Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Association of Age and Response to Methylphenidate HCL Treatment in Adult ADHD: A Proton Magnetic Resonance Spectroscopy Study
Received 30 September 2023
Accepted for publication 13 February 2024
Published 20 February 2024 Volume 2024:20 Pages 317—324
DOI https://doi.org/10.2147/NDT.S442655
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Gonca Ayse Unal,1 Ayse Nur Inci Kenar2
1Clinic of Psychiatry, Mersin City Hospital, Mersin, Turkey; 2Department of Psychiatry, Faculty of Medicine, Pamukkale University, Denizli, Turkey
Correspondence: Ayse Nur Inci Kenar, Department of Psychiatry, Faculty of Medicine, Pamukkale University, Denizli, 20070, Turkey, Tel +90-258-2966000, Email [email protected]
Purpose: This study investigated the age-dependent effects of methylphenidate (MPH) on brain metabolites including choline (Cho), N-acetyl aspartate (NAA) and creatine (Cr) levels in the dorsolateral prefrontal cortex (DLPFC), striatum, cerebellum, and anterior cingulate cortex (ACC) regions of the brain in adult patients with attention deficit hyperactivity disorder (ADHD).
Patients and Methods: The study was included 60 patients with ADHD between the ages of 18 and 60 years. The patients were grouped with respect to their ages as follows: 18– 24 years, 25– 30 years, and 31 and over years. Levels of NAA, Cr and Cho in DLPFC, ACC, cerebellum and striatum were measured with magnetic resonance spectroscopy (MRS). Subjects were then given 10 mg of oral MPH and the same metabolite levels were measured 30 minutes apart.
Results: Twelve (20%) of the cases were female and 48 (80%) were male. The age distribution of the cases is as follows: 15 subjects between the ages of 18– 24, 26 subjects between the ages of 25– 30 and 19 subjects over the age of 30. NAA levels were higher after MPH in the DLPFC of the 18– 24 age group (p = 0.016) and in the cerebellum of the 25– 30 age group (p = 0.041). No increase in Cho and Cr levels was observed after treatment compared to before (p > 0.05).
Conclusion: It is thought that treatment of MPH can be effective on metabolites in different brain regions and this effect can vary upon age adult ADHD patients. After MPH treatment, both the 18– 24 age group (in the DLPFC) and the 25– 30 age group (in the cerebellum) was detected significantly higher NAA levels compared to pre-treatment levels. This increase in NAA levels suggested that pharmacotherapy, especially at early ages, may be effective on neuronal damage.
Keywords: adult, attention deficit hyperactivity disorder, magnetic resonance spectroscopy, methylphenidate, age
Introduction
Neuroimaging techniques have been crucial to understanding the functional and structural changes in brain regions associated with attention deficit hyperactivity disorder (ADHD). Recent advances in these techniques also enable such further research into brain structures and functions in response to psychostimulant drug treatments. In structural neuroimaging studies; volume reduction has been reported in brain regions such as the frontal lobe, cerebellum, corpus callosum, total and right brain, and caudate nucleus.1 In functional neuroimaging studies; It has been reported that regional blood circulation and glucose metabolism decrease in the prefrontal cortex (PFC) and cerebellar regions, but increase in the parietooccipital cortex at rest, and symptoms regress after psychostimulant drug treatment.2 Magnetic resonance spectroscopy (MRS) is used in the differential diagnosis of diseases with neurodegenerative activity. N-acetyl aspartate (NAA) as an indicator of overall neuronal integrity, low NAA/creatine (Cr) ratio is associated with neuronal loss or damage. Choline (Cho) reflects membrane integrity and higher choline levels or Cho/Cr ratio indicate higher cellular destruction, myelin degradation, gliosis and inflammation. Creatine is an invariable member of cellular energy metabolism.3
A meta-analysis of 16 MRS studies analyzed the effect of age on neurochemical abnormality in both children and adults with ADHD.4 Eleven studies included children with ADHD, while five involved adults with ADHD.5–9 All five studies included drug-free adults with ADHD. In this meta-analysis, it was reported that the NAA level in the PFC of children with ADHD was higher than normal, but there was no difference in the striatum and cerebellum. No difference in metabolite levels was found at any other site in adults with ADHD. In addition, it has been reported that there is a negative correlation between high NAA levels in PFC and the mean age of the patients. It has been suggested that the age-related abnormality of the NAA level in the PFC is a potential neural basis for the age-related variation of ADHD symptoms.4
Most neuroimaging studies have supported disruption in the frontostriatal cerebellar circuit. Methylphenidate (MPH) has been shown to affect frontostriato-thalamic circuit functions related to the pathophysiology of ADHD.10 It has been reported that blood flow velocity increased in caudate, bilateral prefrontal and thalamic regions after MPH application.2 Methylphenidate is effective in maintaining adequate attention through the dopamine and serotonin system in the neocortex and filtering out unnecessary sensory stimuli by normalizing hyperexcitability in the somatosensory cortex.2
Studies examining treatment-related metabolic changes in adults with ADHD are very few.11 In the literature, MRS studies investigating the effect of stimulant treatment was availabed only thirteen studies.11 Five of these studies were conducted in adult ADHD.11–15 In these studies, changes in the brain were examined before and after MPH. Different results have been reported.
