Back to Journals » Advances in Medical Education and Practice » Volume 14
Assessment of Self-Medication Practice and Its Determinants Among Undergraduate Health Science Students of College of Medicine and Health Sciences, Bahir Dar University, North West Ethiopia: A Cross-Sectional Study
Authors Yismaw MB , Feyisa K , Yehualaw A , Tafere C , Demsie DG , Bahiru B , Kefale B
Received 18 January 2023
Accepted for publication 21 March 2023
Published 27 March 2023 Volume 2023:14 Pages 279—288
DOI https://doi.org/10.2147/AMEP.S401565
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Malede Berihun Yismaw, Kebede Feyisa, Adane Yehualaw, Chernet Tafere, Desalegn Getnet Demsie, Bereket Bahiru, Belayneh Kefale
Department of Pharmacy, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Correspondence: Malede Berihun Yismaw, Department of Pharmacy, College of Medicine and Health Sciences, Bahir Dar University, PO Box 79, Bahir Dar, Ethiopia, Tel +251966335852, Email [email protected]
Background: Self-medication (SM) is the use of drugs or herbs to treat self-diagnosed physical ailments or symptoms without consulting a healthcare professional. It plays a great role in daily life and common in the healthcare system around the globe, especially in developing countries. Due to their expertise, health science students are also predicted to practice it more frequently.
Objective: To evaluate the use of SM and its determinants among undergraduate health science students at the College of Medicine and Health Sciences, Bahir Dar University, North West Ethiopia.
Methods: 241 students took part in the study from September to November 2021. Using a recall time of four weeks, a quantitative descriptive cross-sectional study was utilized to evaluate the practice of self-medication and associated factors. Interviews and structured questionnaires were used to collect the data. Data were analyzed using SPSS version 25.
Results: Overall, 246 students were approached. The questionnaire received responses from 241 students, for a 98% response rate. Self-medication was used by 58.1% of students over the course of the previous four weeks. Analgesic and antipyretic medications were the most often utilized pharmacological category (57.1%), followed by antibiotics (42.1%). The most frequent (50%) complaints involving SM were headache and fever. The mildness of the sickness was the primary factor in the study participants’ practice of self-medication (50%). Self-medication is linked to gender (AOR: 3.415; 95% CI: 1.014– 11.503), poor monthly income (AOR: 0.007; 0.0003– 0.175), pharmacy student status (AOR: 52.603; 4.371– 633.098), and medical laboratory student status (AOR: 0.037; 0.002– 0.631).
Conclusion: Self-medication was common among health science students. Students frequently use over-the-counter and prescription-only medications for SM. Sex, field of study and monthly income are independent predictors for SM use. Though it is not absolutely discouraged, awareness on the associated risks should be created.
Keywords: self-medication, students, health sciences, Ethiopia
Introduction
Individual self-care in the family and local community has been the predominant model of healthcare throughout the course of human history. People were in charge of looking for their own and their families' health. Self-care is perhaps not just as old as humanity, but it is also the most popular.1 As a component of self-care, self-medication (SM) involves choosing and using medications on one’s own initiative to address self-identified illnesses or symptoms. It also includes the use of non-prescription medications.2,3
Self-medication is commonly used in both industrialized and developing nations, while the specifics of how it is used and why can vary from one nation to the next. A major public health concern is the use of SM on a global scale.4 Many pharmaceuticals are sold over-the-counter (OTC) without a doctor’s prescription in a number of underdeveloped nations, including Ethiopia. Nearly 12.1–87% of medical illnesses are treated by SM, which is optional and costs less money.5–9 Even though they are aware of the negative effects and potential risks, health care professionals self-medicate at dangerously high rates.10–12
Although over-the-counter (OTC) medications are designed for self-medication and have been shown to be effective and safe, using them improperly could have serious consequences, especially in the case of irresponsible SM because it could result in risks like incorrect self-diagnosis, severe adverse reactions, drug interactions, improper administration, and dependence.2,13 The national drug regulatory authority may, however, approve of responsible SM as safe for self-medication; such medications are typically used for the prevention or treatment of minor illnesses or symptoms that do not require medical consultations, and in some chronic or recurring illnesses, self-medication is also possible after initial prescription with the doctor retaining an advisory role.4
Although SM is an effective method for treating minor illnesses, health sciences students’ attitude toward it is leading to misuse and abuse of both over-the-counter and prescription medications. Serious medication responses and even deadly outcomes could result from this. Additionally, there is currently a concern concerning the development of antibiotic resistance that may have been greatly increased by SM on a global scale.13–15 Another significant issue in Ethiopia is the rising incidence and widespread use of self-medication by medical personnel.6
Students studying health sciences often self-manage their ailments until they are no longer under control, which can sometimes result in death. Despite the importance of the self-prescription issue and its wide-ranging effects among health science students, little information is currently accessible on the topic, particularly in the study field. It is crucial to examine this behavior among health science students because they may eventually work as medical professionals and may need to advise patients and clients on the benefits and drawbacks of self-medication. In light of this, we evaluated the extent of SM and its associated factors among Bahir Dar University health science students.
