Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 19
Association Between Serum Anion Gap and Mortality in Critically Ill Patients with COPD in ICU: Data from the MIMIC IV Database
Authors Chen X , Yang Q, Gao L, Chen W , Gao X, Li Y, Ao L, Sun D
Received 22 September 2023
Accepted for publication 15 February 2024
Published 29 February 2024 Volume 2024:19 Pages 579—587
DOI https://doi.org/10.2147/COPD.S433619
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Zhang
Xiaojing Chen,1– 3,* Qilin Yang,4,* Li Gao,1– 3 Weinan Chen,1 Xiaoyu Gao,1– 3 Yameng Li,1– 3 Liying Ao,5 Dejun Sun1– 3
1Department of Respiratory and Critical Care Medicine, Inner Mongolia People’s Hospital, Hohhot, 010017, People’s Republic of China; 2NHC Key Laboratory of Diagnosis & Treatment of COPD, Inner Mongolia People’s Hospital, Hohhot, 010017, People’s Republic of China; 3Inner Mongolia Key Laboratory of Respiratory Diseases, Inner Mongolia People’s Hospital, Hohhot, 010017, People’s Republic of China; 4Department of Critical Care, the Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, People’s Republic of China; 5Department of Otolaryngology, Inner Mongolia People’s Hospital, Hohhot, 010017, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Dejun Sun, Department of Respiratory and Critical Care Medicine, Inner Mongolia People’s Hospital, No. 26 Zhaowuda Road, Saihan District, Hohhot, 010017, People’s Republic of China, Email [email protected]
Background: Serum anion gap (AG) has been proven to be associated with prognosis in critically ill patients. However, few studies have investigated the association between AG and all-cause mortality in critically ill patients with chronic obstructive pulmonary disease (COPD).
Objective: We hypothesized that the initial AG level would predict the mortality risk in critically ill patients with COPD.
Methods: This retrospective cohort study was based on the Medical Information Mart for Intensive Care (MIMIC) IV database. We extracted demographics, vital signs, laboratory tests, comorbidity, and scoring systems from the first 24 hours after patient ICU admission. Multivariable logistic regression analysis models were used to explore the association between serum AG levels and mortality. Interaction and stratified analyses were conducted including age, gender and comorbidity.
Results: A total of 5531 critically ill patients with COPD were enrolled, composed of 53.6% male and 46.4% female with a median age of 73 years. The all-cause mortality of these patients during ICU hospitalization was 13.7%. The risk of all-cause mortality increased as the AG level increased in the univariate logistic regression analysis (OR=1.13, 95% CI: 1.11– 1.15, p< 0.01). After adjusting for all the covariates in multivariate logistic regression analysis, the odds ratio was 1.06 (95% CI: 1.04– 1.09, p< 0.01). Compared with the lowest AG group Q1 (≤ 11mmol/L), the adjusted OR value for AG and mortality in Q2 (12– 13mmol/L) was 0.89 (95% CI: 0.63– 1.25, p=0.502), Q3 (14– 15mmol/L) was 0.95 (95% CI: 0.68– 1.34, p=0.788), and Q4 (≥ 16mmol/L) was 1.49 (95% CI: 1.10– 2.02, p=0.009) respectively. In addition, the results of the subgroup and stratified analyses were robust.
Conclusion: AG is positively related to all-cause mortality in critically ill patients with COPD.
Keywords: AG, COPD, mortality, MIMIC IV
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogeneous clinical syndrome characterized by injury to the airway, airspace and lung vascular, and is often accompanied by a group of comorbidities, such as respiratory failure, cardiovascular disease, malignancies.1 COPD is a major cause of mortality worldwide characterized by progressive decline in lung function, and the exacerbation of COPD often leads to the needing of corticosteroids, antibiotics, or even hospitalization.2–4 Studies have shown that patients with COPD are at a higher risk of mortality in intensive care units (ICUs).5 Critically ill patients with COPD are particularly vulnerable to developing acidosis due to hypoxia and metabolic disorders leading to the overproduction of acid.
