Back to Journals » ClinicoEconomics and Outcomes Research » Volume 14
Association Between Bio-Fermentation Derived Hyaluronic Acid and Healthcare Costs Following Knee Arthroplasty
Authors Nicholls M , Niazi F, Nelson WW , Lau E , Kurtz SM, Ong KL
Received 9 November 2021
Accepted for publication 13 August 2022
Published 30 August 2022 Volume 2022:14 Pages 575—585
DOI https://doi.org/10.2147/CEOR.S347512
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Video abstract of "Association between Bio-HA and Healthcare Costs following KA" [ID 347512].
Views: 200
Mathew Nicholls,1 Faizan Niazi,2 Winnie W Nelson,2 Edmund Lau,3 Steven M Kurtz,4 Kevin L Ong4
1Virginia Mason Orthopaedics and Sports Medicine, Seattle, WA, USA; 2Ferring Pharmaceuticals Inc, Parsippany, NJ, USA; 3Exponent, Inc, Menlo Park, CA, USA; 4Exponent, Inc, Philadelphia, PA, USA
Correspondence: Kevin L Ong, Exponent, Inc, Philadelphia, PA, USA, Tel +1 215 594-8800, Email [email protected]
Background: Limiting access to intra-articular knee injections, including hyaluronic acid (HA), has been advocated as a cost-containment measure in the treatment of knee osteoarthritis. The association between presurgical injections and post-surgical complications such as early periprosthetic joint infection and revision remained to be investigated. This study evaluated pre- and post-surgical costs and rates of post-surgical complications in knee arthroplasty (KA) patients with or without prior HA use.
Methods: Commercial and Medicare Supplemental Claims Data (IBM MarketScan Research Databases) from January 1, 2012 to December 31, 2018 were used to identify unilateral KA patients. Those who completed a course of bio-fermentation derived HA (Bio-HA) as the first-line HA therapy comprised of the test group (n = 4091), while the control group did not use HA prior to KA (n = 118,659). Using multivariable regression with propensity score (PS) weighting, overall healthcare costs, readmission rates, and revision rates were assessed at six months following KA.
Results: Healthcare costs following KA were significantly lower for the Bio-HA group ($10,021 ± $22,796) than No HA group ($12,724 ± $32,966; PS p < 0.001). Bio-HA patients had lower readmission rates (8.9% vs 14.0%; PS p < 0.001) and inpatient costs per readmitted patient ($43,846 ± $50,648 vs $50,533 ± $66,150; PS p = 0.005). There were no differences in revision rate for any reason (Bio-HA: 0.78% vs No HA: 0.67%; PS p = 0.361) and with PJI (Bio-HA: 0.42% vs No HA: 0.33%; PS p = 0.192). Costs in the six months up to and including the KA were similar for both groups (Bio-HA: $49,759 ± $40,363 vs No HA: $50,532 ± $43,183; PS p = 0.293).
Conclusion: Bio-HA use prior to knee arthroplasty did not appear to increase overall healthcare costs in the six months before and after surgery. Allowing access to HA injections provides a non-surgical therapeutic option without increasing cost or risk of post-surgical complications.
Keywords: bio-fermentation derived hyaluronic acid, healthcare costs, intra-articular hyaluronic acid, knee arthroplasty, readmissions
Introduction
The treatment options for knee osteoarthritis (OA) range from non-invasive medical management, to minimally invasive therapies such as intra-articular injections, to surgical inventions like knee arthroplasty (KA),1 depending on the stage and progression of OA, along with the patient’s pain levels and function. Primary KA is recognized as providing substantial improvement in pain, function, and overall health-related quality of life in the majority of patients,2 but the appropriateness of non-arthroplasty treatments continues to be debated.1,3 The costs of non-arthroplasty treatments leading up to KA, such as those for opioids, physical therapy, hyaluronic acid (HA) injections, and corticosteroid injections, have been examined.4–8 Some of those studies concluded that limiting the use of some of these interventions may help reduce healthcare costs,4–6 despite evidence that HA contributed less than 2% of knee OA-related costs among KA patients. Moreover, others have found that HA was associated with a large reduction in knee OA-related healthcare costs for patients who progressed to total knee arthroplasty.8 HA patients have also been found to have a 15-month delay in the peak healthcare spend related to the KA;7 however, it is unclear whether HA impacts post-surgical costs.
