Back to Journals » Psychology Research and Behavior Management » Volume 16
Assessment of Levels of Anxiety and Fear of Covid-19 in a Population of Pregnant Women in Spain
Authors Muñoz-Vela FJ, Fernández-Carrasco FJ, Gómez-Salgado J , Allande-Cussó R , Marques Monteiro Dias Mendes IM, Martins Teixeira-da-Costa EI , Vázquez-Lara JM, Fagundo-Rivera J , Rodríguez-Díaz L
Received 28 July 2023
Accepted for publication 14 October 2023
Published 16 November 2023 Volume 2023:16 Pages 4665—4676
DOI https://doi.org/10.2147/PRBM.S432792
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Francisco Javier Muñoz-Vela,1,2,* Francisco Javier Fernández-Carrasco,3 Juan Gómez-Salgado,4,5 Regina Allande-Cussó,6,* Isabel Margarida Marques Monteiro Dias Mendes,7 Emilia Isabel Martins Teixeira-da-Costa,8,9 Juana María Vázquez-Lara,3 Javier Fagundo-Rivera,10 Luciano Rodríguez-Díaz3
1Department of Nursing, Faculty of Health Sciences, University of Málaga, Málaga, Spain; 2Obstetrics and Gynecology Area, Hospital Regional Universitario de Málaga, Málaga, Spain; 3Department of Gynaecology and Obstetrics, Ceuta University Hospital, Midwifery Teaching Unit of Ceuta, University of Granada, Ceuta, Spain; 4Department of Sociology, Social Work and Public Health, Faculty of Labour Sciences, University of Huelva, Huelva, Spain; 5Safety and Health Postgraduate Programme, Universidad Espíritu Santo, Guayaquil, Ecuador; 6Department of Nursing. University of Seville, Seville, Spain; 7Unidade Científico-Pedagógica de Enfermagem de Saúde Materna, Obstétrica e Ginecológica, UICISA: E. Escola Superior de Enfermagem de Coimbra, Coimbra, Portugal; 8Department of Nursing, Health School, University of Algarve, Faro, Portugal; 9Health Sciences Research Unit: Nursing, Escola Superior de Enfermagem de Coimbra, Coimbra, Portugal; 10Centro Universitario de Enfermería Cruz Roja, Sevilla, Spain
*These authors contributed equally to this work
Correspondence: Juan Gómez-Salgado, Department of Sociology, Social Work and Public Health, Faculty of Labour Sciences, University of Huelva. Avda. Tres de Marzo, S/N, 21007, Huelva, Spain, Tel +34 959219700, Email [email protected]
Objective: The aim of the study was to assess the levels of fear and anxiety in the particularly vulnerable population group of women during pregnancy.
Methods: Cross-sectional study between March 2022 and July 2022 involving 978 pregnant women aged 16 to 50 years. It was carried out based on the scale for the assessment of fear and anxiety in pregnant women (AMICO_Pregnant) and the collection of sociodemographic data. Normality analysis was performed prior to univariate and bivariate statistical analysis.
Results: The sample was composed of a total of 978 pregnant women. The mean of the AMICO_Pregnant scale was intermediate (5.04 points; SD=2.36). The bivariate analysis showed a statistically significant relationship between the AMICO_Pregnant scale and the following variables: vaccination schedule status, contact with the disease, weeks of gestation, altered delivery or birth plan.
Conclusion: Women with pregnancies closer to term, with no contact with the disease, without a complete vaccination schedule, or who had undergone changes in their delivery or birth plans, showed higher levels of fear and anxiety.
Keywords: pregnancy, COVID-19, fear, anxiety, questionnaire, mental health, public health
A Letter to the Editor has been published for this article.
A Response to Letter by Mr Tasijawa has been published for this article.
Introduction
The coronavirus disease pandemic of 2019 (COVID-19) became a global health emergency resulting in the need to take measures to prevent the spread of the virus such as containment, quarantine, and border closures. These measures have produced profound changes in lifestyle, and the fear of getting infected with the disease and its possible consequences at a personal, family, or social level have generated high levels of anxiety.1–3
Data related to the COVID-19 pandemic has been evolving since the year 2020, where SARS-CoV-2 struck the entire world. The pandemic has not only resulted in physical disturbances, but has also led to psychological, economic, and social alterations. COVID-19 develops as a result of a respiratory tract infection caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).