The serum anion gap (AG) is the difference between the unmeasured cations and anions in the blood and is composed of organic acids, serum albumin, phosphate, and sulfate. AG is used to detect acid-base disorders and analyze the primary metabolic acidosis.6 Recent studies have shown that a high AG level is associated with increased mortality in ICU patients with conditions such as aortic aneurysm,7 sepsis,8 acute kidney injury(AKI) requiring continuous renal replacement therapy(CRRT),9 cardiogenic shock,10 acute pancreatitis11 and hip fractures.12
However, few studies have investigated the association between AG and all-cause mortality in critically ill patients with COPD. Therefore, we aimed to conduct a large retrospective cohort study using the MIMIC IV database to further explore the relationship between AG and mortality in this group of patients. Our hypothesis was that high AG would be associated with an increased risk of mortality in critically ill patients with COPD, and we anticipated that a simple AG measurement might be a useful laboratory predictor of prognosis in these individuals.
Methods
Data Source
The Medical Information Mart for Intensive Care (MIMIC) IV database (version: 1.0) is a large database containing information on over 50,000 patients who were hospitalized in the ICU of Beth Israel Deaconess Medical Center in Boston, MA, from 2008 to 2019.13 This database is freely accessible and open to researchers who wish to use it for medical research purposes. The authors of this study used Structured Query Language (SQL) with PostgreSQL (version 9.6) to extract data relevant to their study from the MIMIC IV database. It is important to note that the use of this database was approved by the Massachusetts Institute of Technology (MIT) and Beth Israel Deaconess Medical Center (BIDMC), and one of the authors, Xiaojing Chen, completed the Collaborative Institutional Training Initiative (CITI) examination, received authorization to enter the MIMIC IV database, and obtained certification (ID: 11765076).
Patient Selection
All the ICU consecutive adult patients (aged>18 years) who had a diagnosis of COPD using International Classification of Diseases (ICD)-9 and ICD-10 codes (code = 49,120, 49,121, 49,122, 496, J44, J44, J440, J441 and J44) in MIMIC IV database were selected in the present study. Only the first ICU admission record was selected. Patients who did not measure serum anion gap within the first 24 hours after being admitted to ICU were excluded. This study was was performed with the approval of Ethics Committee of Inner Mongolia People’s Hospital (202306109L).
Data Extraction
We extracted demographic parameters (age, gender, race), vital signs, laboratory tests, comorbidity diseases, mortality, the length of ICU stay and scoring systems from the first 24 hours after patient ICU admission. Vital signs including heart rate (HR), mean arterial pressure (MBP), respiratory rate (RR) and temperature were used as the mean value. The following laboratory parameters were also extracted: the first anion gap, white blood cell (WBC), hematocrit, hemoglobin, platelets, creatinine, blood urea nitrogen (BUN) and glucose. The comorbidities included congestive heart failure (CHF), renal disease, cerebrovascular disease, peptic ulcer disease, malignancy and sepsis. We also calculated Charlson Comorbidity Index (CCI) for each patient. Sepsis calculated depended on the sequential organ failure assessment (SOFA) score,14 and SOFA was based on the scores of six different systems, including the respiratory, cardiovascular, hepatic, coagulation, renal and neurological. The endpoint of our study was all-cause mortality in hospitals.
Statistical Analysis
Patients were classified into four groups based on the quartile distribution of serum AG. Continuous variables were expressed as mean ± standard deviation (SD) or median (interquartile range [IQR]), while categorical variables were presented as proportions (percentages). The two-sample t-test was used for inter-group comparisons of continuous variables, while the chi-squared test was used for categorical variables.
Logistic regression analysis models were used to determine the odds ratios (ORs) and 95% confidence intervals (CIs) for the association between serum AG levels/quartiles and the risk of mortality. The lowest quartile of serum AG was used as the reference group. Model I adjusted for age, gender, race, and vital signs (heart rate, respiratory rate, mean blood pressure, temperature). Model II further adjusted for comorbidities (congestive heart failure [CHF], cerebrovascular disease, peptic ulcer, renal disease, malignancy, and sepsis), platelet count, blood urea nitrogen (BUN), white blood cell (WBC) count, creatinine, hematocrit, hemoglobin, glucose, and Charlson Comorbidity Index (CCI). Subgroup analysis was performed to assess whether the effect of serum AG levels on mortality differed across subgroups. The statistical software packages R (http://www.R-project.org, The R Foundation) and Free Statistics software versions 1.7 were used for the analyses, and a P-value of less than 0.05 was considered statistically significant.
Results
Participants Characteristics
In the MIMIC IV database, there were initially 5684 critically ill patients with COPD. After excluding 153 patients due to missing data (see Figure 1 for details), a total of 5531 patients were included in the final analysis, with 53.6% male and 46.4% female with a median age of 73 years. Among the included patients, the all-cause mortality during ICU hospitalization was 13.7%. Table 1 presents the baseline characteristics of all participants.
