Back to Journals » Infection and Drug Resistance » Volume 16
Association Between Vitamin D Receptor Polymorphism and the Response to Helicobacter Pylori Treatment
Authors Abo-Amer YEE , Mohamed AA, Elhoseeny MM, Rezk SM, Abdel-Salam S, Alrohaimi AH, Abdelgeliel AS , Alzahrani SS, Jafri I, Alqahtani LS, Fayad E, Fakhry M, Soliman MY
Received 21 April 2023
Accepted for publication 10 June 2023
Published 8 July 2023 Volume 2023:16 Pages 4463—4469
DOI https://doi.org/10.2147/IDR.S414186
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Yousry Esam-Eldin Abo-Amer,1 Amal Ahmed Mohamed,2 Mohamed Mahmoud Elhoseeny,3 Samar M Rezk,4 Sherief Abdel-Salam,5 Abdulmohsen H Alrohaimi,6 Asmaa Sayed Abdelgeliel,7 Seham Saeed Alzahrani,8 Ibrahim Jafri,8 Leena S Alqahtani,9 Eman Fayad,8 Mohamed Fakhry,10 Moataz Yousry Soliman11
1Mahala Hepatology Teaching Hospital, Hepatology& Gastroenterology Department, Gharbia, Elgharbia, Egypt; 2National Hepatology & Tropical Medicine Research Institute, Department of Biochemistry, Cairo, Egypt; 3Department of Internal Medicine, Faculty of Medicine, Suez University, Suez, Egypt; 4Department of Clinical Nutrition, Mahalla Hepatology Teaching Hospital, El-Mahalla El-Kubra, Elgharbia, Egypt; 5Department of Tropical Medicine, Hepatology & Gastroenterology Unit, Faculty of Medicine, Tanta University, Tanta, Egypt; 6Department of Pharmacy Practice, College of Pharmacy, Shaqra University, Shaqra, 11961, Saudi Arabia; 7Department of Botany & Microbiology, Faculty of Science, South Valley University, Qena, 83523, Egypt; 8Department of Biotechnology, College of Science, Taif University, Taif, 21944, Saudi Arabia; 9Department of Biochemistry, College of Science, University of Jeddah, Jeddah, 23445, Saudi Arabia; 10Department of Gastroenterology, Hepatology and Infectious Diseases, Faculty of Medicine, Al-Azhar University, Asyut, Egypt; 11Department of Hepatology, Gastroenterology and Infectious Diseases, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Correspondence: Sherief Abdel-Salam, Department of Tropical Medicine, Hepatology & Gastroenterology Unit, Faculty of Medicine, Tanta University, El-Bahr Street, Tanta, Egypt, Tel +201147773440, Email [email protected]
Background & Aims: This research aimed to determine how variations in the vitamin D receptor gene affected the response of H. pylori infections to eradication therapy.
Patients and Methods: On 105 adult H. Pylori-positive patients, a prospective cohort study was carried out. PCR was used to genotype all patients’ VDR gene polymorphisms. The patients in the study received standard triple eradication medication (clarithromycin 500 mg, amoxicillin 1000 mg, and omeprazole 20 mg) twice daily for 14 days. A stool test for H. pylori Ag was conducted 4 weeks following the end of treatment.
Results: In our study, the usual triple therapy’s H. pylori eradication rate was 75.2%. The successful eradication of H. pylori and VDR rs 2228570 gene polymorphisms was more prevalent in CT gene polymorphism (64.6%) compared to non-responders (19.2%), while treatment failure was more prevalent in CC gene polymorphism (73.1% in non-responders compared to responders 24.1%), which is statistically significant. In regards to the eradication of H. pylori and VDR rs7975232 gene polymorphisms, the success of eradication was more prevalent in AC gene polymorphism (54.4%) vs non-responders (30.4%), while all patients (14) with gene AA (17.7%) are responders to standard treatment, while the failure of treatment was more prevalent in CC gene polymorphism (69.2% in non-responder vs 27.8% in responders) which is statistically significant. Our findings demonstrated a strong correlation between patients’ responses to H. pylori treatment and polymorphisms in the VDR gene (ApaI and TaqI) (P 0.05).
