Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
Association Between Thyroid Function and Acute Exacerbation of Chronic Obstructive Pulmonary Disease
Authors Huang D, Wu D, He J, Chen M, Zhao X, Li D, Wu B
Received 12 November 2020
Accepted for publication 1 February 2021
Published 17 February 2021 Volume 2021:16 Pages 333—339
DOI https://doi.org/10.2147/COPD.S291807
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Dan Huang, Dong Wu, Jinhong He, Min Chen, Xuanna Zhao, Dongming Li, Bin Wu
Department of Respiratory and Critical Care Medicine, Affiliated Hospital of Guangdong Medical University, Zhanjiang, People’s Republic of China
Correspondence: Dongming Li; Bin Wu
Department of Respiratory and Critical Care Medicine, Affiliated Hospital of Guangdong Medical University, 57th South Renmin Road, Zhanjiang, Guangdong, 524001, People’s Republic of China
Tel/Fax +867592387413
Email [email protected]; [email protected]
Purpose: Chronic obstructive pulmonary disease (COPD) was the fourth leading cause of death in the world. Many studies have shown that COPD often exists with thyroid dysfunction; however, the relationship between thyroid function and COPD is often ignored in clinical. We retrospectively analyze the serum thyroid hormone levels in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD) and explore the association between thyroid function and AECOPD.
Methods: The study included patients hospitalized for AECOPD in our institution between January 2018 and September 2020. Patients with AECOPD were divided into moderate-to-severe and very severe groups based on lung function, and into normal and abnormal thyroid function groups based on thyroid hormone levels. Collected data and compared data between groups to identify risk factors for thyroid dysfunction in patients with AECOPD.
Results: The cohort included 97 in the moderate-to-severe group (72.39%) and 37 in the very severe group (27.61%). Compared with the very severe group, the moderate-to-severe group had higher triglyceride (P=0.017), high-density lipoprotein (P< 0.05), partial pressure of carbon dioxide (PaCO2; P< 0.05), and serum thyroid-stimulating hormone (TSH; P< 0.001). FEV1 as a percentage of the predicted value (FEV1%pred) was positively correlated with TSH and FT3 (r=0.329, r=0.192, respectively, both P< 0.05). Duration of hospitalization was negatively correlated with TSH (r=− 0.256, P=0.003). Among the 134 subjects, 98 (73.13%) had normal thyroid function and 36 (26.87%) had abnormal thyroid function. The two groups significantly differed regarding forced vital capacity (FVC), forced expiratory volume in 1 second, FEV1%pred, and albumin level. Logistic regression analysis showed that high FVC correlated with a low risk of thyroid dysfunction in AECOPD.
Conclusion: In patients with AECOPD, TSH is related to lung function and duration of hospitalization, and high FVC reduces the risk of thyroid dysfunction.
Keywords: AECOPD, thyroid hormone, retrospective cohort study, risk factor
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable chronic airway inflammatory disease. COPD was the fourth leading cause of death in the world in 2019 and is predicted to be the third leading cause of death in 2020.1 In China, the estimated overall prevalence of COPD was 13.6% in 2014–2015,2 and COPD was the fifth leading cause of death in 2016.3
COPD often exists with comorbidities that may significantly affect the disease course. Comorbidities not only affect symptom burden and health status but also affect the risk of hospitalization and mortality in patients with COPD.4 It is well known that the chronic inflammation of COPD is not just limited to the lungs, but spreads to other organs through the circulation.5 Comorbidities commonly recognized in patients with COPD include cardiovascular diseases, metabolic syndrome, osteoporosis, and anxiety. However, thyroid disease is also common in patients with COPD.6 A cross-sectional study from Spain showed that patients with COPD had a higher prevalence of thyroid disease (14.2%) than the expected standardized prevalence of chronic diseases (11.06%), and the prevalence of thyroid disease was higher in female than male patients (24.6% vs 10.9%).7 Acute exacerbation of COPD (AECOPD) and the exacerbation frequency have negative effects on quality of life and survival. We recalculated Gumus A’s study data and found a decrease in triiodothyronine (T3; 18.2%) and thyroid-stimulating hormone (TSH; 30.3%) in patients with exacerbation of COPD;8 furthermore, the exacerbation frequency was higher in patients with COPD with hypothyroidism than in those without hypothyroidism. The frequency of COPD exacerbation was positively correlated with TSH levels.9,10
The abovementioned findings suggest that the relationship between thyroid function and COPD may be underestimated. Therefore, we reviewed the clinical data of patients with AECOPD who had been admitted to our hospital in the past 2 years, analyzed the relationship between thyroid function and severity of illness in patients with AECOPD, and explored the related risk factors.