There is no study in the English literature investigating the effects of MPH on the age-related brain. This study aimed to evaluate the age-related effects of MPH on NAA, Cr and Cho levels in the dorsolateral prefrontal cortex (DLPFC), striatum, cerebellum, and anterior cingulate cortex (ACC) in adult ADHD patients.
Patients and Methods
Study Design
Sixty patients aged 18–60 years who met the criteria for adult ADHD according to the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV) were included in the study. Patients with concomitant neurological disease, mental retardation and psychiatric disorders were excluded from the study. Wender Utah Rating Scale (WURS) and Adult ADHD Diagnosis and Rating Scale were used to evaluate patients.
Wender–Utah Rating Scale (WURS)
This scale can be used to assess adults for attention deficit hyperactivity disorder with a subset of 25 questions associated with that diagnosis. A validity and reliability study of WURS was conducted for Turkish individuals with a cut-off score of 36.16
Adult ADD/ADHD DSM IV- Based Diagnostic Screening and Rating Scale
This scale is a self assessment scale and patients can complete the questionnaire after being duly informed. When developing adult ADD/ADHD Scale, 18 symptoms of the diagnostic criteria in DSM-IV were reframed, so patients can understand them. The first part of this scale had 9 inattention questions and the second part had 9 hyperactivity/impulsivity questions. The Adult ADD/ADHD DSM-IV Based Diagnostic Screening and Rating Scale has a validity and reliability study for Turkish individuals.17
Patients who scored 36 points or more on the WURS and gave an answer of 2 or 3 points to at least six of the nine questions in the first and/or second parts of the Adult ADHD Diagnosis and Evaluation Scale were diagnosed with ADHD.
Levels of NAA, Cr and Cho in DLPFC, ACC, cerebellum and striatum were measured via proton MRS. Subjects were then given 10 mg of oral MPH and the same metabolite levels were measured 30 minutes apart. The patients were grouped with respect to their ages as follows: 18–24 years, 25–30 years, and ≥31 years. The study was conducted in line with the principles of the Declaration of Helsinki and was approved by the Pamukkale University Faculty of Medicine Ethics Committee (date:25/03/2011 no:52). Informed written consent was obtained from all patients included in the study.
Proton Magnetic Resonance Spectroscopy
1.5 Tesla MR device (GE Medical System, Milwaukee, WI, USA) used with a standard head coil. The MRS protocol was as follows: horizontal plane, 10 mm thickness; TR/TE, 3000/88.2; Angle of View, 10; matrix, 512 × 512; Then 1. T2 weighted fast spin echo sequences were obtained using these parameters. MRS was performed using the single voxel (¹H-voxel) technique inserted into each of the DLPF, ACC, cerebellum and striatum. A volume of interest was manually placed in each area of the appropriate brain tissue. The chemical shift selective pulse (CHESS) method was used to suppress water-borne signals. Following this, point-resolved spectroscopy (PRESS) technique was used to localize the spectroscopy volume (TR/TE: 3000–35). As a result, short TE time spectra were obtained from the VOI in the ACC, striatum, DLPFC and cerebellum regions, and the metabolite ratios obtained with the “General Electric software spectral analysis program” were evaluated. H1 MRS analyzes were performed by the radiologist and NAA, Cho, Cr values were measured in the DLPFC, ACC, cerebellum and striatum areas. Patients were given 10 mg oral methylphenidate and after a 30-minute waiting period, NAA, Cho, Cr values were measured again.