Methods and Materials
Study Area and Period
The research was done at the Bahir Dar University (BDU), College of Medicine and Health Sciences (CMHS), in Sebatamit Kebele, Bahir Dar, Ethiopia. Bahir Dar is the capital of Amhara region situated 565 kilometers from Addis Ababa, the nation’s capital. BDU was founded in 1963 and has since grown to six sites. Of which, CMHS is the one that trains medical personnel. It functions as a training center for medical students in their undergraduate and graduate studies, as well as for pharmacists, nurses, midwives, medical laboratory technologists, anesthesia, and physiotherapists.
The Tibebe Gihion Comprehensive Specialized Hospital (TGSH), which was established in 2000 E.C. as a teaching hospital of BDU, provides medical care for the students. The hospital serves more than 7 million residents of the Amhara region and the nearby Benishangul Gumuz region with emergency, inpatient, and outpatient care. Pharmacy, clinical laboratory, surgery, gynecology and obstetrics, maternal and child health, emergency, and other preventative healthcare services are some of these.
Study Design and Period
The practice of SM among health science students enrolled in the College of Medicine and Health Sciences at Bahir Dar University was examined using a quantitative cross-sectional study methodology. The information was gathered between 15 September and 15 October 2021. The SM recall period lasted for four weeks.
Source Population and Study Population
The College of Medicine and Health Sciences regular undergraduate students at Bahir Dar University served as the source population, while the College of Medicine and Health Sciences regular undergraduate students who attended their classes during the study period constitute the study population.
Study Variables and Eligibility Criteria
Sex, age, marital status, field of study, year of study, family residency, and monthly income are the independent factors, while SM practice is the dependent variable.
Inclusion Criteria
All BDU, CMHS health science students who were available on campus throughout the study time, willing to engage in the study, and who met these criteria were included. Students with serious illness during data collection, and collected questionnaires with incomplete information were excluded from the study.
Sample Size Determination and Sampling Technique
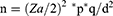
Sample size was determined using a single population proportion formula:
Where;
n= the desired sample size (if the target population is greater than 10,000).
Z α/2= the standard normal deviate 1.96 at 95% confidence interval.
P- Prevalence (0.5) since the reasonable estimate of the key proportion to be studied is unknown.
d= 0.05- which is the level of significance at 95% or acceptable margin of error
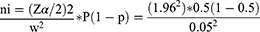
The sample size calculation was based on the assumption that 50% of Health Science Students are involved in SM practice during the last 4 weeks. Therefore:
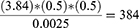
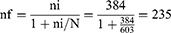
As the sample was taken from a relatively small population (N = 603), the required minimum sample was obtained from the above estimate by making some adjustment with formula:
Considering a 5% non-response rate, the total sample size was:
Hence, 246 regular health science students were included in this study.
Based on the field and years of study, a stratified multistage random sampling technique was used. Accordingly, based on the corresponding total number of regular undergraduate Health Science Students, the sample was proportionally distributed across the four departments of the School of Health Sciences at CMHS, BDU. The proportional allocation of the sample was done in accordance with the stratification of those departments into various study years. Last but not least, research participants were chosen based on proportional allocation in each department and year of study using a simple random sampling procedure.