Patients and Methods
Study Population
This was a retrospective cohort study. Data were collected from patients hospitalized for AECOPD in the Department of Respiratory and Critical Care Medicine, Affiliated Hospital of Guangdong Medical University between January 2018 and September 2020. Collected data included demographics, smoking history, diagnosis, treatment, duration of hospitalization, thyroid hormone levels, serum biochemical indexes, lung function, and arterial blood gas findings.
For all included patients, COPD was clinically diagnosed and confirmed by lung function testing, and hospitalization was initiated because of AECOPD. The diagnosis of COPD and classification of severity were based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) spirometry guidelines. AECOPD was defined as an acute worsening of respiratory symptoms that required additional therapy. Patients with AECOPD were divided in accordance with their lung function into a moderate-to-severe group (forced expiratory volume in 1 second as a percentage of the predicted value (FEV1%pred) 30–79%) and a very severe group (FEV1%pred <30%). The inclusion criteria were: (1) age ≥40 years; (2) moderate to very severe airflow limitation, post-bronchodilator FEV1/forced vital capacity (FVC) ratio <0.7 and FEV1%pred <0.8; (3) detected serum thyroid hormone levels. The exclusion criteria were: (1) primary diagnosis of asthma; (2) severe bronchiectasis, pulmonary tuberculosis, or pulmonary fibrosis; (3) history of lung volume reduction surgery, pneumonectomy, or lung transplantation; (4) history of cancer; (5) history of thyroid disease, thyroid surgery, or administration of drugs containing iodine; (6) severe infection; (7) treatment administered before hospital admission.
Our study complied with the Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. As this was a retrospective study, informed consent of patient was not required by the Ethics Committee of Affiliated Hospital of Guangdong Medical University. The privacy of all participants was protected, we confirmed the data were anonymized and maintained with confidentiality.
Statistical Methods
SPSS statistical package (SPSS 22.0, IBM, USA) was used for all data analyses. The distributions of continuous variables were examined using the Kolmogorov–Smirnov normality test. Continuous variables with normal distribution were presented as mean ± standard deviation, while continuous variables with non-normal distribution were presented as median and interquartile range (IQR). The chi-squared test was used to compare categorical variables between the moderate-to-severe group and the very severe group. Correlations among variables were analyzed using Spearman correlation test. Binary regression analyses were performed to evaluate the potential independent association between thyroid function and each of the assessed parameters. P<0.05 was considered statistically significant.
Results
Patient Characteristics
A total of 134 patients with AECOPD were included, including 97 (72.39%) in the moderate-to-severe group and 37 (27.61%) in the very severe group. The two groups did not differ regarding age, sex, BMI classification, smoking status and course of disease. Blood gas analysis showed a lower PaCO2 in the moderate-to-severe group than the very severe group (43.30 mmHg vs 47.80 mmHg; P<0.001), but no intergroup differences in pH and PaO2. The serum triglyceride level was higher in the moderate-to-severe group than in the very severe group (0.91 mmol/L vs 0.80 mmol/L; P=0.017), while the high-density lipoprotein level was lower in the very severe group than in the moderate-to-severe group (1.37 mmol/L vs 1.54 mmol/L, P=0.025). The other assessed biochemical indexes (albumin, calcium ion, creatinine, urea, uric acid, total cholesterol, and low-density lipoprotein) did not differ between the two groups. The TSH level significantly differed between the two groups (P=0.001), but the FT3 and FT4 did not (Table 1, Supplemental Table 1)
 |
Table 1 Demographic and Clinical Characteristics of the Moderate-to-Severe Group Compared with the Very Severe Group |
Correlations Between FEV1%pred, PaCO2, PaO2, Duration of Hospitalization, and Thyroid Hormone Levels
There were no correlations between the thyroid hormone levels and either PaCO2 or PaO2. However, TSH and FT3 were positively correlated with FEV1%pred (r=0.329 and r=0.192, respectively, both P<0.05). The duration of hospitalization was negatively correlated with TSH (r=−0.256, P=0.003), but was not correlated with FT3 and FT4 (Table 2).