Conclusion: As far as we are aware, this is the first study to identify a potential link between the FokI and Apal VDR polymorphism and treatment response in H pylori-positive patients. To evaluate the findings, more research with larger number of patients and different population is required.
Keywords: Helicobacter, infection, gene, polymorphism, response, eradication
Introduction
The spiral-shaped Gram-negative bacteria Helicobacter pylori (H. Pylori) exhibits a variety of processes and distinct virulence factors that impact the characteristics of the gastric mucosa and determine its adhesion and survival in this environment.1 The main cause of persistent gastritis is infection with the H. Pylori bacteria. Nearly half of the world’s population is impacted.2 Additionally, a study conducted on Egyptian patients by Abo-Amer et al discovered that 538 patients (83.3%) of Egyptian patients had H. pylori infection.3
Other gastrointestinal conditions such peptic ulcer disease, gastric adenocarcinoma, and gastric lymphoma are influenced by H. Pylori in their aetiology. H. pylori infection is linked to most duodenal ulcers and stomach malignancies.2 The strains that reside in the stomach mucosa and how they interact with the host’s immune system determine the long-term colonisation of H. pylori and the production of chronic gastritis.2 Additionally, the susceptibility and clinical development of the infection are also in part influenced by human genetic variations. They can create various levels of immune system mediators that are connected to infection rates, the eradication of H. pylori and colonisation by more virulent strains, the augmentation of stomach inflammation, and cell damage.4
The expression of the vitamin D receptor (VDR) in the stomach epithelia may improve as a result of H. pylori infection, according to a recent theory. Through the stimulation of cathelicidin antimicrobial peptides and the reduction of inflammatory cytokine and chemokine levels, it has been found in vitro that the active form of vitamin D, 1a,25-dihydroxy vitamin D3, exhibits immune modulators capabilities against this pathogen.5 In metanalysis done by Yang et al6 found that Vitamin D has a protective role in H pylori infection. Also, El Shahway et al,7 found that low level of Vitamin D associated with failure of treatment while Shafrir et al8 reported that increased vitamin D levels are associated with successful H. pylori eradication. The VDR gene, which spans a length of DNA larger than 60 kb, is found on the 12q13.11 chromosome.9 The restriction fragment length polymorphism (RFLP) for the FokI, BsmI, ApaI, and TaqI restriction enzymes is being utilised in investigations of genetic vulnerability to infectious diseases as well as response to treatment.10–12
The FokI polymorphism (rs2228570; C>T), characterized by the change of thymine to cytosine (ATG to ACG)13 and ApaI polymorphism (rs7975232, A>C) where cytosine is changed to adenine.14 The FokI and Apal VDR polymorphism and H. pylori infection may go hand in hand.15 This research aimed to determine how variations in the vitamin D receptor gene affected how H. pylori infections responded to eradication therapy.
Subject and Methods
Subject
From 176 adult H. Pylori-positive patients, only 105 H. Pylori-positive patients who meet the eligibility criteria, a prospective cohort study was carried out at Mahala Hepatology Teaching Hospital during the period from May 2021 to Jan 2022. Research was approved by Mahala Hepatology Teaching Hospital research ethical committee. No animals were used for studies that are the basis of this research. All human procedures followed were in accordance with the guidelines of Helsinki Declaration of 1975. Informed consent was obtained from all participants of this study.
Methods
All of the enrolled patients had their H. pylori status confirmed as positive using the Eliza procedure in accordance with the manufacturer’s instructions.
The following is administered to all patients;
1) PCR was used to genotype all patients’ VDR gene polymorphisms.
2) The widely used clarithromycin-based triple therapy, which includes omeprazole 20 mg, amoxicillin 1000 mg, and clarithromycin 500 mg twice daily for 14 days.
3) Four weeks following the completion of treatment, a stool sample was tested for H. pylori Ag.
Laboratory Analysis
Genotyping and DNA extraction: The DNA was extracted using the QIAamp® DNA Blood Mini Kit. Using a Nano Drop® (ND-1000) Spectrophotometer (Nano Drop Technologies Inc., Washington, USA), the concentration of the isolated DNA was determined.