Statistical Analysis
Statistical Package for the Social Sciences version 16 (SPSS, Inc., Chicago, Il, USA) was used for data analysis. The change from before in brain metabolite levels after MPH administration was analyzed with a paired t-test. The Kruskal–Wallis test was used to compare brain metabolite levels before and after MPH administration between age groups. A p-value <0.05 was considered statistically significant. Mann Whitney U-test was used to determine the group that caused the difference. Bonferroni correction for multiple comparisons using the Mann–Whitney U-test was performed (0.05/3 = 0.017) to analyze the nonparametric Kruskal–Wallis test results. Therefore, the p value was considered significant as 0.05/3=0.017 since there were three groups.
Results
The study included 60 patients (20% of them were female) with a mean age of 28.98 ± 7.66 years (range, 18–59 years). The distribution of the patients regarding ADHD subtype groups was as follows: 21 (35.0%) were predominantly inattentive, 11 (18.3%) were predominantly hyperactive/impulsive and 28 (46.7%) were combined type.
In the 18–24 years age group, the increase in the NAA levels in the DLPFC region of the patients after MPH treatment was significant compared to their pretreatment levels (p = 0.016). In the 25–30 years age group, the increase in the NAA levels in the cerebellum region of the patients after MPH treatment was significant compared to their pretreatment levels (p = 0.041).
Table 1 shows the NAA levels of the patients measured in the ACC, striatum, cerebellum, and DLPFC regions before and after MPH treatment between the age groups. There was a significant difference in NAA levels between the age groups before MPH treatment in the striatum (p = 0.005). Accordingly, NAA levels of the patients in the 18–24 years age group were significantly higher than that of the 25–30 years and ≥31 years age groups (respectively Mann Whitney U = 82,500; p = 0.002 < 0.017 (0.05/3)), Mann Whitney U = 66,000; p = 0.008 < 0.017 (0.05/3). In other brain regions, before and after MPH treatment, there were no significant differences in NAA levels between age groups (p > 0.05).
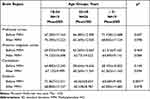 |
Table 1 Age-Dependent Distribution of N-Acetyl Aspartate Levels Before and After Methylphenidate Treatment |
Table 2 outlines the Cr levels of the patients measured in the ACC, striatum, cerebellum, and DLPFC regions before and after MPH treatment regarding age groups. In striatum, before MPH treatment, there was significant difference in Cr levels between age groups (p = 0.001). According to data, Cr levels of the patients in the 18–24 years age group were significantly higher than that of the 25–30 years and ≥31 years age groups (respectively MannWhitney U = 76,000; p = 0.001 < 0.017 (0.05/3), Mann Whitney U = 44,500; p = 0.001 < 0.017 (0.05/3)). Additionally, there was a significant difference between age groups in Cr levels after MPH treatment in the striatum (p = 0.047). Accordingly, the Cr levels of the patients in the 18–24 years age group were significantly higher than that of the 25–30 years age group (Mann Whitney U = 107,000; p = 0.017 (0.05/3)). There was no significant difference in Cr levels between the age groups before and after MPH treatment in other parts of the brain (p > 0.05).
 |
Table 2 Age-Dependent Distribution of Creatine Levels Before and After Methylphenidate Treatment |
Table 3 displays the Cho levels of the patients measured in the ACC, striatum, cerebellum, and DLPFC regions before and after MPH treatment regarding age groups. In striatum, before MPH treatment, there was significant difference in Cho levels between age groups (p = 0.041). Accordingly, Cho levels of the patients in the 18–24 years age group were significantly higher than that of the 25–30 years age group (Mann Whitney U = 106,000; p = 0.016 < 0.017 (0.05/3)). There was no significant difference between age groups in Cho levels before and after MPH treatment in other brain regions (p > 0.05).
 |
Table 3 Age-Dependent Distribution of Choline Levels Before and After Methylphenidate Treatment |
Discussion
The current study results demonstrated that there were significant differences in the brain metabolite levels between different age groups of ADHD patients prior to the MPH treatment. Following MPH treatment, there were significant differences both between age groups and within the same age groups compared to their pretreatment levels.
