Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 10 » Issue 1
Association between vitamin D receptor polymorphisms and osteoporosis in patients with COPD
Authors Kim SW , Lee J, Ha JH, Kang HH, Rhee CK, Kim JW, Moon HS, Baek KH , Lee SH
Received 4 July 2015
Accepted for publication 5 August 2015
Published 4 September 2015 Volume 2015:10(1) Pages 1809—1817
DOI https://doi.org/10.2147/COPD.S91576
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Sei Won Kim,1 Jong Min Lee,1 Jick Hwan Ha,1 Hyeon Hui Kang,1 Chin Kook Rhee,1 Jin Woo Kim,1 Hwa Sik Moon,1 Ki Hyun Baek,2 Sang Haak Lee1
1Division of Pulmonology, Critical Care and Sleep Medicine, 2Division of Endocrinology and Metabolism, Department of Internal Medicine, St Paul’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
Background: Patients with COPD are at an increased risk of osteoporosis. Although many studies have addressed the relationship between the vitamin D receptor (VDR) polymorphisms and bone health, this relationship has not been fully investigated in patients with COPD. In this study, we investigated the association of VDR polymorphisms with bone mineral density (BMD) and other clinical parameters in patients with COPD.
Patients and methods: In total, 200 patients with COPD were included in this study. The VDR polymorphisms rs1544410 (A/G-BsmI), rs7975232 (A/C-ApaI), rs731236 (C/T-TaqI), and rs10735810 (C/T-FokI) were determined by Sanger sequencing using blood DNA samples. BMD of the lumbar vertebra and the femoral neck was measured by dual-energy X-ray absorptiometry. Other clinical parameters were also evaluated. Haplotype and multivariate analyses were also performed.
Results: Sex, body mass index, steroid use, percentage of forced expiratory volume in 1 second (FEV1), alkaline phosphatase, and 25-hydroxyvitamin D significantly influenced the risk of osteoporosis. Patients with osteoporosis were more likely to carry the rs7975232 C allele compared to normal patients with BMD. Haplotypes GCT and GAT were related to osteoporosis. Patients without the haplotype GAT allele showed a significantly lower T-score at the femoral neck and an increased risk of osteoporosis (odds ratio [OR]= 2.78, 95% confidence interval [CI]= 1.20–6.48, P=0.018) compared with carriers in the dominant model.
Conclusion: Genetic variations in VDR are significantly associated with osteoporosis among patients with COPD. Further studies are required to confirm the role of the VDR polymorphisms in osteoporosis among patients with COPD.
Keywords: chronic obstructive pulmonary disease, osteoporosis, vitamin D receptor gene, polymorphism, haplotype
Introduction
COPD is a major cause of chronic morbidity and mortality worldwide.1 Predictions from the Global initiative for chronic Obstructive Lung Disease (GOLD) indicate that COPD will rise from the sixth to the third highest mortality rate by 2020 worldwide.2 Additionally, with aging populations, the burden of COPD has been consistently increasing.3 Although COPD is primarily a pulmonary disease, it has been linked to many extra-pulmonary comorbidities, leading to a significant burden of disease.4,5
Osteoporosis is a systemic skeletal disease characterized by low bone mineral density (BMD) and microarchitectural deterioration of the bone, leading to increased fragility and a high risk of fracture.6 COPD and osteoporosis are strongly related because of common risk factors, such as age, smoking, inactivity, vitamin D deficiency, and the use of systemic corticosteroids.7–10 In patients with COPD, the prevalence of osteoporosis is approximately two to five times higher than that in the same age group without airflow limitation.8 However, our ability to predict the occurrence of osteoporosis in patients with COPD is still limited.
