Back to Journals » Journal of Inflammation Research » Volume 16
Association of Inflammatory Indicators and Clinical Signs and Itch in Atopic Dermatitis Patients Treated with Simiao Pill Combined with Halomethasone Cream
Received 19 June 2023
Accepted for publication 2 August 2023
Published 23 August 2023 Volume 2023:16 Pages 3643—3653
DOI https://doi.org/10.2147/JIR.S423131
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Jun Cao,1 Hui Liu,1 Xiaojie Ding2
1Department of Dermatology, Wuxi 9th Affiliated Hospital of Soochow University, Wuxi, People’s Republic of China; 2Department of Dermatology, The Second Affiliated Hospital of Nanjing University of Chinese Medicine, Jiangsu Second Chinese Medicine Hospital, Nanjing, People’s Republic of China
Correspondence: Xiaojie Ding, Department of Dermatology, The Second Affiliated Hospital of Nanjing University of Chinese Medicine, No. 336, Shuiximen street, Jianye District, Nanjing, 210000, People’s Republic of China, Email [email protected]
Background: Atopic dermatitis (AD) is a chronic inflammatory skin disease characterized by symptoms such as itchiness, scaling, and erythema. Previous studies have suggested that inflammatory indicators obtained from peripheral blood cell count can serve as markers for atopic dermatitis pruritus and severity. The objective of this study was to investigate whether these indicators are associated with treatment efficacy in AD patients who received a combination of halomethasone cream and Simiao pill (SMP).
Methods: 131 adult patients diagnosed with AD between January 2020 to August 2022 and treated with topical halometasone ointment combined with oral Simiao pill for a month were recruited and clinical dates of patients were collected. Inflammatory indicators included Eosinophil-to-lymphocyte ratio (ELR), neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR), platelet-to-lymphocyte ratio (PLR), serum leukotriene B4 (LTB4), and thymic stromal lymphopoietin (TSLP) and clinical indexes for assessing eczema area and severity index (EASI) and peak pruritus-numerical rating scale (PP-NRS). Relationship of baseline and changes of these Inflammatory indicators and that of clinical indexes were analyzed.
Results: ELR, NLR, LTB4, and TSLP levels have positive association with EASI before treatment, and baseline ELR and LTB4 levels have positive relationship with PP-NRS. ELR, NLR, LTB4, and TSLP showed a significant decrease at week 2 and the low levels were maintained until week 8 after treatment, while no significant changes were observed in levels of MLR and PLR. There was a significant correlation between the decrease of ELR and the decreases of EASI and PP-NRS at weeks 2, 4 and 8 of the treatment.
Conclusion: ELR may serve as an effective and convenient indicator in assessing the disease severity and efficacy of SMP therapy for AD.
Keywords: clinical efficacy, atopic dermatitis, halometasone cream, inflammatory indicators, Simiao pill
Introduction
Atopic dermatitis (AD) is a chronic and recurrent inflammatory disease, manifesting as persistent skin itching.1,2 Topical corticosteroid is still a preferred treatment for inflammatory AD onset. The Simiao pill (SMP) is a well-known prescription medication that exhibits anti-inflammatory, analgesic, and immunomodulatory properties. Simiao pill is composed of traditional Chinese medicines, including Rhizoma Smilacis Glabrae, Cortex Phellodendri, Radix Salviae Miltiorrhizae, Cortex Eucommiae, Radix Achyranthis Bidentatae, and Radix Glycyrrhizae. The therapeutic mechanism of SMP is based on its effective anti-inflammatory and antioxidant effects. It can inhibit the secretion of inflammatory factors, including tumor necrosis factor, rheumatoid factor, and prostaglandins, while also upregulating the expression of cellular antioxidant regulators.3 AD is characterized by abnormal “damp heat” based on the traditional Chinese medicine theory and SMP has therapeutic effects of alleviating this kind of “heat”. Clinically, it is utilized for the treatment of inflammatory ailments like rheumatoid arthritis and gouty arthritis.3 Our previous study demonstrated that administration of halomethasone cream combined with SMP for 4 weeks had a better therapeutic efficacy with good tolerance, when compared with halomethasone cream alone in AD patients.4 Major side effects observed were pain in limbs and digestive system symptoms including mild nausea. All of these side effects were gone after 2 weeks of withdrawal.