Genotyping of VDR SNPs: Applied Biosystems (Applied Biosystems-Life Technologies, Carlsbad, California, USA) genotyped the VDR FokI (rs2228570) and ApaI (rs7975232) SNPs.
All patients provided written, informed consent.
Exclusion Criteria
A proton pump inhibitor (PPI) was taken within the previous month by subjects or those who reported receiving H. pylori medication within the previous six months, being pregnant, abusing alcohol, or using illegal drugs were excluded from the study. Utilisation of corticosteroids, immunosuppressive therapy, anti-inflammatory medications, or antibiotics in the two months prior. Gastric surgery, renal failure, liver cirrhosis, autoimmune diseases with a history, liver cirrhosis, and cancers were disqualified.
Statistical Analysis
Statistical tests were performed using SPSS 21.0. Qualitative data were expressed as number and percentage and quantitative variables were expressed as the mean ± standard deviation (mean ±SD) for parametric data. Chi-square test was used to evaluate qualitative data. Regression analysis was done to determine the independent risk factors for the H. pylori eradication. A level for statistical significance was significant at p < 0.05.
Results
The study involved 105 patients, whose average age was 49.44 + 10.94. Male patients made up 56 (53.3%) and female patients were 49 (46.7%). Only 26 patients (24.8%) smoked, and their average BMI was 29.43 5.75. The average lab results for CBC, liver enzyme, and creatinine were displayed in (Table 1).
 |
Table 1 Baseline Characteristic Features of the H. Pylori Infected Patients |
As seen in Table 1, the distribution of TT, CT, and CC genotypes among the patients under study was 10.5%, 53.3%, and 36.2%, respectively. As shown in Table 2, the proportions of males and females with VDR rs 2228570 gene polymorphisms are 7.1%, 14.3%, 50.0%, and 57.1%, respectively, in TT, CT, and CC. The distribution of the genotypes AA, AC, and CC for the VDR rs 7975232 gene polymorphisms was 13.3%, 48.6%, and 38.1%, respectively, among the overall study population. According to Table 2, the percentages of males and females with VDR rs 7975232 gene polymorphisms are as follows: AA (12.5% and 14.3%), AC (42.9% and 55.1%), and CC (44.6% and 30.6%).
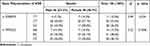 |
Table 2 Gene Polymorphism of VDR in Relation to Gender |
In 79 of the individuals under study, H pylori was completely eradicated (75.2% success rate). The successful eradication of H. pylori and VDR rs 2228570 gene polymorphisms was more prevalent in CT gene polymorphism (64.6%) compared to non-responders (19.2%), while treatment failure was more prevalent in CC gene polymorphism (73.1% in non-responders compared to responders 24.1%), which is statistically significant (Table 3). In regards to the eradication of H. pylori and VDR rs7975232 gene polymorphisms, the success of eradication was more prevalent in AC gene polymorphism (54.4%) vs non-responders (30.4%), while all patients (14) with gene AA (17.7%) are responders to standard treatment, while the failure of treatment was more prevalent in CC gene polymorphism (69.2% in non-responder vs 27.8% in responders) which is statistically significant.
 |
Table 3 Gene Polymorphism of VDR in Relation to the Treatment Outcome of H.pylori |
The VDR rs 2228570 and VDR rs 7975232 gene polymorphisms were found to be independent risk factors for the elimination of H. pylori after regression analysis (Table 4). There were significant correlations between H.Pylori response to eradication therapy and VDR rs 2228570 and VDR rs 7975232 alleles (Table 5).
