Back to Journals » Journal of Inflammation Research » Volume 16
Association of M-Type Phospholipase A2 Receptor Deposition in Kidney Tissue with Treatment Outcomes in Patients with Idiopathic Membranous Nephropathy
Authors Xie NQ, Zhang YL, Zheng ZL, Zheng QL, Chen RJ
Received 21 June 2023
Accepted for publication 17 November 2023
Published 22 December 2023 Volume 2023:16 Pages 6319—6328
DOI https://doi.org/10.2147/JIR.S427045
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Ning-Qiu Xie,1,* Yu-Lin Zhang,2,* Zi-Li Zheng,1 Quan-Lin Zheng,1 Ruo-Ji Chen1
1Department of Nephrology, Jinjiang Municipal Hospital, Jinjiang, Fujian, 362200, People’s Republic of China; 2Department of Pediatric, Jinjiang Municipal Hospital, Jinjiang, Fujian, 362200, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ruo-Ji Chen, Department of Nephrology, Jinjiang Municipal Hospital, Baolong International Community, Changxing Road, 288 Qingyang Street, Jinjiang, Fujian, 362200, People’s Republic of China, Tel +86 13665970368, Email [email protected]
Objective: The purpose of this study was to investigate the correlation between the deposition of M-type phospholipase A2 receptor (PLA2R) in the kidney tissues of patients with idiopathic membranous nephropathy (IMN).
Method: We enrolled a total of 61 patients diagnosed with IMN in the past 8 years who were admitted at the Jinjiang Municipal Hospital and the 2nd Affiliated Hospital of Fujian Medical University. PLA2R immunofluorescence was used to stain kidney tissues, and all patients were treated with steroid combined with immunosuppressive agents or conservative regimens. The duration of follow-up was more than 48 weeks. Based on the deposition of PLA2R in kidney tissues, we divided the patients into the PLA2R Positive group and the PLA2R Negative group. Further, patients with PLA2R-positive kidney tissues were divided into “ 1+”, “ 2+”, and “ 3+” groups based on the extent of their PLA2R deposition, and we compared the therapeutic outcomes of the various groups.
Results: At week 12 of follow-up, the partial remission rate of kidney tissues in the PLA2R Negative group was significantly higher than that in the Positive group (P = 0.004). Among the various deposition groups with PLA2R-positive kidney tissues, the complete remission rate of the “ 2+” group was higher than that of the “ 3+” group at weeks 24, 36, and 48 of follow-up (P < 0.05). In IMN patients treated with a combination regimen of steroid and tacrolimus, the complete remission rate in kidney tissues of the PLA2R Negative group was higher than that of the Positive group at weeks 24 and 48 of follow-up (P < 0.05).
Conclusion: The overall effective rate of treatment in kidney tissues of PLA2R-negative patients was higher than that in the kidney tissues of PLA2R-positive patients. The varied levels of PLA2R deposition in kidney tissues were related to the treatment outcomes of IMN, and those with lower PLA2R deposition levels had better outcomes.
Keywords: anti-M-type phospholipase A2 receptor, idiopathic membranous nephropathy, IgG4
Corrigendum for this paper has been published.
Introduction
Idiopathic membranous nephropathy (IMN) is an autoimmune glomerulopathy commonly seen in clinical practice. Its incidence has been increasing in recent years, making it the most common cause of nephrotic syndrome in non-diabetic adults worldwide.1 IMN is characterized by diffuse thickening of the glomerular basement membrane accompanied by the deposition of many immune complexes under epithelial cells. The granular deposition of C3 and IgG along the glomerular capillary wall can be seen as immunofluorescence.2 The discovery of PLA2R in kidney podocytes of IMN patients by Beck et al at the beginning of this century3 triggered new insights and continuous in-depth research on IMN.