In general population studies, genetic factors are often suggested as potential risk factors for osteoporosis.11 Among the multiple candidate genes investigated in osteoporosis, the vitamin D receptor (VDR) was the first,12 and it has been actively discussed in other studies.11,13–15 The VDR gene has four polymorphisms (rs1544410, rs7975232, rs731236, and rs10735810) that are most frequently studied in considering the association of BMD with osteoporosis.6,16–19 Although many studies have investigated the association between VDR polymorphisms and bone health, the results were conflicting. This may be due to heterogeneous study populations, small sample size, different ethnicities, and environmental factors. To find the association of VDR polymorphisms with BMD and other clinical parameters in patients with COPD, we narrowed the study population to stable Korean patients with COPD, and the factors that could affect bone metabolism were investigated and controlled. This is the first study of VDR gene polymorphism and osteoporosis in patients with COPD.
Patients and methods
Study participants
In total, 200 patients at St Paul’s Hospital who were diagnosed with COPD using the post-bronchodilator pulmonary function test were included in this prospective study. COPD was diagnosed according to the guidelines of the American Thoracic Society/European Respiratory Society20 and categorized in accordance with the Global initiative for chronic Obstructive Lung Disease guidelines.21 The inclusion criteria were 1) men over 50 years old and postmenopausal women and 2) patients who had a pulmonary function test and dual energy X-ray absorptiometry (DEXA) 3 months before or after registration. The exclusion criteria were subjects who had 1) an acute exacerbation within 6 weeks of registration; 2) other active pulmonary or infectious diseases; 3) any other diseases that could affect bone metabolism, such as hyperthyroidism, parathyroid disease, diabetes mellitus, malignancy, chronic kidney disease, connective tissue disease, pituitary disease, and adrenal disease; 4) history of using vitamin D, calcium, or bisphosphonate; 5) steroid use for diseases other than COPD and; 6) walking difficulty more than 1 month before DEXA. Patients were enrolled from January 2012 to January 2014. This study was approved by the institutional review board of St Paul’s Hospital. All patients provided written informed consent before study registration.
Clinical measurements
Demographic information, sex, age, body mass index (BMI), and smoking history were collected. The enrolled patients’ cumulative alcohol and steroid dose were taken from medical records or interviews. Cumulative steroid dose was calculated from COPD diagnosis to study registration. Oral and intravenous steroid dose were combined to give a prednisolone equivalent dosage, and the inhaled steroid dose was assessed to give a budesonide equivalent dosage. Pulmonary function tests were performed using a SensorMedics Vmax 229 (VIASYS Healthcare, Yorba Linda, CA, USA). Biochemical parameters related to bone metabolism, such as calcium, phosphorus, alkaline phosphatase (ALP), 25-hydroxyvitamin D (25(OH)D), and parathyroid hormone were measured.
BMD measurement
BMD (amount of mineral matter per square centimeter of bones) is used as an indirect indicator of osteoporosis and fracture risk. BMD was measured by DEXA using a DPX Bravo (GE Healthcare, Milwaukee, WI, USA) at the lumbar spine and the femoral neck. For the lumbar BMD evaluation, we used the average value for lumbar vertebrae 1–4 (L1–L4), excluding any vertebral fractures, degenerative changes, and calcifications. We classified the subjects into three groups based on the World Health Organization criteria: normal, osteopenia, and osteoporosis. Osteoporosis was defined as a T-score of −2.5 or less, osteopenia was defined as a T-score between −2.5 and −1.0, and normal was defined as a T-score of −1.0 or higher.22
Genotyping
Genomic DNA was extracted from peripheral blood using the Puregene DNA isolation kit (Gentra Systems, Minneapolis, MN, USA). Molecular genetic studies were performed by BIOFACT© (Daejeon, South Korea). PCR/DNA sequencing was used to determine the genotype of four single-nucleotide polymorphisms (SNPs) in the VDR gene. Primer information for each SNP is given in Table S1. Briefly, the region of the VDR gene that encompasses each SNP was amplified by PCR using purified genomic DNA. The DNA amplicons were sequenced using the same PCR primers with the Big Dye Terminator v3.1 Cycle Sequencing Kit (Thermo Fisher Scientific, Waltham, MA, USA). The products were cleaned with the Big Dye XTerminator Purification Kit (Thermo Fisher Scientific) and resolved with the ABI 3730xl Genetic Analyzer (Thermo Fisher Scientific). The data were analyzed using the ABI Data Collection software v3.0 (Thermo Fisher Scientific), Sequencing Analysis software v5.4 (Thermo Fisher Scientific), and SeqScape software v2.6 (Thermo Fisher Scientific).
