Back to Journals » International Journal of General Medicine » Volume 9
Association between sarcopenia and quality of life in quilombola elderly in Brazil
Authors Sinesio Silva Neto L , Gomes de Oliveira Karnikowski M, Barbosa Osório N, Pereira L , Barbosa Mendes M, Galato D, Barbaresco Gomide L, Chieregato Matheus JP
Received 15 July 2015
Accepted for publication 4 December 2015
Published 19 April 2016 Volume 2016:9 Pages 89—97
DOI https://doi.org/10.2147/IJGM.S92404
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Luiz Sinésio Silva Neto,1–3 Margô GO Karnikowski,2 Neila B Osório,3 Leonardo C Pereira,2 Marcilio B Mendes,1 Dayani Galato,2 Liana B Gomide Matheus,4 João Paulo C Matheus2,4
1School of Medicine, Federal University of Tocantins, Palmas, Tocantins, 2Graduate Program in Health Sciences and Technology, Ceilândia College, University of Brasilia, Federal District, 3Graduate Program in Education, Federal University of Tocantins, Palmas, Tocantins, 4School of Physiotherapy, Ceilândia College, University of Brasília, Federal District, Brazil
Introduction: Currently, there is no single consensual definition of sarcopenia in the literature. This creates a challenge for the evaluation of its prevalence and its direct or indirect impact on the quality of life of elderly populations of different races and ethnicities. Furthermore, no studies as yet have analyzed these variables in populations of elderly subjects of the "quilombola" ethnic group.
Objective: We aimed to verify the association between sarcopenia and quality of life in quilombola elderly using the Baumgartner and the European Working Group on Sarcopenia in Older People (EWGSOP) criteria.
Methods: This was a cross-sectional study of 70 male and female participants (mean age: 65.58±6.67 years). Quality of life was evaluated using the multidimensional 36-item Short-Form Health Survey (SF-36) of the Medical Outcomes Study. Sarcopenia was diagnosed according to the Baumgartner cutoff for appendicular skeletal muscle mass and the criteria recommended by the EWGSOP. Muscle mass and fat mass percentages were analyzed by dual-energy X-ray absorptiometry, while handgrip strength (HGS) was evaluated using a hand-held dynamometer. Physical performance was assessed through a gait speed test.
Results: The prevalence of sarcopenia was 15% according to the Baumgartner cutoff and 10% according to EWGSOP criteria. Quilombola elderly classified as physically active or very active were at least six times less likely to develop sarcopenia than those classified as irregularly active or sedentary. HGS was negatively associated with a diagnosis of sarcopenia according to both sets of criteria. Subjects with sarcopenia reported lower scores than those without the condition on the physical role functioning and bodily pain domains of the SF-36.
Conclusion: In this sample of quilombola elderly, quality of life was negatively associated with sarcopenia, regardless of the classification criteria used. Additionally, the results showed that diagnostic criteria for sarcopenia should include reductions in lean mass in addition to measures of functioning and physical performance because some subjects showed the former symptom without any alteration of the latter two variables. The cutoff value suggested by Baumgartner criteria were less accurate than that specified by the EWGSOP criteria because they do not consider functioning and physical performance. However, Baumgartner criteria were more sensitive in detecting sarcopenia because reductions in lean mass predict alterations in strength and walking speed.
Keywords: sarcopenia, quality of life, elderly, quilombola, vulnerable groups
Introduction
The term sarcopenia comes from the Greek words “sarco”, meaning muscle, and “penia”, meaning loss, and was first used by Irwin Rosenberg.1 This condition was originally described by Evans and Campbell2 and was defined by Evans3 as an age-related reduction in muscle mass. This phenomenon has been increasingly investigated in the literature, and there is now a growing body of research into sarcopenia.