Data Collection Tool and Management
The information was gathered using a self-administered comprehensive and well-organized questionnaire that was developed after examining related literature and tailored for our situation. The fact that the information gathered would be anonymous and that participation would be completely voluntary was made clear to the study subjects. Both open-ended and closed-ended questions on sociodemographic and SM related topics are included in the survey. Before beginning the actual data collection and making the necessary corrections, a pre-test of the questionnaire was conducted. After received the necessary instruction and training for a day, two fifth year pharmacy students collected the data. Daily checks were made for any consistency and/or incompleteness in the obtained data.
Data Processing and Analysis
The data was categorized, coded and analyzed using Statistical Package for the Social Sciences (SPSS) version 25® software. Data was presented in tables, figure and text. Descriptive statistics was used for all variables. In addition, factor analysis was done using both univariate and multivariable binary logistic regression to test for significance. Only variables with p< 0.2 were included in the multivariable binary logistic regression to avoid effect of confounders. A p< 0.05 was used to declare association to the outcome variable, SM practice.
Ethical Consideration
A letter of ethical clearance (Ref. No/Phar01/26/01/2014 E.C.) was received from the College of Medicine and Health Sciences, Bahir Dar University, before data collection period. All study participants were informed about the purpose of the study and provided written consent. Confidentiality was also achieved by omitting participant identifiers. Our study was conducted in accordance with the Declaration of Helsinki.
Results
Socio-Demographic Characteristics of the Study Participants
Out to 246 students approached, 241 of them responded to the questionnaire, giving us a 98% response rate. The average age of the participants was between 21 and 23 years old (55.6%). Male respondents constitute 55% of the sample, and single individuals about 83.4%. About 86% of the respondents were Orthodox Christian followers, while 53.5% of the participants’ families had a permanent residence in an urban region. According to Table 1, 36.1% of students were studying pharmacy, followed by nursing (32.0%).
 |
Table 1 Socio-Demographic Characteristics of Study Participants, CMHS, Bahir Dar University, Bahir Dar, Ethiopia (n=241) |
Prevalence of Self-Medication
Self-medication was practiced by 58.1% of the participants and the majority of these participants (n=49) had only practiced self-medication once (Table 2).
Illness/Symptoms for Self-Medication and Duration of Illness Before Self-Medication
The major illness leads for self-medication was headache/fever (50%) followed by gastrointestinal symptoms (42.1%) and respiratory tract infections (40%). More than half of self-medicated respondents (n=74) took the drug within 24 hours of becoming ill, while only a tiny number of respondents (n=4) used the medication after 5 to 12 weeks had passed since becoming ill, as indicated in Table 3.
 |
Table 3 Illness/Symptoms for Self-Medication and Duration of Illness Before Self-Medication Among Students of CMHS, Bahir Dar University, Bahir Dar, Ethiopia |
Reasons for Self-Medication Practice
The major reason mentioned by the study participants who practice SM was because of the mildness of the illness (50%) followed by for emergency use (33.1%) as depicted in the following Figure 1.
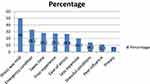 |
Figure 1 Reasons of the study participants for Self-Medication among Students of CMHS, BDU, Bahir Dar, Ethiopia. |
Source and Type of Requested Drug
Antimicrobials (42.1%) and painkillers (analgesics/antipyretics) were the two drug classes most frequently used by respondents who reported using SM. Seventy percent of the medications used for self-medication were obtained from pharmacies (n = 98), followed by friends (n = 46) (Table 4).
 |
Table 4 Source and Type of Requested Drug for Self Medication Among Health Science Students of Bahir Dar University, CMHS, Bahir Dar, Ethiopia |
Reasons of Not Using Self Medication Practice
Among SM non-users, majority (51.5%) did not practice SM because they prefer to go to hospital for further checkup (Table 5).
 |
Table 5 Reasons for Not Using Self-Medication Among Health Science Students of Bahir Dar University, CMHS, Bahir Dar, Ethiopia |
Factors Associated with Self-Medication Practice
Using a univariate binary logistic regression analysis, all the covariates, including sex, age, religion, marital status, monthly income, year of study, and field of study, were examined for associations with SM practice. Variables having a p<0.2 were taken into consideration for multivariable binary logistic regression analysis to establish a relationship under the presumption that confounders will be removed. Accordingly, SM use was significantly associated with female respondents (AOR: 3.415; 95% CI: 1.014–11.503), pharmacy students (AOR: 52.603; 4.371–633.098), medical laboratory students (AOR: 0.037; 0.002–0.631), and students with monthly incomes of less than 500ETB (AOR: 0.007; 0.0003–0.175) (Table 6).