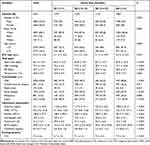 |
Table 1 Baseline Characteristics of Participants According to Anion Gap |
 |
Figure 1 Flowchart of subject screening. Abbreviations: ICU, intensive care unit; MIMIC-IV, Medical Information Mart for Intensive Care version IV; COPD, chronic obstructive pulmonary disease. |
Relationship Between Serum Anion Gap and Mortality
Table 2 shows the risk of all-cause mortality increased as the AG level increased in univariate logistic regression analysis (OR=1.13, 95% CI: 1.11–1.15, p<0.01). Table 3 shows after adjusting for all the covariates in multivariate logistic regression analysis, the odds ratio is 1.06 (95% CI: 1.04–1.09, p<0.01), and the ORs representing the strength of the association between serum AG and mortality in various multivariate logistic regression models for all participants. Compared with the lowest AG group Q1 (≤11mmol/L), the adjusted OR value for AG and mortality in Q2 (12–13mmol/L) was 0.89 (95% CI: 0.63–1.25, p=0.502), Q3 (14–15mmol/L) was 0.95 (95% CI: 0.68–1.34, p=0.788), Q4 (≥16mmol/L) was 1.49 (95% CI: 1.10–2.02, p=0.009) respectively.
 |
Table 2 Association Between Anion Gap (AG) and Covariates with Mortality Risk |
 |
Table 3 Association Between Anion Gap (AG) and All-Cause Mortality Risk in Different Models |
In univariate logistic regression analysis (Table 2), several covariates were associated with mortality. The mortality risk increased with age, heart rate, respiratory rate, white blood cell count, blood urea nitrogen, creatinine, glucose and Charlson Comorbidity Index scores. Comorbidities except for peptic ulcer were positively correlated with mortality, while temperature, mean blood pressure, hematocrit, hemoglobin and platelet were negatively correlated with mortality.
Subgroup Analysis
To further examine the robustness of the relationship between serum AG levels and mortality, we conducted a subgroup analysis based on gender, age and comorbidities, which is shown in the forest plot in Figure 2. The results indicated that the association between serum AG and mortality were consistent across patients with different genders, age and comorbidities. The interaction analysis revealed that sepsis had interactions with AG in predicting mortality (P<0.05).
Discussion
In aggregate, the current large retrospective cohort study showed that high serum AG levels were associated with increased mortality risk in critically ill patients with COPD who are admitted to the ICU, as per the MIMIC IV database. The multivariate logistic regression analysis revealed that, even after accounting for confounding variables, high serum AG was independently associated with all-cause mortality in these patients. Furthermore, compared with the lowest AG group, the highest AG group had a 1.49-fold increased risk of all-cause mortality. These findings are consistent with earlier research.
COPD is a leading cause of mortality worldwide,2–4 especially among critically ill patients in the ICU, possibly due to its association with acid-base disturbances. The acute exacerbation of COPD may cause severe acidemia, which can lead to myocardial depression, weakness of respiratory muscle, an increase in pro-inflammatory cytokines and so on, exerting a major impact on a poor clinical outcome.15 Metabolic acidosis is a strong predictor of prognosis in critically ill patients.16 AG is commonly used to evaluate acid-base disorders and analyze primary metabolic acidosis.6 High AG metabolic acidosis is a subcategory of metabolic acidosis,9 and therefore, AG may be a useful predictor of adverse clinical outcomes in ICU patients.17 Recent retrospective studies have shown that elevated AG is associated with increased mortality in ICU patients with aortic aneurysm,7 AKI requiring CRRT,9 cardiogenic shock,10 acute pancreatitis11 and hip fractures.12 Moreover, other studies have examined the correlation between AG and mortality in ICU patients. Wang et al18 found that high AG (>14mmol/L) within 48 hours after tissue plasminogen activator (rtPA) treatment in patients with cerebral infarction was linked to significantly higher overall, 1-year, and 4-year mortality. Dafal A.19 and Mehta HJ.20 discovered that high AG levels were associated with increased mortality and longer stays in the MICU. These results suggest that AG can be used to identify ICU patients at risk of mortality early on.