Sarcopenia leads to a reduction in fat-free mass and muscle strength, as well as impaired physical performance.4,5 This condition is also associated with other illnesses such as osteoporosis, osteopenia, obesity, diabetes mellitus type II, and breast cancer, as well as cardiovascular and respiratory diseases, bone fragility, falls, impaired mobility, alterations in glycemic and metabolic control, reduced basal metabolism, and reduced functional capacity.6–8 These conditions may cause functional dependence and increase the likelihood of hospitalization and institutionalization, as well as causing significant health care costs and taking a heavy toll on quality of life.9
According to the literature, there is significant difficulty in estimating the prevalence of sarcopenia10 due to the various techniques used to assess muscle mass, muscle strength, and physical performance, as well as the different diagnostic cutoffs and the variability in the anthropometric and socioeconomic diversity of the populations studied. Therefore, to improve the management of this condition, diagnostic criteria for sarcopenia in different elderly populations should also consider variables such as race and ethnicity.
The association between low levels of lean mass, reduced muscle strength, and poor health-related quality of life (HRQOL) is not exclusive to Caucasian populations. One study demonstrated an association between low lean body mass, reduced mobility and low quality of life in African Americans.11 Additional research has also analyzed changes in muscle mass and strength in elderly individuals of different races and ethnicities.12 These studies found that men lost twice as much muscle strength than women, and Blacks lost 28% more strength than Whites. Leg muscle strength decreased by 3.4% annually in Caucasian males, 4.1% in Black males, 2.6% in Caucasian females, and 3.0% in Black females.
The “quilombola” population is formed by ethnic/racial groups with a particular historical background, specific territorial relations, and self-declared ancestry from Blacks who resisted slavery.13 In addition to their shared genetics, the quilombola people have a strong ethnic group identity, follow a particular form of social organization, and live in predominantly rural areas.14
According to the Palmares Foundation, a federal agency responsible for the registration of quilombola communities, a total of 1,500 such groups are officially recognized in Brazil.15 However, the actual number of quilombola communities is estimated to be ~5,000. As per the global trend, the elderly population of quilombola communities has also increased.14 Although the health of minority populations is a widely recognized priority, few studies have focused on elderly quilombola populations. Investigations of the relationship between health and quality of life in these subjects are especially scarce, and the few existing studies on the topic usually involve stratified samples.15
Although the literature suggests that sarcopenia may have a negative impact on health and HRQOL, little is known regarding the repercussions of this condition on elderly Blacks, especially those who live in quilombola communities.10 As such, the aim of this study was to evaluate the association between sarcopenia and quality of life in elderly individuals from quilombola communities using the Baumgartner and European Working Group on Sarcopenia in Older People (EWGSOP) criteria.
Methods
The sample included adults of both sexes of at least 60 years of age, recruited from the quilombola communities of Malhadinha and Córrego Fundo, located in the rural outskirts of Brejinho do Nazaré, 100 km from Palmas, the state capital of Tocantins. Data were collected over the course of 12 trips to these locations, incurring significant costs in terms of transportation, food, and expendable supplies. All subjects provided written consent for participation. This study was approved by the Research Ethics Committee of the Federal University of Tocantins under protocol number 045/2014. All experimental procedures were performed in accordance with Federal Resolution 466/12.
Procedure
The inclusion criteria for the study were age 60 years or older, residence in the Malhadinha or Córrego Fundo communities (Brejinho de Nazaré, Tocantins), and scores of at least 17 on the Mini-Mental State Examination (MMSE). Exclusion criteria consisted of the following: inability to move without assistance, presence of metallic prostheses, self-reported cardiac or respiratory disorders, self-reported acute pain in the upper or lower limbs, physical disability, as well as a history of stroke, cancerous cachexia, untreated chronic disease or mental illness, severe arthritis, inflammatory diseases, and/or medication-induced anorexia. All interviewers were trained to administer the assessment instruments involved in this study.
Instruments
Socioeconomic questionnaire
This instrument was used to collect data on the socioeconomic status, as well as information on participant age, sex, and education level.