Statistical analysis
Means and standard deviation were computed for normally distributed continuous variables, whereas medians and interquartile ranges (25th–75th) were used for non-normally distributed continuous data. Categorical data were described as numbers and percentages. For the genotype distribution, the Hardy–Weinberg equilibrium was tested for each SNP by the standard χ2 test. For comparison of the continuous variables between subgroups, Student’s t-test was performed for normally distributed data and Mann–Whitney U test was used for non-normally distributed data. Univariate comparison between categorical variables was made using the χ2 and Fisher’s exact tests when appropriate. The χ2 test or the Fisher’s exact test was also used to analyze the frequency of the genotype, the allele, and the haplotype. An independent t-test or analysis of variance (ANOVA) test was used to find the relationship between the genotype and the T-score. Logistic regression analysis was performed to evaluate the effects of genetic variations of VDR on osteoporosis. Statistical analyses were performed using the SAS version 9.2 (SAS Institute Inc., Cary, NC, USA) and R Statistical Programming Language version 3.1.1 (The R Foundation for Statistical Computing, Vienna, Austria). A P-value <0.05 was considered significant.
Results
Baseline characteristics of the study group
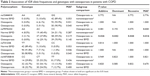
The basic characteristics of the patients are shown in Table 1. Osteoporosis was present in 27.5%, osteopenia in 49.0%, and normal BMD in 23.5% of the total patients with COPD. The osteoporosis group had significantly more women (P=0.031 and P=0.010) and a lower average BMI (P<0.001, both) compared with the nonosteoporosis (normal BMD + osteopenia group) and the normal BMD group. The osteoporosis group had significantly less alcohol history (P<0.001 and P=0.001), cumulative alcohol dose (P<0.001, both), and forced expiratory volume in 1 second (FEV1 %, P=0.001, both) compared with the nonosteoporosis or the normal BMD group. History of steroid use (P=0.037), cumulative dose of oral or intravenous steroid (P=0.028), and cumulative dose of inhaled steroid (P=0.031) were significantly higher in the osteoporosis group compared with the normal BMD group. With regard to the bone metabolic markers, the osteoporosis group showed a significantly higher ALP (P=0.003 and P<0.001) and significantly lower 25(OH)D (P=0.013 and P=0.003) compared with the nonosteoporosis and the normal BMD group.
Association of VDR allele frequencies and genotypes with osteoporosis in COPD patients
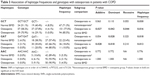
The minor allele frequency (MAF) of the rs1544410, rs7975232, rs731236, and rs10735810 polymorphisms were 0.04, 0.22, 0.05, and 0.41, respectively, in total patients with COPD. The MAF and genotype frequency of the four SNPs of the VDR gene in the subgroups are shown in Table 2. No differences were identified between the osteoporosis group and the nonosteoporosis or normal BMD groups in the MAF of rs1544410, rs731236, and rs10735810. However, the MAF of rs7975232 was significantly different between the osteoporosis group and the nonosteoporosis or normal BMD group (P=0.041 and P=0.016). All of the genotype distributions were followed using the Hardy–Weinberg equilibrium (P>0.05). Genotype distribution of the VDR rs7975232 was significantly different in the osteoporosis group compared with the normal BMD group in all models (P=0.026, P=0.042, and P=0.044 for the additive, dominant, and recessive models, respectively). No significant association between the average BMD values (T-score of femoral neck and L-spine) and SNPs in the VDR gene was found in any of the models (Table S2). There was no significant relationship between the VDR polymorphisms and the level of 25(OH)D in our study (data not shown).