Currently, several studies have confirmed the significance of PLA2R antibody levels in the diagnosis of IMN, disease activity, and prognosis evaluation.4–6 However, serum PLA2R antibody titers are easily impacted by the immune response and immunosuppressants of the human body. Detecting PLA2R deposition in kidney tissues in the early stages of the disease using immunofluorescence staining can aid in identifying early PLA2R related membranous nephropathy before serum PLA2R antibodies are produced. As a result, studying the detection of PLA2R in kidney tissues has important value in the clinical diagnosis and prognosis evaluation of diseases. Most current research suggests that the deposition of PLA2R in kidney tissues of IMN patients is unrelated to the severity of the condition,7 but there are also a few studies that have confirmed that IMN patients with positive PLA2R deposition in kidney tissues are more severely affected in terms of urinary protein, kidney function damage, and kidney interstitial tubular lesions than those with negative PLA2R deposition.8
With respect to treatment efficacy, most studies concur that immunosuppressive treatment is more efficacious in IMN patients with negative PLA2R deposition in kidney tissues than those with positive PLA2R deposition in kidney tissues.9 There is also a paucity of research on the relationship between the intensity of PLA2R deposition in kidney tissues and treatment efficacy in IMN patients. Therefore, in this study, we compared and analyzed the deposition and intensity of PLA2R in kidney tissues with the treatment efficacy of IMN patients to further understand the relationship between PLA2R deposition in kidney tissues and IMN disorders. The results of this research may provide a valuable reference for the future clinical diagnosis and management of this disease.
Materials and Methods
Study Respondents
We selected patients who were admitted to the Jinjiang Municipal Hospital and the 2nd Affiliated Hospital of Fujian Medical University between January 2015 and January 2023 to be enrolled in this study. Patients also underwent laboratory investigations to check for antinuclear antibody (ANA), extractable nuclear antigens (ENA), tumor markers, and infectious diseases to exclude secondary membranous nephropathy (SMN). A total of 61 patients with IMN were diagnosed through kidney biopsy pathology, and kidney biopsy samples were subjected to PLA2R immunofluorescence staining. Patients received standardized treatment and were maintained on regular follow-up. Complete follow-up treatment lasted more than 48 weeks.
Inclusion and Exclusion Criteria
Inclusion criteria: (1) Patients who fulfilled the diagnostic criteria for IMN as per the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines.10 (2) Patients aged between 18 and 75 years, irrespective of gender; (3) Kidney tissues where PLA2R deposition was detected, with pathological stages ranging from I to III; patients on regular outpatient follow-up after discharge, with complete follow-up treatment and pathology data; (4) Patients where contraindications have been checked for, who consented to use cyclosporin A (CsA), tacrolimus (TAC), cyclophosphamide (CTX) combined with glucocorticoids for treatment during the treatment process or only received conservative treatment, signed an informed consent form, and underwent treatment for a minimum of 48 weeks. (5) The follow-up duration was more than 48 weeks; (6) The patient was not treated with steroid or immunosuppressants in the past.
Exclusion criteria: (1) The presence of other kidney diseases; (2) The patient had serious complications such as severe infections; (3) The patient had diseases that are not suitable for immunosuppressive therapy, such as cancer and active gastrointestinal bleeding; (4) The patient had sensitivity to allergens; was allergic to the relevant treatment drugs.
Treatment Plan
The treatment regimen consisted of steroid therapy combined with CTX, steroid therapy combined with TAC, steroid therapy combined with CsA, or conservative supportive treatment.
Steroid therapy combined with cyclophosphamide: Patients were administered prednisone 1 mg/kg d orally, and this dosage was gradually reduced after 8 weeks as follows: the original dose was reduced by 10% every 2 weeks to 0.5 mg/kg · d, the dose was reduced by 5 mg each month to reach a maintenance dose of 5 mg per day, and the treatment was continued for at least 48 weeks. Two intravenous infusions of cyclophosphamide 1.0 g/month were administered, with a total dose of 150 mg/kg.
Low dose steroid therapy combined with tacrolimus: Patients were administered oral prednisone 0.15 mg/kg per day, taken orally at 8:00 a.m. after meals, and were maintained on this dosage for at least 48 weeks. The administration regimen for tacrolimus was as follows: The daily dose was within the range of 0.05–0.075 mg/kg, taken orally twice a day, every 12 hours, for six months. The level of tacrolimus concentration in the blood was measured after one week, and then once a month. The trough concentration was maintained at 5–10 ug/L. After six months of treatment, if clinical complete or partial remission was achieved, the dosage was gradually reduced, maintained for at least 48 weeks, and continued for a maximum of 1.5 years.