Recently, the role of systemic inflammatory markers, including neutrophil/lymphocyte ratio (NLR), monocyte/lymphocyte ratio (MLR), and platelet/lymphocyte ratio (PLR), has been investigated in various diseases like cancers, cardiovascular disease, and immune and autoinflammatory diseases.5–7 NLR was observed to have close association with AD severity and reflects therapy efficacy in psoriasis patients.8,9 A previous study found that tissue eosinophilia existed in both acute and chronic atopic dermatitis lesions and peripheral eosinophil (EOS) levels were parallel with disease severity.10 EOS relative count was observed to serve as an independent indicator for evaluating severity of atopic dermatitis.11 The relationship between EOS-to-lymphocyte ratio (ELR) and autoimmune skin diseases was also investigated recently. The study of Hagino et al demonstrated that ELR was significantly associated with clinical signs and itch in atopic dermatitis patients treated with upadacitinib.12 Leukotriene B4 (LTB4), an inflammatory chemokine, is capable of mediating interleukin and promoting the development of AD while inducing hypersensitivity by binding with neutrophils.13 Additionally, it enhances the infiltration of inflammatory cells such as lymphocytes into the affected area of the epidermis. By regulating the expression of T and B cells in various microcirculation environments, thymic stromal lymphopoietin (TSLP) can moderate the involvement of T helper 2 cells in allergic reactions and exacerbate chronic AD.14 Our previous study revealed the significant relationship between concentrations of serum LTB4 and TSLP and therapeutic effects in AD patients.4 Nevertheless, the precise assessment of the transition of these two parameters during treatment for AD was not conducted.
This study aimed to investigate the potential of inflammatory indicators such as ELR, NLR, MLR, PLR, LTB4, and TSLP in predicting the improvement of clinical symptoms in moderate-to-severe AD patients treated with SMP. The researchers hypothesized that changes in these indicators could serve as markers for the effectiveness of SMP treatment, which was evaluated using the Eczema Area and Severity Index (EASI) and the Peak Pruritus-Numerical Rating Scale (PP-NRS).
Materials and Methods
Study Design
A total of 131 patients with chronic AD treated with topical halometasone ointment (Aomei, China, approval number: hc20150050, batch number: 6201722), twice a day at 12 h intervals, combined with twice daily oral Simiao pill (Jilin Zixin Pharmaceutical Co., Ltd., China, approval No. gyzzz22024960, batch No. 201101), 6 g each time for a month, between January 2020 to August 2022 in Wuxi 9th Affiliated Hospital of Soochow University were recruited and retrospectively analyzed. This study is a secondary data analysis. The inclusion criteria were as follows: (I) The AD was diagnosed based on the Guide of AD Media;15 (II) patients with clinical manifestations of the disorder; (III) no hormones, immunosuppressants, and other drugs were taken 1 month before treatment. The exclusion criteria were as follows: (I) patients did not complete the whole treatment as established protocol; (II) patients with liver, kidney, heart, and other important organ failure; (III) patients with other skin diseases; (IV) patients with incomplete case data. All participants provided informed consent. The Ethics Committee of Wuxi 9th Affiliated Hospital of Soochow University approved the study (2020131), and it was conducted in compliance with the Declaration of Helsinki (2004).
The inflammatory indicators were calculated and measured at weeks 0, 2, 4 during treatment and at week 8 post-treatment. AD severity was evaluated using EASI.16 Details of scoring method of EASI can be found in our previous study. PP-NRS is a self-reported tool for evaluating the maximum pruritus experienced by patients within the last 24 hours using a scale of 0 to 10, with 0 indicating the absence of perceived itch and 10 representing the most severe itch imaginable.17
LTB4 and TSLP Detection
Prior to and after treatment at 2, 4, and 8 weeks, a volume of 2 mL of fasting elbow vein peripheral blood was collected and treated with EDTA-K2 anticoagulant (De sheng, China). The sample was then centrifuged using Hettich’s mikro 220/220r centrifuge (parameters: 3000 rpm, time =10 min, inner diameter =10 cm) to obtain the supernatant. The serum was used to determine the concentrations of LTB4 and TSLP through the use of BioTek Synergy H1 automatic enzyme labeling instrument and enzyme-linked immunosorbent assay kits, obtained from Beijing Baiolabo Technology Co., Ltd. (China). All procedures were conducted in compliance with the manufacturer’s instructions.