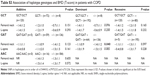
Association of haplotype frequencies and genotypes with osteoporosis in COPD patients
The pairwise linkage disequilibrium (LD) among all four polymorphisms of the VDR genes was estimated using the maximum likelihood of D (D′) and a measure of LD association (r2).23 Strong LD was observed between two SNPs in the 3′ region, rs1544410 and rs731236. The correlation coefficient r2 of rs10735810 with the other three SNPs were very low (r2=0.002–0.072); however, the r2 for rs1544410–rs731236 was 0.836, for rs1544410–rs7975232 was 0.152, and for rs7975232–rs731236 was 0.126. Therefore, we excluded rs10735810 in the haplotype analysis. Several studies have shown that the rs10735810 polymorphism has no linkage to any of the other VDR polymorphisms.24 Haplotypes, other than GCT, GAT, and AAC were excluded, as their frequency was less than 1%. Carrying the GCT haplotype was associated with osteoporosis (Table 3), as was not carrying the GAT haplotype. The BMD values (T-score of the femoral neck and the L-spine) according to haplotype genotypes are shown in Table S3. The T-score of the femoral neck was significantly lower in the subgroup that was not carrying the GAT haplotype in the dominant model (P=0.040).
Multivariate analysis of VDR genotypes and haplotypes in patients with COPD
Multivariate logistic regression analysis for osteoporosis in patients with COPD was performed. BMI, alcohol use, steroid use, FEV1 (%), ALP, and 25(OH)D were all significantly different in the osteoporosis group compared with the normal group and were therefore included as covariates. After a stepwise selection, BMI, cumulative alcohol dose, and FEV1 (%) were entered as variables into the model. In the GAT haplotype dominant model, the group without the GAT haplotype included significantly more patients with osteoporosis (odds ratio [OR] =2.783, P=0.018) compared with the group containing the GAT haplotype (Table 4). The rs7975232 recessive model (OR =2.093, P=0.057) and GCT haplotype recessive model (OR =2.117, P=0.059) showed statistically borderline results.
Discussion
Studies investigating twins and families have shown that osteoporosis has a strong genetic component, and up to 50% of the variance in BMD can be attributed to genetic factors.25,26 The VDR gene is composed of a 5′ promotor (from exon 1a to f), coding exons (exon 2–9), and a 3′ untranslated region in chromosome 12q13.1.27 Morrison et al first showed that the polymorphisms located at the 3′ end of the VDR gene, as determined by the restriction enzymes BsmI, ApaI, and TaqI, were related to BMD.12 As polymorphisms at the VDR gene locus have been suggested to be associated with bone mass, the VDR gene polymorphisms were considered important for osteoporosis.24,28
In this study, we investigated the role and influence of four VDR polymorphisms in patients with COPD: rs1544410 (A/G-BsmI), rs7975232 (A/C-ApaI), rs731236 (C/T-TaqI), and rs10735810 (C/T-FokI). The rs7975232 (A/C-ApaI), haplotype GCT, and GAT polymorphisms were related to osteoporosis in our study. Patients not carrying the GAT haplotype showed a significantly lower T-score at the femoral neck in the dominant model. Furthermore, not carrying the GAT haplotype was associated with osteoporosis in the dominant model after adjustment of confounders.
Low body weight, low FEV1, smoking, older age, female sex, inactivity, systemic inflammation, systemic corticosteroids, and vitamin D deficiency are known COPD-related risk factors for osteoporosis.8,29,30 In our study, sex, BMI, steroid use, FEV1, and vitamin D deficiency were confirmed as risk factors of osteoporosis in patients with COPD. Meanwhile, smoking was unrelated, and alcohol consumption was significantly lower in COPD patients with osteoporosis. This was mainly due to the high proportion of females in the osteoporosis group. Korean society traditionally places a taboo on women who smoke or drink. Among females in our study, there was one current, four ex-, and 15 never-smokers, compared with 51 current, 122 ex-, and seven never-smokers among the males. Additionally, all females in our study had no history of alcohol consumption, whereas 72.2% of men had a history of alcohol. Serum ALP is the most commonly used biomarker of bone formation, showing a higher value in patients with osteoporosis compared with normal subjects.31 In our study, serum ALP was significantly increased in the osteoporosis group.