Sample characteristics
Cognitive impairment was investigated using the MMSE. Scores were analyzed as recommended by Brucki et al.16 Physical activity levels were evaluated using the short version of the International Physical Activity Questionnaire (IPAQ), which has already been validated for use in Brazilian populations. This instrument was administered in individual interviews, as recommended for developing countries, and it allowed for the classification of participants as very active, active, infrequently active, or sedentary, according to their scores.17
Anthropometric measurements
Body mass was measured using a digital scale accurate to 0.1 kg (Filizola, São Paulo, Brazil). Height was measured using a wall-mounted stadiometer accurate to 0.1 cm (Cardiomed, Curitiba, Paraná, Brazil). These values were then used to calculate the body mass index (BMI) of each participant. Waist and hip circumference were then measured18 to allow for a calculation of the waist-to-hip ratio (WHR) of each subject.
Appendicular skeletal muscle mass (ASMM) and fat mass percentages were analyzed using a Lunar DPX dual-energy X-ray absorptiometer and the Encore 2013 software. Low ASMM was defined according to the cutoffs described by Baumgartner et al19 (5.45 kg/m2 for women and 7.26 kg/m2 for men). Relative ASMM was calculated by dividing dual-energy X-ray absorptiometry (DEXA)-determined ASMM by the square of participant height.
Physical performance
All participants performed a 3 m walking speed test, in which gait speed was measured in meters per second.20 Performance on this task was analyzed according to the cutoffs recommended by the EWGSOP.4 Speeds of ≤0.8 m/s were considered indicative of impaired physical performance. Handgrip strength (HGS) was measured using a standard dynamometer (Saehan, Masan, South Korea).21 HGS values <30 kg in men and <20 kg in women were considered indicative of mobility limitations.4
Definition of sarcopenia
This study used the definition of sarcopenia provided by the EWGSOP,4 which describes the disorder based on three main factors, which consist of muscle mass, muscle strength, and physical performance. Sarcopenia can be diagnosed based on the presence of reduced walking speed and/or HGS in addition to low ASMM. The criteria proposed by Baumgartner et al,19 however, can be used to diagnose sarcopenia based solely on the presence of reduced ASMM.
Quality of life
Quality of life was investigated using the 36-item Short-Form Health Survey (SF-36) of the Medical Outcomes Study. This instrument has been translated and validated for use in Brazilian populations.22 The SF-36 is a multidimensional questionnaire composed of 36 items, each of which is scored on a rating scale containing two to six response options. The items are distributed into eight domains, which can be grouped into two main categories: physical (physical functioning, bodily pain, general health perceptions, and physical role functioning) and mental (mental health, vitality, social role functioning, and emotional role functioning) health. Each item is scored on a scale ranging from one to six. The questionnaire yields a total score of zero to 100, in which zero corresponds to the “worst” and 100 to the “best” possible health status.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences, version 20.0 (IBM Corporation, Armonk, NY, USA). Categorical variables were first summarized as absolute and relative frequencies, while continuous variables were described as mean values and standard deviations (n=70). The association between exposure and outcome variables (a diagnosis of sarcopenia according to EWGSOP and Baumgartner criteria) was evaluated using chi-square or Fisher’s exact test. Odds ratios and 95% confidence intervals were also calculated. Exposure variables were categorized at the median, in the case of height and weight, or as described in the previous section.
The distribution of quality-of-life scores was analyzed using the Kolmogorov–Smirnov method. Nonparametric Friedman tests were then used to investigate the association between quality of life and a diagnosis of sarcopenia according to Baumgartner and EWGSOP criteria. Once the normality of each variable had been tested, Mann–Whitney U-tests were used to analyze nonparametric variables, while Student’s t-tests for independent samples were used to compare the mean value of parametric variables between subjects with and without sarcopenia. Results were considered significant at P≤0.05.
Results
The sample consisted of 70 elderly quilombola subjects aged between 60 years and 85 years, with a mean age of 65.58±6.67 years. Twenty-six participants lived in the Malhadinha community, while 44 lived in the Córrego Fundo community. The prevalence of sarcopenia in the sample was 10.0% (n=7) according to EWGSOP criteria and 15.7% (n=11) according to the Baumgartner cutoffs.