 |
Table 4 Logistic Regression of H.Pylori Response to Eradication Therapy |
 |
Table 5 Logistic Regression Between H.Pylori Response to Eradication Therapy and VDR Rs 2228570 and VDR Rs 7975232 Alleles |
Discussion
The virulent strains of H. pylori are linked to gastric ulcers and cancer because they cause extensive immune cell infiltration in the gastric mucosa and cause noticeable inflammatory reactions.16 Due to its ability to neutralise gastric acid through the potent action of its urease enzymes4 and the activity of glutamyl transpeptidase enzyme, which supports its proliferation and survival in the gastric mucosa,17 H. pylori can persist in the gastric mucosa for an extended period of time during infection. Treatment with vitamin D inhibits both mechanisms.18 Because the vitamin D metabolites are implicated in the induction of antimicrobial activity and have anti-inflammatory and immune-system modulating properties.19,20 Failure to eradicate H. pylori may be associated with vitamin D deficiency, necessitating vitamin D supplementation prior to H. pylori eradication.21 VDR has a role in the immune-modulating abilities of active vitamin D.22 Vitamin D receptor gene polymorphisms (ApaI and TaqI) lead to decreased vitamin D level which associated with the response to treatment. In patients with H. pylori infection, Guo et al5 found a statistically significant positive connection between chronic inflammation and VDR mRNA expression.
105 patients who tested positive for H. pylori participated in the study. Our findings demonstrated a substantial correlation between patients’ responses to H. pylori treatment and polymorphisms in the VDR gene (ApaI and TaqI). Also, the eradication of H. pylori is at risk due to polymorphisms in the VDR gene (ApaI and TaqI). According to Mohamed et al’s findings, H. pylori infection and the FokI and Apal VDR polymorphism are related.15 Additionally, Qadir et al discovered a substantial correlation between the VDR Bsml SNP and increased risk of gastric cancer, particularly in obese individuals.23 In contrast to Martins et al,24 who claimed that there were no appreciable changes between patients with H. pylori infection and control groups in terms of the allelic and genotypic distribution of the FokI and ApaI polymorphisms of the VDR gene. Additionally, Eom et al25 discovered no conclusive associations between vitamin D intake and the prevalence of gastric cancer, and genetic variation related to vitamin D had no impact on these associations. The rates of H. pylori eradication do, however, appear to be related to vitamin D levels, according to Huang et al.26 The discrepancy in the findings could be attributed to the complex interactions between genetic, environmental, and societal factors that lead to H. pylori infections. Together with ethnic characteristics, these interactions—which are crucial for illness development and genetic makeup—were most likely responsible for the disparity in allelic frequencies observed in the research population. The results of Mohamed et al15 were consistent with the lack of a statistically significant variation in the sex distributions across the various genotypes. This is consistent with our findings.
In our study, the usual triple therapy had a 75.2% H. pylori eradication rate, and other studies have reported rates between 61 and 77%.27–30 In contrast to other studies, certain investigations31,32 showed greater rates (85–94%). Therefore, it makes sense to assume that variations in eradication rates are correlated with the degree of adherence and/or the local susceptibility pattern of H. pylori in the investigated areas. A meta-analysis has recommended that antibiotic selection be localised in light of this regional diversity.33 The present study found that there was a significant difference in the response to eradication therapy of H.Pylori regarding VDR (ApaI and TaqI) gene polymorphism. Also, the independent risk factors for H. pylori eradication were VDR rs 2228570 and VDR rs7975232 gene polymorphisms. There is also, a significant correlation between H. Pylori response to eradication therapy and VDR rs 2228570 and VDR rs 7975232 alleles.
