Back to Journals » Nature and Science of Sleep » Volume 14
Association of Dietary Behaviors with Poor Sleep Quality and Increased Risk of Obstructive Sleep Apnea in Korean Military Service Members
Authors Choi Y , Son B, Shin WC, Nam SU, Lee J, Lim J , Kim S , Yang C , Lee H
Received 14 June 2022
Accepted for publication 13 September 2022
Published 25 September 2022 Volume 2022:14 Pages 1737—1751
DOI https://doi.org/10.2147/NSS.S378564
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ahmed BaHammam
Yujin Choi,1,* Byunwoo Son,2,* Woo-Chul Shin,3,4 Seong-uk Nam,5 Jaehong Lee,6 Jinwoong Lim,3,7 Sungha Kim,1 Changsop Yang,1 Hyeonhoon Lee8– 10
1KM Science Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea; 2Combined Dispensary, 7th Corps, Republic of Korea Army, Icheon, Republic of Korea; 3Department of Clinical Korean Medicine, Graduate School, Kyung Hee University, Seoul, Republic of Korea; 4Medical Company, 1st Airborne Special Forces Brigade, Republic of Korea Army, Seoul, Republic of Korea; 5 28th Division, Republic of Korea Army, Yangju-si, Republic of Korea; 6Medical Corps, The Capital Defense Command, Seoul, Republic of Korea; 7Department of Acupuncture and Moxibustion, Wonkwang University Gwangju Korean Medicine Hospital, Gwangju, Republic of Korea; 8Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Republic of Korea; 9Biomedical Research Institute, Seoul National University Hospital, Seoul, Republic of Korea; 10 9th Division, Republic of Korea Army, Goyang, Republic of Korea
*These authors contributed equally to this work
Correspondence: Changsop Yang, KM Science Research Division, Korea Institute of Oriental Medicine, 1672, Yuseong-daero, Yuseong-gu, Daejeon, 34054, Republic of Korea, Tel +82-42-869-2705, Fax +82-42-868-9395, Email [email protected] Hyeonhoon Lee, Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, 101 Daehak-ro, Jongno-gu, Seoul, 03080, Republic of Korea, Tel +82-2-2072-0505, Fax +82-2-747-5639, Email [email protected]
Purpose: Sleep quality among military service members is important for enhancing their capabilities and preventing psychiatric problems. We aimed to explore the association of dietary behaviors with poor sleep quality and increased risk of obstructive sleep apnea (OSA) in military men on active duty.
Patients and Methods: A large-scale multi-site cross-sectional survey was conducted in five units of the Republic of Korea’s army. Poor sleep quality and increased risk of OSA were defined using the Pittsburgh sleep quality index (PSQI) and Berlin Questionnaire, respectively. Information on dietary behaviors, including the frequency of skipping breakfast, eating snacks, consuming a night meal, and overeating, were collected.
Results: From August 2021 to September 2021, 4389 male respondents, mean age (20.8 ± 1.3 years), completed the survey; 2579 (58.8%) were assessed as having poor sleep quality, and 614 (14.0%) increased risk of OSA. After adjusting for lifestyle and occupational covariates, skipping breakfast 1– 2 times weekly was associated with an increased likelihood of experiencing poor sleep quality, compared with not skipping breakfast (odds ratio: 1.23 [95% CI 1.02– 1.47]). Eating night meals 5– 6 times weekly was also associated with poor sleep quality (odds ratio: 5.54 [95% CI 2.49– 14.18]). In addition, skipping breakfast daily (odds ratio: 2.28 [95% CI 1.27– 4.03]) and eating night meals daily (odds ratio: 2.30 [95% CI 1.21– 4.22]) were related to an increased risk of OSA.
Conclusion: Dietary behaviors appear to be related to poor sleep quality and a high risk of OSA. To improve sleep quality, dietary factors could be considered when promoting health programs for military personnel in further research.