Although we did not investigate the relationship between VDR polymorphism and osteoporosis in healthy population without COPD, several studies have investigated the association of the VDR gene with BMD, especially using BsmI, ApaI, TaqI, and FokI. However, the results have been inconsistent.6,28,32,33 Morita et al investigating ApaI, TaqI, and FokI found that the effect of the VDR genotype on bone mass was negligible in Japanese women.32 Several other studies reported that the VDR gene has no significant effect in BMD.11,28,33–35 However, other studies have shown a relationship between the VDR genotype and osteoporosis.13,36–40 A meta-analysis by Zintzaras et al showed that the BsmI polymorphism was more closely related to osteoporosis than were the ApaI, TaqI, and FokI polymorphisms.6 In Korea, the FokI polymorphism has been suggested as the factor associated with osteoporosis in postmenopausal women.41,42 These inconsistent results are mainly due to different study populations, insufficient sample size, different ethnicities, high allelic heterogeneity, variable LD across population groups, and environmental factors that would have confounded the underlying genetic effect.23 In our study, the patient population was selected from stable Korean patients with COPD, and the factors that could affect bone metabolism were investigated and controlled. Although direct comparisons are difficult, there are a few VDR polymorphism genotyping data in Korean healthy subjects regardless of osteoporosis diagnosis.43–47 Compared with our results, rs1544410, rs731236, and rs10735810 showed the almost similar genotype distribution in normal BMD, osteopenia, and osteoporosis group. However, rs7975232 genotype distribution showed a difference in osteoporosis group.
In this study, we performed haplotype analysis. When there are multiple polymorphisms within the same gene, information contained at each polymorphic site is “linked” to its neighbors. Therefore, inheriting one polymorphism means a high likelihood of inheriting the neighboring polymorphism.48 Compared with single SNP analysis, a haplotype study gives more information and has an advantage in disease association studies, as it gives the cumulative effect of all SNPs in that gene.23 Although there was no association between the BsmI–ApaI–TaqI haplotype and any osteoporotic type in the GENOMOS study,11,49 Thakkinstian et al reported an association between the BAT haplotype and osteoporosis (OR =4.21 [CI =2.2–8.10], P<0.001).48 Uitterlinden et al showed an association between the bAT haplotype and low BMD and subsequently, an overrepresentation of the baT haplotype among fracture cases.50 In our study, the GCT (baT) and GAT (bAT) haplotypes were related to osteoporosis. Especially, not carrying the GAT haplotype was a risk factor for osteoporosis. Taken together, the results from the haplotype analysis suggest the strong effect of rs7975232.
We are aware of the several limitations of this study. First, the sample size was not large enough to reach definitive conclusions. However, there has been no prior VDR polymorphism research in patients with COPD with osteoporosis. Repetitive, large-scale population studies are warranted in the future. Second, although the prevalence of osteoporosis is high in severe patients with COPD, most patients in this study were considered to be suffering from mild-to-moderate COPD. Many severe patients with COPD were excluded from the study due to recent acute exacerbations, comorbidities, and pulmonary infections. Third, in our study, the population was weighted toward men. Sex differences in COPD have been suggested by other studies;51,52 therefore, subgroup analysis by sex in a large population is needed. Fourth, no index representing physical activity was included in our study. Physical activity is one of the important factors in both COPD and osteoporosis. A detailed physical activity questionnaire or a 6-minute walk test is warranted in future studies.
Conclusion
Genetic variations in VDR are significantly associated with osteoporosis among patients with COPD. In this study, the rs7975232 C allele and GCT haplotype were risk factors for osteoporosis in patients with COPD. Furthermore, not carrying haplotype GAT was associated with osteoporosis prevalence and low BMD in the dominant model. Further studies are needed to confirm the role of VDR polymorphisms in osteoporosis among patients with COPD.