In a meta-analysis including sixteen MRS studies, it was analyzed that the effect of age on neurochemical abnormality in both children and adult with ADHD.4 Five of these studies was on adult ADHD.5–9 In this meta-analysis, increased NAA levels were found in the medial prefrontal cortex of children with ADHD but no abnormal data in adults with ADHD.4 In adults with ADHD, no difference in metabolite levels was found in any other region. In addition, it was revealed a negative correlation between heightened NAA levels and mean age of patients in PFC.4 In a previous study, significantly lower concentrations of NAA were measured in the left DLPFC in unmedicated ADHD patients compared to healthy controls and they emphasized that NAA levels have a particular importance in brain metabolite studies because a decrease in NAA levels implies a reversible stage of severe neuronal dysfunction in the patients.18 In this study, before MPH treatment, in the striatum region, NAA levels of the patients in the 18–24 years age group were significantly higher than the other age groups and in the same region. Additionally, considering that age and NAA levels are negatively correlated in the literature, and NAA levels decrease as the brain develops, higher NAA levels were found at earlier ages in accordance with the literatüre in our study.19
In this study, after MPH treatment, both the 18–24 years age group (in the DLPFC) and the 25–30 years age group (in the cerebellum) displayed significantly increased NAA levels compared to their pretreatment levels. In a study conducted by Bertolino et al20 on schizophrenic patients; After 4 weeks of atypical antipsychotic use, an increase in the NAA/Cr ratio was observed in DLPFC and it was suggested that pharmacotherapy may be effective on brain metabolites. NAA is an indicator of overall neuronal integrity, and a decrease in NAA levels indicates a reversible phase of severe neuronal dysfunction.18 In light of this information, this increase in NAA levels suggested that the treatment of MPH may be effective on neuronal damage, especially at early ages. Additionally, the study suggests that ongoing neuronal plasticity, which is likely to be the case before more than half of our patients were also receiving treatment, continues after a single dose of MPH treatment.
Before MPH treatment, in the striatum region, Cr levels of the patients in the 18–24 years age group were significantly higher than the other age groups and in the same region. In normal people, Cr increases with age. On the other hand, it decreases in hypoxia and hypoperfusion.21 In a study examining the effects of long-term use of MPH on cerebral blood flow in ADHD patients, a decrease in regional cerebral blood flow was found in the right hemisphere orbitofrontal cortex and anterior part of the middle PFC compared to the control group before treatment.22 This abnormal decrease in the right PFC returned to normal after treatment. Regional cerebral blood flow in the right striatum decreased with MPH treatment. However, the treatment resulted in increased blood flow in the upper PFC regions. Striatal activity may have been inhibited by MPH-induced prefrontal activation. Because inhibitory signals are sent to the striatum by cortical dopamine activity in the prefrontal region via the frontostriatal circuit. These comments support the view that the main pathology in ADHD is PFC dysfunction and subsequent striatal hyperactivation.22 In our study, increased striatal blood flow and Cr values were found before MPH, which was consistent with this study. Higher Cr levels at early ages may be related to the fact that ADHD symptoms are more severe at these ages and that striatal hyperactivation is more common at this age.