Conclusion
According to our knowledge, this is the first study to have discovered a connection between H pylori positivity and the FokI and Apal VDR polymorphism, which are separate risk factors for H pylori eradication. There is also, a significant correlations between H. Pylori response to eradication therapy and FokI and Apal VDR polymorphism alleles. To evaluate the findings, more research with numerous populations is required.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yang I, Nell S, Suerbaum S. Survival in hostile territory: the microbiota of the stomach. FEMS Microbiol Rev. 2013;37(5):736–761. doi:10.1111/1574-6976.12027
2. Rana R, Wang SL, Li J, Wang YX, Rao QW, Yang CQ. Helicobacter pylori infection: a recent approach to diagnosis and management. Review. J Biomed Sci. 2017;2:45–56. doi:10.7150/jbm.17612
3. Abo-Amer YE, Sabal A, Ahmed R, et al. Relationship between helicobacter pylori infection and nonalcoholic fatty liver disease (NAFLD) in a developing country: a cross-sectional study. Diabetes Metab Syndr Obes. 2020;13:619–625. doi:10.2147/dmso.S237866
4. Kusters JG, Vliet AH, Kuipers EJ. Pathogenesis of Helicobacter pylori Infection. Clin Microbiol Rev. 2006;19(3):449–490. doi:10.1128/cmr.00054-05
5. Guo L, Chen W, Zhu H, et al. Helicobacter pylori induces increased expression of the vitamin d receptor in immune responses. Helicobacter. 2014;19(1):37–47. doi:10.1111/hel.12102
6. Yang L, He X, Li L, Lu C. Effect of vitamin D on Helicobacter pylori infection and eradication: a meta-analysis. Helicobacter. 2019;24(5):e12655. doi:10.1111/hel.12655
7. El Shahawy MS, Hemida MH, El Metwaly I, Shady ZM. The effect of vitamin D deficiency on eradication rates of Helicobacter pylori infection. JGH Open. 2018;2(6):270–275. doi:10.1002/jgh3.12081
8. Shafrir A, Shauly-Aharonov M, Katz LH, Paltiel O, Pickman Y, Ackerman Z. The association between serum vitamin D levels and helicobacter pylori presence and eradication. Nutrients. 2021;13(1):278. doi:10.3390/nu13010278
9. Crofts LA, Hancock MS, Morrison NA, Eisman JA. Multiple promoters direct the tissue-specific expression of novel N-terminal variant human vitamin D receptor gene transcripts. Proc Natl Acad Sci USA. 1998;95(18):10529–10534. doi:10.1073/pnas.95.18.10529
10. Alagarasu K, Honap T, Mulay AP, Bachal RV, Shah PS, Cecilia D. Association of vitamin D receptor gene polymorphisms with clinical outcomes of dengue virus infection. Hum Immunol. 2012;73(11):1194–1199. doi:10.1016/j.humimm.2012.08.007
11. Sortica VA, Cunha MG, Ohnishi MD, et al. IL1B, IL4R, IL12RB1 and TNF gene polymorphisms are associated with Plasmodium vivax malaria in Brazil. Malar J. 2012;11:409. doi:10.1186/1475-2875-11-409
12. Salimi S, Farajian-Mashhadi F, Alavi-Naini R, Talebian G, Narooie-Nejad M. Association between vitamin D receptor polymorphisms and haplotypes with pulmonary tuberculosis. Biomed Rep. 2015;3(2):189–194. doi:10.3892/br.2014.402
13. Colin EM, Weel AE, Uitterlinden AG, et al. Consequences of vitamin D receptor gene polymorphisms for growth inhibition of cultured human peripheral blood mononuclear cells by 1, 25-dihydroxyvitamin D3. Clin Endocrinol. 2000;52(2):211–216. doi:10.1046/j.1365-2265.2000.00909.x
14. Sherry ST, Ward MH, Kholodov M, et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. 2001;29(1):308–311. doi:10.1093/nar/29.1.308
15. Mohamed AA, Moussa S, Shaheen MM, et al. Association between vitamin d receptor gene polymorphisms and infection. Open Biomark J. 2020;10(1):8–14. doi:10.2174/1875318302010010008
16. Nogueira C, Figueiredo C, Carneiro F, et al. Helicobacter pylori genotypes may determine gastric histopathology. Am J Pathol. 2001;158(2):647–654. doi:10.1016/s0002-9440(10)64006-0