 |
Table 2 Correlations Between FEV1%pred, PaCO2, PaO2, Duration of Hospitalization, and Thyroid Hormone Levels |
Thyroid Hormone Levels in Patients with AECOPD
We separated all patients into two groups in accordance with the serum thyroid hormone levels (normal ranges of serum FT3, FT4, and TSH: 2.3–6.8 pmol/L, 10–23.5 pmol/L, and 0.34–4.0 mIU/L, respectively); the normal thyroid hormone group (normal group) comprised 98 patients (73.13%) and the abnormal thyroid hormone group (abnormal group) comprised 36 (26.87%). The two groups did not differ regarding age, sex, BMI classification, smoking status. The FVC, FEV1, and FEV1%pred were higher in the normal group than the abnormal group (1.82 vs 1.38, 0.91 vs 0.7, and 42.72% vs 35.39%, respectively, all P<0.05). Blood gas analysis revealed that pH, PaO2, and PaCO2 did not differ between the two groups. The serum albumin level was higher in the normal group than the abnormal group (39.15 g/L vs 37.47 g/L, P=0.033), but the other assessed biochemical indexes did not differ between the two groups (Table 3, Supplemental Table 2).
 |
Table 3 Clinical Data of Patients with AECOPD with Normal and Abnormal Thyroid Hormone Levels |
Risk Factors for AECOPD Complicated with Abnormal Thyroid Function
Table 4 shows that smoking history, FVC, FEV1, and FEV1%pred significantly differed between the normal and abnormal groups. We analyzed these data using binary regression analyses to identify the risk factors for abnormal thyroid function in patients with AECOPD. The FVC tended to be a protective factor to reduce the prevalence of abnormal thyroid function in patients with AECOPD (OR 0.114, 95% CI 0.015–0.887), while the other assessed variables showed no association with thyroid function.
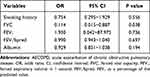 |
Table 4 Risk Factors for AECOPD Complicated with Abnormal Thyroid Function |
Discussion
COPD is a respiratory disease that is prevalent worldwide and has chronic airway inflammation as is its major characteristic. In addition to airway inflammation, patients with COPD have inflammation in other body systems. The GOLD guidelines state that COPD is often complicated with many diseases,11 but thyroid dysfunction may be an underestimated complication of COPD due to insufficient clinical data. As we know, COPD patients often had a smoke history. Both cigarette smoke and chronic inflammatory in COPD itself can impair the thyroid gland, and lead to abnormal thyroid hormone production.12 Karadag et al demonstrated that the prevalence of non-thyroidal illness syndrome (abnormal thyroid hormone levels not due to thyroid disease) was 14–20% in patients with stable COPD, and 70% in patients with AECOPD.13 Of the 134 patients with AECOPD in the present study, approximately 26.87% had abnormal thyroid hormone levels. Due to the difference of AECOPD inclusion criteria between us, our data shown the prevalence of AECOPD with abnormal thyroid function was lower than in the study by Karadag et al.13 But our findings still suggest that thyroid dysfunction is common in patients with AECOPD.