HA has been shown to provide improved joint function and mobility,9,10 particularly with higher molecular HA.11–15 HA products with an average molecular weight of at least 3000 kDa were found to provide favorable efficacy results than products of an average molecular weight of less than 3000 kDa.11 Unlike low molecular weight HA, high molecular weight HA also exceeded the minimal clinically important improvement threshold or minimal important difference for pain relief.12,14 There are several mechanisms in which HA injections may provide clinical benefit in knee OA, with chondroprotection being the most frequently reported mechanism.15 HA therapy is also reported to stimulate proteoglycan and glycosaminoglycan synthesis and provide anti-inflammatory, mechanical, subchrondral, and analgesic effects. The safety profile differences between bio-fermentation derived HA (Bio-HA) and avian-derived HA are also unclear,11,15 as others have found that the potential risk of localized reactions may not be greater for HA of avian origin.16 In terms of clinical outcomes, patients who used Bio-HA have been observed to have a longer time to KA than patients who used non-Bio-HA therapies.17
Previous researchers have questioned whether presurgical injections may be associated with complications after TKA, including early periprosthetic joint infection (PJI) and revision.18–21 Claims database studies have observed an association between intra-articular injections and short-term PJI within six months post-KA,18–20 albeit without evaluating the type of injection or adjusting for potentially confounding surgical factors. For example, prior knee arthroscopy has also been implicated with increased risk of PJI after KA.22 On the other hand, others have found that there was no association between the administration of HA within four months of TKA and the risk of PJI up to 24 months after surgery, after considering the differences in patient mix and many other risk factors.21 The costs of treating PJI are high, as revision KA for PJI patients has the longest length of stay and incur higher costs than revisions for any other diagnosis, except periprosthetic fracture.23
With suggestions that HA injections prior to KA add pre-surgical costs to the healthcare system and increase the post-surgical risk of PJI, we tested the hypothesis that KA patients with prior Bio-HA use incur higher healthcare costs both before and following KA and have higher rates of readmissions and revisions.
Methods
Commercial and Medicare Supplemental Claims Data (IBM MarketScan Research Databases, IBM Corporation, Somers, NY) from January 1, 2012 to December 31, 2018 were used to compile a dataset for knee OA patients who underwent KA with or without use of HA injections prior to KA. The commercial portion of the dataset is constructed by collecting data from employers and health plans, which encompasses employees, spouses, and dependents covered by employer-sponsored private health insurance. The Medicare Supplemental portion consists of data from retirees with Medicare supplemental insurance paid by employers, including Medicare-covered and employer-paid portions, as well as out-of-pocket expenses. The dataset contains service-level claims for inpatient and outpatient services, and outpatient prescription drugs, including claims for mail order prescriptions and specialty pharmacies. The data is fully de-identified with a unique identifier for each enrollee to allow for tracking of beneficiary-level claims over time.