17. Gong M, Ling SS, Lui SY, Yeoh KG, Ho B. Helicobacter pylori gamma-glutamyl transpeptidase is a pathogenic factor in the development of peptic ulcer disease. Gastroenterology. 2010;139(2):564–573. doi:10.1053/j.gastro.2010.03.050
18. Kawaura A, Takeda E, Tanida N, et al. Inhibitory effect of long term 1α-hydroxyvitamin administration on helicobacter pylori infection. J Clin Biochem Nutr. 2006;38(2):103–106. doi:10.3164/jcbn.38.103
19. Youssef DA, Miller CW, El-Abbassi AM, et al. Antimicrobial implications of vitamin D. Dermatoendocrinol. 2011;3(4):220–229. doi:10.4161/derm.3.4.15027
20. Mangin M, Sinha R, Fincher K. Inflammation and vitamin D: the infection connection. Inflamm Res. 2014;63(10):803–819. doi:10.1007/s00011-014-0755-z
21. Yildirim O, Yildirim T, Seckin Y, Osanmaz P, Bilgic Y, Mete R. The influence of vitamin D deficiency on eradication rates of Helicobacter pylori. Adv Clin Exp Med. 2017;26(9):1377–1381. doi:10.17219/acem/65430
22. White JH. Vitamin D metabolism and signaling in the immune system. Rev Endocr Metab Disord. 2012;13(1):21–29. doi:10.1007/s11154-011-9195-z
23. Qadir J, Majid S, Khan MS, Wani MD. Association of Vitamin D receptor gene variations with Gastric cancer risk in Kashmiri population. Mol Biol Rep. 2021;48(4):3313–3325. doi:10.1007/s11033-021-06376-z
24. Martins DJ, Matos GC, Loiola RS, D’Annibale V, Corvelo T. Relationship of vitamin D receptor gene polymorphisms in Helicobacter pylori gastric patients. Clin Exp Gastroenterol. 2018;11:19–27. doi:10.2147/ceg.S143332
25. Eom SY, Yim DH, Kim DH, et al. Dietary vitamin D intake and vitamin D related genetic polymorphisms are not associated with gastric cancer in a hospital-based case-control study in Korea. J Biomed Res. 2018;32(4):257–263. doi:10.7555/jbr.32.20170089
26. Huang B, Yan S, Chen C, Ye S. Effect of 25-hydroxyvitamin D on Helicobacter pylori eradication in patients with type 2 diabetes. Wien Klin Wochenschr. 2019;131(3–4):75–80. doi:10.1007/s00508-018-1416-y
27. Ramas M, Donday MG, McNicholl AG, Gisbert JP. Efficacy and safety of rifaximin associated with standard triple therapy (omeprazole, clarithromycin and amoxicillin) for H. pylori eradication: a Phase IV pilot clinical trial. Gastroenterol Hepatol. 2017;40(10):658–662. doi:10.1016/j.gastrohep.2017.05.017
28. Ahmed HM, Abd-Elsalam S, Mahrous MA. Moxifloxacin based triple therapy as alternative to standard therapy in Helicobacter Pylori Eradication. Anti-Infective Agents. 2021;19(3):299–302. doi:10.2174/2211352518999200925154501
29. Abd-Elsalam S, Kobtan A, El-Kalla F, et al. A 2-week Nitazoxanide-based quadruple treatment as a rescue therapy for Helicobacter pylori eradication: a single center experience. Medicine. 2016;95(24):e3879. doi:10.1097/md.0000000000003879
30. Shehata MA, Talaat R, Soliman S, Elmesseri H, Soliman S, Abd-Elsalam S. Randomized controlled study of a novel triple nitazoxanide (NTZ)-containing therapeutic regimen versus the traditional regimen for eradication of Helicobacter pylori infection. Helicobacter. 2017;22:5.
31. Fock KM, Chelvam P, Lim SG. Triple therapy in the eradication of Helicobacter pylori in patients with duodenal ulcer disease: results of a multicentre study in South-East Asia. South-East Asia Multicenter Study Group. Aliment Pharmacol Ther. 2000;14(2):225–231. doi:10.1046/j.1365-2036.2000.00691.x
32. Gebeyehu E, Nigatu D, Engidawork E. Helicobacter pylori eradication rate of standard triple therapy and factors affecting eradication rate at Bahir Dar city administration, Northwest Ethiopia: a prospective follow up study. PLoS One. 2019;14(6):e0217645. doi:10.1371/journal.pone.0217645
33. Xin Y, Manson J, Govan L, et al. Pharmacological regimens for eradication of Helicobacter pylori: an overview of systematic reviews and network meta-analysis. BMC Gastroenterol. 2016;16(1):80. doi:10.1186/s12876-016-0491-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