Keywords: sleep, dietary behavior, insomnia, obstructive sleep apnea, military
Introduction
Sleep is an integral component of well-being that critically influences physical and mental abilities. In the military, sufficient sleep is important to ensure the adequate performance of individual members, promote mission success in each military unit, and even enhance national security.1,2 Enlisted personnel tend to have worse sleep quality than officers because they live in more crowded sleeping quarters.3,4 In addition, the number of patients visiting the United States (US) military medical facilities for insomnia and obstructive sleep apnea (OSA) showed a tendency to increase over time.4,5 Furthermore, there have been multiple studies of military personnel reporting the association of sleep disorders with post-traumatic stress disorder,6 depression,7 and anxiety.8–12
Epidemiological studies assessing sleep conditions have been conducted in the military across several countries. A Korean military health survey reported that 8.8–10.1% of the total respondents had moderate-to-severe sleep difficulty.13,14 Similarly, 8.1% of the study population in a single Korean military hospital had a high risk of OSA.15 Contrarily, a study involving US military personnel indicated that the incidence rates of insomnia and OSA were 2.7% and 3.3%, respectively.5 Additionally, the prevalence of subthreshold insomnia in multiple US army units ranged from 29.6 to 54.3%.16
In our previous study, most military personnel with insomnia had indigestion and were likely to eat night meals and snacks more frequently. After prescribing herbal medicine that could enhance digestive function, their insomnia improved.17 In a previous study regarding sleep disorders and associated medical comorbidities, pain syndrome was found to increase the risk of insomnia.6 Since it has been observed that many young male patients in the Korean army with insomnia also have indigestion symptoms linked to dietary habits, a large-scale cross-sectional study exploring the association between dietary behaviors and sleep was planned. The association between sleep and dietary behaviors has been examined in various populations, including factory workers18 and white-collar workers,19 but there is limited related research among military personnel. Military service members share similar sleep and nutritional conditions, and the effect of personal dietary behaviors on sleep can be clearly assessed after adjusting for related lifestyle and occupational factors.
This study, therefore, aimed to explore dietary factors, including skipping breakfast, overeating, snacking, and eating night meals, associated with poor sleep quality and high risk of OSA among military service members. Potential covariates of demographic and occupational factors in the military were also comprehensively evaluated.
Materials and Methods
Study Population
This cross-sectional survey was conducted among five units of the Republic of Korea’s army from August to September 2021. A link to the online survey was provided to members on active duty, and the responses were collected by five Korean medical doctors. Eligible service members participated in the study using their cellular phones. All participants provided informed consent and voluntarily participated in the study. The collected data were managed anonymously, and access was restricted so that only the specific researchers could access the personal information of the enrolled participants. The protocol and survey questionnaire were approved by the institutional review board of the Armed Forces Medical Command (AFMC-202107-HR-054-02). This study was conducted in accordance with the Declaration of Helsinki.
This study included enlisted service members on active duty aged ≥19 years who had completed their basic military training course. They comprised only enlisted service members in the following ranks: private, private first-class, corporal, and sergeant.
Definition of Poor Sleep Quality and High Risk of OSA
Poor sleep quality was defined by the global score of the Pittsburgh sleep quality index (PSQI), which is calculated by summing the seven component scores, including subjective quality, latency, duration, efficiency, disturbance of sleep, use of sleep medication, and daytime dysfunction.20 Two studies validated the Korean version of the PSQI and reported cut-off values of > 8 and > 5, respectively.21,22 Herein, we defined poor sleep quality as a global PSQI score > 5. An additional analysis was also carried out with the higher PSQI threshold of > 9, based on a previous PSQI study on military personnel.23 High risk of OSA was defined using the Berlin Questionnaire,24 which comprises three categories: snoring and witnessed apnea, daytime sleepiness or tiredness, and presence of hypertension or obesity. A high risk of OSA was reported when two or three categories were present.25
Study Variables
Dietary behavior information was collected using the dietary habit survey questionnaire,26 which included 25 items used to evaluate dietary habits, and we selected four items based on previous research. The frequencies of skipping breakfast, overeating, snacking, and eating night meals were included in the analysis.17–19
Data on demographic, lifestyle, and occupational factors were also collected to be analyzed as covariates. Participants’ age, educational level, height, and weight were recorded. Lifestyle factors included perceived stress level, smoking history, frequency of drinking, aerobic exercise per week, and coffee consumption. Occupational factors within the military included rank (private, private first class, corporal, or sergeant), position (combat arms, driver, military chef, administration), and the frequency of night shifts.
Statistical Analyses
Categorical variables were presented as frequencies (%), while continuous variables were presented as means (standard deviation). To compare the frequencies or means between the two groups (PSQI ≤ 5 and PSQI > 5) and (high risk or low risk of sleep apnea), the chi-square test or independent t-test was performed, respectively. Multivariable logistic regression analysis was used to explore the association between poor sleep quality and dietary behaviors; and between high risk of OSA and dietary behaviors. Demographic, lifestyle, and occupational factors were also included in the model as covariates. Unadjusted (univariate), and adjusted (multivariable) odds ratios, 95% confidence interval (CI), and p-value are presented. For statistical significance, p < 0.05. All analyses were performed using R version 4.1.3.27,28
Results
Study Flow and Characteristics of the Participants
In total, 4869 responses were collected through the online survey. After removing 35 duplicate responses and 139 responses from participants who did not meet the inclusion criteria (aged under 19 years or members not on active duty), 4695 responses from eligible participants remained. Of the 4695 eligible respondents, 4389 completed the entire survey without missing any sections.
