Back to Journals » International Journal of General Medicine » Volume 14
Association of Admission Blood Glucose Level with All-Cause Mortality According to Age in Patients with Community Acquired Pneumonia
Authors Shen Y, Xu X, Meng S, Qin M, Li H, Chu D, Zheng C
Received 1 August 2021
Accepted for publication 27 September 2021
Published 6 November 2021 Volume 2021:14 Pages 7775—7781
DOI https://doi.org/10.2147/IJGM.S331082
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yejing Shen,1,2 Xiaowen Xu,2 Siming Meng,2 Meng Qin,2 Hailing Li,2 Dejie Chu,1 Cuixia Zheng2
1Department of Respiratory Medicine, Shanghai Eighth People’s Hospital, Shanghai, 200235, People’s Republic of China; 2Department of Respiratory Medicine, Yangpu Hospital Affiliated to Tongji University, Shanghai, 200090, People’s Republic of China
Correspondence: Dejie Chu
Department of Respiratory Medicine, Shanghai Eighth People’s Hospital, 8 Caobao Road, Shanghai, 200235, People’s Republic of China
Email [email protected]
Cuixia Zheng
Department of Respiratory Medicine, Yangpu Hospital Affiliated to Tongji University, 450 Tengyue Road, Shanghai, 200090, People’s Republic of China
Email [email protected]
Objective: To assess the impact of blood glucose levels on the prognosis of patients with community-acquired pneumonia (CAP) who were elderly or middle-aged.
Methods: From January 1, 2018, to December 31, 2020, patients with CAP (≥ 45 years) were retrospectively enrolled in this observational study. They were stratified by age (45– 64 or ≥ 65 years) and blood glucose level (≥ 11.1 or < 11.1 mmol/l). The effect of admission blood glucose on 28-day mortality was assessed with the Cox proportional hazards model, adjusted for demographic factors and comorbidity.
Results: Among 1656 patients with CAP, increased blood glucose (HR=2.08, 95% CI: 1.38– 3.49; P< 0.01) and advanced age (HR=2.76, 95% CI: 1.65– 3.77; P< 0.01) were significantly associated with a higher risk of 28-day mortality, after controlling for potential confounding factors. The strength of the association of blood glucose level with 28-day mortality decreased with age (P=0.01 for the interaction) as the adjusted HRs for death were 4.48 (95% CI: 1.40– 13.65; P< 0.01) for middle-age patients 45– 64 years and 1.52 (95% CI: 1.09– 2.17; P=0.05) for elderly patients ≥ 65 years.
Conclusion: The association of blood glucose level upon admission for CAP with all-cause mortality was stronger at younger ages.
Keywords: age, community-acquired pneumonia, hyperglycemia, mortality, prognosis
Introduction
Community-acquired pneumonia (CAP) is a common respiratory disease that causes significant morbidity and mortality throughout the world.1,2 The incidence rate of CAP for the overall population is 7.13/1000 person-years in China, which appears to increase in an age-dependent manner from 2.40/1000 person-years for younger individuals (18–30 years) to 14.98/1000 person-years for oldest-old subjects (≥ 80 years).3
Hyperglycemia was reported to be independently associated with worsened clinical outcomes in patients with respiratory diseases such as chronic obstructive pulmonary disease (COPD), asthma, and respiratory failure.4 Recently, the association of admission blood glucose level with the prognosis of CAP has also been evaluated. Lepper et al5 summarized evidence from several large CAP cohorts (including patients with and without COVID-19) from different geographical regions and ethnic groups, strongly suggesting that individuals with elevated blood glucose levels required special attention as they represented a group at high risk for increased mortality. However, it is still unclear whether the impact of hyperglycemia is different across various age groups.
This study aims to compare the predictive value of blood glucose levels in elderly patients and middle-aged patients with CAP.