Prevalence rates per sex are shown in Table 1. Elderly quilombola females were four times more likely than males to receive a diagnosis of sarcopenia according to Baumgartner, but not EWGSOP, criteria. Participants were then divided by their median age into two groups. The prevalence of sarcopenia did not differ between younger and older subjects. Most patients with the disorder were illiterate, although the association between sarcopenia and education level was not found to be significant.
MMSE scores showed that all participants had sufficient intellectual ability to complete the tasks involved in this study. The analysis of physical activity levels showed that most subjects were active to very active, and all sedentary subjects were diagnosed as having sarcopenia according to both sets of criteria. Participants who were active to very active were at least six times less likely to develop sarcopenia than those who were irregularly active or sedentary. These findings suggest that physical activity may be protective against this condition.
When sarcopenia was diagnosed solely on the basis of ASMM levels, subjects with the condition were found to have lower body weight than the remainder of the sample, although the two groups did not differ in height. BMI values suggested that subjects who met both diagnostic criteria for sarcopenia were either normal (EWGSOP: n=5; and Baumgartner: n=6) or underweight (EWGSOP: n=2; and Baumgartner: n=5). Body composition data demonstrated that individuals with sarcopenia had normal waist circumference and fat mass percentage, as well as low-to-moderate cardiovascular risk (CVR). Interestingly, fat mass percentages were found to be elevated in 67.17% (n=47) of the sample. According to Baumgartner criteria, subjects with low-to-moderate CVR were eight times more likely to develop sarcopenia than those with high CVR. Patients with sarcopenia showed low HGS and ASMM values but had normal gait speed.
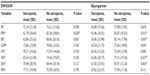
The analysis of quality-of-life assessments showed that subjects with sarcopenia obtained lower scores on the pain and physical aspects domain of the SF-36 than those without the condition, as described in Table 2. Additionally, the social and emotional domains of the SF-36 were influenced by lean mass percentage. A negative correlation was identified between a diagnosis of sarcopenia according to both classification criteria and the following domains of the SF-36: physical role functioning (Baumgartner: P=0.014; and EWGSOP: P=0.012), bodily pain (Baumgartner: P=0.001; and EWGSOP: P=0.001), social role functioning (Baumgartner: P=0.036; and EWGSOP: P=0.042), and emotional role functioning (Baumgartner: P=0.001; and EWGSOP: P=0.002).
Discussion
Age-associated changes in body composition have been investigated by several studies.23 However, the repercussions of these alterations and their impact on the quality of life of elderly subjects have not been entirely elucidated,24 especially in quilombola populations.
Although several methods are available for the assessment of body composition in elderly populations, DEXA is among the most reliable tools for this purpose and is considered the ideal method to diagnose sarcopenia in multiracial patients.25 Unfortunately, its routine use in clinical practice is impractical, especially in small cities or rural areas such as the quilombola communities near Brejinho do Nazaré, in the state of Tocantins.
The results of this study showed that quilombola elderly experienced significant alterations in their body mass, with more than half the sample showing elevated fat mass percentages and 30% being overweight or obese. The sample also showed an elevated prevalence of sarcopenia, although this value was higher when estimated using Baumgartner (15%) than EWGSOP (10%) criteria. The findings described herein corroborate those of previous studies11,26 on the prevalence of sarcopenia in elderly Black populations. However, no studies of this nature had ever been performed in a quilombola community in Brazil. The discrepancies between various diagnostic methods for sarcopenia have been investigated by several studies.27,28 In this investigation, the cutoff value suggested by Baumgartner was less accurate than that specified by the EWGSOP because it does not consider functioning and physical performance, both of which have been found to predict fragility, mortality, mobility incidents, disability, and the risk of institutionalization and hospitalization in elderly populations.10 However, the Baumgartner criteria were more sensitive in detecting sarcopenia because reductions in lean mass predict alterations in strength and walking speed.11 Therefore, additional studies comparing the use of different criteria and cutoff points in this population are required, as is the adaptation of the said criteria and cutoffs to other racial/ethnic groups.27,28 There is an urgent need for a consensus on the best method to diagnose sarcopenia in racial and ethnic groups such as the quilombola population.