The participants were men with a mean age of 20.8 ± 1.3 years. A PSQI global cutoff score >5 indicated poor sleep quality in 2579 (58.8%) respondents. The distribution of the PSQI global score in all participants is presented in Figure 1. Furthermore, 614 (14.0%) respondents were assessed as having a high risk of OSA according to the Berlin questionnaire. The participants’ characteristics are presented in Table 1. According to the existence of poor sleep quality and high risk of OSA, the characteristics of the participants showed differences in various demographic, lifestyle, occupational, and dietary factors.
 |  |  |
Table 1 Characteristics of Military Service Members |
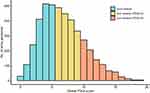 |
Figure 1 Distribution of global Pittsburgh sleep quality index (PSQI) scores. |
Poor Sleep Quality and Associated Factors
Dietary Behaviors
The adjusted odds ratios of dietary behaviors in the presence of poor sleep quality are presented in Figure 2 and Table 2. In the multivariable logistic regression, skipping breakfast 1–2 times a week was related to a greater likelihood of poor sleep quality than not skipping breakfast (odds ratio: 1.23 [95% confidence interval (CI): 1.02–1.47], p<0.001). The results of the univariable and multivariable logistic regression showed that the odds ratios tended to increase as the frequency of skipping breakfast increased to 5–6 times a week. Additionally, overeating 1–2 times or 3–4 times per week was associated with poor sleepers. Those who frequently ate snacks showed a significantly greater likelihood of experiencing poor sleep quality than those who did not (X2 = 13.6, df = 6, p = 0.035). Eating night meals 3–4 times or 5–6 times per week significantly increased the likelihood of poor sleep quality. However, eating night meals daily did not appear to be associated with an increased likelihood of poor sleep quality. The overall effect of night meals on poor sleep quality was significant (X2 = 22.3, df = 5, p < 0.001). Also, additional results of dietary behaviors for poor sleep quality (defined as a higher PSQI threshold > 9), are shown in Table 3. A similar tendency was observed between the dietary behaviors and poor sleep quality in both models for the two PSQI thresholds. The effects of skipping breakfast, overeating, and eating night meals on poor sleep quality seem distinctive when applying a higher PSQI threshold.
 |
Table 2 Multivariable Logistic Regression of Dietary Behaviors for Poor Sleep Quality (PSQI > 5) |
 |
Table 3 Multivariable Logistic Regression of Dietary Behaviors for Poor Sleep Quality (PSQI > 9) |
Other Lifestyle and Occupational Factors
The overall results of the multivariable logistic regression are presented in Tables S1 and S2. The severity of stress was highly associated with an increased likelihood of poor sleeping (X2 = 375.1, df = 4, p < 0.001). Additionally, coffee consumption more than twice daily had distinct effects on poor sleep quality when compared with drinking coffee less than once a week (twice daily: odds ratio 1.35 [95% CI 1.02–1.81], ≥three times daily: odds ratio 1.51 [95% CI: 1.02–2.27]). Among occupational factors, servicemen with military chef positions showed a greater likelihood of poor sleep quality than men in combat arms’ positions. In contrast, servicemen who were drivers showed a lower likelihood of being poor sleepers. Regardless of being off-duty after a night shift, frequent night shifts for more than five times a month were associated with poor sleep quality, compared with no night shifts.
High Risk of OSA and Associated Factors
Dietary Behaviors
The adjusted odds ratios of dietary behaviors in the presence of a high risk of OSA are presented in Figure 3 and Table 4. The results of the univariate and multivariable logistic regression showed that skipping breakfast every day led to a greater likelihood of being at high risk of OSA, compared with not skipping breakfast. Moreover, overeating 3–4 times a week was associated with a high risk of OSA. Frequent overeating was associated with a greater likelihood of being at high risk of OSA, as shown in the univariate logistic regression. However, this tendency decreased after adjusting for demographic factors, mainly body mass index (BMI). Snacking did not appear to be associated with a high risk of OSA after adjusting for covariates. In contrast, eating night meals was associated with a high risk of OSA. The overall effect of night meals on high risk of OSA was statistically significant (X2 = 13.2, df = 5, p = 0.021).
 |
Table 4 Multivariable Logistic Regression of Dietary Behaviors for High Risk of OSA |
Other Lifestyle and Occupational Factors
The overall results of the multivariable logistic regression are presented in Table S3. Exercising for more than 3–4 times a week was negatively correlated with a high risk of OSA. Furthermore, stress and drinking coffee more than three times a day had distinct effects on high risk of OSA. Among occupational factors, servicemen in administrative positions showed a lower likelihood of being at high risk of OSA than men in the combat arms division. The frequency of night shifts did not seem to be associated with high-risk OSA.
Discussion
In this cross-sectional study conducted among military service members in Korea, we explored poor sleep quality, high risk of OSA, and associated dietary factors. Among various dietary behaviors, a higher frequency of snacking and frequent and irregular eating of night meals were associated with poor sleep quality. In addition, a higher frequency of skipping breakfast, overeating, and having night meals seemed to be associated with a high risk of OSA.