Discussion
Numerous researches have revealed that SM practice is widely used throughout the world.5,6,8,10–12 Self-medication practice has persisted in both developing and developed nations, and it is more common among college students.6,7,16,17 Self-medication behavior is linked to ineffective use of both over-The-counter (OTC) and prescription-only drugs (POM). Accordingly, the purpose of this study was to evaluate the prevalence and contributing factors of SM among generic health science students at CMHS, BDU.
According to this survey, SM use was reported to be practiced by 58.1% of the participants. Studies including university students from Egypt have found a similar incidence (62.9%),10 Najran University in Saudi Arabia (60%),18 University of Gondar (52.4%),7 Mbarara University of Science and Technology in Uganda (63.5%)16 among medical and non-medical students at Taibah University, Madinah, Saudi Arabia (64.8%).8 On the contrary, our study finding was much higher than study conducted in Rwanda (12.1%)8 and Ayder campus of Mekelle University, Ethiopia (43.24%).5
Conversely, a higher prevalence of SM practice was reported in Selected Hospitals of Western Ethiopia (73.4%),6 Arsi University, Ethiopia (77.1%) [32], Asmara College of Health Sciences, Eritrea (79.2%),19 Nigeria (81.8%),17 U.A.E (86%),20 North India (87.00%),9 Mahadevappa Rampure Medical College Gulbarga, Karnataka, India. (88.18%)21 and among students of Delhi University North Campus, New delhi, India (85.4%).22 The differences in SM practices between and within nations may be attributed to the respondents’ cultural backgrounds, healthcare systems, infrastructures, study time variability, availability of over-The-counter medications, economic standing of the study area, and sociodemographic traits.
Fever and headache (50%) were the most commonly reported symptoms that led to SM, followed by gastrointestinal complaints (42.1%) and respiratory tract infections. Likewise, these complaints are common among self-medicated individuals as per local studies.5–7,12,23 According to self-medicating students in a Saudi Arabian survey, they also utilized over-The-counter drugs to manage headache (35.6%), sore throat and upper respiratory tract infections (42.9%), fever (14.1%), GIT difficulties (4.9%), and skin issues (91.2%).8 Additionally, studies carried out in India revealed that the most common medical conditions leading to self-medication were cough, cold, and headache.21,22 Similar findings were found in a Cross-Sectional study of self-medication practices in medical students during the COVID-19 pandemic.24
Fever/headache, respiratory tract infections and gastrointestinal complaints such as peptic ulcer disease symptoms are considered as minor ailments by students and they tend to treat themselves without consulting healthcare professionals. The type of complaint might also vary depending on the study time at which respiratory infections are more common in cold weather.
Non-seriousness of the sickness (50%) was the leading factor in SM, followed by the occurrence of an emergency situation (33.1%). In a different study, mildness of disease symptoms was also commonly noted.7,12,16,20 Students frequently believe that there are no risks involved in treating mild illnesses without seeking medical advice. However, a study of undergraduate students at a private university in Nigeria found that the lack of time to visit the school clinic, the distance between the clinic and the hostel, and the drugs prescribed there do not improve health conditions to be the top three causes of self-medication (27.7%, 26.7%, and 15.3%, respectively).17
Self-medicating individuals most frequently obtain their medications from pharmacies (70%) and friends (32.9%). In accordance with our study, the Mbarara University of Science and Technology in Uganda16 and the Ayder campus of Mekelle University in Ethiopia.5 Pharmacy and drug stores are typical places to buy medication, according to a number of earlier researches. Additionally, past prescriptions, friends, and family are reflected for regularly reported sources.10,11 There may be a connection between Ethiopia’s restrictive drug access laws and the informal accessibility of all pharmaceuticals from drug stores and pharmacies. The rise of responders who could use self-medication could be attributed to the lack of robust legislation in the nation. As a result, these approaches run the risk of fostering drug resistance patterns, irrational drug use, and harm to human life. Inappropriate practice of sharing of medicines was also seen in about 32.9% of self-medication users. The risk is much higher if antibiotics are shared among individuals due the development of antimicrobial resistance.