Knee OA patients were identified by International Classification of Diseases (ICD) diagnosis codes (Supplementary Table 1), from which unilateral KA patients were included in the study based on those with Current Procedural Terminology (CPT) procedure codes 27446 and 27447. The inclusion criteria were as follows: 1) at least 18 years old; 2) at least six months claim history pre- and post-KA with continuous enrollment; and 3) known laterality for KA (using modifier code for left or right side). The test group was then determined based on the use of bio-fermentation derived HA (Euflexxa; Ferring Pharmaceuticals Inc., Parsippany, NJ) prior to the KA (“Bio-HA group”), while the control group was those without any prior HA use (“No HA” “group”) (Supplementary Table 1). Since the dataset included claims starting January 1, 2012 and patients needed to have at least six months of claim history both pre-KA and post-KA, the index KA procedures were between July 1, 2012 and June 30, 2018. Bio-HA must be the first-line HA therapy used with no other HA between enrollment or start of the data period and the KA. Included Bio-HA patients were also required to have exactly three Bio-HA injections within a six-week period, in the same knee that was subsequently operated on (matching Bio-HA and KA laterality). The exclusion criteria were as follows: 1) unknown laterality for KA; 2) without pharmacy benefits in the six months pre- and post-KA; 3) with non-Bio-HA treatment prior to KA; 4) with Bio-HA without concurrent CPT 20610 or 20611 or without concurrent knee OA diagnosis; and 5) with revision KA prior to primary KA. For the Bio-HA patients, additional exclusion criteria were as follows: 1) with unknown laterality to any of their Bio-HA injections during the index Bio-HA treatment; 2) without completed course of Bio-HA treatment during the index Bio-HA treatment (less than three per knee within a six-week period); 3) who exceeded the course of Bio-HA treatment during the index Bio-HA treatment (more than three per knee within a six-week period); and 4) without matching laterality for the knee with the completed index Bio-HA treatment and the KA. A total of 419,714 KA patients were initially identified, of which 163,051 patients did not have the requisite six-month claim history both before and after the KA (Figure 1). Of the remaining 256,643 patients, a final group of 4091 Bio-HA patients and 118,659 No HA patients met the remaining inclusion and exclusion criteria, with stepwise exclusion of 32,576 patients without pharmacy benefit, 56,049 patients with prior non-Bio-HA use, 332 patients with prior non-knee OA Bio-HA use, 37,815 with unknown or incomplete laterality (KA or Bio-HA) or incomplete or exceeded Bio-HA treatment courses, and 7121 with bilateral KA.
 |
Figure 1 Patient attrition flowchart. |
Based on a follow-up of six months following KA, the overall healthcare costs (adjusted to Jan 2019 medical service consumer price index) were evaluated. This included all medical and facility claims from the physician office, urgent care, inpatient hospital, outpatient hospital, emergency room, ambulatory surgical center, pharmacy, and outpatient facilities. The six-month period was based on a previously observed association between intra-articular injections and short-term PJI within six months post-KA.18–20 Readmission rates were determined during this follow-up, along with the corresponding primary procedure performed and costs of the inpatient services. Revision for any reason and revision with PJI as a diagnosis at six months were also assessed. The overall healthcare costs in the six months up to and including the KA were also compared between the Bio-HA and No HA groups. Univariate analysis was conducted using t-test for the cost comparisons and Chi-square test for the rate comparisons. Multivariable statistics with and without propensity score (PS) weighting were performed to compare the costs, readmission rates, and revision rates. The multivariable analysis for both the PS- and non-PS weighted models adjusted for age, gender, census region, Charlson comorbidity index, diabetes, obesity, heart disease, renal failure, and year of KA, along with use of knee imaging, physical therapy (with knee OA diagnosis), knee brace, knee arthroscopy, and intra-articular corticosteroids in the six months prior to KA. In the PS-weighted model, the PS was used to reweight the populations by creating a pseudo-population where the treatment assignment is independent of the observed covariates. Propensity score for the use of Bio-HA before KA was based on the probability of receiving Bio-HA accounting for the above variables. Patients who did not fall within the overlapping range of PS in the Bio-HA (n = 2) and No HA (n = 79) groups were excluded from the multivariable regression analysis with PS weighting.
Results
The Bio-HA and No HA groups had similar patient characteristics at the time of KA (Table 1). Females comprised a greater percentage of the KA patients (Bio-HA: 61.5%; No HA: 58.2%). Most patients were under 65 years (Bio-HA: 69.7%; No HA: 67.7%) with the largest groups aged 60–64 years (Bio-HA: 27.8%; No HA: 28.8%) and 55–59 years (Bio-HA: 22.3%; No HA: 22.1%). Patients were predominantly from the South (Bio-HA: 40.8%; No HA: 39.3%) and Midwest (Bio-HA: 31.4%; No HA: 32.4%) regions. Regarding comorbidities, most patients had a Charlson comorbidity score of 0. 54.5% of the Bio-HA cohort had a score 0, while 27.5% had a score of 1–2, 9.0% with 3–4, and 9.0% with at least 5. 52.4% of the No HA cohort had a score of 0, while 30.4% had a score of 1–2, 8.9% with 3–4, and 8.3% with at least 5. A diagnosis of heart disease was present for 44.1% of the Bio-HA group and 40.5% of the No HA group in the six months prior to KA, as was obesity in about one-third of the patients (Bio-HA: 30.2%; No HA: 31.4%) and diabetes in about one-fifth of the patients (Bio-HA: 21.4%; No HA: 22.7%). Renal failure diagnosis was identified in 4.8% of both groups.