Dietary Behaviors and Poor Sleep Quality
Night Meals
The time of eating has a major impact on circadian rhythms, and eating at night may shift and even disrupt such rhythms.29,30 In a previous study, higher caloric intake during dinner and late in the night was associated with longer sleep latency and lower sleep efficiency in women.31 In another study, late dinner was positively associated with poor sleep quality when compared to having an early dinner.32 In our study, we found that the higher frequency of eating night meals was associated with an increased tendency for poor sleep quality. In particular, the odds ratio dramatically increased when eating night meals 5–6 times per week. Interestingly, the effect of eating night meals on poor sleep quality was partially eliminated by eating night meals daily, 7 times per week. Frequent and irregular eating of night meals appears to be negatively associated with sleep quality. In addition to circadian rhythm disruptions, having to digest food or indigestion that might arise from eating night meals may negatively affect sleep quality.31,33 At the same time, the possibility of reverse causation also exists, in that participants with poor sleep quality may tend to eat night meals. Meanwhile, the concept of “night eating syndrome” has been proposed as a stress-related eating disorder, which is mainly characterized by night eating patterns and sleep disturbance.34,35 The pathophysiology of “night eating syndrome” describes the stress-induced decrease in the nocturnal secretion of melatonin and leptin as causing both eating night meals and insomnia.36 Eating night meals and poor sleep quality seems to be highly associated. The possible mechanism related to the association requires further research.37
Snacks/Overeating
In an epidemiological study of Japanese men aged 20–59 years, snacking habits were related to insufficient hours of sleep.18 Herein, the calculated odds ratio of poor sleep quality increased as the frequency of snacking and overeating increased. Furthermore, overeating 1–4 times a week also increased the likelihood of poor sleep. Snacking and overeating habits may also cause indigestion.38 Furthermore, consuming high-fat diets has been reported to worsen sleep/wake fragmentation in mice models.39 In addition, stress-induced eating in individuals with poor sleep quality may increase snacking habits, with a preference for eating energy-dense items.40 Further, sleeping for a short duration is known to affect appetite regulatory hormones, reducing leptin and elevating ghrelin,41 which may induce overeating. A recent randomized trial reported that interventions to increase sleep duration significantly decreased energy intake in overweight patients.42 Poor sleep quality and habits of snacking and overeating seem to have a reciprocal relationship.
Skipping Breakfast
Previous studies on the relationship between skipping breakfast and sleep patterns commonly reported that late sleepers typically tend to skip breakfast and a late bedtime is associated with the tendency to skip breakfast.43,44 This could be a confounding factor in the relationship between skipping breakfast and sleep quality.30 We collected data from military service members whose bedtime and meal times were almost identical since their regular sleep time was set from 10 pm to 6 am and the same meal was provided three times a day. Therefore, the data could be relatively independent of these confounding factors. In other studies, skipping breakfast was associated with shorter sleep duration in male workers aged 40–59 years,19 and daily breakfast consumption was associated with sufficient sleep in children.44 In addition, an intervention study reported that eating breakfast for seven days improved perceived sleep quality compared with skipping breakfast.45 In our study, we collected the frequency of skipping breakfast during the week, and a higher frequency of skipping breakfast was generally associated with a greater likelihood of poor sleep quality. However, responders who skipped breakfast daily showed a lower tendency of being poor sleepers. It seems that skipping breakfast irregularly adversely affects the maintenance of circadian rhythms.
Occupational Factors and Poor Sleep Quality
Some interesting occupational factors associated with poor sleep quality were observed in the participants. Our study included only enlisted personnel, most of them being in combat arms, and others being drivers, military chefs, or working in the administration. Poor sleepers were relatively frequent among military chefs since they are expected to wake up early at dawn to prepare the food and therefore get extra sleep time in the late morning after work. Possible reasons for frequent poor sleep quality in these military chefs may be related to the fact that splitting sleep could negatively affect subjective sleep quality.46 Contrarily, drivers had lower sleep disturbances, which can be explained by the efforts of the military to prevent vehicle accidents that could be caused by drowsy driving.47,48 In Korea, drivers are rarely assigned to night sentry duties, and even if assigned, they are placed early in the night or early in the morning rather than in the middle of the night. The likelihood of lower sleep disturbances in drivers was significant, even after adjusting the frequency of night shifts. Policies implemented by the military seem to have been relatively effective in preventing sleep disorders among drivers.
Military rank was also related to sleep disturbances, with a private rank leading to a lower likelihood of experiencing poor sleep quality. In the Korean army, mandatorily enlisted personnel are of the private rank until the 8th week, and they receive basic military training courses during the first five to seven weeks. During these courses, enlisted personnel receive intensive physical training, maintain a constant schedule for sleep and meals, and cannot eat snacks or night meals. In the present study, those with private ranks who had just completed this training course showed a lower likelihood of experiencing poor sleep quality. Approximately 5–7 weeks of regular sleep/meal rhythms and intensive physical training may be related to a reduced number of poor sleepers. In support of this, regularizing the sleep-wake schedule was reported to improve subjective sleep efficiency in an experimental study.49 However, a previous study showed that the duration of military service was a factor that increased the risk of insomnia symptoms.50 This may partially explain the concluded results that first-class privates, corporals, and sergeants showed a higher tendency of experiencing sleep disturbances, compared to privates.