Administration regimen of cyclosporine A: The daily dose was within the range of 3.5–5.0 mg/kg, taken orally twice, every 12 hours, for six months. The blood concentration level of cyclosporine A was measured after one week, and then once a month. The trough concentration was maintained at 104–146 nmol/L, and a concentration of 333–500 nmol/L was maintained for 2 hours after taking the medication. After six months of treatment, if complete or partial remission was achieved, the dosage was gradually reduced and maintained for at least 48 weeks, up to a maximum of 1.5 years.
Conservative treatment focused on supportive symptomatic treatment and close monitoring during follow-up.
Follow-Up and Data Collection
Baseline Data Collection at the Time of Kidney Biopsy
Clinical information of the patient that was collected at the time of kidney biopsy included age, gender, 24-hour urine protein quantification, serum albumin, and creatinine, among other parameters. Pathology data that was gathered included the following details: pathology staging, light microscopy description, including glomerulosclerosis, mesangial cell proliferation, mesangial matrix hyperplasia, kidney tubular atrophy, kidney tubular fibrosis, interstitial inflammatory cell infiltration, kidney arteriosclerosis, and immunofluorescence staining for PLA2R, immunoglobulin G (IgG), immunoglobulin M (IgM), immunoglobulin A (IgA), immunoglobulin G1 (IgG1), immunoglobulin G4 (IgG4), complement component 3 (C3), and complement component 1q (C1q).
Follow-Up Duration and Content
Patients were followed up at weeks 12, 24, 36, and 48 of treatment, and 24-hour urine protein quantification, serum albumin, creatinine, and other indicators were collected.
Efficacy Evaluation
Treatment outcomes were defined as follows:
Complete remission (CR): Urinary protein excretion < 0.3 g/d, along with normal serum albumin concentration or serum creatinine value; Partial remission (PR): Urinary protein excretion < 3.5 g, with a decrease in urine protein exceeding 50% of the peak, along with improvement or return to normal serum albumin concentration and stable serum creatinine; No remission (NR): Those who did not fulfill the above indicators. Effective rate: the sum of complete and partial remission rates.
Study Content and Grouping
- Comparative analysis of PLA2R deposition in kidney tissues of IMN patients and their therapeutic outcomes;
- Kidney PLA2R-positive cases were divided into “1+”, “2+”, and “3+” groups (Figure 1) for comparison of treatment efficacy between the groups;
- Within the same treatment plan, we selected a larger number of patients on the steroid + TAC regimen and compared the therapeutic outcomes of different groups of PLA2R deposition in kidney tissues.
 |
Figure 1 (A) Kidney tissue PLA2R immunofluorescence positive 1+. (B) Kidney tissue PLA2R immunofluorescence positive 2+. (C) Kidney tissue PLA2R immunofluorescence positive 3+. |
Statistical Analysis
Normal measurement data were represented as x ± s, and we used independent sample t-tests for comparison between the two groups. Non-normal measurement data were represented by M (range), and comparisons between the two groups were conducted with the Mann Whitney U test. Counting data were represented using composition ratio, and the comparison between groups was done using chi-square test. Hierarchical data were represented using constituent ratios, and comparisons between two groups and multiple groups were done using rank sum tests. We used analysis of variance to compare measurement data between multiple groups. We analyzed the correlation between the parameters using Pearson correlation analysis for normal distribution data and Spearman correlation analysis for non-normal distribution and categorical variables. All data were statistically analyzed with SPSS 25.0 software, with P < 0.05 indicating a statistically significant difference.
Results
Analysis of General Data
We included a total of 61 patients in this study, and their general information is as follows:
- Gender: There were 36 males (59%) and 25 females (41%), with a male: female ratio of 1.5:1.
- Age: The age range of IMN patients was between 25 and 75 years, and there was no statistically significant difference in the age of patients of different genders (P > 0.05).
- Kidney PLA2R deposition: Among the 61 patients, 47 (77.1%) had positive kidney PLA2R deposition and 14 (22.9%) had negative kidney PLA2R deposition. Among them, kidney PLA2R deposition was mainly “1+” in 36 cases (59.0%), “2+” in 7 cases (11.5%), and “3+” in 4 cases (6.6%).
- Pathology staging.