Methods
The study population was inpatients (≥ 45 years) with a confirmed diagnosis of CAP at the Yangpu Hospital Affiliated to Tongji University from Jan. 1, 2018, to Dec. 31, 2020. The inclusion and exclusion criteria were described in Table 1.
 |
Table 1 Inclusion and Exclusion Criteria |
Baseline demographics (age, gender, and smoking status), comorbidities (ischemic heart disease, malignancy, kidney disease, diabetes mellitus, cerebrovascular disease, congestive heart failure, asthma, chronic obstructive pulmonary disease, bronchiectasis, and chronic liver diseases), physical examination (altered mental status, tachycardia, respiratory rate, systolic blood pressure, and temperature), laboratory test results (blood glucose, blood urea nitrogen, hematocrit, hypoxemia, and arterial pH), chest radiography findings (pleural effusion), and etiology at admission were collected from patients’ medical records. Individuals should be fasting until the glucose test is being performed. The severity of illness within 24 h after admission was determined using the CURB-65 scoring system.6
Continuous data are presented as means ± standard deviations (SDs) and compared using the unpaired t-test, categorical data are presented as numbers and percentages and compared using the chi-square test. Kaplan-Meier curves were generated for each age and blood glucose group to examine the probabilities of 28-day mortality and compared by the Log rank test. Univariate associated factors from Table 2 were offered for backward stepwise multivariable analysis with entry and exclusion limits at 0.05 and 0.10, respectively. Multivariate Cox proportional-hazards regression was employed to calculate the hazard ratio (HR) for mortality and 95% confidence interval (CI), after controlling for potential confounding factors. The interaction between age groups and blood glucose levels was also tested for significance. A P value<0.05 was considered significant. The analyses were performed with the use of SPSS software v. 20.0 (IBM Corp., Armonk, NY).
 |
Table 2 Demographic and Clinical Characteristics at Admission |
Results
A total of 1656 subjects diagnosed with CAP aged≥ 45 years were enrolled in this study, including 592 middle-aged subjects aged 45–64 years and 1064 elderly subjects aged ≥ 65 yrs. Patients’ demographics are displayed in Table 2. Most of the evaluated comorbidities (cerebrovascular disease, kidney disease, diabetes mellitus, congestive heart failure, ischemic heart disease, and chronic obstructive pulmonary disease) and several clinical presentations and laboratory test results (altered mental status, abnormal blood urea nitrogen, and abnormal hematocrit levels) were less common among middle-age patients (P<0.01). The proportion of patients with an elevated blood glucose≥11.1 mmol/L was 51.6% in those with known diabetes mellitus on admission.
The total 28-day mortality rate among all patients with CAP was 11.2%, while the numbers in middle-aged and elderly subjects were 5.6% and 14.3%, respectively. Figure 1 displayed the Kaplan–Meier curves categorized by blood glucose level and age. Figure 1A showed that patients with higher blood glucose levels had a lower event-free survival rate than those with lower blood glucose levels (HR=2.36, 95% CI: 1.46–3.82; P<0.01). Figure 1B indicated that elderly patients had a lower chance of survival (HR=2.41, 95% CI: 1.82–3.20; P<0.01). Higher blood glucose levels were associated with worse event-free survival in both middle-aged (Figure 1C, HR=4.28, 95% CI: 1.31–14.03; P<0.01) and elderly (Figure 1D, HR=1.73, 95% CI: 1.03–2.91; P=0.04) patients.
Univariate analyses (Table 3) indicated that age, gender, malignancy, kidney disease, diabetes mellitus, congestive heart failure, asthma, altered mental status, tachycardia, respiratory rate, systolic blood pressure, blood urea nitrogen, hypoxemia, arterial pH, pleural effusion, CURB-65, and ICU admission were significantly associated with the 28-day mortality (all P<0.05). Multivariate Cox proportional-hazards regression analyses showed that both blood glucose level (HR=2.08, 95% CI: 1.38–3.49; P<0.01) and age (HR=2.76, 95% CI: 1.65–3.77; P<0.01) were significantly associated with a higher risk of mortality in all patients, after controlling for potential confounder factors including gender, malignancy, kidney disease, diabetes mellitus, congestive heart failure, asthma, altered mental status, tachycardia, respiratory rate, systolic blood pressure, blood urea nitrogen, hypoxemia, arterial pH, pleural effusion, CURB-65, and ICU admission (Table 4). In the stratified analysis, the association of blood glucose level and mortality was demonstrated to be statistically significant in both middle-age (HR=4.48, 95% CI: 1.40–13.65; P<0.01) and elderly patients (HR=1.52, 95% CI: 1.09–2.17; P=0.05); however, the effect of blood glucose appeared to be more pronounced among middle-aged patients than among elderly patients (P=0.01 for the interaction).