The night shift was a major factor involved in the development of sleep disturbances in previous studies.51,52 When the frequency of night shift was > 5 times in one month, the likelihood of poor sleep quality significantly increased in this study.
Dietary Behaviors and High Risk of OSA
Overeating
Overeating was clearly associated with a high risk of OSA in the univariate logistic regression, but the tendency was diminished in the multivariable logistic regression. The association between overeating and the high risk of OSA seemed to be mainly explained by BMI because the strength of the association decreased after adjusting for BMI. Being overweight is a risk factor for OSA,53,54 and frequent overeating can lead to a higher BMI.
Night Meals
The effect of eating night meals on the high risk of OSA was significant after adjusting for BMI. Additionally, the odds ratio increased as the frequency of night meals increased. Previous studies have also reported that eating night meals adversely affects symptom severity in patients with OSA. Increased food intake in the evening was related to decreased sleep quality in patients with sleep apnea.55 Additionally, patients with OSA who had a late dinner showed a higher apnea-hypopnea index (AHI) than those who had an early dinner.32 Further, consuming fatty meals before bedtime significantly increased the AHI compared with light meals, in patients with OSA.56 Considering the Republic of Korea army environment where this survey was conducted, military service members usually eat calorific foods such as fried chicken and pizza for night meals. Both the timing and characteristics of night meals appear to have a negative effect on OSA. Avoiding night meals appears to be an important dietary behavior that plays a role in preventing or alleviating sleep apnea.
Skipping Breakfast
Skipping breakfast daily was clearly associated with a high risk of OSA. This behavior is different from the one associated with poor sleep quality, which involved irregular skipping behaviors. In a previous study that researched meal timing and sleep parameters in patients with OSA, skipping breakfast did not influence the severity of sleep apnea.32 In contrast, in a different study of patients with obesity and OSA, higher caloric intake at breakfast was associated with lower AHI.55 The reason for this association between skipping breakfast and high risk of OSA is unclear, but the potential factors include being overweight,57 having hypertension,58 and insulin resistance,58 which are known to be related to the habit of skipping breakfast. Being overweight and having hypertension or insulin resistance are both risk factors for OSA.59,60 Further research is required to explore the effects and mechanisms of skipping breakfast on OSA.
Occupational Factors and High Risk of OSA
In the present study, sedentary workers in administrative positions showed a lower likelihood of being at high risk of OSA, compared with personnel in combat arms whose main tasks were special qualifications’ training. In a study conducted in Korea, the prevalence of high risk of OSA was 10.7% in the white-collar group and 13.4% in the blue-collar group, but the difference between the two groups was not significant.61 When comparing the characteristics of personnel in administration and combat arms, older age, higher educational level, and negative smoking status were observed in the administrative group (Table S4). Although the odds ratio of the administration group compared to the combat arms group was still below one after adjusting for all covariates, some reports suggest that a higher educational level is associated with a lower risk of OSA.62–64 The characteristics of personnel in administrative positions may explain the lower risk of OSA; thus, further studies are required.
Limitations and Implication
This study has several limitations. First, only men in their early 20s were included. Therefore, generalizing the results of this study to other sex and age groups is limited. Second, due to the limitations imposed by a cross-sectional design, it is difficult to demonstrate causality, and only an association can be derived. Third, poor sleep quality and high risk of OSA were defined using self-reported questionnaires. Fourth, objective sleep parameters were not included in this study.
Nevertheless, we successfully obtained practical data from a large population to understand the relationship between dietary behaviors and sleep quality. Although the association between sleep and dietary conditions should be comprehensively examined with various potential covariates, it is challenging when the type and amount of data are limited.65 Therefore, our large-scale study using various symptom examination tools may provide a deep and broad understanding of the association between sleep and other factors, which could be a milestone for future studies (Table S5).
Additionally, these results may provide insights for military policymakers regarding the development of health promotion programs for military personnel. Based on our findings and related previous research, the dietary behaviors of military service members should receive attention to improve their sleep quality and prevent the risk of OSA. Especially, a policy to avoid frequent changes in meal timings (higher frequency of eating night meals or skipping breakfast) should be considered to improve sleep quality. In addition, an educational program to decrease the frequency of snacking and overeating can be developed to prevent the risk of OSA.