Statistical Analysis
Data analysis was performed using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). Normally distributed measurement data were presented as mean ± standard deviation and assessed using Student’s t-test, while count data were expressed as n (%). Friedman test was employed to assess differences of non-parametrically distributed variables. Bonferroni correction was applied to correct P-values. Correlations between variables were evaluated using Spearman correlation coefficient. A statistically significant difference was considered for a P-value < 0.05. A linear multivariate regression analysis was conducted to determine independent predictive factors. Variables with a p-value < 0.05 in univariate analyses were included in the analysis and adjusted for age.
Results
Patient Characteristics
Table 1 presents the baseline characteristics of the enrolled patients. A total of 131 patients diagnosed with AD participated in the study, consisting of 78 male and 53 female patients. The mean age at diagnosis for all cases was 45.2 years, ranging from 17 to 78 years.
 |
Table 1 Baseline Characteristics of Patients with Atopic Dermatitis |
Associations Between Baseline Inflammatory Indicators and EASI or PP-NRS
Initial (week 0) values of ELR, NLR, LTB4, and TSLP were positively associated with initial EASI, as shown in Table 2. Additionally, the initial levels of ELR and LTB4 exhibited a positive correlation with baseline PP-NRS.
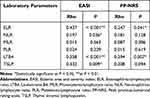 |
Table 2 Correlation Between Baseline Values of Laboratory Parameters versus Those of Clinical Indexes in Patients with Atopic Dermatitis (n = 131) |
Changes of Inflammatory Indicators After SMP Treatment
As shown in Figure 1A and B, EASI and PP-NRS exhibited significant reductions at week 2, which were sustained until weeks 4 and 8. Similarly, the levels of ELR, NLR, LTB4, and TSLP showed a significant reduction at week 2 compared to baseline, after which the decreased values were sustained up to week 8 (Figure 1C, D, G and H). While PLR reduction was observed at week 2 (Figure 1E), and then reverted to normal levels, signifying transient changes. MLR did not exhibit any alterations (Figure 1F).
Association Between Decrease of Inflammatory Indicators and EASI or PP-NRS
Relationship between decrease of inflammatory indicators and EASI or PP-NRS was demonstrated in Table 3. The decrease of ELR was significantly associated with change trends of EASI and PP-NRS within 8 weeks. The decrease of EASI was related to change trend of LTB4 and TSLP during treatment. The decrease of EASI was associated with reduction of NLR and PLR at week 4. The decrease of PP-NRS was related to reduction of LTB4 and TSLP at week 2.
 |
Table 3 Correlations Between Percent Reductions of Laboratory Parameters versus Those of Clinical Indexes at Weeks 2, 4, or 8 of Patients with Atopic Dermatitis (n = 131) |
Association of Baseline Factors with Improvement of EASI After SMP Treatment
Table 4 presented the association between baseline characteristics, including gender, age, BMI, disease duration, and inflammatory markers, with EASI improvement resulting from SMP treatment at weeks 2, 4, or 8. The findings revealed that age and LTB4 demonstrated positive correlations with the decrease of EASI at weeks 2 and 4, while ELR and TSLP were positively associated with the decrease of EASI at week 2. However, baseline EASI, PP-NRS, NLR, MLR, PLR, gender, BMI, and disease duration had no relationship with decrease of EASI. Multivariate analysis indicated that age had an association with decrease of EASI at weeks 2 and 4 (Table 5). Additionally, LTB4 was linked to the decrease of EASI at week 2, while no association was observed between that of EASI with ELR or TSLP. These results suggest that older patients are more likely to experience significant improvements in clinical signs during weeks 2 and 4 of SMP treatment. Similarly, elevated baseline levels of LTB4 may be a predictor of significant improvement in disease severity at week 2.