The increased likelihood of loss of lean mass in males according to the criteria specified by Baumgartner et al19 may be partly attributed to the reduction in testosterone and growth hormone levels observed with advancing age.29,30 Interestingly, when sarcopenia was diagnosed based on functional capacity in addition to lean mass loss, no significant sex differences in its prevalence were observed. These findings suggest that, although elderly subjects with sarcopenia do show reductions in lean mass, their HGS may be preserved, regardless of their sex.
Unlike most other studies in the literature,27,31 this investigation identified no association between age and a diagnosis of sarcopenia according to either set of criteria. This may be partly explained by the relatively young age of the sample, as well as the fact that all participants were at least 60 years of age. In a recent systematic review, Cruz-Jentoft et al32 found that age was not consistently reported in studies of sarcopenia: while some investigations report mean values for whole samples, others report age ranges or break this variable down into categories, preventing a comprehensive analysis of the relationship between age and sarcopenia.
The high level of physical activity reported by the quilombola population proved to be a protective factor against the development of sarcopenia. This result corroborates the findings of several previous studies9,33,34 on the association between sarcopenia and lifestyle factors in elderly populations, which found that subjects who report little to no physical activity are at higher risk of developing both sarcopenia and disability than those with high activity levels. As such, interventions which aim to promote or maintain high levels of physical activity, such as resistance training, may be a useful tool for the prevention and treatment of sarcopenia.35 These interventions have been found to have a beneficial effect on muscle mass, strength, and physical function.7 Although there is some disagreement in the literature as to the ideal exercise program for subjects with sarcopenia, resistance training has yielded positive results in these populations due to its effects on skeletal muscle hypertrophy.36
All subjects who met both diagnostic criteria for sarcopenia were either normal (EWGSOP: n=5; and Baumgartner: n=6) or underweight (EWGSOP: n=2; and Baumgartner: n=5). This result corroborates the results of previous studies, which reported a negative association between BMI and sarcopenia, whereby subjects with low BMI were more likely to develop the disorder, even in rural elderly populations.37 In the Brazilian population, Da Silva et al38 obtained a similar finding in both men and women and found that social conditions such as low income, low educational levels, loneliness, and lifestyle factors may also be associated with sarcopenia.
HGS was associated with sarcopenia according to both classification criteria, suggesting that the maintenance of HGS may be important for adequate functioning and may have a protective effect against sarcopenia. Studies show that muscle strength decreases more rapidly than muscle mass, suggesting that aging may compromise the quality of muscle tissue.35 Researchers have also found that muscle mass maintenance or gain may not prevent the age-related decline in muscle strength.39 Low HGS value is also a prognostic factor for falls, cognitive impairment, hospitalization, cardiovascular disease, and mortality.39 These findings underscore the importance of prevention and rehabilitation interventions directed at HGS.
Functional independence is crucial for healthy aging and has been found to be associated with both functional capacity and quality of life in elderly populations.40,41 The physical role functioning and bodily pain scores of subjects with sarcopenia (diagnosed according to either classification criteria) were lower than those reported by individuals without the condition. Both domains are part of the physical component of HRQOL. These findings suggest that sarcopenia may have a greater effect on physical health than on mental health. According to the literature, low muscle strength and low muscle mass may both be associated with poor quality of life.42,43 In a study performed by Sayer et al,44 the relationship between HGS and HRQOL was evaluated in 2,987 men and women aged between 59 years and 73 years. HRQOL was evaluated using the SF-36, while a hand-held dynamometer was used to measure HGS. The study found that low HGS was associated with lower scores on the physical functioning, physical role functioning, general health perceptions, vitality, and bodily pain scales of the SF-36 and was therefore related to both sarcopenia and generalized frailty. A comparative study of HRQOL in subjects with “sarco-osteopenia” and healthy adults found that the former obtained lower scores on the physical functioning, vitality, physical role functioning, and emotional role functioning domains than the latter, which is consistent with the impact of sarcopenia on HRQOL.45 Sarcopenia had a negative impact on the quality of life of quilombola subjects, as shown by the correlational analysis performed in this study. As such, future studies may wish to develop a measure of HRQOL specific to sarcopenia.
