Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Association among genetic polymorphisms of GSTP1, HO-1, and SOD-3 and chronic obstructive pulmonary disease susceptibility
Authors Du Y, Zhang H, Xu Y, Ding Y, Chen X, Mei Z, Ding H , Jie Z
Received 24 April 2019
Accepted for publication 22 August 2019
Published 6 September 2019 Volume 2019:14 Pages 2081—2088
DOI https://doi.org/10.2147/COPD.S213364
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chunxue Bai
Yong Du1,*, Hui Zhang2,*, Yan Xu3,*, Yi Ding1, Xuru Chen1, Zhoufang Mei1, Heyuan Ding4, Zhijun Jie1
1Department of Pulmonary and Critical Care Medicine, The Fifth People’s Hospital of Shanghai, Fudan University, Shanghai 200240, People’s Republic of China; 2Department of Endocrinology, People’s Hospital of Rizhao, Rizhao 276800, People’s Republic of China; 3Department of Laboratory Medicine, Rizhao Central Hospital, Rizhao 276800, People’s Republic of China; 4Department of Endocrinology, The Fifth People’s Hospital of Shanghai, Fudan University, Shanghai 200240, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhijun Jie
Department of Pulmonary and Critical Care Medicine, The Fifth People’s Hospital of Shanghai, Fudan University, No. 801 Heqing Road, Minhang District, Shanghai 200240, People’s Republic of China
Tel +86 189 181 68602
Fax +86 21 640 85875
Email [email protected]
Background: Chronic obstructive pulmonary disease (COPD) is a progressive lung disease characterized by incomplete reversible airflow limitation, which is associated with emphysema and chronic inflammation. Oxidative/antioxidant imbalance is one of the mechanisms of the current pathogenesis of COPD and several recent studies have attempted to uncover genetic causes of COPD and its progression. GST, HO-1, and SOD-3 are important susceptibility genes related to COPD.
Methods: A total of 300 blood samples were included in two groups: Control group and COPD group. We genotyped 4 single nucleotide polymorphisms (SNPs) from these 3 genes in 150 COPD patients and 150 controls to analyze genetic polymorphisms and interactions with COPD-related quantitative traits using correlation analysis and multivariate logistic regression analysis.
Results: The results indicated that genotype distributions and allele frequencies of GSTP1, HO-1, and SOD-3 were significantly different between the COPD and the control group, while there is no correlation between the polymorphism of GSTP1, HO-1, SOD3, and the different stages of COPD. Furthermore, multivariate logistic regression analysis indicated that COPD GSTP1-exon5 SNP and HO-1 (GT)n SNP are high-risk factors for COPD and there was interaction between GSTP1 exon5 SNPS and HO-1 (GT)n SNP. More important, the genotypes, AG, GG of GSTP1 exon5 and L/M*S, L/L of HO-1 (GT)n associated with increased 8-iso-prostaglandin F (2 alpha) (8-iso-PGF2) and malondialdehyde (MDA) concentration and decreased catalase (CAT) activity.
Conclusion: Collectively, this study shows that genetic polymorphisms of GSTP1, HO-1, and SOD-3 are associated with COPD susceptibility.
Keywords: chronic obstructive pulmonary disease, GSTP1, HO-1, SOD-3, SNPs
Introduction
Chronic obstructive pulmonary disease is a major chronic respiratory disease, which has risen to the third leading cause of mortality worldwide. It is characterized by incomplete reversible airflow obstruction and associated with emphysema and chronic inflammation.1 The pathogenesis of COPD is complex involving inflammation response, oxidative stress (oxidant/antioxidant imbalance), protease/protease imbalances, environmental insults, and host genetics.2 Cigarette smoking is the main risk factor for COPD and there are more than 40 million COPD patients in China which was caused by cigarette smoking mostly up to 2014.3,4 Oxidative/antioxidant imbalance is one of the mechanisms of the pathogenesis of COPD;5 cigarette smoking can bring a large amount of oxygen free radical into lung and trigger oxidative stress, which directly damages the lung tissue in the pathological progression of COPD. To deal with the damage, a series of antioxidases are involved in the antioxidant system to resist the harm of oxygen free radicals.6
Many of the antioxidants in the body, including glutathione-S transferase (GSTP1), heme oxygenase (HO-1), and superoxide dismutase (SOD), have been reported as important factors to reduce the occurrence of COPD.7–9 GSTP1 is recognized as a member of GSTs superfamily which is located on chromosomes 11q13. It was reported to be associated with COPD by replication and meta-analysis.10 There are two GSTP1 genotype polymorphic sites, including exon 5 A313G (Ile105Val) mutation and exon 6 C341T (Ala114Val) mutation.11 HO-1 is the inducible isoform of heme oxygenase which serves as “sensor/effector” by sensing cellular stress (oxidative, nitrosative, inflammatory, and metabolic).12 The HO-1 gene is located on human chromosome 22 (22q12), and the repeated sequence polymorphism of GT in its promoter region can reduce the induction of HO-1 and weaken the antioxidant capacity of the body.8 The SOD3 gene is located in human chromosome 4 (4pter-q21), with two introns and three exons. It is widely expressed and can remove the superoxide ions in the organism. Studies have shown that the polymorphism of SOD-3 gene may be associated with the occurrence of COPD.13 However, the role of genetic polymorphisms of these three genes on COPD susceptibility has not been evaluated yet.