 |
Table 1 Patient Characteristics for the Bio-Fermentation Derived Hyaluronic Acid (Bio-HA) Group and No Hyaluronic Acid (No HA) Group |
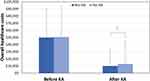
The overall healthcare costs in the six months following KA were significantly lower by about $2700 per patient for the Bio-HA group ($10,021 ± $22,796) than No HA group ($12,724 ± $32,966; univariate p < 0.001) (Figure 2), which corresponded to 20% lower adjusted costs for the Bio-HA group without and with PS weighting (p < 0.001 for both) (Table 2). Fewer Bio-HA patients were readmitted with inpatient visits following KA (8.9% vs 14.0%; univariate p < 0.001). The odds for the Bio-HA group were 38% lower without PS weighting (p < 0.001) and 39% lower with PS weighting (p < 0.001). The corresponding mean inpatient costs per readmitted patient were also significantly lower by about $6700 for the Bio-HA patients ($43,846 ± $50,648 vs $50,533 ± $66,150; univariate p = 0.011). This corresponded to lower adjusted costs for the Bio-HA by 16% (p = 0.002) without PS weighting and by 14% (p = 0.005) with PS weighting.
 |
Table 2 Healthcare Cost Comparisons in the Six Months Following Knee Arthroplasty for the Bio-Fermentation Derived Hyaluronic Acid (Bio-HA) Group and No Hyaluronic Acid (No HA) Group |
Contralateral KA was the most frequent primary procedure performed in both groups when readmitted. This comprised 30.0% of readmissions in the Bio-HA group (or 2.9% of all readmitted and non-readmitted patients) and 50.6% of readmissions in the No HA group (or 7.6% of all readmitted and non-readmitted patients) (Table 3). Knee arthrotomy was the second most frequent primary procedure performed in both groups when readmitted, representing 6.8% of readmissions in the Bio-HA group (or 0.66% of all readmitted and non-readmitted patients) and 4.0% of readmissions in the No HA group (or 0.60% of all readmitted and non-readmitted patients). There was no significant difference in short-term revision for any reason between groups (Bio-HA: 0.78% vs No HA: 0.67%) (univariate p = 0.409; without PS weighing p = 0.340; with PS weighting p = 0.361). No differences in the short-term revision with PJI were observed (Bio-HA: 0.42% vs No HA: 0.33%) (without PS weighing p = 0.328; with PS weighting p = 0.192). Costs in the six months up to and including the KA, as well as cost of HA, were also not observed to be higher for the Bio-HA group ($49,759 ± $40,363 vs $50,532 ± $43,183; univariate p = 0.233; without PS weighing p = 0.204; with PS weighting p = 0.293).
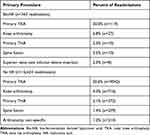 |
Table 3 Top Primary Procedures During the Readmissions |
Discussion
Our study found lower healthcare costs post-surgery for KA patients who had prior use of Bio-HA, which was driven primarily by fewer readmissions and lower inpatient costs. There were also no higher risks for the Bio-HA patients in terms of short-term revision for any reason or with PJI. Bio-HA patients did not have added costs leading up to and including the KA compared to No HA patients, despite their added cost from the Bio-HA.