 |
Table 4 The Relationships of Clinical Characteristics with Decrease of EASI at Weeks 2, 4, or 8 of Patients with Atopic Dermatitis (n = 131) |
Association of Baseline Factors with Improvement of PP-NRS After SMP Treatment
Table 6 presented the association between baseline characteristics, including gender, age, BMI, disease duration, and inflammatory markers, with PP-NRS improvement resulting from SMP treatment at weeks 2, 4, or 8. The findings revealed that age and TSLP demonstrated positive correlations with the decrease of EASI at week 2, while LTB4 and PP-NRS were positively associated with the decrease of EASI at weeks 2 and 4. However, baseline EASI, ELR, NLR, MLR, PLR, gender, BMI, and disease duration had no relationship with the decrease of PP-NRS. Multivariate analysis indicated that age and baseline PP-NRS had no association with the decrease of PP-NRS at weeks 2 and 4. Additionally, LTB4 was linked to the decrease of PP-NRS at week 2, while no association was observed between that of PP-NRS with TSLP (Table 7). These results suggest that older or high baseline PP-NRS patients are more likely to experience significant improvements in clinical signs during weeks 2 and 4 of SMP treatment. Similarly, elevated baseline levels of LTB4 may be a predictor of significant improvement in disease severity at week 2.
 |
Table 6 The Relationships of Clinical Characteristics with Decrease of PP-NRS at Weeks 2, 4, or 8 of Patients with Atopic Dermatitis (n = 131) |
 |
Table 7 The Predictive Factors for Decrease of PP-NRS at Weeks 2, 4, or 8 of Treatment Assessed by Linear Multivariate Regression Analysis in Patients with Atopic Dermatitis (n = 131) |
Discussion
In recent decades, there has been a consistent increase in the prevalence of AD, observed not only in highly urbanized and economically developed nations but also in developing countries.1 Approximately 20% of the global population suffers from this chronic condition, particularly among children. AD takes a significant toll on mental health, work productivity, and overall quality of life of both patients and their caregivers. Topical corticosteroids remain the preferred treatment for the onset of inflammatory AD. However, nearly all of these patients experience a relapse if they discontinue topical anti-inflammatory medications. Application of systemic immunosuppressants is always accompanied by some intolerable side effects. Novel treatment for AD is warranted. Our previous study confirmed that combination of SMP and halomethasone cream in AD treatment could have favorable therapeutic efficacy with tolerable side effects.4
In this study, we explored the relationship between inflammatory indicators and EASI or PP-NRS. Dynamic changes of these indicators were also assessed during treatment. This study found significant associations between baseline ELR, NLR, LTB4, and TSLP with baseline EASI, and baseline ELR and LTB4 with baseline PP-NRS. The decrease of ELR was positively associated with those of EASI or PP-NRS at weeks 2, 4, or 8 in AD patients treated with SMP. Similar significant correlations were also observed in LTB4 and TSLP at weeks 2, 4, and NLR only at week 2. Furthermore, multivariate analyses showed that age was related to the decrease of EASI and PP-NRS during the whole follow-up, while baseline LTB4 was associated with the decrease of EASI and PP-NRS after 2 weeks treatment. Initial PP-NRS was also associated with the decrease of PP-NRS after 2 or 4 weeks treatment. Our study demonstrated that level of ELR was significantly correlated with the changes of severity of AD symptoms at pre-treatment, midpoint, and post-treatment assessment sessions. Therefore, ELR may serve as an effective indicator for evaluation of therapeutic efficacy in AD treatment with SMP.