Acknowledgments
The authors would like to thank Jong Y Park (Department of Cancer Epidemiology, Moffitt Cancer Center, Tampa, FL, USA) for helpful discussion and Sun Hee Gang (St Paul’s Hospital, Seoul, Korea) for assistance in data collection. This study was funded by the Department of Internal Medicine, College of Medicine, The Catholic University of Korea.
Disclosure
The authors report no conflicts of interest in this work.
References
Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. | ||
Hurd S. The impact of COPD on lung health worldwide: epidemiology and incidence. Chest. 2000;117(2 Suppl):1s–4s. | ||
Tsai TY, Livneh H, Lu MC, Tsai PY, Chen PC, Sung FC. Increased risk and related factors of depression among patients with COPD: a population-based cohort study. BMC Public Health. 2013;13:976. | ||
Wouters EF. Introduction: systemic effects in chronic obstructive pulmonary disease. Eur Respir J Suppl. 2003;46:1s. | ||
May SM, Li JT. Burden of chronic obstructive pulmonary disease: healthcare costs and beyond. Allergy Asthma Proc. 2015;36(1):4–10. | ||
Zintzaras E, Rodopoulou P, Koukoulis GN. BsmI, TaqI, ApaI and FokI polymorphisms in the vitamin D receptor (VDR) gene and the risk of osteoporosis: a meta-analysis. Dis Markers. 2006;22(5–6):317–326. | ||
Romme EA, Rutten EP, Smeenk FW, Spruit MA, Menheere PP, Wouters EF. Vitamin D status is associated with bone mineral density and functional exercise capacity in patients with chronic obstructive pulmonary disease. Ann Med. 2013;45(1):91–96. | ||
Lehouck A, Boonen S, Decramer M, Janssens W. COPD, bone metabolism, and osteoporosis. Chest. 2011;139(3):648–657. | ||
Jaramillo JD, Wilson C, Stinson DJ, et al. Reduced bone density and vertebral fractures in smokers: men and COPD patients at increased risk. Ann Am Thorac Soc. 2015;12(5):648–656. | ||
Xiaomei W, Hang X, Lingling L, Xuejun L. Bone metabolism status and associated risk factors in elderly patients with chronic obstructive pulmonary disease (COPD). Cell Biochem Biophys. 2014;70(1):129–134. | ||
Uitterlinden AG, Ralston SH, Brandi ML, et al. The association between common vitamin D receptor gene variations and osteoporosis: a participant-level meta-analysis. Ann Intern Med. 2006;145(4):255–264. | ||
Morrison NA, Qi JC, Tokita A, et al. Prediction of bone density from vitamin D receptor alleles. Nature. 1994;367(6460):284–287. | ||
Cooper GS, Umbach DM. Are vitamin D receptor polymorphisms associated with bone mineral density? A meta-analysis. J Bone Miner Res. 1996;11(12):1841–1849. | ||
Boron D, Kaminski A, Kotrych D, et al. Polymorphism of vitamin D3 receptor and its relation to mineral bone density in perimenopausal women. Osteoporos Int. 2015;26(3):1045–1052. | ||
Liu YZ, Liu YJ, Recker RR, Deng HW. Molecular studies of identification of genes for osteoporosis: the 2002 update. J Endocrinol. 2003;177(2):147–196. | ||
Qin G, Dong Z, Zeng P, Liu M, Liao X. Association of vitamin D receptor BsmI gene polymorphism with risk of osteoporosis: a meta-analysis of 41 studies. Mol Biol Rep. 2013;40(1):497–506. | ||
Wang D, Liu R, Zhu H, Zhou D, Mei Q, Xu G. Vitamin D receptor Fok I polymorphism is associated with low bone mineral density in postmenopausal women: a meta-analysis focused on populations in Asian countries. Eur J Obstet Gynecol Reprod Biol. 2013;169(2):380–386. | ||