The present study found fewer Bio-HA patients were readmitted within six months, correlating with a reduced per-patient inpatient cost of approximately $6700. Conflicting studies have reported the association of intra-articular knee injection use before KA with PJI risk.18–21 A study of Medicare total knee arthroplasty (TKA) patients identified a higher incidence of PJI at 3 and 6 months after TKA when a knee injection was performed with less than 3 months to the TKA, but the authors were unable to differentiate between specific types of injections.19 Bedard et al examined PJI outcomes in a cohort of 83,684 TKA patients and found that patients who received pre-operative injections within 6 or 7 months before the TKA had greater odds of developing PJI within 6 months post-TKA than patients who did not receive an injection.18 However, the analysis was unable to identify the anatomic site of injection nor the specific type of injection. Another study reported that preoperative CS or HA injections within three months before the TKA increased the risk of PJI, but there was no difference in risk with multiple injections compared with a single injection.20 Conversely, Kurtz et al found that intra-articular HA injections given within four months prior to TKA were not associated with the risk of PJI up to 24 months after surgery.21 Moreover, the present study found no increased revision risk at 6 months for the Bio-HA group compared to No HA group. The risk of revision with PJI was also comparable in both groups, suggesting that there was no increased PJI risk requiring surgical intervention for the Bio-HA group. Contralateral KA was also found to be the more frequent procedure performed in both groups, although the rate appeared to be lower for the Bio-HA group. This may be a key driver for the lower costs post-KA in the Bio-HA group. The study design did not permit an assessment of any potential causal relationship between Bio-HA and delaying contralateral KA. However, HA patients have been reported to be associated with a delay to their first KA.7,8,17,24,25
Some researchers have suggested that limiting access to knee injections, including HA, prior to KA will reduce healthcare costs.5,18 However, we did not find higher costs in the six months leading up to and including the KA procedure for the Bio-HA group than the no HA group, despite the added HA costs in the Bio-HA group. Concoff et al also reported lower median knee OA-related healthcare costs for patients who received HA before their TKA ($860.24) compared to those who did not receive HA before their TKA ($2,659.49).8 It may be that the Bio-HA patients were using fewer opioids and corticosteroids and therefore not experiencing any associated adverse events with opioids and corticosteroids after completing their Bio-HA treatment course, but this needs to be investigated further for our cohort. The use of HA has been reported by others to reduce the need for analgesic or rescue medication or corticosteroids at six months by others,10,26,27 and may even extend out to 12 months.28 Wilson and coworkers also found that TKA patients who received two or more HA injections in the year before TKA had significantly lower odds of becoming chronic opioid users, in terms of filling opioid prescriptions for at least 120 pills or at least 10 opioid prescriptions within 90 days to 1 year postoperatively.29 Niazi et al further observed a 54% reduction in the number of opioid users at 6 months after receiving a HA injection.30 Almost 80% of HA patients also did not require additional corticosteroid injections during that six-month period.
Limitations
Information derived from administrative claims data could not determine the severity of OA prior to KA. The impact, however, is minimized by the study design because the inclusion of only KA patients introduced a proxy restriction to the most severe patients who needed surgical intervention. This study only evaluated short-term costs within six months following KA; it is unclear if lower costs for the Bio-HA group will continue with longer follow-up. Our study was limited to Bio-HA patients and the findings may not be generalizable to patients who are treated with HA products other than Bio-HA prior to KA. Conflicting data have been reported on the relative risk of localized reactions for Bio-HA and avian-derived HA,11,15,16 which could have an impact on the costs. Due to the observational nature of the study design, we cannot attribute causation of the differences to Bio-HA. However, our study demonstrated that prior use of Bio-HA did not correspond to an increase in six-month pre-arthroplasty costs nor six-month revision rates. Moreover, the Bio-HA patients were observed to have lower overall healthcare and inpatient costs at six months post-surgery. It is unclear whether post-surgical costs may be associated with pre-surgical costs as this was not adjusted for the comparisons of post-surgical costs. Despite this uncertainty, the present study did not find any significant differences in costs in the six months up to and including the KA between the Bio-HA and no HA groups. While the study population included patients over 65 years, these results may not be generalizable to Medicare patients because the study cohort had private insurance with Medicare supplemental insurance. The study did not exclude patients enrolled in capitated health plans or Health Maintenance Organizations (HMOs), nor differentiate between those with and without Medicare supplemental insurance as the perspective was the cost to the insurer rather than patient costs. Moreover, the payments vary depending on the program type and whether the beneficiary has multiple coverages and other special insurance situations. However, the dataset did not contain sufficient information to be able to account for this. It is unclear if the findings would differ between those patients.