Thyroid hormones play an important role in the regulation of metabolism by enhancing mitochondrial oxidation and augmenting the metabolic rate.14 The effect of thyroid hormones on the metabolic rate is probably responsible for the relationship between thyroid hormone levels and respiratory drive.15 Both hypothyroidism and hyperthyroidism can impair respiratory muscle function, respiratory mechanics, and exercise capacity in patients with COPD.16 Lung function (especially FEV1%pred) is used as the basis for grading COPD and is closely related to the severity of AECOPD. Siafakas et al showed that in patients with hyperthyroidism, inspiratory and expiratory muscle weakness (expressed as a reduction in the FEV1, FVC, vital capacity, maximal expiratory pressure, and maximal inspiratory pressure) were positively correlated with the severity of hyperthyroidism;17 this was also supported by Terzano et al.18 Our results showed that the TSH level was higher in patients with moderate-to-severe AECOPD than in those with very severe AECOPD. Furthermore, the FVC, FEV1, and FEV1%pred were higher in patients with AECOPD with normal thyroid hormone levels than in those with abnormal thyroid hormone levels. We further analyzed the association between thyroid hormone levels and lung function and found that the FEV1%pred was positively correlated with the levels of TSH and FT3. These results demonstrated that the severity of airway obstruction was associated with the levels of TSH and FT3. These findings were consistent with Okutan O and Gao F’s study.19,20 Ulasli et al found that TSH was the decisive factor in the frequency of AECOPD.9 In addition, Bacakoglu showed that low serum concentrations of FT3 and FT4 increased the incidence and mortality of invasive mechanical ventilation in patients with respiratory failure.21 These findings suggest that thyroid hormone levels probably influence the prognosis of AECOPD. Therefore, we analyzed the relationship between TSH and the duration of hospitalization and found that these factors were negatively correlated. We speculate that this is related to the lower severity of AECOPD in patients with higher TSH which is positively correlated to FEV1%pred. Furthermore, binary regression analysis revealed that the FVC was a protective factor to reduce the prevalence of thyroid dysfunction in patients with AECOPD.
The mechanism of thyroid dysfunction in COPD is not clear but may be related to hypoxemia and hypercapnia.21 Karadag et al found that TSH and FT3 were lower in patients with COPD with severe hypoxemia than in patients with milder hypoxia.13 In contrast, some studies demonstrated that thyroid hormones were not correlated with pH, PaO2, or PaCO2.22,23 We also did not detect any relationship between TSH, FT3, FT4 and PaO2 or PaCO2. On the one hand, we speculate that this may be related to the fact that most of the patients included did not have respiratory failure; on the other hand, it may be related to the dynamic changes of hormones, PaCO2, PaO2 in the body, and dynamic observations may be better able to capture their correlations. Therefore, our team also plans to conduct prospective studies in order to provide more sufficient evidence for the relationship between thyroid hormones and AECOPD.
The results of the present study not only enhance the previous findings on the relationship between thyroid hormones and AECOPD but also add information that thyroid hormone levels influence the prognosis of AECOPD.
Limitation
As with all studies using retrospective information data, our study had some limitations. The clinical data that we could obtain from the medical record were limited. Therefore, we could not group subjects according to ABCD GOLD classification and perform more comprehensive comparisons between groups. Our findings were based on a single center and the sample size was limited, so the relationship between thyroid function and COPD maybe was underestimated or overestimated. Most stable COPD patients always inhaled hormones to control symptoms, we could not exclude it will affect the thyroid function. Although this study had some limitations, we hope these findings can raise clinical concerns about thyroid function in patients with COPD.
Conclusion
The clinical symptoms of thyroid dysfunction are often concealed by the symptoms of AECOPD, which leads to neglect and diagnostic difficulties. Our study shows that thyroid dysfunction is common in patients with AECOPD. Furthermore, serum TSH levels are positively correlated with the FEV1%pred and negatively correlated with the duration of hospitalization. These findings suggest that the thyroid function should be monitored in patients with AECOPD because this is related to patient recovery.
Acknowledgments
The authors would like to thank the staff of the Department of Respiratory and Critical Care Medicine, Affiliated Hospital of Guangdong Medical University for providing all the clinical data, and for their support and cooperation. We thank Kelly Zammit, BVSc, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Disclosure
The authors of this study declare no conflicts of interest in this work.