Here, we genotyped 4 single nucleotide polymorphisms (SNPs) from these 3 genes in 150 COPD patients and 150 controls to analyze genetic polymorphisms and interactions with COPD-related quantitative traits using correlation analysis and multivariate logistic regression analysis. The results indicated that genotype distributions and allele frequencies of GSTP1, HO-1, and SOD-3 were significantly different between the COPD and the control group, while there is no correlation between the polymorphism of GSTP1, HO-1, and SOD3 and the different stages of COPD. Furthermore, multivariate logistic regression analysis indicated that COPD GSTP1-exon5 SNP and HO-1 (GT)n SNP are high-risk factors for COPD and there was interaction between GSTP1 exon5 SNPS and HO-1 (GT)n SNP. We also showed that the GSTP1-exon5 and HO-1 polymorphisms were associated with oxidative stress markers level including 8-iso-PGF2, MDA, and CAT. Collectively, this study shows that genetic polymorphisms of GSTP1, HO-1, and SOD-3 are associated with COPD susceptibility.
Materials and methods
Patient characteristics and clinical features
All patients were divided into three groups based on clinical features according to Global Initiative for Chronic Obstructive Lung Disease criteria.14,15 Patients with COPD were clinically stable, with no evidence of respiratory infection or an acute exacerbation for at least. The groups contained 150 blood samples in each: Control group and COPD group. Moreover, the COPD group was also divided into stable COPD and acute aggravation COPD. Table 1 summarized the patient characteristics and clinical features. The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Fifth People’s Hospital of Shanghai, Fudan University. All participants provided written informed consent.
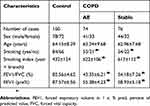 |
Table 1 Baseline characteristics of patients included in the study |
Collection of blood samples and extraction of DNA
Peripheral blood samples (2–4 mL) were collected with EDTA and were stored at −20°C. Genomic DNA was extracted from the blood samples using DNA extraction kit (TIANGEN Co., China).
SNPs selection and genotyping
Primer sequences, amplification, and details of purification conditions were conducted as described in previous studies.8,11,13 The SNPs were genotyped by using Polymerase chain reaction-sequence based typing (PCR-SBT), contained Taq DNA polymerase (Takara, Dalian, China) and BigDyeTM Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems). All the purified products were separated on agarose gel electrophoresis to define whether the amplification was successful. Then, the Cycle Sequencing Kit was used to sequence the purified PCR products directly. At last, Seqman software was applied to analysis the genotype of each specimen on the basis of nucleic acid sequence.
Biochemical parameters
Plasma MDA levels and CAT activity were measured as previously described on a high-throughput Spectramax-plus384 Spectrophotometer (Molecular Devices, USA).16,17 The 8-iso-PGF2α concentration was determined in serum using 8-isoprostane ELISA Kit (Cayman Chemical; Ann Arbor, MI, USA), and the results were read by means of EL808 IU (BioTek; Winooski, VT, USA). The coefficient of variation was <5% for intra- and inter-batch assessment.