Conclusions
With the ongoing debate about healthcare cost containment by limiting HA use, the analysis from the present study did not support the hypothesis that Bio-HA use prior to knee arthroplasty was associated with increased overall healthcare costs in the six months before and after surgery. Instead, those patients were found to have fewer readmissions and lower inpatient costs in the six-month post-operative period compared to patients without prior HA therapy. It was also notable that there were no differences in overall healthcare costs in the six months leading up to and including the surgery, despite additional HA costs for the Bio-HA patients. No added risks for Bio-HA patients in terms of short-term revision for any reason or with PJI were also observed. Limiting access to HA injections may divert patients to other non-surgical treatments that may not provide equivalent clinical benefits and/or introduce additional risks.
Ethics Statement/Ethics Waiver
This study was based on a data set that is available for purchase. The data set was de-identified, did not involve human subject research, and therefore did not require oversight by an institutional review board. Studies involving the use of publicly available databases that do not include personal identifying information have been determined by an IRB (Exponent) to be exempt, with a waiver of approval. Such studies meet the criteria stipulated in the Code of Federal Regulations, Title 45, Part 46, section 46.101(b)(4), which states that “…(b) Unless other required by department or agency heads, research activities in which the only involvement of human subjects will be in one or more of the following categories are exempt from this policy: … (4) Research, involving the collection or study of existing data, documents, records, pathological specimens, or diagnostic specimens, if these sources are publicly available or if the information is recorded by the investigator in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects.”
Funding
Exponent, Inc. received funding from Ferring Pharmaceuticals Inc. for this study. Two of the authors (FN, WNN) are employees of the study sponsor and were involved in the design of the study, interpretation of data, critical revision of the manuscript, and the decision to submit the report for publication. The study sponsor was not involved in the initial collection and analysis of the data.
Disclosure
K Ong is an employee and shareholder of Exponent, a scientific and engineering consulting firm. Exponent has been paid fees for K Ong’s consulting services on behalf of Ferring Pharmaceuticals, during the conduct of the study; Exponent has been paid fees for K Ong’s consulting services on behalf of Bioventus, Medtronic, Stryker Orthopaedics, Sanofi, Pacira Pharmaceuticals, Paradigm Spine, St. Jude Medical, Relievant Medsystems, International Society for the Advancement of Spine Surgery, SI-Technology, LLC; Exponent has been paid fees for K Ong’s litigation consulting services on behalf of Zimmer Biomet, Joerns Healthcare, SpineFrontier, Ethicon, DJO, Ossur, Karl Storz Endoscopy-America, Rex Medical, Smith & Nephew and Covidien, outside the submitted work.
S Kurtz reports grants from Ferring Pharmaceuticals, during the conduct of the study; grants from Stryker, Zimmer Biomet, Invibio, Wright Medical Technology, Ceramtec, Celanese, Ferring Pharmaceuticals, Formae, Lima Corporate, SINTX Technologies, Orthoplastics, Osteal Therapeutics, 3Spine, DJO Global, Carbofix, DePuy Synthes; is an employee and shareholder of Exponent, Inc, a scientific and engineering consulting firm. Exponent has been paid fees by companies and suppliers for S Kurtz consulting services on behalf of such companies and suppliers outside the submitted work.
F Niazi reports being employed by Ferring Pharmaceuticals Inc.
W Nelson was an employee of Ferring Pharmaceuticals.
E Lau reports E Lau’s employer, Exponent Inc., received payment for consulting and other services to Ferring Pharmaceutical, Osteal Therapeutic, Ceramtec Inc. and Relievant Medsystem Inc., outside the submitted work.
References
1. American Academy of Orthopaedic Surgeons. Treatment of Osteoarthritis of the Knee. Evidence-based Guideline; 2013. Available from: https://www.aaos.org/globalassets/quality-and-practice-resources/osteoarthritis-of-the-knee/osteoarthritis-of-the-knee-2nd-editiion-clinical-practice-guideline.pdf.