This study had some limitations, such as the absence of a validated diagnostic protocol for sarcopenia in Brazilian elderly. Additionally, the cross-sectional nature of this investigation precludes the assignment of cause and effect relationships to the variables studied. Nevertheless, our study was able to provide prevalence estimates of sarcopenia in a population that has only been scarcely studied. The advantages of this study include its well-characterized sample of both men and women and its clear geographical focus, as well as the fact that it is the first investigation of sarcopenia in quilombola elderly.
Conclusion
The high prevalence of sarcopenia in quilombola elderly is a public health emergency, not least due to the impact of this condition on quality of life, as shown in this study. Although there does not appear to be a single consensual definition of sarcopenia in the literature, our study showed that, regardless of the diagnostic criteria used, this condition was significantly associated with quality of life.
We also found that diagnostic criteria for sarcopenia should include reductions in lean mass in addition to measures of functioning and physical performance, because some subjects showed the former symptom without any alteration of the latter two. Additionally, all subjects showed adequate physical fitness, reinforcing the need for prophylactic interventions to promote high physical activity levels, because reductions in lean mass and muscle strength are prognostic of impaired physical performance.
In this study, both the EWGSOP and Baumgartner criteria were applied to an elderly quilombola population. Although both were effective in diagnosing sarcopenia, we underscore the need for consensus diagnostic criteria that consider patients’ ethnic and/or racial backgrounds.
This study may serve as a basis for future investigations of the body composition of elderly quilombola subjects, for the development of prevention and rehabilitation strategies for sarcopenia, as well as the elaboration of assessment instruments to measure HRQOL in quilombola elderly with this condition.
Acknowledgments
The authors thank the Mature University Program (Program University of Maturidade-UMA) of the Federal University of Tocantins, the Graduate Program in Health Sciences and Technology of the University of Brasilia, and the Arai Kaminish and Costa Laboratory, Tocantins, Brazil.
Author contributions
Luiz Sinésio Silva Neto contributed to project development, researcher training, data collection, as well as manuscript drafting and revision. Margô GO Karnikowski contributed to data analysis, the description of study results, and manuscript drafting. Neila B Osório was involved in data collection and manuscript drafting. Leonardo C Pereira took part in manuscript drafting. Marcilio B Mendes was involved in data collection. Dayani Galato contributed to data analysis. Liana B Gomide Matheus contributed to manuscript revision. João Paulo C Matheus took part in project design, in the critical reading of the manuscript, and approved the final version of this article. He is also responsible for the accuracy and integrity of this work. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Rosenberg I. Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19–21, 1988. Am J Clin Nutr. 1989;50(5 suppl):1121–1235. | |
Evans WJ, Campbell WW. Sarcopenia and age-related changes in body composition and functional capacity. J Nutr. 1993;123:465–468. | |
Evans W. What is sarcopenia? J Gerontol. 1995;50A(special issue):5–8. | |
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing. 2010;39:412–413. | |
Janssen I. Evolution of sarcopenia research. Appl Physiol Nutr Metab. 2010;35:707–712. | |
Dixit V, Dhanwal D. Handgrip strength as a measure of sarcopenia in type 2 diabetes mellitus. J Adv Res Med. 2014;1(1):10–14. | |