Conclusion
In this large-scale cross-sectional study that included 4389 Korean military service members, eating a night meal 5–6 times/week, skipping breakfast irregularly, and eating snacks frequently were associated with poor sleep quality. Whereas, eating night meals and skipping breakfast daily were associated with a high risk of OSA. Irregular dietary behaviors appear to be related to poor sleep quality and a high risk of OSA. To determine the possible mechanisms related to the associations between sleep and dietary behaviors needs further research.
Funding
This research was supported by a grant from the Korea Institute of Oriental Medicine [KSN2022210].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Capaldi VF, Balkin TJ, Mysliwiec V. Optimizing sleep in the military: challenges and opportunities. Chest. 2019;155(1):215–226. doi:10.1016/j.chest.2018.08.1061
2. Good CH, Brager AJ, Capaldi VF, Mysliwiec V. Sleep in the United States military. Neuropsychopharmacology. 2020;45(1):176–191. doi:10.1038/s41386-019-0431-7
3. Taylor DJ, Pruiksma KE, Hale WJ, et al. Prevalence, correlates, and predictors of insomnia in the US Army prior to deployment. Sleep. 2016;39(10):1795–1806. doi:10.5665/sleep.6156
4. Caldwell JA, Knapik JJ, Lieberman HR. Trends and factors associated with insomnia and sleep apnea in all United States military service members from 2005 to 2014. J Sleep Res. 2017;26(5):665–670. doi:10.1111/jsr.12543
5. Moore BA, Tison LM, Palacios JG, Peterson AL, Mysliwiec V. Incidence of insomnia and obstructive sleep apnea in active duty United States military service members. Sleep. 2021;44(7):zsab024. doi:10.1093/sleep/zsab024
6. Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. Sleep. 2013;36(2):167–174. doi:10.5665/sleep.2364
7. Livingston WS, Rusch HL, Nersesian PV, Baxter T, Mysliwiec V, Gill JM. Improved sleep in military personnel is associated with changes in the expression of inflammatory genes and improvement in depression symptoms. Front Psychiatry. 2015;6:59. doi:10.3389/fpsyt.2015.00059
8. Mysliwiec V, Gill J, Lee H, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549–557. doi:10.1378/chest.13-0088
9. Miller KE, Brownlow JA, Gehrman PR. Sleep in PTSD: treatment approaches and outcomes. Curr Opin Psychol. 2020;34:12–17. doi:10.1016/j.copsyc.2019.08.017
10. Cappuccio FP, Miller MA. Sleep and cardio-metabolic disease. Curr Cardiol Rep. 2017;19(11):110. doi:10.1007/s11886-017-0916-0
11. Vitiello MV, Zhu W, Von Korff M, et al. Long-term improvements in sleep, pain, depression, and fatigue in older adults with comorbid osteoarthritis pain and insomnia. Sleep. 2022;45(2). doi:10.1093/sleep/zsab231
12. Generaal E, Vogelzangs N, Penninx BW, Dekker J. Insomnia, sleep duration, depressive symptoms, and the onset of chronic multisite musculoskeletal pain. Sleep. 2017;40(1). doi:10.1093/sleep/zsw030
13. Kim TK, Lee HC, Lee SG, Han KT, Park EC. The combined effect of sleep duration and quality on mental health among Republic of Korea Armed Forces. Mil Med. 2016;181(11):e1581–e1589. doi:10.7205/MILMED-D-15-00538
14. Yeom CW, Oh GH, Jung S, et al. Prevalence and comorbidities of adult ADHD in male military conscripts in Korea: results of an epidemiological survey of mental health in Korean military service. Psychiatry Res. 2020;293:113401. doi:10.1016/j.psychres.2020.113401
15. Lee YC, Eun YG, Shin SY, Kim SW. Prevalence of snoring and high risk of obstructive sleep apnea syndrome in young male soldiers in Korea. J Korean Med Sci. 2013;28(9):1373–1377. doi:10.3346/jkms.2013.28.9.1373
16. Mantua J, Bessey AF, Mickelson CA, et al. Sleep and high-risk behavior in military service members: a mega-analysis of four diverse U.S. Army units. Sleep. 2021;44(4). doi:10.1093/sleep/zsaa221
17. Lee H, Nam S, Choi Y, Son B. Effectiveness of herbal medicines for the treatment of insomnia in Korean military service members: a prospective pilot study. BMJ Mil Health. 2022;e002070. doi:10.1136/bmjmilitary-2021-002070
18. Imaki M, Hatanaka Y, Ogawa Y, Yoshida Y, Tanada S. An epidemiological study on relationship between the hours of sleep and life style factors in Japanese factory workers. J Physiol Anthropol Appl Human Sci. 2002;21(2):115–120. doi:10.2114/jpa.21.115
19. Nishiura C, Noguchi J, Hashimoto H. Dietary patterns only partially explain the effect of short sleep duration on the incidence of obesity. Sleep. 2010;33(6):753–757. doi:10.1093/sleep/33.6.753
20. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
21. Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012;16(3):803–812. doi:10.1007/s11325-011-0579-9
22. Shin S, Kim SH, Reliability T. Validity testing of Korean version of the Pittsburgh Sleep Quality Index. J Converg Inf Technol. 2020;10(11):148–155.