EOS infiltration is a common observation in various skin diseases, despite their absence in normal physiological conditions. In most cases, the presence of EOSs in the skin is reactive and mediated by cytokines. However, clonal expansion of EOSs due to intrinsic mutations can also occur. EOSs play a significant role in several biological processes, including host defense, regulation of immune response, generation of itchiness, tissue remodeling, induction of fibrosis, and tissue damage. This involvement contributes to the pathogenesis of various diseases, including atopic dermatitis (AD). In AD, EOSs secrete granules that can harm keratinocytes and stimulate the release of IL-33, which further activates basophils, mast cells, and EOSs.18 Additionally, EOS-derived granules can induce mast cell degranulation, leading to the secretion of histamine and cytokines.19,20 Furthermore, EOSs express type 2 cytokines, reaffirming their active contribution to AD inflammation. Moreover, EOSs can initiate pruritus by releasing toxic granule proteins, neuromediators, and cytokines such as IL-31.21 EOSs produce higher levels of IL-31, which further triggers chemotaxis and IL-31 production in EOSs themselves. It is evident that EOSs have multifaceted roles in the pathogenesis of AD, not only defending against pathogens using toxic granule proteins but also promoting inflammation, contributing to fibrosis, and initiating itch.22 SMP is a traditional Chinese medicinal formula that has demonstrated anti-inflammatory, analgesic, and immunomodulatory effects. It is commonly used in clinical practice to treat various inflammatory diseases, including rheumatoid arthritis and gouty arthritis.3 Our previous study showed favorable outcomes in AD treatment with SMP combined with topical halometasone ointment.4 The potential molecular and cellular mechanisms of SMP in suppressing itch are poorly defined. Previous studies indicated that increased levels of circulating EOS were parallel with degree of clinical symptoms in AD.10,23 ELR and NLR were observed to decrease and maintain a lower level during the treatment, while MLR and PLR showed a transient fall or no changes when SMP was administered for AD in this study. Additionally, decrease of ELR was associated with that of EASI and PP-NRS. Results of this study revealed that EOSs rather than neutrophils, monocytes, or platelets may participate in SMP-induced improvement of clinical signs. The study of Hagino et al also exhibited a similar result. In their study, ELR served as a marker for the improvement of disease symptoms in atopic dermatitis treated with upadacitinib, a JAK1 inhibitor, and dynamic changes of ELR correlated with symptom indicators.12
LTB4, a conventional lipid chemoattractant, has been traditionally identified to stimulate EOSs, differentiated T cells, and dendritic cells’ chemotaxis.24 A prior investigation has proposed the crucial involvement of LTB4 in the pathogenesis of AD. LTB4 is known to initiate the infiltration of neutrophils, EOSs, and Th2 cells into the skin, thereby contributing to the inflammatory response in AD.13 Indeed, several studies have observed increased levels of LTB4 in the skin lesions of AD or allergic contact patients.25–27 Our previous study also found that level of serum LTB4 significantly decreased and paralleled with improvement of clinical symptoms and itch after SMP treatment in AD patients.4 This study further revealed a significant consistent association trend between decrease of serum LTB4 level and those of EASI or PP-NRS at weeks 2 and 4. Therefore, SMP may provide new strategies for the pharmacological intervention for the amelioration of AD by targeting LTB4. TSLP is a multifaceted member of the interleukin-2 family and a distant paralog of interleukin-7. TSLP, highly expressed by keratinocytes, could contribute to an acute episode of AD by stimulating EOS extracellular traps formation.28,29 Previous studies have indicated that TSLP may indirectly contribute to pruritus through the induction of Th2-related cytokines activating sensory neurons. TSLP can also elicit pruritus signals directly by activating transient receptor potential cation channel A1 through its interaction with TSLPR-expressing dorsal root ganglia neurons.30–32 The results indicate a significant correlation between the epidermal synthesis of TSLP and AD’s clinical manifestations, including the presence of lesions, severity, and longevity, which is consistent with the results of our study. Targeting TSLP and its downstream signaling pathways may provide a promising treatment approach for AD. Further research is necessary to elucidate the underlying mechanisms of SMP in TSLP.