Statistical analysis
Statistical analyses were performed in SPSS version 17.0 (SPSS Inc, Chicago, IL, USA). The demographic and clinical data of the COPD patients and the control subjects were compared using the χ2 test and Student’s t-test. Differences in allelic and genotypic frequencies of the gene polymorphisms in healthy controls and patients with COPD were compared by χ2 test, which was also used to evaluate Hardy–Weinberg equilibrium for each individual locus. A multiple logistic regression analysis was performed to correct the significant P-value.18
Results
Smoking was closely related to the general characteristics of COPD patients
The participants consisted of 150 cases (85 males) and 150 controls (78 males). As shown in Table 1, there was no statistically significant difference (P>0.05) in sex and age between the two groups by an independent-samples t-test and chi-squared (χ2) test, respectively. Patients with stable or acute exacerbations (AE) of COPD had significant higher smoking index and smoking history compared with control participants. Furthermore, FEV1/FVC (%) and FEV1(pre%) were significantly lower in COPD groups compared with control (P<0.05), suggesting that smoking was closely related to the occurrence of COPD.
Association of the GSTP1, HO-1, and SOD-3 polymorphism with COPD
The genotype distributions and allele frequencies of GSTP1, HO-1, and SOD-3 in the COPD and control groups are listed in Tables 2 and 3. There were significant differences in genotype frequencies at GSTP1, HO-1, and SOD-3 polymorphic sites between the two groups. The allele frequencies of these three SNPs display the significant difference between the COPD and control group after passing correlation analysis. To sum up, the polymorphism of GSTP1, HO-1, and SOD3 is correlated with the occurrence of COPD.
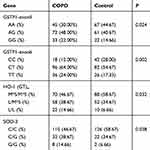 |
Table 2 Genotype frequencies of the GSTP1, HO-1, and SOD-3 in the two groups |
 |
Table 3 The allele frequencies of GSTP1, HO-1, and SOD-3 in the two groups |
Correlation analysis of the polymorphisms of GSTP1, HO-1, and SOD3 in different stages of COPD
The COPD patients were divided into smoker with stable COPD (COPD-Stable) group and smoker with acute exacerbation COPD (COPD-AE). The genotypes and allele frequencies of these three selected genes in these groups are listed in Tables 4 and 5. Correlation analysis demonstrated that there were not significant differences in GSTP1, HO-1, and SOD3 among the three groups. These results indicated that the polymorphisms of GSTP1, HO-1, and SOD3 are correlated with the occurrence of COPD, but there is no correlation with the different stages of COPD.
 |
Table 4 Frequency analysis of GSTP1, HO-1, and SOD3 genotypes in different stages of COPD |
 |
Table 5 Allele frequency analysis of GSTP1, HO-1, and SOD3 in different stages of COPD |
Multivariate logistic regression analysis of risk factors associated with COPD
The multivariate logistic regression analysis of COPD-related risk factors is presented in Table 6. Comparing with the control group, the odds ratio (OR) of COPD in smoking, GSTP1-exon6 SNP, and SOD-3 SNP increased by 1.342 [95% confidence interval (CI): 1.145–3.218, P=0.084], 1.028 (95% CI: 0.788–3.331, P=0.175) and 0.886 (95% CI: 0.567–3.025, P=0.223), respectively, suggesting that there was no statistically significant difference in the incidence of COPD between smoking, GSTP1-exon6 SNP and SOD-3 SNP. While the OR of COPD in GSTP1-exon5 SNP and HO-1 (GT)n SNP was 2.923 (95% CI: 1.245–4.616, P=0.023) and 4.127 (95% CI: 1.887–5.525, P=0.008), respectively. From the above, it is indicated that the incidence of COPD in GSTP1-exon5 SNP and HO-1 (GT)n SNP are high-risk factors for COPD.
 |
Table 6 Logistic regression analysis of risk factors |
Analysis of the interaction between GSTP1-exon5 and HO-1 (GT)n SNP
Then, we analyzed the interactions between the two high-risk factors GSTP1-exon5 and HO-1 (GT)n SNP. As shown in Table 7, compared with the control group, the risk of COPD in smokers with GSTP1-exon5 SNP but without- HO-1 (GT)n SNP was 1.234 times higher than that of the control group, while that of with HO-1 (GT)n SNP but without GSTP1-exon5 SNP was 2.543 times higher than that of the control group. However, in persons with both two SNPs, the risk was as much as 5.128-fold higher than that in the control group (P<0.05, 95% CI: 1.784–9.387), and the OR value of which was much more than the product of the former two conditions (5.128>1.234×2.543). These results suggested that there was interaction between GSTP1 exon5 SNPS and HO-1 (GT)n SNP.