23. Matsangas P, Mysliwiec V. The utility of the Pittsburgh Sleep Quality Index in US military personnel. Mil Psychol. 2018;30(4):360–369. doi:10.1080/08995605.2018.1478547
24. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485–491. doi:10.7326/0003-4819-131-7-199910050-00002
25. Kang K, Park KS, Kim JE, et al. Usefulness of the Berlin Questionnaire to identify patients at high risk for obstructive sleep apnea: a population-based door-to-door study. Sleep Breath. 2013;17(2):803–810. doi:10.1007/s11325-012-0767-2
26. Jo JS, Kim KN. Development of a questionnaire for dietary habit survey of Korean adults. Korean J Community Nutr. 2014;19(3):258–273. doi:10.5720/kjcn.2014.19.3.258
27. R Core Team. R: a language and environment for statistical computing. R foundation for statistical computing; 2022. Available from: https://www.R-project.org/.
28. Harrison E, Drake T, Ots R. Finalfit: quickly create elegant regression results tables and plots when modelling; 2021. Available from: https://CRAN.R-project.org/package=finalfit.
29. Kräuchi K, Cajochen C, Werth E, Wirz-Justice A. Alteration of internal circadian phase relationships after morning versus evening carbohydrate-rich meals in humans. J Biol Rhythms. 2002;17(4):364–376. doi:10.1177/074873040201700409
30. Rogers M, Coates AM, Banks S. Meal timing, sleep, and cardiometabolic outcomes. Curr Opin Endocr Metab Res. 2021;18:128–132. doi:10.1016/j.coemr.2021.03.006
31. Crispim CA, Zimberg IZ, Dos Reis BG, Diniz RM, Tufik S, de Mello MT. Relationship between food intake and sleep pattern in healthy individuals. J Clin Sleep Med. 2011;7(6):659–664. doi:10.5664/jcsm.1476
32. Lopes T, Borba ME, Lopes R, et al. Eating late negatively affects sleep pattern and apnea severity in individuals with sleep apnea. J Clin Sleep Med. 2019;15(3):383–392. doi:10.5664/jcsm.7658
33. Uçar C, Özgöçer T, Yıldız S. Effects of late-night eating of easily-or slowly-digestible meals on sleep, hypothalamo-pituitary-adrenal axis, and autonomic nervous system in healthy young males. Stress Health. 2021;37(4):640–649. doi:10.1002/smi.3025
34. Stunkard AJ, Grace WJ, Wolff HG. The night-eating syndrome; a pattern of food intake among certain obese patients. Am J Med. 1955;19(1):78–86. doi:10.1016/0002-9343(55)90276-X
35. Vander Wal JS. Night eating syndrome: a critical review of the literature. Clin Psychol Rev. 2012;32(1):49–59. doi:10.1016/j.cpr.2011.11.001
36. Birketvedt GS, Sundsfjord J, Florholmen JR. Hypothalamic-pituitary-adrenal axis in the night eating syndrome. Am J Physiol Endocrinol Metab. 2002;282(2):E366–369. doi:10.1152/ajpendo.00251.2001
37. Svedlund J, Sjödin I, Dotevall G. GSRS--a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci. 1988;33(2):129–134. doi:10.1007/BF01535722
38. Sahu S, Dey M. Changes in food intake pattern of nurses working in rapidly rotating shift. Al Ameen J Med Sci. 2011;4(1):14–22.