 |
Table 3 Univariate Analysis of Risk Factors for 28-Day Mortality in Patients with Community-Acquired Pneumonia (CAP) |
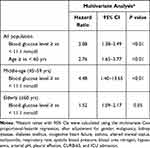 |
Table 4 Multivariate Analysis for Evaluating the Association of Blood Glucose Level and Age with 28-Day Mortality in Patients with Community Acquired Pneumonia (CAP) |
Discussion
Our research outcomes confirm the positive association of admission blood glucose and mortality in subjects with CAP. Moreover, the strength of the association decreased with age (P=0.01 for the interaction) as the adjusted hazard ratios for 28-day mortality were 4.48 (95% CI: 1.40–13.65) in patients aged 45–64 years and 1.52 (95% CI: 1.09–2.17) in patients aged above ≥65 years.
People with an increased blood glucose level face a greater risk of infections.7 However, the biological mechanism was not elaborated. It is argued that a hyperglycemic environment may impair the function of neutrophils and monocytes and increase susceptibility to certain organisms.8,9 A Danish retrospective study involving 1318 adult CAP patients reported that in subjects without diabetes metabolism, a higher blood glucose level was an independent predictor for intensive care unit (ICU) admission (OR=1.25, 95% CI 1.13–1.39).10 Multivariate logistic regression analysis in a Chinese retrospective study showed that a higher admission blood glucose level was significantly associated with the 30-day all-cause mortality (OR=1.91, 95% CI: 1.746–2.082; P <0.001) and cardiac mortality (OR=1.97, 95% CI: 1.774–2.191; P<0.001) after adjusting for potential confounding factors.11 Consistent with previous studies, our results confirmed that an elevated admission blood glucose level was significantly associated with a higher risk of all-cause mortality in patients with CAP.
The most important finding of this study is that the association between CAP and short-term mortality was stronger at younger ages. A Mexico study involving 757,210 patients with COVID-19 indicated that the risk of death associated with diabetes decreased with age. The hazard ratio for death was 3.12 (95% CI: 2.86–3.40) for patients aged 20–39 years, 2.33 (95% CI: 2.22–2.44) for patients aged 40–49 years, 1.74 (95% CI: 1.68–1.79) for patients aged 50–59 years, 1.41 (95% CI: 1.37–1.45) for patients aged 60–69 years, 1.20 (95% CI: 1.17–1.24) for patients aged 70–79 years, and 1.11 (95% CI: 1.06–1.16) for patients aged 80 years or older (trend test: P=0.004).12 Their outcomes were similar to our findings. However, the mechanism behind the weaker association of blood glucose and CAP-related mortality in older subjects was not clear. Several pre-existing comorbidities were less likely to be identified or reported in the older population, which may attenuate the association of blood glucose with mortality in these patients. In addition, ageing is associated with a progressively weakened immune system and decreased lung performance. In line with previous studies,13,14 our results indicate that age is one of the strongest independent predictors of mortality in patients with pneumonia. Thus, it is assumed that elevated blood glucose may not further increase the risk of death in older patients as they are already at very high risk.
There are some limitations in the present study. As a retrospective study, it is not possible to conclude any causal inference between blood glucose and clinical outcome as some residual confounding may not be captured. In addition, the variations in serum glucose during the hospitalization were not measured. The potential risk of mortality caused by hyperglycemia might be underestimated as patients with a higher blood glucose level may have received antihyperglycemic treatments.
Conclusions
In conclusion, our study indicated that an increased blood glucose level at admission was significantly associated with an elevated risk of 28-day mortality in patients with CAP, and the association was stronger at younger ages.
Data Sharing Statement
All data accessed complied with relevant data protection and privacy regulations. Data are available on reasonable request from the corresponding authors.
Ethics Approval and Informed Consent
All procedures were conducted according to the ethical standards of the Institutional Review Board of Yangpu Hospital Affiliated to Tongji University and the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consents were waived by Institutional Review Board of Yangpu Hospital Affiliated to Tongji University as it is a retrospective observational study.
Disclosure
The authors declare that there is no conflict of interest.