Jakubowska-Pietkiewicz E, Mlynarski W, Klich I, Fendler W, Chlebna-Sokol D. Vitamin D receptor gene variability as a factor influencing bone mineral density in pediatric patients. Mol Biol Rep. 2012;39(5):6243–6250. | ||
Mohammadi Z, Fayyazbakhsh F, Ebrahimi M, et al. Association between vitamin D receptor gene polymorphisms (Fok1 and Bsm1) and osteoporosis: a systematic review. J Diabetes Metab Disord. 2014;13(1):98. | ||
Xia Y, Guan Y, Fan L, et al. Dynamic contrast enhanced magnetic resonance perfusion imaging in high-risk smokers and smoking-related COPD: correlations with pulmonary function tests and quantitative computed tomography. COPD. 2014;11(5):510–520. | ||
Maio S, Baldacci S, Martini F, et al. COPD management according to old and new GOLD guidelines: an observational study with Italian general practitioners. Curr Med Res Opin. 2014;30(6):1033–1042. | ||
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9(8):1137–1141. | ||
Singh M, Singh P, Singh S, Juneja PK, Kaur T. Vitamin D receptor (VDR) gene polymorphism influences the risk of osteoporosis in postmenopausal women of Northwest India. Arch Osteoporos. 2013;8(1–2):147. | ||
Uitterlinden AG, Fang Y, Van Meurs JB, Pols HA, Van Leeuwen JP. Genetics and biology of vitamin D receptor polymorphisms. Gene. 2004;338(2):143–156. | ||
Pocock NA, Eisman JA, Hopper JL, Yeates MG, Sambrook PN, Eberl S. Genetic determinants of bone mass in adults. A twin study. J Clin Invest. 1987;80(3):706–710. | ||
Seeman E, Hopper JL, Young NR, Formica C, Goss P, Tsalamandris C. Do genetic factors explain associations between muscle strength, lean mass, and bone density? A twin study. Am J Physiol. 1996;270(2 Pt 1):E320–E327. | ||
Choi SK, Park MS, Song JK, Yoon KS, Yoon KL, Shim KS. Association of polymorphisms in the vitamin D receptor promoter with idiopathic short stature. J Korean Med Sci. 2013;28(9):1329–1333. | ||
Yoldemir T, Yavuz DG, Anik G, Verimli N, Erenus M. Vitamin D receptor gene polymorphisms in a group of postmenopausal Turkish women: association with bone mineral density. Climacteric. 2011;14(3):384–391. | ||
Graat-Verboom L, Wouters EF, Smeenk FW, van den Borne BE, Lunde R, Spruit MA. Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J. 2009;34(1):209–218. | ||
Chubachi S, Nakamura H, Sasaki M, et al. Polymorphism of LRP5 gene and emphysema severity are associated with osteoporosis in Japanese patients with or at risk for COPD. Respirology. 2015;20(2):286–295. | ||
Cho JH, Kim MT, Lee HK, Hong IS, Jang HC. Factor analysis of biochemical markers associated with bone mineral density in adults. J Phys Ther Sci. 2014;26(8):1225–1229. | ||
Morita A, Iki M, Dohi Y, et al. Prediction of bone mineral density from vitamin D receptor polymorphisms is uncertain in representative samples of Japanese Women. The Japanese Population-based Osteoporosis (JPOS) Study. Int J Epidemiol. 2004;33(5):979–988. | ||
Sioka C, Papakonstantinou S, Markoula S, et al. Vitamin D receptor gene polymorphisms in multiple sclerosis patients in northwest Greece. J Negat Results Biomed. 2011;10:3. | ||
Fang Y, Rivadeneira F, van Meurs JB, Pols HA, Ioannidis JP, Uitterlinden AG. Vitamin D receptor gene BsmI and TaqI polymorphisms and fracture risk: a meta-analysis. Bone. 2006;39(4):938–945. | ||
Shen H, Xie J, Lu H. Vitamin D receptor gene and risk of fracture in postmenopausal women: a meta-analysis. Climacteric. 2014;17(4):319–324. | ||
