P, Boudoulas H. Coronary atherosclerosis: pathophysiologic basis for diagnosis and management. Prog Cardiovasc Dis. 2016;58(6):676–692. doi:10.1016/j.pcad.2016.04.003
24. Ramos AR, Weng J, Wallace DM, et al. Sleep patterns and hypertension using actigraphy in the Hispanic Community Health Study/Study of Latinos. Chest. 2018;153(1):87–93. doi:10.1016/j.chest.2017.09.028
25. Malliani A, Montano N. Emerging excitatory role of cardiovascular sympathetic afferents in pathophysiological conditions. Hypertension. 2002;39(1):63–68. doi:10.1161/hy0102.099200
26. Seravalle G, Mancia G, Grassi G. Sympathetic nervous system, sleep, and hypertension. Curr Hypertens Rep. 2018;20(9):74. doi:10.1007/s11906-018-0874-y
27. Dijk DJ, Groeger JA, Stanley N, Deacon S. Age-related reduction in daytime sleep propensity and nocturnal slow wave sleep. Sleep. 2010;33(2):211–223. doi:10.1093/sleep/33.2.211
28. Klerman EB, Dijk DJ. Age-related reduction in the maximal capacity for sleep--implications for insomnia. Curr Biol. 2008;18(15):1118–1123. doi:10.1016/j.cub.2008.06.047
29. Münch M, Knoblauch V, Blatter K, et al. The frontal predominance in human EEG delta activity after sleep loss decreases with age. Eur J Neurosci. 2004;20(5):1402–1410. doi:10.1111/j.1460-9568.2004.03580.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