References
1. Lopez-Campos JL, Soler-Cataluna JJ, Miravitlles M. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2019 report: future challenges. Arch Bronconeumol. 2020;56(2):65–67. doi:10.1016/j.arbres.2019.06.001
2. Fang L, Gao P, Bao H, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. 2018;6(6):421–430.
3. Collaborators GBDCoD. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210.
4. Vanfleteren LE, Spruit MA, Groenen M, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(7):728–735.
5. Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33(5):1165–1185.
6. Milkowska-Dymanowska J, Bialas AJ, Zalewska-Janowska A, Gorski P, Piotrowski WJ. Underrecognized comorbidities of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1331–1341.
7. Garcia-Olmos L, Alberquilla A, Ayala V, et al. Comorbidity in patients with chronic obstructive pulmonary disease in family practice: a cross sectional study. BMC Fam Pract. 2013;14:11.
8. Gumus A, Ozyurt S, Ozcelik N, Kara BY. Prevalence of non-thyroidal illness syndrome in COPD exacerbation and effect of hypoxaemia and hypercapnia on thyroid functions. Clin Respir J. 2020;14(9):806–812.
9. Sarinc Ulasli S, Bozbas SS, Ozen ZE, Ozyurek BA, Ulubay G. Effect of thyroid function on COPD exacerbation frequency: a preliminary study. Multidiscip Respir Med. 2013;8(1):64.
10. Chaudhary SC, Ahmad T, Usman K, et al. Prevalence of thyroid dysfunction in chronic obstructive pulmonary disease patients in a tertiary care center in North India. J Family Med Prim Care. 2018;7(3):584–588. doi:10.4103/jfmpc.jfmpc_84_17
11. Disease GIfCOL. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2020 report. 2019. Available from: https://goldcopd.org/gold-reports/.
12. Milkowska-Dymanowska J, Bialas AJ, Laskowska P, Gorski P, Piotrowski WJ. Thyroid gland in chronic obstructive pulmonary disease. Adv Respir Med. 2017;85(1):28–34.
13. Karadag F, Ozcan H, Karul AB, Yilmaz M, Cildag O. Correlates of non-thyroidal illness syndrome in chronic obstructive pulmonary disease. Respir Med. 2007;101(7):1439–1446.
14. Silva JE. Thermogenesis and sympathoadrenal system in thyrotoxicosis. In: The Thyroid. A Fundamental and Clinical Text.
15. Saaresranta T, Polo O. Hormones and breathing. Chest. 2002;122(6):2165–2182.
16. Laghi F, Adiguzel N, Tobin MJ. Endocrinological derangements in COPD. Eur Respir J. 2009;34(4):975–996.
17. Siafakas NM, Milona I, Salesiotou V, Filaditaki V, Tzanakis N, Bouros D. Respiratory muscle strength in hyperthyroidism before and after treatment. Am Rev Respir Dis. 1992;146(4):1025–1029.
18. Terzano C, Romani S, Paone G, Conti V, Oriolo F. COPD and thyroid dysfunctions. Lung. 2014;192(1):103–109.
19. Gao F. Correlation analysis of thyroid hormone levels and pulmonary function and nutritional status of patients with COPD in acute exacerbation. Zhejiang J Integr Trad Chin Western Med. 2017;27(03):199–202.
20. Bacakoglu F, Basoglu OK, Gurgun A, Bayraktar F, Kiran B, Ozhan MH. Can impairments of thyroid function test affect prognosis in patients with respiratory failure? Tuberk Toraks. 2007;55(4):329–335.
21. Akpinar EE. An underestimated comorbidity of COPD: thyroid dysfunction. Tuberk Toraks. 2019;67(2):131–135.
22. Banks WA, Cooper JA. Hypoxia and hypercarbia of chronic lung disease: minimal effects on anterior pituitary function. South Med J. 1990;83(3):290–293.
23. Semple PD, Hume R, Beastall GH, Watson WS. Thyroid function and endocrine abnormalities in elderly patients with severe chronic obstructive lung disease. Thorax. 1988;43(11):945–946.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