In contrast, the relationship between serum AG and mortality in critically ill patients has yielded inconsistent findings in previous studies. Boniatti et al conducted a single-center prospective study with 175 ICU patients and found no significant difference in AG (P=0.619) or corrected AG (P=0.106) between survivors and non-survivors.21 Mitra et al illustrated that AG has limited value as a sole measure.22 In a large retrospective diagnostic-validation study that included 4159 patients with sepsis, the authors observed that AG was a poor predictor of changes in mortality but may be useful in further risk-stratifying patients for ongoing sepsis care when lactate levels are unavailable.23 However, a meta-analysis16 does not endorse using a single AG measurement for risk stratification in critically ill patients. Differences in study designs, statistical heterogeneity, and the significant variation between patient cohorts could account for the discrepancies in previous reports.
Our study’s subgroup analyses revealed that the association between serum AG and mortality persisted and that sepsis had significant interactions with AG in predicting mortality (P<0.05, Figure 2). Sepsis is a serious life-threatening condition worldwide, with a high risk of death24 that is often complicated by organ dysfunction and acid-base balance disorders. AG is a sensitive indicator of metabolic disturbance, and Zhu et al demonstrated that high AG was significantly associated with increased sepsis mortality risk (P < 0.001).8 Therefore, recognizing an increase in AG levels early is essential to prevent sepsis progression and improve outcomes. However, additional studies are required to investigate the clinical value of AG for early sepsis management.
Limitations
This study is a retrospective cohort study based on the MIMIC IV database, and it has limitations. First, inherent biases may exist because of the retrospective nature of the data. However, we endeavored to screen all patients who met the criteria to avoid this issue. Second, we only measured serum AG for the first admission to the ICU and did not evaluate its dynamic variation, more studies were needed. Finally, although we adjusted for confounding variables, other unknown and underlying factors may still exist. Therefore, considering these considerations, further extensive multicenter prospective studies are necessary to verify the role of serum AG as a prognostic factor for predicting adverse clinical outcomes in critically ill patients with COPD.
Conclusion
Our findings suggest that serum AG is positively associated with all-cause mortality in critically ill patients with COPD. Further studies are needed to support the use of AG clinically for early identification of critically ill COPD patients with higher mortality.
Abbreviations
AG, anion gap; bpm, beats per minute; AKI, acute kidney injury; BNU, blood urea nitrogen; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; CCI, Charlson Comorbidity Index; CI, confidence interval; CRRT, continuous renal replacement therapy; HR, heart rate; HR, hazard ratio; ICU, Intensive Care Unit; MIMIC, Medical Information Mart for Intensive Care; MBP, mean blood pressure; Q, quartile; RR, respiratory rate; Ref, reference; SOFA, sequential organ failure assessment; WBC, white blood cells.
Acknowledgment
We thank Jie Liu, PhD (Department of Vascular and Endovascular Surgery, Chinese PLA General Hospital) for his helpful comments regarding the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2019PT350001), National Natural Science Foundation of China (81960013), Science and Technology Program of Inner Mongolia (NeiCaiKe [2022] No.662), The central government guided local science and technology development fund project (ZYZ20200486).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Serban KA, Pratte KA, Bowler RP. Protein Biomarkers for COPD Outcomes. Chest. 2021;159(6):2244–2253. doi:10.1016/j.chest.2021.01.004
2. Pezzuto A, Tonini G, Ciccozzi M, et al. Functional Benefit of Smoking Cessation and Triple Inhaler in Combustible Cigarette Smokers with Severe COPD: a Retrospective Study. J Clin Med. 2022;12(1):234. doi:10.3390/jcm12010234
3. Iyer AS, Sullivan DR, Lindell KO, Reinke LF. The Role of Palliative Care in COPD. Chest. 2022;161(5):1250–1262. doi:10.1016/j.chest.2021.10.032