Among the 61 IMN patients, the pathology staging was mainly stage II, with a total of 46 cases (75.4%), 6 cases (9.8%) in stage I, and 9 cases (14.7%) in stage III. There were significant differences in the intensity of PLA2R deposition in kidney tissues among patients with different pathology stages (P=0.003). (Details are shown in Table 1).
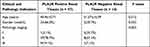 |
Table 1 Clinical and Pathology Staging Characteristics of Patients in the PLA2R Positive and Negative Renal Tissue Groups |
Correlation Between PLA2R Deposition and Treatment Outcomes in IMN
Comparison of Treatment Regimens and Outcomes Between PLA2R Positive and Negative Kidney Tissue Groups
There were 47 cases in the PLA2R Positive kidney tissue group, and this included 10 cases of steroid therapy + CTX, 18 cases of steroid therapy + TAC, 8 cases of steroid therapy + CsA, and 11 cases of conservative treatment, accounting for 21.3%, 38.3%, 17.0%, and 23.4%, respectively. There were 14 cases in the PLA2R Negative kidney tissue group, which included 3 cases of steroid therapy + CTX, 9 cases of steroid therapy + TAC, 2 cases of steroid therapy + CsA, and 0 case of conservative treatment, accounting for 21.4%, 64.3%, 14.3%, and 0.0%, respectively. There was no statistically significant difference in the treatment plan composition between the two groups (P = 0.174).
In terms of treatment outcomes, there was no statistically significant difference in CR and PR rates between the kidney PLA2R Negative group and the kidney PLA2R Positive group at weeks 24, 36, and 48 of follow-up (P > 0.05); The PR rate of the kidney PLA2R Negative group at week 12 was significantly higher than that of the kidney PLA2R Positive group (P = 0.004). There was no statistically significant difference in the effective rates between the two groups at follow-up weeks 12, 24, 36, and 48 (P > 0.05). (Details are given in Tables 2 and 3).
 |
Table 2 Comparison of Composition of Treatment Regimens Between PLA2R Positive and Negative Renal Tissue Groups |
 |
Table 3 Comparison of Therapeutic Effects Between PLA2R Antibody Positive and Negative Renal Tissue Groups |
Comparison of Treatment Regimens and Outcomes Between Different Deposition Groups Among Patients with PLA2R-Positive Kidney Tissues
There were a total of 47 cases with PLA2R-positive kidney tissues. Among these, there were 36 cases in the 1+ group distributed as follows: 8 cases of steroid therapy + CTX, 9 cases of steroid therapy + TAC, 8 cases of steroid therapy + CsA, and 11 cases of conservative treatment methods, respectively, accounting for 22.2%, 25.0%, 22.2%, and 30.6%, respectively. There were a total of 7 patients in the 2+ group, with 1 case of steroid therapy + CTX, 6 cases of steroid therapy + TAC, 0 case of steroid therapy + CsA, and 0 case of conservative treatment, accounting for 14.3%, 85.6%, 0.0%, and 0.0% of the total, respectively. There are a total of 4 patients in the 3+ group, with 1 case of steroid therapy + CTX, 3 cases of steroid therapy + TAC, 0 case of steroid therapy + CsA, and 0 case of conservative treatment, accounting for 25.0%, 75.0%, 0.0%, and 0.0%, respectively. There was no statistically significant difference in the proportion of treatment regimens among the three groups (P = 0.052).
In terms of treatment outcomes, there was a statistically significant difference in CR rates among the three groups at weeks 24, 36, and 48 of follow-up (P < 0.05). Further pairwise comparison among the three groups showed that the CR rates of the 2+ group at weeks 24, 36, and 48 were higher than those of the 3+ group and 1+ group (P < 0.001). There was a statistically significant difference in PR rates among the three groups at week 36 of follow-up (P = 0.007); PR rates of the 1+ and 2+ groups at week 36 of follow-up were higher than those of the 3+ group (P < 0.05) while there was no statistically significant difference in PR rates between the 1+ and 2+ groups (P > 0.05).