Landi F, Cruz-Jentoft AJ, Liperoti R, et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from il SIRENTE study. Age Ageing. 2013;42(2):203–209. | |
Morley JE, Malmstrom TK. Frailty, sarcopenia, and hormones. Endocrinol Metab Clin North Am. 2013;42(2):391–405. | |
Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. Sarcopenic obesity and risk of cardiovascular disease and mortality: a population-based cohort study of older men. J Am Geriatr Soc. 2014;62(2):253–260. | |
Beaudart C, Rizzoli R, Bruyère O, Reginster JY, Biver E. Sarcopenia: burden and challenges for public health. Arch Public Health. 2014;72:45. | |
Malmstrom TK, Miller DK, Herning MM, Morley JE. Low appendicular skeletal muscle mass (ASM) with limited mobility and poor health outcomes in middle-aged African Americans. J Cachexia Sarcopenia Muscle. 2013;4(3):179–186. | |
Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass and quality in older adults: The Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–1064. | |
Volochko A, Batista LE. Saúde nos quilombos. [Health in quilombos]. São Paulo: Instituto de Saúde; 2009. | |
Bezerra VM, Andrade AC, de Souza CL, César CC, Caiaffa WT. Health survey in Quilombola communities (descendants of Afro-Brazilian slaves who escaped from slave plantations that existed in Brazil until abolition in 1888) in Vitória da Conquista in the state of Bahia (COMQUISTA Project), Brazil: methodological aspects and descriptive analysis. Cad. Saúde Pública. 2013;29(9):1889–1902. | |
Freitas DA, Caballero AD, Marques AS, et al. Health and quilombolas communities. Rev Cefac. 2011;13(5):937–943. | |
Brucki SMD, Nitrini R, Caramelli P, Bertolucci PH, Okamoto IH. Suggestions for utilization of the mini-mental state examination in Brazil. Arq Neuropsiquiatr. 2003;61(3B):777–781. | |
Matsudo SM, Matsudo VKR, Barros Neto TL. Atividade física e envelhecimento: aspectos epidemiológicos. [Physical activity and aging: epidemiological]. Rev Bras Med Esporte. 2001;7:2–13. | |
Lerario DDG, Gimeno SG, Franco LJ, Iunes M, Ferreira SRG. Grupo de Estudos em Diabetes na Comunidade Nipo-brasileira. Excesso de peso e gordura abdominal para a síndrome metabólica em nipo-brasileiros. [Group of Diabetes Studies in Community Nipo-Brazilian. weight and abdominal fat excess for metabolic syndrome in Japanese-Brazilians]. Rev Saúde Pública. 2002;36:4–11. | |
Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–763. | |
Nakano MM. Versão brasileira da short physical performance battery – SPPB: adaptação cultural e estudo da confiabilidade [dissertação]. [Brazilian version of the short physical performance battery - SPPB: cultural adaptation and reliability study of [dissertation]]. Campinas, SP: Universidade Estadual de Campinas; 2007. | |
Go SW, Cha YH, Lee JA, Park HS. Association between sarcopenia, bone density, and health-related quality of life in Korean men. Korean J Fam Med. 2013;34:281–288. | |
Ciconelli, RM. Tradução para o português e validação do questionário genérico de avaliação de qualidade de vida Medical outcomes study 36-item short-form health survey (SF-36), Tese (doutorado). [Translation into Portuguese and validation of the generic questionnaire to evaluate quality of life Medical outcomes study short-form health survey 36-item (SF-36), Thesis (PhD)]. Universidade Federal de São Paulo, São Paulo, 1997. | |
Argilés JM, Busquets S, Stemmler B, López-Soriano FJ. Cachexia and sarcopenia: mechanisms and potential targets for intervention. Current Opinion in Pharmacology. 2015;22:100–106. | |
Tanimoto Y, Watanabe M, Sun W, et al. Association between sarcopenia and higher-level functional capacity in daily living in community-dwelling elderly subjects in Japan. Arch Gerontol Geriatr. 2012;55(2):e9–e13. | |