2. Rankin EA, Alarcon GS, Chang RW, Cooney LM. NIH consensus statement on total knee replacement. NIH Consens State Sci Statements. 2003;20(1):1–34.
3. American Academy of Orthopaedic Surgeons. Appropriate use criteria for non-arthroplasty treatment of osteoarthritis of the knee; 2013. Available from: https://www.aaos.org/globalassets/quality-and-practice-resources/osteoarthritis-of-the-knee/auc-non-arthroplasty-treatment-osteoarthritis-knee.pdf.
4. Bedard NA, Dowdle SB, Anthony CA, et al. The AAHKS clinical research award: what are the costs of knee osteoarthritis in the year prior to total knee arthroplasty? J Arthroplasty. 2017;32(9S):S8–S10e11. doi:10.1016/j.arth.2017.01.011
5. Cohen JR, Bradley AT, Lieberman JR. Preoperative interventions and charges before total knee arthroplasty. J Arthroplasty. 2016;31(12):2730–2735 e2737. doi:10.1016/j.arth.2016.05.048
6. Weick JW, Bawa HS, Dirschl DR. Hyaluronic acid injections for treatment of advanced osteoarthritis of the knee: utilization and cost in a national population sample. J Bone Joint Surg Am. 2016;98(17):1429–1435. doi:10.2106/JBJS.15.01358
7. Malanga G, Niazi F, Kidd VD, et al. Knee osteoarthritis treatment costs in the medicare patient population. Am Health Drug Benefits. 2020;13(4):144–153.
8. Concoff A, Niazi F, Farrokhyar F, Alyass A, Rosen J, Nicholls M. Delay to TKA and costs associated with knee osteoarthritis care using intra-articular hyaluronic acid: analysis of an administrative database. Clin Med Insights Arthritis Musculoskelet Disord. 2021;14:1179544121994092. doi:10.1177/1179544121994092
9. Altman RD, Rosen JE, Bloch DA, Hatoum HT, Korner P. A double-blind, randomized, saline-controlled study of the efficacy and safety of EUFLEXXA for treatment of painful osteoarthritis of the knee, with an open-label safety extension (the FLEXX trial). Semin Arthritis Rheum. 2009;39(1):1–9. doi:10.1016/j.semarthrit.2009.04.001
10. Waddell DD, Bricker DC. Clinical experience with the effectiveness and tolerability of hylan G-F 20 in 1047 patients with osteoarthritis of the knee. J Knee Surg. 2006;19(1):19–27. doi:10.1055/s-0030-1248072
11. Altman RD, Bedi A, Karlsson J, Sancheti P, Schemitsch E. Product differences in intra-articular hyaluronic acids for osteoarthritis of the knee. Am J Sports Med. 2016;44(8):2158–2165. doi:10.1177/0363546515609599
12. Hummer CD, Angst F, Ngai W, et al. High molecular weight Intraarticular hyaluronic acid for the treatment of knee osteoarthritis: a network meta-analysis. BMC Musculoskelet Disord. 2020;21(1):702. doi:10.1186/s12891-020-03729-w
13. Vannabouathong C, Bhandari M, Bedi A, et al. Nonoperative treatments for knee osteoarthritis: an evaluation of treatment characteristics and the intra-articular placebo effect: a systematic Review. JBJS Rev. 2018;6(7):e5. doi:10.2106/JBJS.RVW.17.00167
14. Phillips M, Vannabouathong C, Devji T, et al. Differentiating factors of intra-articular injectables have a meaningful impact on knee osteoarthritis outcomes: a network meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2020;28(9):3031–3039. doi:10.1007/s00167-019-05763-1
15. Altman RD, Manjoo A, Fierlinger A, Niazi F, Nicholls M. The mechanism of action for hyaluronic acid treatment in the osteoarthritic knee: a systematic review. BMC Musculoskelet Disord. 2015;16:321. doi:10.1186/s12891-015-0775-z
16. Ong KL, Runa M, Xiao Z, Ngai W, Lau E, Altman RD. Severe acute localized reactions following intra-articular hyaluronic acid injections in knee osteoarthritis. Cartilage. 2020;13:1474S–86S.