There was no statistically significant difference in PR rates among the three groups at the same follow-up time points. In summary, we found that among patients with PLA2R-positive kidney tissues, those with lower PLA2R deposition levels had better therapeutic outcomes. (Details are given in Tables 4 and 5).
 |
Table 4 Comparison of Composition Ratios Between Different Deposition Level Groups Among PLA2R Positive Renal Tissue Patients |
 |
Table 5 Comparison of Therapeutic Effects Between Different Deposition Level Groups Among PLA2R Positive Renal Tissue Patients |
Comparison of Composition and Treatment Outcomes of Steroid-Combined TAC Treatment Regimens
To eliminate the interference of different treatment plans on the efficacy, we conducted a subgroup analysis on 18 cases of steroid + TAC with a higher number of cases in the same treatment plan and compared the relationship between different levels of PLA2R deposition in kidney tissues and treatment outcomes. Among IMN patients treated with the steroid + TAC regimen, there were 18 cases with positive kidney PLA2R deposition and 4 cases with negative kidney PLA2R deposition. We found that the CR rates of the PLA2R Negative kidney tissue group were higher than those of the Positive group at weeks 24 and 48 of follow-up (P < 0.05). There was no significant difference in PR rates between the two groups at weeks 12, 24, 36, and 48 (P > 0.05).
We did a further comparative analysis on the therapeutic outcomes of different deposition groups in patients with PLA2R-positive kidney tissues. The PR rates among the three groups were statistically significant (P < 0.05) at weeks 24, 36, and 48 of follow-up. Among them, at week 24 of follow-up, the PR rate of the 1+ group was significantly higher than that of the 2+ group; at week 36 of follow-up, the PR rate of the 1+ group was significantly higher than that of the 2+ and 3+ groups (P < 0.05) while there was no significant difference in the PR rate between the 2+ and 3+ groups (P > 0.05). At week 48 of follow-up, the PR rate of the 3+ group was significantly higher than that of the 2+ and 1+ groups (P < 0.05) while there was no statistically significant difference in the PR rate between the 1+ and 2+ groups (P > 0.05). Overall, patients with low levels of PLA2R deposition in kidney tissues had higher remission rates during the short-term follow-up. (Details are given in Tables 6 and 7).
 |
Table 6 Comparison of Therapeutic Effects Between Renal PLA2R Positive and Negative Groups in Patients on Hormone + TAC Regimen |
 |
Table 7 Comparison of Therapeutic Effects Between Different Deposition Groups of PLA2R in Renal Tissues in Patients on Hormone + TAC Regimen |
Discussion
Membranous nephropathy is a common pathological type in adult nephrotic syndromes, with approximately 3/4 of patients having membranous nephropathy of unclear etiology, known as idiopathic membranous nephropathy (IMN). The discovery of PLA2R autoantibodies was a milestone breakthrough in understanding the complex pathogenesis of IMN. There are varying reports on the relationship between kidney PLA2R and the manifestations and treatment effects of IMN. In this study, we aimed at examining and correlating varied levels of PLA2R deposition in kidney tissues of IMN patients with treatment outcomes. We anticipate that this study can provide a reference basis for the clinical diagnosis and treatment of patients with IMN.
General Data Analysis and discussion
In this study, we included a total of 61 patients with IMN, with an age range of 25–75 years and an average age of 49.66 ± 12.31 years. The overall gender distribution was predominantly male, with a male-to-female ratio of 1.5:1. Idiopathic membranous nephropathy is now thought to affect more middle-aged and elderly people. An epidemiological analysis of 837 kidney biopsies conducted by the Southern Medical University11 revealed that membranous nephropathy was more common in patients aged over 66 years, followed by those aged 41–65 years, and finally those aged 18–40 years. This disease was found to be more common in males, with a male-to-female ratio of approximately 2:1. Our data in this study are roughly consistent with these findings.
Positive rates of PLA2R deposition in kidney tissues of patients with IMN have been reported differently in Chinese and international studies. Our results were similar to those reported by Beck et al,3 who found that the positive rate of PLA2R deposition in kidney tissues was 70%, and Hou et al,12 who reported an 82.3% positive rate of PLA2R deposition in kidney tissues of IMN patients. In this study, there were 14 cases (22.9%) with negative PLA2R deposition in kidney tissues. However, the current understanding of the pathophysiology, prognosis, and therapeutic strategies for PLA2R accumulation in kidney tissues remains sketchy, and there is no unified opinion. Probable reasons for the negative findings are as follows: ① IMNs expressing other pathogenic target antigens other than PLA2R, such as type 1 platelet reactive protein 7A domain (THSD7A), have been found recently to be associated with membranous nephropathy. Thus, there may also be other undiscovered pathogenic target antigens. ② There are secondary factors that may have been overlooked if patients had not yet shown typical clinical manifestations and related clinical indicators. ③ Such patients may have been in the early stages of development of the disease and the expression of the PAL2R antigen in kidney tissues could have been low; hence, they may not have tested positive.