In addition, after MPH treatment, Cr levels in the striatum region of the patients in the 18–24 years age group were significantly higher than that of the 25–30 years age group. Similarly, Cr level, which is higher in early-aged ADHD patients, is thought to decrease relatively at the same rate due to a single dose of 10 mg MPH in each age group, but it is a possible finding that it is still higher after MPH. It is speculated that the increase in Cr levels after MPH treatment as in the current study, may be resulting from the normalization of cerebral blood flow and glucose metabolism following psychostimulant administration in ADHD.4 At the same time, in studies evaluating MRS findings, it is stated that the findings about Cr level are contradictory and show less reliability.23
In another meta-analysis, researchers found an increase in the Cho signal in the striatum of children with ADHD and the bilateral pregenual ACC of adults with ADHD.3,24 Similarly, in a meta-analysis including both child and adult ADHD patients, significant changes of Cho levels in the right frontal lobe and left striatum were observed in children and the variations in Cho levels were significant in the left and right ACC in adults.24 Before MPH treatment, in the striatum region, Cho levels of the patients in the 18–24 years age were significantly higher than that of 25–30 years age group. The fact that Cho, which is one of the indicators of cell destruction, is high at early ages, and that ADHD symptoms and neuronal damage are more severe at that age, suggests that it may be associated with a decrease in symptoms and/or severity in adulthood.
Contrary to these studies reporting variations in the brain metabolites, another study showed no significant difference in NAA, Cho and Cr concentration compared to the healthy control group which may be due to the study patients using distinct medication protocols.25 In line with this study, a double-blind, placebo-controlled MRS study among adult ADHD patients documented that 12-week MPH treatment did not significantly affect Cr, Cho or NAA levels in the cerebellar hemisphere and ACC.11
The heterogeneity and conflict in the results of the ADHD studies concerning brain metabolites might be related to many varying factors in the patient populations such as being different ages, using different medications, being in different subtypes of ADHD, and having comorbidities. In addition, some other studies are claiming that genetic diversity in ADHD patients can also influence the levels of brain metabolites in specific regions. In a study among patients with ADHD, after MPH treatment, there were significant differences in the NAA, Cho, and Cr levels in different genotype carriers suggesting that polymorphisms of the catechol-O-methyltransferase gene in ADHD patients can explain individual differences in neurochemical responses to MPH.26 Another study by the current group concerning genetic polymorphism in ADHD patients reported that patients with the 10/10 genotype DAT1 gene showed increased Cr levels after MPH uptake in the cerebellum and in patients with the SNAP-25 Mnll polymorphism G/G genotype and Ddel polymorphism T/T genotype, NAA levels were significantly increased after MPH treatment compared with pretreatment levels in the ACC.27,28
There are several limitations of the current study. Lack of control groups, the inevitable effects of other stimulants on the patients such as smoking, low-filed MR imaging and the unilateral area evaluating can be considered as limitations. This is the first study to investigate brain metabolites from the age-related effects of MPH perspective in ADHD.
Conclusion
The current study findings show that there might be an association between age groups and dynamics of brain metabolites before/after MPH treatment in adult ADHD patients which supports the literature on neuro-metabolite associations with ADHD symptoms. In this study, after MPH treatment, both the 18–24 age group (in the DLPFC) and the 25–30 age group (in the cerebellum) was detected significantly higher NAA levels compared to pre-treatment levels. This increase in NAA levels suggested that pharmacotherapy, especially at early ages, may be effective on neuronal damage. Although the research field of ADHD is rapidly developing, it is still mostly focused on pediatric patients. Further developments may lead to novel strategies in spectroscopic investigations of ADHD and further studies focusing on specific brain regions in the course of different age groups may help better clinical understanding of ADHD.
Abbreviations
ADHD, attention deficit hyperactivity disorder; PFC, prefrontal cortex; MRS, Magnetic resonance spectroscopy; NAA, N-acetyl aspartate; Cr, creatine; Cho, Choline; MPH, Methylphenidate; DLPFC, dorsolateral prefrontal cortex; ACC, anterior cingulate cortex; DSM-IV, Diagnostic and Statistical Manual for Mental Disorders; WURS, Wender Utah Rating Scale.
Data Sharing Statement
The data associated with the paper are available from the corresponding author upon reasonable request.
Ethics Approval
The study was conducted in line with the principles of the Declaration of Helsinki and approved by the Ethics Committee of Faculty of Medicine, Pamukkale University (date:25/03/2011 approval number:52). All patients included in the study provided written informed consent.