References
1. Shoar S, Musher DM. Etiology of community-acquired pneumonia in adults: a systematic review. Pneumonia. 2020;12:11. PubMed PMID: 33024653; PubMed Central PMCID: PMCPMC7533148. doi:10.1186/s41479-020-00074-3
2. McLaughlin JM, Khan FL, Thoburn EA, et al. Rates of hospitalization for community-acquired pneumonia among US adults: a systematic review. Vaccine. 2020;38(4):741–751. PubMed PMID: 31843272. doi:10.1016/j.vaccine.2019.10.101
3. Sun Y, Li H, Pei Z, et al. Incidence of community-acquired pneumonia in urban China: a national population-based study. Vaccine. 2020;38(52):8362–8370. PubMed PMID: 33199077. doi:10.1016/j.vaccine.2020.11.004
4. Liu SP, Zhang Q, Wang W, et al. Hyperglycemia is a strong predictor of poor prognosis in COVID-19. Diabetes Res Clin Pract. 2020;167:108338. PubMed PMID: 32712122; PubMed Central PMCID: PMCPMC7377976. doi:10.1016/j.diabres.2020.108338
5. Lepper PM, Bals R, Juni P, et al. Blood glucose, diabetes and metabolic control in patients with community-acquired pneumonia. Diabetologia. 2020;63(11):2488–2490. PubMed PMID: 32676817; PubMed Central PMCID: PMCPMC7366469. doi:10.1007/s00125-020-05225-1
6. Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. PubMed PMID: 12728155; PubMed Central PMCID: PMCPMC1746657. doi:10.1136/thorax.58.5.377
7. Abu-Ashour W, Twells L, Valcour J, et al. The association between diabetes mellitus and incident infections: a systematic review and meta-analysis of observational studies. BMJ Open Diabetes Res Care. 2017;5(1):e000336. PubMed PMID: 28761647; PubMed Central PMCID: PMCPMC5530269. doi:10.1136/bmjdrc-2016-000336
8. Insuela DBR, Ferrero MR, Goncalves-de-Albuquerque CF, et al. Glucagon reduces neutrophil migration and increases susceptibility to sepsis in diabetic mice. Front Immunol. 2021;12:633540. PubMed PMID: 34295325; PubMed Central PMCID: PMCPMC8290340. doi:10.3389/fimmu.2021.633540
9. Johnson J, Jaggers RM, Sreejit G, et al. Oxidative stress in neutrophils: implications for diabetic cardiovascular complications. Antioxid Redox Signal. 2021. PubMed PMID: 34148367. doi:10.1089/ars.2021.0116
10. Jensen AV, Egelund GB, Andersen SB, et al. The impact of blood glucose on community-acquired pneumonia: a retrospective cohort study. ERJ Open Res. 2017;3(2):00114–2016. PubMed PMID: 28656133; PubMed Central PMCID: PMCPMC5478863. doi:10.1183/23120541.00114-2016
11. Ma J, He L, Wang X, et al. Relationship between admission blood glucose level and prognosis in elderly patients without previously known diabetes who undergo emergency non-cardiac surgery. Intern Emerg Med. 2015;10(5):561–566. PubMed PMID: 25616429. doi:10.1007/s11739-015-1191-y
12. Woolcott OO, Castilla-Bancayan JP. The effect of age on the association between diabetes and mortality in adult patients with COVID-19 in Mexico. Sci Rep. 2021;11(1):8386. PubMed PMID: 33863997; PubMed Central PMCID: PMCPMC8052362. doi:10.1038/s41598-021-88014-z
13. Ruiz LA, Espana PP, Gomez A, et al. Age-related differences in management and outcomes in hospitalized healthy and well-functioning bacteremic pneumococcal pneumonia patients: a cohort study. BMC Geriatr. 2017;17(1):130. PubMed PMID: 28633626; PubMed Central PMCID: PMCPMC5477680. doi:10.1186/s12877-017-0518-0
14. Han X, Zhou F, Li H, et al. Effects of age, comorbidity and adherence to current antimicrobial guidelines on mortality in hospitalized elderly patients with community-acquired pneumonia. BMC Infect Dis. 2018;18(1):192. PubMed PMID: 29699493; PubMed Central PMCID: PMCPMC5922029. doi:10.1186/s12879-018-3098-5
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