Comparison of Therapeutic Outcomes Between PLA2R and IMN
Treatment regimens for all IMN patients in this study consisted of steroid therapy combined with CTX, steroid therapy combined with TAC, steroid therapy combined with CsA, or only conservative supportive care. The prediction of serum PLA2R antibodies has aided the clinical diagnosis and management of IMN. However, whether the level of PLA2R expression in kidney tissues is related to the efficacy of treatment in IMN is not clearly known.
Some authors13 found no correlation between the expression of PLA2R in kidney tissues and 24-hour urine protein, but reported that a higher deposition of PLA2R was related to a higher complete remission rate. In an efficacy observation study on 122 patients with IMN, Liu et al14 found that after six months of immunosuppressive therapy combined with steroid treatment, the urinary protein remission rates in the PLA2R Positive and PLA2R Negative kidney tissue groups were 83.9% and 54.5%, respectively. Results from a single-center retrospective study15 showed that patients with PLA2R-associated IMN treated with steroid or immunosuppressive therapy had lower urinary protein response rates compared to those with non-PLA2R-associated IMN.
In this study, 61 patients with IMN were treated with steroid and immunosuppressive agents, with some patients receiving only conservative supportive treatment. The composition ratio of treatment plans did not significantly differ among the groups. After 48 weeks of follow-up, the results showed that the complete response rate, partial response rate, and effective rate of patients in the PLA2R Negative kidney tissue group were higher than those of the PLA2R Positive group at weeks 36 and 48. The PLA2R Negative kidney tissue group had a high partial response rate at week 12 of follow-up (P = 0.004). This finding is similar to some of the earlier reports mentioned above.
We conducted a further comparative analysis of the intensity of PLA2R deposition and treatment efficacy in IMN patients with PLA2R-positive kidney tissues. We found that the partial response rate of the 1+ and 2+ groups was higher than that of the 3+ group at week 36 of follow-up (P < 0.05), and the complete response rate of the 2+ group was higher than that of the 3+ group at weeks 24, 36, and 48 of follow-up (P < 0.05). This suggests that patients with PLA2R-negative kidney tissues or low PLA2R deposition in kidney tissues showed better treatment outcomes in the short term.
We performed a subgroup analysis on IMN patients who received steroid therapy combined with TAC to account for the influence of different treatment regimens on treatment outcomes. The results showed that at weeks 24 and 48 of follow-up, the complete response rate of the PLA2R Negative kidney tissue group was higher than that of the PLA2R Positive group (P < 0.05). Therefore, patients with negative PLA2R deposition in kidney tissues and lower deposition levels had better remission rates in treatment.
In clinical practice, predicting and assessing the efficacy of treatment for IMN patients is possible through the detection of PLA2R expression in kidney tissues. However, in the results of this study, among the different deposition groups of PLA2R-positive patients on steroid therapy combined with TAC, the PR rate of the 3+ group was significantly higher than that of the 2+ and 1+ groups at week 48 of follow-up (P < 0.05). This is different from other results of this study, and we speculate that the statistical results are not representative due to the small sample size.
Some of the results of this study are consistent with certain prior research, but they also differ in key respects. Our analysis of the reasons for this is as follows: ① Patients who test negative for PLA2R in kidney tissues tend to be at an earlier pathological stage, which is associated with a better response to therapy; ② In this analysis, treatment outcomes in patients may be affected by the variety of treatment strategies employed. The findings of this study may not be entirely representative because of its small sample size and the equally smaller number of individuals who tested negative for PLA2R in kidney tissues.
Limitations and Shortcomings
- The sample size included in this study is small and lacks conclusiveness.
- The proportion of PLA2R-negative patients in kidney tissues in this study was relatively low, and there may be some additional antigenic IMN patients, such as those with THSD7A antigen expression or unknown secondary causes.