In the current study, analgesics (57.1%) were the most widely used drug classes followed by antimicrobials (42.1%). Similar research in Selected Hospitals in Western Ethiopia revealed that analgesics (44.4%) and antibiotics were the most popular drug classes utilized for SM.6 Other studies also reported analgesics as the most utilized agents for SM.5,8,17,19 The increase in use of analgesics in our study and others might be because of these drug classes are the drug of choice utilized for females to relieve menstrual related symptoms.
Antibiotics account for 42.7% of all medicine types used for SM. Similarily, a research in India found that 63.91% of students utilized antibiotics for SM.21 A study in Bangladesh found that about 77% students were uncertain about the treatment outcome due to injudicious use of antibiotics and 70% respondents strongly disagreed about development of antibiotic resistance due to skipping 1–2 doses.25 SM with antibiotics is a human practice in which a person uses antibiotics to address problems that they have self-diagnosed. Although most antibiotic medications require a prescription, some topical antibiotics are available over-The-counter (OTC). Additionally, taking antibiotics for self-treatment poses a serious risk to one’s health because it raises the likelihood that antibiotic resistance will emerge and necessitates strict regulatory controls.
Self-medication was discovered to be considerably correlated with sex, academic field, and monthly income. Similarly, being female is associated with an increase in SM use in different studies done elsewhere.6–8,17,24 The likely cause is that female students were more likely than male students to experience repeated disease problems due to their lower immunity and ongoing menstrual cycle as a result of hormonal effects. The use of anti-pain medications is significantly correlated with this monthly menstrual cycle, which may lead to gradual drug adaptation and make people reluctant to seek medical attention, ultimately resulting in high levels of SM. Students with low monthly income are associated with lower SM use due to the fact that they cannot afford to buy the medications from pharmacies and go to the campus student clinic which gives free service to students. Pharmacy students are practicing self-medication in a higher extent probably due to their perception of considering themselves as drug experts though miss diagnosis is the major problem seen in self-medication users.
Study Limitations
Because only one facility was involved in the study, its generalizability may be constrained. Apart from this, there might be recall bias and lack of standardized and validated questionnaire for conducting the study.
Conclusion
The use of SM is particularly prevalent among health science students. The most frequently reported conditions for self-medication were respiratory tract infections, gastrointestinal issues, and headaches/fever. The characteristics that were revealed to be significantly associated with SM practice included sex, field of study, and monthly income. Analgesics are majorly utilized followed by antibiotics. The regulatory authority and drug dispensers should take a strong measure on the utilization of drugs for self-medication.
Acknowledgments
We would like to acknowledge Department of pharmacy, College of Medicine and Health Sciences, Bahir Dar University FOR the ethical approval of the study. We also would like to acknowledge fifth year pharmacy students (Ahmed Seid, Alemu Tebabal) for helping in the data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kickbusch I. Self-care in health promotion. Soc Sci Med. 1989;29(2):125–130. doi:10.1016/0277-9536(89)90160-3
2. Montastruc J-L, Bondon-Guitton E, Abadie D, et al. Pharmacovigilance, risks and adverse effects of self-medication. Therapies. 2016;71(2):257–262. doi:10.1016/j.therap.2016.02.012
3. Montastruc J, Bagheri H, Geraud T, et al. Pharmacovigilance of self-medication. Therapie. 1997;52(2):105–110.
4. Bennadi D. Self-medication: a current challenge. J Basic Clin Pharma. 2013;5(1):19. doi:10.4103/0976-0105.128253
5. Gutema GB, Gadisa DA, Kidanemariam ZA, et al. Self-medication practices among health sciences students: the case of Mekelle University. J Appl Pharma Sci. 2011;2011:183–189.
6. Fekadu G, Dugassa D, Negera G, et al. Self-medication practices and associated factors among health-care professionals in selected hospitals of Western Ethiopia. Patient Prefer Adherence. 2020;14:353. doi:10.2147/PPA.S244163
7. Zeru N, Fetene D, Geberu DM, et al. Self-medication practice and associated factors among University of Gondar College of Medicine and Health Sciences Students: a cross-sectional study. Patient Prefer Adherence. 2020;14:1779. doi:10.2147/PPA.S274634
8. Aljaouni ME, Hafiz AA, Alalawi HH, Alahmadi GA, AlKhawaja I. Self-medication practice among medical and non-medical students at Taibah University, Madinah, Saudi Arabia. Int J Acad Sci Res. 2015;3(4):54–65.