39. Perron IJ, Pack AI, Veasey S. Diet/energy balance affect sleep and wakefulness independent of body weight. Sleep. 2015;38(12):1893–1903. doi:10.5665/sleep.5236
40. Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23(11–12):887–894. doi:10.1016/j.nut.2007.08.008
41. Taheri S, Lin L, Austin D, Young T, Mignot E, Froguel P. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62. doi:10.1371/journal.pmed.0010062
42. Tasali E, Wroblewski K, Kahn E, Kilkus J, Schoeller DA. Effect of sleep extension on objectively assessed energy intake among adults with overweight in real-life settings: a randomized clinical trial. JAMA Intern Med. 2022;182(4):365–374. doi:10.1001/jamainternmed.2021.8098
43. Chang ZS, Boolani A, Conroy DA, Dunietz T, Jansen EC. Skipping breakfast and mood: the role of sleep. Nutr Health. 2021;27(4):373–379. doi:10.1177/0260106020984861
44. Teixeira GP, Mota MC, Crispim CA. Eveningness is associated with skipping breakfast and poor nutritional intake in Brazilian undergraduate students. Chronobiol Int. 2018;35(3):358–367. doi:10.1080/07420528.2017.1407778
45. Gwin JA, Leidy HJ. Breakfast consumption augments appetite, eating behavior, and exploratory markers of sleep quality compared with skipping breakfast in healthy young adults. Curr Dev Nutr. 2018;2(11):nzy074. doi:10.1093/cdn/nzy074
46. Matsangas P, Shattuck NL. Sleep quality, occupational factors, and psychomotor vigilance performance in the U.S. Navy sailors. Sleep. 2020;43(12). doi:10.1093/sleep/zsaa118
47. McKeon AB, Mantua J, Sowden WJ. Sleep tactics for multidomain operations in US Army military personnel: optimising sleep opportunities to support readiness and lethality. BMJ Mil Health. 2021;bmjmilitary-2020–001731. doi:10.1136/bmjmilitary-2020-001731
48. MacLean AW, Davies DR, Thiele K. The hazards and prevention of driving while sleepy. Sleep Med Rev. 2003;7(6):507–521. doi:10.1016/S1087-0792(03)90004-9
49. Manber R, Bootzin RR, Acebo C, Carskadon MA. The effects of regularizing sleep-wake schedules on daytime sleepiness. Sleep. 1996;19(5):432–441. doi:10.1093/sleep/19.5.432
50. Cooper AD, Kolaja CA, Markwald RR, Jacobson IG, Chinoy ED. Longitudinal associations of military-related factors on self-reported sleep among U.S. service members. Sleep. 2021;44(12). doi:10.1093/sleep/zsab168
51. Goh VH, Tong TY, Lim CL, Low EC, Lee LK. Circadian disturbances after night-shift work onboard a naval ship. Mil Med. 2000;165(2):101–105. doi:10.1093/milmed/165.2.101
52. Helvaci G, Aslan Çin NN, Canbulat Ş, Yardimci H. Evaluating diet and sleep quality of shift and non-shift nurses using three-factor Pittsburgh Sleep Quality Index and healthy eating index-2015. Sleep Med Res. 2020;11(2):94–101. doi:10.17241/smr.2020.00682
53. Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015–3021. doi:10.1001/jama.284.23.3015
54. Pretto JJ, Gyulay SG, Hensley MJ. Trends in anthropometry and severity of sleep-disordered breathing over two decades of diagnostic sleep studies in an Australian adult sleep laboratory. Med J Aust. 2010;193(4):213–216. doi:10.5694/j.1326-5377.2010.tb03870.x
55. de Melo CM, Del Re MP, Dos Santos Quaresma MVL, et al. Relationship of evening meal with sleep quality in obese individuals with obstructive sleep apnea. Clin Nutr ESPEN. 2019;29:231–236. doi:10.1016/j.clnesp.2018.09.077
56. Trakada G, Steiropoulos P, Zarogoulidis P, et al. A fatty meal aggravates apnea and increases sleep in patients with obstructive sleep apnea. Sleep Breath. 2014;18(1):53–58. doi:10.1007/s11325-013-0847-y
57. Stote KS, Baer DJ, Spears K, et al. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults. Am J Clin Nutr. 2007;85(4):981–988. doi:10.1093/ajcn/85.4.981
58. Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr. 2005;81(2):388–396. doi:10.1093/ajcn.81.2.388
59. Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med. 2002;165(5):670–676. doi:10.1164/ajrccm.165.5.2103001
60. Ramadan W, Dewasmes G, Petitjean M, et al. Sleep apnea is induced by a high-fat diet and reversed and prevented by metformin in non-obese rats. Obesity. 2007;15(6):1409–1418. doi:10.1038/oby.2007.169
61. Kang K, Seo JG, Seo SH, Park KS, Lee HW. Prevalence and related factors for high-risk of obstructive sleep apnea in a large Korean population: results of a questionnaire-based study. J Clin Neurol. 2014;10(1):42–49. doi:10.3988/jcn.2014.10.1.42
62. Etindele Sosso FA, Matos E. Socioeconomic disparities in obstructive sleep apnea: a systematic review of empirical research. Sleep Breath. 2021;25(4):1729–1739. doi:10.1007/s11325-020-02274-z
63. Li X, Sundquist K, Sundquist J. Socioeconomic status and occupation as risk factors for obstructive sleep apnea in Sweden: a population-based study. Sleep Med. 2008;9(2):129–136. doi:10.1016/j.sleep.2007.02.003
64. Adams RJ, Piantadosi C, Appleton SL, et al. Investigating obstructive sleep apnoea: will the health system have the capacity to cope? A population study. Aust Health Rev. 2012;36(4):424–429. doi:10.1071/AH11098
65. Kim NH, Shin DH, Kim HT, Jeong SM, Kim SY, Son KY. Associations between metabolic syndrome and inadequate sleep duration and skipping breakfast. Korean J Fam Med. 2015;36(6):273–277. doi:10.4082/kjfm.2015.36.6.273
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