- We were unable to include the detection of serum PLA2R antibody levels for further analysis in this study due to the limited number of IMN cases that underwent both kidney tissue PLA2R testing and serum PLA2R antibody testing at our center and could be followed up regularly as outpatients.
- The follow-up duration of this study was relatively short. Some patients may develop recurrences after treatment remission. Hence, an extended follow-up can offer a more accurate understanding of treatment outcomes in IMN patients.
Conclusion
We found that the overall effective rate of treatment in patients with PLA2R-negative kidney tissues was higher than that in patients with PLA2R-positive kidney tissues. There was a correlation between the levels of PLA2R deposition in kidney tissues and treatment outcomes in IMN, with better efficacy in patients with lower levels of PLA2R deposition.
Ethics approval and consent to participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Jinjiang Municipal Hospital and the 2nd Affiliated Hospital of Fujian Medical University. A written informed consent was obtained from all participants.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Couser WG. Primary membranous nephropathy. Clin J Am Soc Nephrol. 2017;12(6):983–997. doi:10.2215/CJN.11761116
2. Ronco P, Beck L, Debiec H, et al.. Membranous nephropathy. Nat Rev Dis Primers. 2021;7(1):69.
3. Beck LH
4. Safar-Boueri L, Piya A, Beck LH
5. Burbelo PD, Joshi M, Chaturvedi A, et al.. Detection of PLA2R autoantibodies before the diagnosis of membranous nephropathy. J Am Soc Nephrol. 2020;31(1):208–217. doi:10.1681/ASN.2019050538
6. Stefan G, Stancu S, Zugravu A, et al.. Negative anti-phospholipase A2 receptor antibody status at three months predicts remission in primary membranous nephropathy. Ren Fail. 2022;44(1):258–268. doi:10.1080/0886022X.2022.2033265
7. Xu NX, Xie QH, Sun ZX, et al.. renal phospholipase A2 receptor and the clinical features of idiopathic membranous nephropathy. Chin Med J. 2017;130(8):892–898. doi:10.4103/0366-6999.204096
8. Zhang QH, Wu M, Hu ZG, et al.. Serum antibody and glomerular antigen of antiphospholipase A2 receptor in Chinese patients with idiopathic membranous nephropathy. Biomed Res Int. 2020;2020:1693710. doi:10.1155/2020/1693710
9. Xie Z, Dong W, Li Z, et al.. Clinical value of renal phospholipase A2 receptor deposit in the prognosis evaluation and treatment options of idiopathic membranous nephropathy: a retrospective cohort study. Nephrology . 2020;25(3):219–229. doi:10.1111/nep.13691
10. Rovin BH, Adler SG, Barratt J, et al. Executive summary of the KDIGO 2021 guideline for the management of glomerular diseases. Kidney Int. 2021;100(4):753–779. doi:10.1016/j.kint.2021.05.015
11. Li JN. Diagnosis of Idiopathic Membranous Nephropathy in Patients with Serum Anti-M Type phospholipase A2 Receptor (PLA2R) Antibody Negative . Peking Union Medical College; 2015.
12. Hou X, Xu M, Liu YY. Diagnostic value of serum PLA2R antibody and renal PLA2R detection in idiopathic membranous nephropathy. J Pract Med. 2020;37(10):901–902.
13. Cui J, Li WN, Lou JQ, Qi D, Zhang Y. Expression of M-type phospholipase A2 receptor and Nephrin in renal tissue of patients with idiopathic membranous nephropathy and its influence on prognosis. J Clin Exp Pathol. 2015;31(03):333–335.
14. Liu H, Luo W, Gong S, Ding X. Detection and clinical significance of glomerular M-type phospholipase A2 receptor in patients with idiopathic membranous nephropathy. Intern Med J. 2016;46(11):1318–1322. doi:10.1111/imj.13233
15. Zhang D, Zou J, Zhang C, Zhang W, Lin F, Jiang G. Clinical and histological features of phospholipase A2 receptor-associated and thrombospondin Type-I domain-containing 7A-associated idiopathic membranous nephropathy: a Single Center Retrospective Study from China. Med Sci Monit. 2018;24:5076–5083. doi:10.12659/MSM.909815
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