17. Ong KL, Anderson AF, Niazi F, Fierlinger AL, Kurtz SM, Altman RD. Hyaluronic acid injections in medicare knee osteoarthritis patients are associated with longer time to knee arthroplasty. J Arthroplasty. 2016;31(8):1667–1673. doi:10.1016/j.arth.2016.01.038
18. Bedard NA, Pugely AJ, Elkins JM, et al. The John N. Insall Award: do intraarticular injections increase the risk of infection after TKA? Clin Orthop Relat Res. 2017;475(1):45–52. doi:10.1007/s11999-016-4757-8
19. Cancienne JM, Werner BC, Luetkemeyer LM, Browne JA. Does timing of previous intra-articular steroid injection affect the post-operative rate of infection in total knee arthroplasty? J Arthroplasty. 2015;30(11):1879–1882. doi:10.1016/j.arth.2015.05.027
20. Richardson SS, Schairer WW, Sculco TP, Sculco PK. Comparison of infection risk with corticosteroid or hyaluronic acid injection prior to total knee arthroplasty. J Bone Joint Surg Am. 2019;101(2):112–118. doi:10.2106/JBJS.18.00454
21. Kurtz SM, Mont M, Chen AF, et al. Intra-articular corticosteroid or hyaluronic acid injections are not associated with periprosthetic joint infection risk following total knee arthroplasty. J Knee Surg. 2021:35;983–996
22. Gu A, Malahias MA, Cohen JS, et al. Prior knee arthroscopy is associated with increased risk of revision after total knee arthroplasty. J Arthroplasty. 2020;35(1):100–104. doi:10.1016/j.arth.2019.08.043
23. Kamath AF, Ong KL, Lau E, et al. Quantifying the burden of revision total joint arthroplasty for periprosthetic infection. J Arthroplasty. 2015;30(9):1492–1497. doi:10.1016/j.arth.2015.03.035
24. Altman R, Lim S, Steen RG, Dasa V. Hyaluronic acid injections are associated with delay of total knee replacement surgery in patients with knee osteoarthritis: evidence from a Large U.S. health claims database. PLoS One. 2015;10(12):e0145776. doi:10.1371/journal.pone.0145776
25. Dasa V, Lim S, Heeckt P. Real-world evidence for safety and effectiveness of repeated courses of hyaluronic acid injections on the time to knee replacement surgery. Am J Orthop. 2018;47:7.
26. Chitnis AS, Etter K, Holy CE, et al. Real-world impact of the high concentration non-avian high molecular weight hyaluronan on pain medication use among osteoarthritis patients. Curr Med Res Opin. 2019;35(9):1523–1527. doi:10.1080/03007995.2019.1596670
27. McIntyre LF, Beach W, Bhattacharyya S, Yadalam S, Bisson B, Kim M. Impact of hyaluronic acid injections on utilization of pain management medications. Am J Pharm Benefits. 2017;9(6):195–199.
28. Altman RD, Rosen JE, Bloch DA, Hatoum HT. Safety and efficacy of retreatment with a bioengineered hyaluronate for painful osteoarthritis of the knee: results of the open-label Extension Study of the FLEXX Trial. Osteoarthritis Cartilage. 2011;19(10):1169–1175. doi:10.1016/j.joca.2011.07.001
29. Wilson LA, Liu J, Fiasconaro M, Poeran J, Nwachukwu BU, Memtsoudis SG. Increased use of intra-articular steroid injection to treat osteoarthritis is associated with chronic opioid dependence after later total knee arthroplasty but not total hip arthroplasty. J Arthroplasty. 2020;35(8):1979–1982. doi:10.1016/j.arth.2020.04.012
30. Niazi F, Ong KL, Kidd VD, et al. Decrease in opioid and intra-articular corticosteroid burden after intra-articular hyaluronic acid for knee osteoarthritis treatment. Pain Manag. 2020;10:387–397. doi:10.2217/pmt-2020-0057
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.