Additionally, our study also found that age was significantly associated with decrease of EASI and PP-NRS at weeks 2 and 4. Patients with old age may obtain more benefit from SMP in AD. Elderly individuals exhibit variations in their immune system, commonly known as “immunosenescence”, which contributes to the heightened susceptibility to infectious diseases and autoimmune disorders.33 The morphological and functional changes that occur in the skin of elderly individuals result in a distinctive pattern of skin diseases as compared to young people, both in terms of frequency and clinical appearance. For instance, cutaneous xerosis, which is associated with diminished activity of sweat and sebaceous glands, is prevalent in most older adults and frequently causes senile pruritus or AD.34 The aging process in adult patients with AD is associated with decreased levels of cytokines such as IL-31 or IL-13, which are responsible for generating itch, within the skin lesions.35,36 This study indicated that a better efficacy could be achieved in older patient population. What is more, a high percentage reduction of PP-NRS was related to patients presenting with a high initial PP-NRS, which is consistent with those reported in two previous studies.12,37
Our study firstly explored the associations between dynamic changes of inflammatory indicators with treatment efficacy in AD patients who received halomethasone cream combined with SMP. Additionally, inflammatory indicators in this study included ratios of different leukocytes and biomarkers of inflammation in blood. While several limitations also exist in our study. First, confounding and selection bias could not be avoided in this retrospective study. Second, the limited sample sizes, and association analysis was not conducted in control group treated with topical corticosteroids only. Third, this study did not record and analyze relapse or recurrence following treatment. Fourth, a shorter follow-up. Finally, this study evaluated the efficacy of only 6 g, twice daily, of SMP for a month. Whether an increasing dose and longer period of treatment would affect the efficacy need further investigation.
Conclusion
Baseline ELR had a significant association with EASI and PP-NRS before SMP treatment, and change trend of ELR during and after therapy was still significantly correlated with clinical signs and itch in AD patients. ELR could be used to evaluate the therapeutic efficacy for quantitation and avoid subject bias during SMP treatment in AD. Blood test is routine in clinical practice, which means that obtaining ELR is convenient. ELR may serve as an accurate, timely and convenient indicator in assessing the disease severity and efficacy of SMP therapy for AD, helping to create an individualized treatment strategy. Larger-scale study is warranted to validate our finding.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethical Approval
The study was approved by the Ethics Committee of Wuxi 9th Affiliated Hospital of Soochow University (2020131) and was conducted in accordance with the Declaration of Helsinki. All participants provided informed consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Subject of Wuxi 9th Affiliated Hospital of Soochow University (Grant No. JY2021-07-15).
Disclosure
The authors have declared no competing interests in this work.
References
1. Patruno C, Potestio L, Napolitano M. Clinical phenotypes of adult atopic dermatitis and related therapies. Curr Opin Allergy Clin Immunol. 2022;22(4):242–249. doi:10.1097/ACI.0000000000000837
2. Sroka-Tomaszewska J, Trzeciak M. Molecular mechanisms of atopic dermatitis pathogenesis. Int J Mol Sci. 2021;22(8):4130. doi:10.3390/ijms22084130