Acknowledgments
We thank to Dr. Yilmaz Kiroglu, MSc, for their consultancy in radiology and Dr. Hande Senol, MD, for their consultancy in biostatistics.
Author Contributions
Gonca Ayse Unal and Ayse Nur Inci Kenar made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Funding was provided by the Commission of Scientific Research Project, Pamukkale University.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Valera EM, Faraone SV, Murray KE, et al. Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007;61(12):1361–1369. doi:10.1016/j.biopsych.2006.06.011
2. Guney E, Senol S, Sener S. Neuroimaging methods in attention deficit hyperactivity disorder. Klinik Psikiyatri. 2008;11:84–94. Turkish.
3. Endres D, Tebartz van Elst L, Maier SJ, et al. Neurochemical sex differences in adult ADHD patients: an MRS study. Biol Sex Differ. 2019;29:10.
4. Aoki Y, Inokuchi R, Suwa H, et al. Age-related change of neurochemical abnormality in attention-deficit hyperactivity disorder: a meta-analysis. Neurosci Biobehav Rev. 2013;37(8):1692–1701. doi:10.1016/j.neubiorev.2013.04.019
5. Perlov E, Philipsen A, Hesslinger B, et al. Reduced cingulate glutamate/glutamine-to-creatine ratios in adult patients with attention deficit/hyperactivity disorder – a magnet resonance spectroscopy study. J Psychiatry Res. 2007;41(11):934–941. doi:10.1016/j.jpsychires.2006.12.007
6. Perlov E, Tebartz van Elst L, Buechert M, et al. H1-MR-spectroscopy of cerebellum in adult attention deficit/hyperactivity disorder. J Psychiatry Res. 2010;44(14):938–943. doi:10.1016/j.jpsychires.2010.02.016
7. Rüsch N, Boeker M, Büchert M, et al. Neurochemical alterations in women with borderline personality disorder and comorbid attention-deficit hyperactivity disorder. World J Biol Psychiatry. 2010;11(2–2):372–381. doi:10.3109/15622970801958331
8. Ferreira PEMS, Palmini A, Bau CHD, et al. Differentiating attention deficit/hyperactivity disorder inattentive and combined types: a (1)H-magnetic resonance spectroscopy study of fronto-striato-thalamic regions. J Neural Transm. 2009;116(5):623–629. doi:10.1007/s00702-009-0191-3
9. Colla M, Ende G, Alm B, et al. Cognitive MR spectroscopy of anterior cingulate cortex in ADHD: elevated choline signal correlates with slowed hit reaction times. J Psychiatry Res. 2008;42(7):587–595. doi:10.1016/j.jpsychires.2007.06.006
10. Swanson JM, Kinsbourne M, Nigg J, et al. Etiologic subtypes of attention-deficit/hyperactivity disorder: brain imaging, molecular genetics and environmental factors and the dopamine hypothesis. Neuropsychol Rev. 2007;17(1):39–59. doi:10.1007/s11065-007-9019-9
11. Maier S, Tebartz van Elst L, Philipsen A, et al. Effects of 12-week methylphenidate treatment on neurometabolism in adult patients with ADHD: the first double-blind placebo-controlled MR Spectroscopy Study. J Clin Med. 2020;9(8):2601. doi:10.3390/jcm9082601
12. Kronenberg G, Ende G, Alm B, et al. Increased NAA and reduced choline levels in the anterior cingulum following chronic methylphenidate. Eur Arch Psychiatry Clin Neurosci. 2008;258(7):446–450. doi:10.1007/s00406-008-0810-2
13. Inci Kenar AN, Unal GA, Kiroglu Y, et al. Effects of methylphenidate treatment on the cerebellum in adult attention-deficit hyperactivity disorder: a magnetic resonance spectroscopy study. Eur Rev Med Pharmacol Sci. 2017;21(2):383–388.