 |
Table 7 Analysis of the interaction between GSTP1-exon5 SNP and HO-1 (GT)n SNP |
Association of the GSTP1-exon5 and HO-1 (GT)n polymorphism with the oxidative stress markers
We further evaluate the association of GSTP1-exon5 and HO-1 (GT)n genotypes with 8-iso-PGF2α concentration, MDA concentration and CAT activity, respectively. As shown in Table 8, the genotypes AG of GSTP1-exon5 and L/M*S of HO-1 (GT)n were associated with increased 8-iso-PGF2α and MDA concentration (P<0.05), and with decreased CAT activity (P<0.05) compared with AA of GSTP1-exon5 and M*S/M*S of HO-1 (GT)n in patients. The genotypes GG of GSTP1-exon5 and L/L of HO-1 (GT)n were also associated with increased 8-iso-PGF2α and MDA concentration (P<0.05), and with decreased CAT activity (P<0.05) as compared to the genotypes AA, AG of GSTP1-exon5 and M*S/M*S, L/M*S of HO-1 (GT)n in patients.
 |
Table 8 Analysis of the association of GSTP1-exon5 and HO-1 (GT)n genotypes with 8-iso-PGF2α concentration, MDA concentration, and CAT activity in the COPD patients |
Discussion
COPD is a complex polygenic disease with genetic contributions from multiple genes. In our study, we found that the polymorphisms of GSTP1, HO-1, and SOD3 were apparently associated with the occurrence of COPD, while there was no correlation with the different stages of COPD. Moreover, GSTP1-exon5 SNP and HO-1 (GT)n SNP are high-risk factors for COPD and GSTP1-exon5 SNP may interact with HO-1 (GT)n, influencing the COPD risk. We also determined that the genotypes, AG, GG of GSTP1 exon5 and L/M*S, L/L of HO-1 (GT)n associated with increased 8-iso-PGF2 and MDA concentration and decreased CAT activity. In conclusion, smoking is an important factor in COPD, and the polymorphisms of GSTP1, HO-1, and SOD3 are correlated with the occurrence of COPD.
Environmental and genetic factors are involved in the pathogenesis of COPD.19,20 Environmental factors such as smoking and air pollution can lead to a series of complex biological reactions, such as oxidative stress, which can induce the development of COPD, and genetic variation can regulate the expression or function of related antioxidant genes. The molecules involved in these reactions determine the susceptibility of COPD. Studies have shown that cigarette smoking is a main risk factor for COPD, and the interaction between genes and smoking is related to lung function in COPD.21,22 In our study, we found that smoking was closely related to the general characteristics of COPD patients and the polymorphism of GSTP1, HO-1, and SOD3 is correlated with the occurrence of COPD, but there is no correlation with the different stages of COPD.
Accumulated genetic association and genome-wide linkage studies have identified several candidate genes that might be involved in the pathogenesis of COPD. At present, most genetic association studies on COPD risk are focused on determining the individual effects of SNPs and their interaction effects on the disease. Yuan et al found that CDH13 genetic variants determine Chinese individuals’ susceptibility to COPD and could be used as efficient genetic biomarkers for early detection of COPD.18 Xie et al demonstrated that the polymorphisms of WWOX play a role in COPD susceptibility and pulmonary function traits in COPD inheritance.
An et al investigated the interaction among EPHX1, GSTP1, SERPINE2, and TGFB1 contributing to the quantitative traits of COPD.7 But Yang et al drew a conclusion that the results showed no significant association between gene polymorphism and COPD risk in Asian population and Caucasian population through a meta-analysis.23 Guénégou et al found that HO-1 acts against oxidants that were thought to play a major role in the pathogenesis of COPD. A (GT)n repeat polymorphism in the HO-1 gene promoter could modulate the gene transcription in response to oxidative stress.8 Zhou et al also indicated that L allele and type I (L carriers) were the risk factors of COPD in Asian population, not Caucasians. They also found HO-1(GT)n polymorphism was not related to COPD severity.24 Young et al suggest that SOD3 functions as an important antioxidant protein in smokers and the 213Gly SOD3 genetic variant was associated with conferring resistance to COPD in some smokers.13 However, Sorheim et al concluded that polymorphisms in the SOD3 gene were associated with CT emphysema but not COPD susceptibility.25
In our study, the repeated polymorphisms of short tandem repeats in HO-1 gene promoter region were found to carry the frequency of L-type allele and the frequency of carrying L-type allele in COPD patients was significantly higher than that in controls. It is possible that GSTP1-exon5 SNP and HO-1 (GT)n SNP were at increased risk of COPD and there was interaction between GSTP1 exon5 SNPs and HO-1 (GT)n SNP. Additionally, we investigated the correlation between the genotypes and the biomarkers; we observed the genotypes AG, GG of GSTP1 exon5 and L/M*S, L/L of HO-1 (GT)n associated with increased 8-iso-PGF2α, MDA levels, and decreased CAT activity in COPD patients, suggesting an increased oxidative stress. GSTP1 is important for redox regulation and defense from xenobiotics, and it has been shown to be associated with oxidative stress in patients with HBeAg-positive CHB.26 HO-1 acts against oxidants that are thought to play an important role in the pathogenesis of COPD. A (GT)(n) repeat polymorphism in the HO-1 gene promoter can modulate the gene transcription in response to oxidative stress.8 Alteration in expression of detoxifying and antioxidant genes has been shown to be an important susceptibility factor for COPD.