Harris-Love MO, Adams B, Hernandez HJ, DiPietro L, Blackman MR. Disparities in the consequences of sarcopenia: implications for African American Veterans. Front Physiol. 2014;5:250. | |
Van Kan GA. Epidemiology and consequences of sarcopenia. J Nutr Health Aging. 2009;13(8):708–712. | |
Volpato S, Bianchi L, Cherubini A, et al. Prevalence and clinical correlates of sarcopenia in community-dwelling older people: application of the EWGSOP definition and diagnostic algorithm. J Gerontol A Biol Sci Med Sci. 2013;69(4):438–446. | |
Bijlsma AY, Meskers CGM, Ling CHY, et al. Defining sarcopenia: the impact of different diagnostic criteria on the prevalence of sarcopenia in a large middle aged cohort. Age. 2013;35:871–881. | |
Landi F, Liperoti R, Fusco D, et al. Sarcopenia and mortality among older nursing home residents. J Am Med Dir Assoc. 2012;13(2):121–126. | |
Silva TAA, Junior AF, Pinheiro MM, Szejnfeld VL. Sarcopenia Associada ao Envelhecimento: Aspectos Etiológicos e Opções Terapêuticas. [Sarcopenia associated with aging: Etiologic Aspects and Therapeutic Options]. Rev Bras Reumatol. 2006;46(6):391–397. | |
Gariballa S, Alessa A. Sarcopenia: prevalence and prognostic significance in hospitalized patients. Clin Nutr. 2013;(5):32. | |
Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748–759. | |
Montero-Fernandez N, Serra-Rexach JA. Role of exercise on sarcopenia in the elderly. Eur J Phys Rehabil Med. 2013;49(1):131–143. | |
Sayer AA, Robinson SM, Patel HP, Shavlakadze T, Cooper C, Grounds MD. New horizons in the pathogenesis, diagnosis and management of sarcopenia. Age Ageing. 2013;42:145–150. | |
Denison HJ, Cooper C, Sayer AA, Robinson, SM. Prevention and optimal management of sarcopenia: a review of combined exercise and nutrition interventions to improve muscle outcomes in older people. Clin Interv Aging. 2015;10:859. | |
Iolascon G, Di Pietro G, Gimigliano F, et al. Physical exercise and sarcopenia in older people: position paper of the Italian Society of Orthopaedics and Medicine (OrtoMed). Clin Cases Mineral Bone Metabol. 2014;11(3):215–221. | |
Wu CH, Chen KT, Hou MT, et al. Prevalence and associated factors of sarcopenia and severe sarcopenia in older Taiwanese living in rural community: the Tianliao Old People study 04. Geriatr Gerontol Int. 2014;14(S1):69–75. | |
Da Silva AT, de Oliveira Duarte YA, Ferreira Santos JL, Wong R, Lebrão ML. Sarcopenia according to the European Working Group on Sarcopenia in Older People (EWGSOP) versus dynapenia as a risk factor for disability in the elderly. J Nutr Health Aging. 2014;18:547–553. | |
Roberts HC, Denison HJ, Martin HJ, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40(4):423–429. | |
Silva Neto LS, Karnikowiski MG, Tavares AB, Lima RM. Association between sarcopenia, sarcopenic obesity, muscle strength and quality of life variables in elderly women. Braz J Phys Ther. 2012;16(5):360–367. | |
Mijnarends DM, Meijers JMM, Halfens RJG, Luiking, YC, Verlaan S, Schols JMGA. P343 Quality of life is decreased in community-dwelling older people with sarcopenia. Eur Geriatr Med. 2014;5:S189. | |
Ciolac EG, Rodrigues-da-Silva JM. Resistance Training as a Tool for Preventing and Treating Musculoskeletal Disorders. Sports Medicine. Epub 2016 Feb 25. | |
Iannuzzi-Sucich M, Prestwood KM, Kenny AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol A Biol Sci Med Sci. 2002;57:M772–M777. | |
Sayer AA, Syddall HE, Martin HJ, Dennison EM, Roberts HC, Cooper C. Is grip strength associated with health-related quality of life? Findings from the Hertfordshire Cohort Study. Age Ageing. 2006;35:409–415. | |
Kull M, Kallikorm R, Lember M. Impact of a new sarco-osteopenia definition on health-related quality of life in a population-based cohort in Northern Europe. J Clin Densitom. 2012;15:32–38. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.