3. Wang Y, Zhang F, Li X, et al. Integrated multi-omics techniques and network pharmacology analysis to explore the material basis and mechanism of Simiao pill in the treatment of rheumatoid arthritis. ACS Omega. 2023;8(12):11138–11150. doi:10.1021/acsomega.2c07959
4. Cao J, Liu H, Ding XJ. Effect of halometasone cream combined with Simiao pill on the therapeutic effect and expression of serum leukotriene B4 (LTB4) and thymic stromal lymphopoietin (TSLP) in patients with eczema, and the factors influencing its clinical efficacy. Ann Palliat Med. 2021;10(11):11643–11652. doi:10.21037/apm-21-2685
5. Tian BW, Yang YF, Yang CC, et al. Systemic immune-inflammation index predicts prognosis of cancer immunotherapy: systemic review and meta-analysis. Immunotherapy. 2022;14(18):1481–1496. doi:10.2217/imt-2022-0133
6. Stark K, Massberg S. Interplay between inflammation and thrombosis in cardiovascular pathology. Nat Rev Cardiol. 2021;18(9):666–682. doi:10.1038/s41569-021-00552-1
7. Krainer J, Siebenhandl S, Weinhäusel A. Systemic autoinflammatory diseases. J Autoimmun. 2020;109:102421. doi:10.1016/j.jaut.2020.102421
8. Annen S, Horiguchi G, Teramukai S, et al. Association of transition of laboratory markers with transition of disease activity in psoriasis patients treated with biologics. J Nippon Med Sch. 2022;89(6):587–593. doi:10.1272/jnms.JNMS.2022_89-613
9. Hagino T, Saeki H, Kanda N. Biomarkers and predictive factors for treatment response to tumor necrosis factor-α inhibitors in patients with psoriasis. J Clin Med. 2023;12(3):974. doi:10.3390/jcm12030974
10. Kiehl P, Falkenberg K, Vogelbruch M, Kapp A. Tissue eosinophilia in acute and chronic atopic dermatitis: a morphometric approach using quantitative image analysis of immunostaining. Br J Dermatol. 2001;145(5):720–729. doi:10.1046/j.1365-2133.2001.04456.x
11. Inokuchi-Sakata S, Ishiuji Y, Katsuta M, et al. Role of eosinophil relative count and neutrophil-to-lymphocyte ratio in the assessment of severity of atopic dermatitis. Acta Derm Venereol. 2021;101(7):adv00491. doi:10.2340/00015555-3838
12. Hagino T, Saeki H, Fujimoto E, Kanda N. The eosinophil-to-lymphocyte ratio acts as an indicator for improvement of clinical signs and itch by upadacitinib treatment in atopic dermatitis. J Clin Med. 2023;12(6):2201. doi:10.3390/jcm12062201
13. Liu M, Yokomizo T. The role of leukotrienes in allergic diseases. Allergol Int. 2015;64(1):17–26. doi:10.1016/j.alit.2014.09.001
14. Nitta T, Suzuki H. Thymic stromal cell subsets for T cell development. Cell Mol Life Sci. 2016;73(5):1021–1037. doi:10.1007/s00018-015-2107-8
15. Katoh N, Ohya Y, Ikeda M, et al. Japanese guidelines for atopic dermatitis 2020. Allergol Int. 2020;69(3):356–369. doi:10.1016/j.alit.2020.02.006
16. Chopra R, Vakharia PP, Sacotte R, et al. Severity strata for Eczema Area and Severity Index (EASI), modified EASI, Scoring Atopic Dermatitis (SCORAD), objective SCORAD, Atopic Dermatitis Severity Index and body surface area in adolescents and adults with atopic dermatitis. Br J Dermatol. 2017;177(5):1316–1321. doi:10.1111/bjd.15641
17. Yosipovitch G, Reaney M, Mastey V, et al. Peak Pruritus Numerical Rating Scale: psychometric validation and responder definition for assessing itch in moderate-to-severe atopic dermatitis. Br J Dermatol. 2019;181(4):761–769. doi:10.1111/bjd.17744
18. Elovic A, Wong DT, Weller PF, Matossian K, Galli SJ. Expression of transforming growth factors-alpha and beta 1 messenger RNA and product by eosinophils in nasal polyps. J Allergy Clin Immunol. 1994;93(5):864–869. doi:10.1016/0091-6749(94)90379-4
19. Kühn H, Kolkhir P, Babina M, et al. Mas-related G protein-coupled receptor X2 and its activators in dermatologic allergies. J Allergy Clin Immunol. 2021;147(2):456–469. doi:10.1016/j.jaci.2020.08.027
20. Hu Y, Liu S, Liu P, Mu Z, Zhang J. Clinical relevance of eosinophils, basophils, serum total IgE level, allergen-specific IgE, and clinical features in atopic dermatitis. J Clin Lab Anal. 2020;34(6):e23214. doi:10.1002/jcla.23214