This study concluded that genetic polymorphisms in GSTP1, HO-1, and SOD-3 were all correlated with the occurrence of COPD. Nevertheless, the results were not completely consistent with those of other studies abroad and in China above, which may be attributed to environmental factors, different regions, and racial diversities, as well as the differences in experimental design and data analysis. In the later work, we will carry on the further research by expanding the sample size to provide effective theoretical basis for COPD nosogenesis.
In summary, we suggested that GSTP1, HO-1, and SOD3 genetic polymorphisms may play a significant role in the development of COPD susceptibility, while genetic polymorphisms of these three genes were not related to with the different stages of COPD. Moreover, GSTP1 exon-5 SNPS and HO-1 (GT)n SNP were two high-risk factors of COPD, which existed an interaction with each other thus participating in COPD susceptibility. The genotypes AG, GG of GSTP1 exon5 and L/M*S, L/L of HO-1 (GT)n were associated with increased 8-iso-PGF2α, MDA levels, and decreased CAT activity in COPD patients. These findings provide further insights into the polymorphism of genotype combinations at risk of developing COPD and improve understanding on the development of genetic susceptible biomarkers for the detection of COPD.
Acknowledgments
This research was supported by grants from the Shanghai Municipal Health and Family Planning Commission Scientific Research Project (201540123) and the Key Department of Shanghai Fifth People’s Hospital (2017WYZDZK07).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Barnes P, Burney P, Silverman E, et al. Chronic obstructive pulmonary disease. Nat Rev Dis Primers. 2015;1:15076. doi:10.1038/nrdp.2015.76
2. Fischer BM, Pavlisko E, Voynow JA. Pathogenic triad in COPD: oxidative stress, protease-antiprotease imbalance, and inflammation. Int J Chron Obstruct Pulmon Dis. 2011;6:413–421. doi:10.2147/COPD.S10770
3. Hassett DJ, Borchers MT, Panos RJ. Chronic obstructive pulmonary disease (COPD): evaluation from clinical, immunological and bacterial pathogenesis perspectives. J Microbiol. 2014;52(3):211–226. doi:10.1007/s12275-014-4068-2
4. Zhou Y, Chen R. Risk factors and intervention for chronic obstructive pulmonary disease in China. Respirology. 2013;18(Suppl 3):4–9. doi:10.1111/resp.12190
5. Fischer BM, Voynow JA, Ghio AJ. COPD: balancing oxidants and antioxidants. Int J Chron Obstruct Pulmon Dis. 2015;10:261–276. doi:10.2147/COPD.S42414
6. Pickett G, Seagrave J, Boggs S, Polzin G, Richter P, Tesfaigzi Y. Effects of 10 cigarette smoke condensates on primary human airway epithelial cells by comparative gene and cytokine expression studies. Toxicol Sci. 2010;114(1):79–89. doi:10.1093/toxsci/kfp298
7. An L, Lin Y, Yang T, Hua L. Exploring the interaction among EPHX1, GSTP1, SERPINE2, and TGFB1 contributing to the quantitative traits of chronic obstructive pulmonary disease in Chinese Han population. Hum Genomics. 2016;10(1):13. doi:10.1186/s40246-016-0076-0
8. Guenegou A, Leynaert B, Benessiano J, et al. Association of lung function decline with the heme oxygenase-1 gene promoter microsatellite polymorphism in a general population sample. Results from the European Community Respiratory Health Survey (ECRHS), France. J Med Genet. 2006;43(8):e43. doi:10.1136/jmg.2005.040493
9. Zou SC, Jiang J, Song J. IL-33 induced inflammation exacerbated the development of chronic obstructive pulmonary disease through oxidative stress. Eur Rev Med Pharmacol Sci. 2018;22(6):1758–1764. doi:10.26355/eurrev_201803_14593