4. Moll M, Qiao D, Regan EA, et al. Machine Learning and Prediction of All-Cause Mortality in COPD. Chest. 2020;158(3):952–964. doi:10.1016/j.chest.2020.02.079
5. Makris D, Desrousseaux B, Zakynthinos E, Durocher A, Nseir S. The impact of COPD on ICU mortality in patients with ventilator-associated pneumonia. Respir Med. 2011;105(7):1022–1029. doi:10.1016/j.rmed.2011.03.001
6. Li R, Jin X, Ren J, et al. Relationship of Admission Serum Anion Gap and Prognosis of Critically Ill Patients: a Large Multicenter Cohort Study. Dis Markers. 2022;2022:5926049. doi:10.1155/2022/5926049
7. Gao Y, Hong Z, Shen R, et al. Association between anion gap and mortality of aortic aneurysm in intensive care unit after open surgery. BMC Cardiovasc Disord. 2021;21(1):458. doi:10.1186/s12872-021-02263-4
8. Zhu Y, He Z, Jin Y, et al. Serum Anion Gap Level Predicts All-Cause Mortality in Septic Patients: a Retrospective Study Based on the MIMIC III Database. J Intensive Care Med. 2023;38(4):349–357. doi:10.1177/08850666221123483
9. Zhong L, Xie B, Ji XW, Yang XH. The association between albumin corrected anion gap and ICU mortality in acute kidney injury patients requiring continuous renal replacement therapy. Intern Emerg Med. 2022;17(8):2315–2322. doi:10.1007/s11739-022-03093-8
10. Zhang T, Wang J, Li X. Association Between Anion Gap and Mortality in Critically Ill Patients with Cardiogenic Shock. Int J Gen Med. 2021;14:4765–4773. doi:10.2147/IJGM.S329150
11. Gong F, Zhou Q, Gui C, Huang S, Qin Z. The Relationship Between the Serum Anion Gap and All-Cause Mortality in Acute Pancreatitis: an Analysis of the MIMIC-III Database. Int J Gen Med. 2021;14:531–538. doi:10.2147/IJGM.S293340
12. Zhang XB, Shu WB, Li AB, Lan GH. The Anion Gap and Mortality in Critically Ill Patients with Hip Fractures. Contrast Media Mol Imaging. 2022;2022:1591507. doi:10.1155/2022/1591507
13. Johnson AE, Pollard TJ, Shen L, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035. doi:10.1038/sdata.2016.35
14. Lambden S, Laterre PF, Levy MM, Francois B. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019;23(1):374. doi:10.1186/s13054-019-2663-7
15. Trudzinski FC, Kahnert K, Vogelmeier CF, et al. Combined effects of lung function, blood gases and kidney function on the exacerbation risk in stable COPD: results from the COSYCONET cohort. Respir Med. 2019;154:18–26. doi:10.1016/j.rmed.2019.06.007
16. Glasmacher SA, Stones W. Anion gap as a prognostic tool for risk stratification in critically ill patients - a systematic review and meta-analysis. BMC Anesthesiol. 2016;16(1):68. doi:10.1186/s12871-016-0241-y
17. Gunnerson KJ. Clinical review: the meaning of acid-base abnormalities in the intensive care unit part I - epidemiology. Crit Care. 2005;9(5):508–516. doi:10.1186/cc3796
18. Wang H, Liu C, Xu H, et al. The Association between Serum Anion Gap and All-Cause Mortality in Cerebral Infarction Patients after Treatment with rtPA: a Retrospective Analysis. Dis Markers. 2022;2022:1931818. doi:10.1155/2022/1931818
19. Dafal A, Kumar S, Agrawal S, Acharya S, Nirmal A. Admission Anion Gap Metabolic Acidosis and Its Impact on Patients in Medical Intensive Care Unit. J Lab Phys. 2021;13(2):107–111. doi:10.1055/s-0041-1726568
20. Mehta HJ, Bhanusheli G, Nietert PJ, Pastis NJ. WITHDRAWN: the association between initial anion gap and outcomes in medical intensive care unit patients. J Crit Care. 2012. doi:10.1016/j.jcrc.2012.04.003
21. Boniatti MM, Cardoso PR, Castilho RK, Vieira SR. Is hyperchloremia associated with mortality in critically ill patients? A prospective cohort study. J Crit Care. 2011;26(2):175–179. doi:10.1016/j.jcrc.2010.04.013
22. Mitra B, Roman C, Charters KE, O’Reilly G, Gantner D, Cameron PA. Lactate, bicarbonate and anion gap for evaluation of patients presenting with sepsis to the emergency department: a prospective cohort study. Emerg Med Australas. 2020;32(1):20–24. doi:10.1111/1742-6723.13324
23. Mohr NM, Vakkalanka JP, Faine BA, et al. Serum anion gap predicts lactate poorly, but may be used to identify sepsis patients at risk for death: a cohort study. J Crit Care. 2018;44:223–228. doi:10.1016/j.jcrc.2017.10.043
24. Cecconi M, Evans L, Levy M, Rhodes A. Sepsis and septic shock. Lancet. 2018;392(10141):75–87. doi:10.1016/S0140-6736(18)30696-2
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