Gomez C, Naves ML, Barrios Y, et al. Vitamin D receptor gene polymorphisms, bone mass, bone loss and prevalence of vertebral fracture: differences in postmenopausal women and men. Osteoporos Int. 1999;10(3):175–182. | ||
Langdahl BL, Gravholt CH, Brixen K, Eriksen EF. Polymorphisms in the vitamin D receptor gene and bone mass, bone turnover and osteoporotic fractures. Eur J Clin Invest. 2000;30(7):608–617. | ||
Marozik P, Mosse I, Alekna V, et al. Association between polymorphisms of VDR, COL1A1, and LCT genes and bone mineral density in Belarusian women with severe postmenopausal osteoporosis. Medicina (Kaunas). 2013;49(4):177–184. | ||
Jia F, Sun RF, Li QH, et al. Vitamin D receptor BsmI polymorphism and osteoporosis risk: a meta-analysis from 26 studies. Genet Test Mol Biomarkers. 2013;17(1):30–34. | ||
Horst-Sikorska W, Dytfeld J, Wawrzyniak A, et al. Vitamin D receptor gene polymorphisms, bone mineral density and fractures in postmenopausal women with osteoporosis. Mol Biol Rep. 2013;40(1):383–390. | ||
Choi YM, Jun JK, Choe J, et al. Association of the vitamin D receptor start codon polymorphism (FokI) with bone mineral density in postmenopausal Korean women. J Hum Genet. 2000;45(5):280–283. | ||
Kim JG, Lim KS, Kim EK, Choi YM, Lee JY. Association of vitamin D receptor and estrogen receptor gene polymorphisms with bone mass in postmenopausal Korean women. Menopause. 2001;8(3):222–228. | ||
Park S, Kim EJ, Lee SH, et al. Vitamin D-receptor polymorphisms and non-tuberculous mycobacterial lung disease in Korean patients. Int J Tuberc Lung Dis. 2008;12(6):698–700. | ||
Lee CK, Hong JS, Cho YS, Yoo B, Kim GS, Moon HB. Lack of relationship between vitamin D receptor polymorphism and bone erosion in rheumatoid arthritis. J Korean Med Sci. 2001;16(2):188–192. | ||
Cheon CK, Nam HK, Lee KH, Kim SY, Song JS, Kim C. Vitamin D receptor gene polymorphisms and type 1 diabetes mellitus in a Korean population. Pediatr Int. 2015. | ||
Kang TJ, Jin SH, Yeum CE, et al. Vitamin D receptor gene TaqI, BsmI and FokI polymorphisms in Korean patients with tuberculosis. Immune Netw. 2011;11(5):253–257. | ||
Seo IY, Kang IH, Chae SC, et al. Vitamin D receptor gene Alw I, Fok I, Apa I, and Taq I polymorphisms in patients with urinary stone. Urology. 2010;75(4):923–927. | ||
Thakkinstian A, D’Este C, Attia J. Haplotype analysis of VDR gene polymorphisms: a meta-analysis. Osteoporos Int. 2004;15(9):729–734. | ||
Mencej-Bedrac S, Prezelj J, Kocjan T, et al. The combinations of polymorphisms in vitamin D receptor, osteoprotegerin and tumour necrosis factor superfamily member 11 genes are associated with bone mineral density. J Mol Endocrinol. 2009;42(3):239–247. | ||
Uitterlinden AG, Pols HA, Burger H, et al. A large-scale population-based study of the association of vitamin D receptor gene polymorphisms with bone mineral density. J Bone Miner Res. 1996;11(9):1241–1248. | ||
Sorheim IC, Johannessen A, Gulsvik A, Bakke PS, Silverman EK, DeMeo DL. Gender differences in COPD: are women more susceptible to smoking effects than men? Thorax. 2010;65(6):480–485. | ||
Papaioannou AI, Bania E, Alexopoulos EC, Mitsiki E, Malli F, Gourgoulianis KI. Sex discrepancies in COPD patients and burden of the disease in females: a nationwide study in Greece (Greek Obstructive Lung Disease Epidemiology and health ecoNomics: GOLDEN study). Int J Chron Obstruct Pulmon Dis. 2014;9:203–213. |
Supplementary materials
  | Table S1 Primers of vitamin D receptor (VDR) polymorphisms |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.