9. Verma RK, Mohan L, Pandey M. Evaluation of self medication among professional students in North India: proper statutory drug control must be implemented. Evaluation. 2010;3(1):60–64.
10. Babatunde OA, Fadare JO, Ojo OJ, et al. Self-medication among health workers in a tertiary institution in South-West Nigeria. Pan Afr Med J. 2016;24:54.
11. Onchonga D, Omwoyo J, Nyamamba D. Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharma J. 2020;28(10):1149–1154. doi:10.1016/j.jsps.2020.08.003
12. Eticha T, Mesfin K. Self-medication practices in Mekelle, Ethiopia. PLoS One. 2014;9(5):e97464. doi:10.1371/journal.pone.0097464
13. Robinson GM, Robinson S, McCarthy P, Cameron C. Misuse of over-The-counter codeine-containing analgesics: dependence and other adverse effects. NZ Med J. 2010;123(1317):59–64.
14. Shahzad H, Malik F, Ashfaq KM, et al. Prevalence of self-medication and health-seeking behavior in a developing country. Afri J Pharma Pharmacol. 2011;5(7):972–978.
15. Nepal G, Bhatta S. Self-medication with antibiotics in WHO Southeast Asian Region: a systematic review. Cureus. 2018;10(4):112.
16. Niwandinda F, Lukyamuzi EJ, Ainebyona C, et al. Patterns and practices of self-medication among students enrolled at Mbarara University of Science and Technology in Uganda. Integr Pharm Res Pract. 2020;9:41. doi:10.2147/IPRP.S237940
17. Esan DT, Fasoro AA, Odesanya OE, et al. Assessment of self-medication practices and its associated factors among undergraduates of a private university in Nigeria. J Environ Public Health. 2018;2018:1–7. doi:10.1155/2018/5439079
18. Al-Qahtani AM, Shaikh IA, Shaikh MAK, et al. Prevalence, perception, and practice, and attitudes towards self-medication among undergraduate medical students of Najran University, Saudi Arabia: a Cross-Sectional Study. Risk Manag Healthc Policy. 2022;Volume 15:257–276. doi:10.2147/RMHP.S346998
19. Araia ZZ, Gebregziabher NK, Mesfun AB. Self medication practice and associated factors among students of Asmara College of Health Sciences, Eritrea: a cross sectional study. J Pharma Policy Pract. 2019;12(1):1–9. doi:10.1186/s40545-019-0165-2
20. Sharif SI, Ibrahim OH, Mouslli L, Waisi R. Evaluation of self-medication among pharmacy students. Am J Pharmacol Toxicol. 2012;7(4):135–140. doi:10.3844/ajptsp.2012.135.140
21. Patil SB, S H V, B V P, et al. Self-medication practice and perceptions among undergraduate medical students: a cross-sectional study. J Clin Diagn Res. 2014;8(12):HC20. doi:10.7860/JCDR/2014/10579.5313
22. Adhikary M, Tiwari P, Singh S, et al. Study of self-medication practices and its determinant among college students of Delhi University North Campus, New Delhi, India. Int J Med Sci Public Health. 2014;3(4):406–409. doi:10.5455/ijmsph.2014.260120146
23. Abay S, Amelo W. Assessment of Self-medication practices among medical, pharmacy, health science students in Gondar University, Ethiopia. J Young Pharma. 2010;2(3):306–310. doi:10.4103/0975-1483.66798
24. Yasmin F, Asghar MS, Naeem U, et al. Self-medication practices in medical students during the COVID-19 pandemic: a cross-sectional analysis. Front Public Health. 2022;10. doi:10.3389/fpubh.2022.803937
25. Nasir M, Perveen RA, Farha N, et al. Knowledge, attitude and practice about use of antibiotic by medical students: a cross sectional pilot study on para-clinical students in HFRCMC. J Med Sci Res. 2016;25(1):15–19. doi:10.47648/jmsr.2016.v2501.03
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.