21. Nakashima C, Ishida Y, Kitoh A, Otsuka A, Kabashima K. Interaction of peripheral nerves and mast cells, eosinophils, and basophils in the development of pruritus. Exp Dermatol. 2019;28(12):1405–1411. doi:10.1111/exd.14014
22. Kunsleben N, Rüdrich U, Gehring M, Novak N, Kapp A, Raap U. IL-31 induces chemotaxis, calcium mobilization, release of reactive oxygen species, and CCL26 in eosinophils, which are capable to release IL-31. J Invest Dermatol. 2015;135(7):1908–1911. doi:10.1038/jid.2015.106
23. Walker C, Kägi MK, Ingold P, et al. Atopic dermatitis: correlation of peripheral blood T cell activation, eosinophilia and serum factors with clinical severity. Clin Exp Allergy. 1993;23(2):145–153. doi:10.1111/j.1365-2222.1993.tb00310.x
24. Nakamura M, Shimizu T. Recent advances in function and structure of two leukotriene B4 receptors: BLT1 and BLT2. Biochem Pharmacol. 2022;203:115178. doi:10.1016/j.bcp.2022.115178
25. Fogh K, Herlin T, Kragballe K. Eicosanoids in skin of patients with atopic dermatitis: prostaglandin E2 and leukotriene B4 are present in biologically active concentrations. J Allergy Clin Immunol. 1989;83(2 Pt 1):450–455. doi:10.1016/0091-6749(89)90132-2
26. Reilly DM, Parslew R, Sharpe GR, Powell S, Green MR. Inflammatory mediators in normal, sensitive and diseased skin types. Acta Derm Venereol. 2000;80(3):171–174. doi:10.1080/000155500750042907
27. Ruzicka T, Simmet T, Peskar BA, Ring J. Skin levels of arachidonic acid-derived inflammatory mediators and histamine in atopic dermatitis and psoriasis. J Invest Dermatol. 1986;86(2):105–108. doi:10.1111/1523-1747.ep12284061
28. Simon D, Hoesli S, Roth N, Staedler S, Yousefi S, Simon HU. Eosinophil extracellular DNA traps in skin diseases. J Allergy Clin Immunol. 2011;127(1):194–199. doi:10.1016/j.jaci.2010.11.002
29. Morshed M, Yousefi S, Stöckle C, Simon HU, Simon D. Thymic stromal lymphopoietin stimulates the formation of eosinophil extracellular traps. Allergy. 2012;67(9):1127–1137. doi:10.1111/j.1398-9995.2012.02868.x
30. Wang SH, Zuo YG. Thymic stromal lymphopoietin in cutaneous immune-mediated diseases. Front Immunol. 2021;12:698522. doi:10.3389/fimmu.2021.698522
31. Oetjen LK, Mack MR, Feng J, et al. Sensory neurons co-opt classical immune signaling pathways to mediate chronic itch. Cell. 2017;171(1):217–228.e13. doi:10.1016/j.cell.2017.08.006
32. Wilson SR, Thé L, Batia LM, et al. The epithelial cell-derived atopic dermatitis cytokine TSLP activates neurons to induce itch. Cell. 2013;155(2):285–295. doi:10.1016/j.cell.2013.08.057
33. Tétart F, Joly P. Eczema in elderly people. Eur J Dermatol. 2020;30(6):663–667. doi:10.1684/ejd.2020.3915
34. Kimura N, Nakagami G, Takehara K, et al. Prevalence of asteatosis and asteatotic eczema among elderly residents in facilities covered by long-term care insurance. J Dermatol. 2013;40(9):770–771. doi:10.1111/1346-8138.12217
35. Nomura T, Kabashima K. Advances in atopic dermatitis in 2019–2020: endotypes from skin barrier, ethnicity, properties of antigen, cytokine profiles, microbiome, and engagement of immune cells. J Allergy Clin Immunol. 2021;148(6):1451–1462. doi:10.1016/j.jaci.2021.10.022
36. Zhou L, Leonard A, Pavel AB, et al. Age-specific changes in the molecular phenotype of patients with moderate-to-severe atopic dermatitis. J Allergy Clin Immunol. 2019;144(1):144–156. doi:10.1016/j.jaci.2019.01.015
37. Norlin JM, Nilsson K, Persson U, Schmitt-Egenolf M. Complete skin clearance and Psoriasis Area and Severity Index response rates in clinical practice: predictors, health-related quality of life improvements and implications for treatment goals. Br J Dermatol. 2020;182(4):965–973. doi:10.1111/bjd.18361
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