10. Hua L, An L, Li L, Zhang Y, Wang C. A bioinformatics strategy for detecting the complexity of chronic obstructive pulmonary disease in Northern Chinese Han Population. Genes Genet Syst. 2012;87(3):197–209. doi:10.1266/ggs.87.197
11. Cheng SL, Yu CJ, Chen CJ, Yang PC. Genetic polymorphism of epoxide hydrolase and glutathione S-transferase in COPD. Eur Respir J. 2004;23(6):818–824. doi:10.1183/09031936.04.00104904
12. Motterlini R, Foresti R. Heme oxygenase-1 as a target for drug discovery. Antioxid Redox Signal. 2014;20(11):1810–1826. doi:10.1089/ars.2013.5658
13. Young RP, Hopkins R, Black PN, et al. Functional variants of antioxidant genes in smokers with COPD and in those with normal lung function. Thorax. 2006;61(5):394–399. doi:10.1136/thx.2005.048512
14. Shen W, Liu J, Fan M, et al. MiR-3202 protects smokers from chronic obstructive pulmonary disease through inhibiting FAIM2: an in vivo and in vitro study. Exp Cell Res. 2018;362(2):370–377. doi:10.1016/j.yexcr.2017.11.038
15. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Arch Bronconeumol. 2017;53(3):128–149. doi:10.1016/j.arbres.2017.02.001
16. Vibhuti A, Arif E, Deepak D, Singh B, Qadar Pasha MA. Correlation of oxidative status with BMI and lung function in COPD. Clin Biochem. 2007;40(13–14):958–963. doi:10.1016/j.clinbiochem.2007.04.020
17. Yu D, Liu X, Zhang G, Ming Z, Wang T. Isoliquiritigenin inhibits cigarette smoke-induced COPD by attenuating inflammation and oxidative stress via the regulation of the Nrf2 and NF-kappaB signaling pathways. Front Pharmacol. 2018;9:1001. doi:10.3389/fphar.2018.01001
18. Yuan YM, Zhang JL, Xu SC, et al. Genetic variants of CDH13 determine the susceptibility to chronic obstructive pulmonary disease in a Chinese population. Acta Pharmacol Sin. 2016;37(3):390–397. doi:10.1038/aps.2015.158
19. Kim WJ, Lee SD. Candidate genes for COPD: current evidence and research. Int J Chron Obstruct Pulmon Dis. 2015;10:2249–2255. doi:10.2147/COPD.S80227
20. Dijkstra AE, Smolonska J, van den Berge M, et al. Susceptibility to chronic mucus hypersecretion, a genome wide association study. PLoS One. 2014;9(4):e91621. doi:10.1371/journal.pone.0091621
21. He JQ, Connett JE, Anthonisen NR, Pare PD, Sandford AJ. Glutathione S-transferase variants and their interaction with smoking on lung function. Am J Respir Crit Care Med. 2004;170(4):388–394. doi:10.1164/rccm.200312-1763OC
22. Xie C, Chen X, Qiu F, et al. The role of WWOX polymorphisms on COPD susceptibility and pulmonary function traits in Chinese: a case-control study and family-based analysis. Sci Rep. 2016;6:21716. doi:10.1038/srep21716
23. Yang L, Li X, Tong X, Fan H. Association between glutathione S-transterase P1 lle(105) Val gene polymorphism and chronic obstructive pulmonary disease: Ameta-analysis based on seventeen case-control studies. Meta Gene. 2015;6:59–64. doi:10.1016/j.mgene.2015.08.007
24. Zhou H, Ying X, Liu Y, Ye S, Yan J, Li Y. Genetic polymorphism of heme oxygenase 1 promoter in the occurrence and severity of chronic obstructive pulmonary disease: a meta-analysis. J Cell Mol Med. 2017;21(5):894–903. doi:10.1111/jcmm.13028
25. Sorheim IC, DeMeo DL, Washko G, et al. Polymorphisms in the superoxide dismutase-3 gene are associated with emphysema in COPD. COPD. 2010;7(4):262–268. doi:10.3109/15412555.2010.496821
26. Fan XP, Ji XF, Li XY, Gao S, Fan YC, Wang K. Methylation of the glutathione-S-Transferase P1 gene promoter is associated with oxidative stress in patients with chronic hepatitis B. Tohoku J Exp Med. 2016;238(1):57–64. doi:10.1620/tjem.238.57
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