14. Solleveld MM, Schrantee A, Puts NAJ, et al. Age-dependent, lasting effects of methylphenidate on the GABAergic system of ADHD patients. Neuroimage Clin. 2017;15:812–818. doi:10.1016/j.nicl.2017.06.003
15. Unal GA, Inci Kenar AN, Herken H, et al. Association of adult attention deficit hyperactivity disorder subtypes and response to methylphenidate HCL treatment: a magnetic resonance spectroscopy study. Neurosci Lett. 2015;604:188–192. doi:10.1016/j.neulet.2015.08.006
16. Oncu B, Olmez S, Sentürk V. Validity and reliability of the Turkish version of the Wender Utah Rating Scale for attention-deficit/hyperactivity disorders in adults. Türk Psikiyatri Derg. 2005;16(4):252–259. Turkish.
17. Gunay S, Savran C, Aksoy UM, et al. The Norm Study, transliteral equivalence, validity, reliability of adult hyperactivity scale in Turkish adult population. Türkiye’de Psikiyatri. 2006;8:98–107. Turkish.
18. Hesslinger B, Thiel T, Tebartz van Elst L, et al. Attention-deficit disorder in adults with or without hyperactivity: where is the difference? A study in humans using short echo (1)H-magnetic resonance spectroscopy. Neurosci Lett. 2001;304(1–2):117–119. doi:10.1016/S0304-3940(01)01730-X
19. Ende G, Braus DF, Walter S, et al. Effects of age, medication, and illness duration on the N-acetylaspartate signal of the anterior cingulate region in schizophrenia. Schizophr Res. 2000;41(3):389–395. doi:10.1016/S0920-9964(99)00089-4
20. Bertolino A, Callicott JH, Mattay VS, et al. The effect of treatment with antipsychotic drugs on brain N-acetylaspartate measures in patients with schizophrenia. Biol Psychiatry. 2001;49(1):39–46. doi:10.1016/S0006-3223(00)00997-5
21. Karatag O. İntrakraniyal yer kaplayıcı lezyonların ayırıcı tanısında MR spektroskopinin yeri. Şişli Etfal Eğitim Araştırma Hastanesi, Radyoloji Kliniği, Tez çalışması, İstanbul [The role of magnetic resonance spectroscopy in differential diagnosis of intracranial space occupying lesions. Şişli Etfal Training and Education Hospital, Clinic Of Radiology, Candidate’s Thesis, Istanbul]; 2005. Turkish.
22. Lee JS, Kim BN, Kang E, et al. Regional cerebral blood flow in children with attention deficit hyperactivity disorder: comparison before and after methylphenidate treatment. Human Brain Mapp. 2005;24(3):157–164. doi:10.1002/hbm.20067
23. Port JD, Agarwal N. MR spectroscopy in schizophrenia. J Magn Reson Imagin. 2011;34(6):1251–1261. doi:10.1002/jmri.22787
24. Perlov E, Philipsen A, Matthies S, et al. Spectroscopic findings in attention-deficit/hyperactivity disorder: review and meta-analysis. World J Biol Psychiatry. 2009;10(4–2):355–365. doi:10.1080/15622970802176032
25. Yeo RA, Hill DE, Campbell RA, et al. Proton magnetic resonance spectroscopy investiga- tion of the right frontal lobe in children with attention-deficit/ hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2003;42(3):303–310. doi:10.1097/00004583-200303000-00010
26. Ozturk O, Alacam H, Basay BK, et al. The effect of single dose methylphenidate on neurometabolites according to COMT gene Val158Met polymorphism in the patient with attention deficit hyperactivity disorder: a study using magnetic resonance spectroscopy. Clin Psychopharmacol Neurosci. 2016;14(2):184–193. doi:10.9758/cpn.2016.14.2.184
27. Inci Kenar AN, Unal GA, Guler H, et al. Relationship between the DAT1 gene and the effects of methylphenidate administration in adult attention deficit hyperactivity disorder: a magnetic resonance spectroscopy study. Eur Rev Med Pharmacol Sci. 2016;20(7):1373–1378.
28. Unal GA, Inci Kenar AN, Tepeli E, et al. Relationship between the SNAP-25 gene and the effects of methylphenidate on the anterior cingulate cortex of patients with adult attention deficit hyperactivity disorder: a magnetic resonance spectroscopy study. Eur Rev Med Pharmacol Sci. 2016;20(11):2443–2449.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