This disease, which has affected the entire population to a greater or lesser extent, caused greater concern in certain vulnerable groups such as the elderly, the immunocompromised, or pregnant women, among others, due to previous illnesses or vital situations of special risk.4,5
COVID-19 has effects on the physical health, causing severe pneumonia, acute respiratory distress syndrome (ARDS), bacterial superinfection, cardiac alterations, shock, sepsis, thrombotic complications, pulmonary fibrosis, etc., and on mental health, especially anxiety and depression in the general population6 o it is associated with an increased risk of ICU admissions, hospitalisation,7–9 and although the existence of vertical transmission is extremely rare,10,11 there does appear to be evidence of an increased risk for developing pre-eclampsia, for threatened preterm birth, or low birth weight.12,13
During the pandemic, the impact this has had on the psychological health of the general population has been studied.14,15 However, there are few studies related to vulnerable population groups such as pregnant women.16,17 In addition, psychological reactions secondary to health crises seem to persist over time18 and in this sense, the presence of fear and anxiety on an ongoing basis and in the prenatal period constitutes one of the precursors of postpartum depression.19–21 Although the measures taken over the last three years have been fundamental in minimising the effects of the disease, this may have had a high psychological cost for certain population groups that needs to be assessed.
Previous studies have found that public health emergencies (eg 2003 SARS-CoV) triggered a range of emotional stress responses that involved increased levels of anxiety, fear, and other negative emotions.8,22,23
Fear is defined as a response of the organism that is triggered by a situation of physical or psychological threat or danger, the purpose of which is to provide the organism with energy to overcome or counteract it by means of a response that has an obvious survival purpose.24
However, it is one of the reactions that produces the greatest number of mental, behavioural, emotional, and psychosomatic disorders.25
Fear levels in pregnancy have been studied by many researchers in the pre-pandemic period, as the pregnant woman is considered a high-risk vulnerable group compared to the non-pregnant population due to both physical and psychological changes that occur during pregnancy. According to a systematic review, the prevalence of fear during pregnancy was 14% before the pandemic,26,27 and other research correlates low and high levels of fear of birth with prolonged labour, caesarean section, increased use of epidural analgesia, and prenatal and postpartum depression or anxiety.28–32
Some authors suggest that the psychological effects of uncertainty generated by health crises are more likely to persist over time,33 and that chronic fear and anxiety are precursors to psychological disorders such as depression or stress.34 These are negative emotions that are maintained over time and that, when identified as permanent in the individual, may predispose to physical illnesses and/or generate or aggravate previous mental disorders.35
On the other hand, some research has pointed to the relationship between maternal prenatal stress and anxiety levels with compromised optimal development of the hypothalamic-pituitary-adrenal axis (HPA), limbic system, and prefrontal cortex.36,37 Fear and concern about the disease affect the behaviour of individuals. Although there is no evidence of vertical transmission of SARS-CoV-2, uncertainty affects the most susceptible expectant mothers, as no one wants to be infected with a virus that presents a high risk of morbidity.38
Research on the psychological effect of the COVID-19 pandemic on pregnant women as a group of special vulnerability is still scarce in the Spanish population.23,24 Therefore, there is a need to assess levels of anxiety and fear as attitudinal factors that could be relevant in the adoption of preventive measures against new and future health threats that may require measures to restrict our freedom or health measures such as isolation or confinement.
In this context, for the assessment of the presence of fear and anxiety of COVID-19, a psychometric validation and development of the AMICO_Pregnant scale was carried out, a scale adapted and validated for specific use in the population of pregnant women in Spain. AMICO_Pregnant was designed by a panel of 10 experts using the Delphi technique and it was validated in previous studies, with a two-factor structure and 16 items that explained 78.936% of the variance. The version agreed by the panel of experts was piloted on a set of 1013 pregnant women with a mean age of 33.38 years and a standard deviation of 5.2 years, who completed a total of 978 surveys over a period of 4 months. In relation to the current pregnancy, 3.4% of the pregnant women were in the first trimester of pregnancy, 13.6% in the second one, and the majority were full-term (83%) (median=37 weeks). Over 58.8% were primigravidae and 98.7% had a singleton pregnancy. Pregnancy control was mainly low risk (52.1%).
The mean of the AMICO_Pregnant scale was 5.04 points (SD=2.36), with a range of scores from 1 to 10. The study of percentiles and quartiles allowed for a three-level relationship for the scale, ie low level with scores from 0 to 3.06, intermediate level from 3.07 to 6.53, and high level with a score above 6.54. The reliability indices measured by both Cronbach’s Alpha and McDonald’s Omega were 0.95 and 0.94, respectively. The bivariate analysis showed statistically significant relationships between the AMICO_Pregnant scale and some of the assessed obstetric variables.39
Methods
Objective
The aim of the study was to assess the levels of fear and anxiety of COVID-19 in the particularly vulnerable population group of women during pregnancy.
Hypothesis
There are significant differences between the level of anxiety and fear of COVID-19 and the different categories of the studied variables.
Design
Descriptive cross-sectional study based on questionnaires disseminated between 24 March and 26 July 2022.
Instrument
The study by Gomez-Salgado et al40 developed the Anxiety and Fear of COVID-19 Assessment Scale (AMICO), based on the original 10-item version of the FCV-19 scale and incorporating 8 new items assessing the specific presence of anxiety due to COVID-19. The research confirmed a two-dimensional structure of 16 items, as well as two factors that explained 64.8% of the variance.41 The reliability study gave a total Cronbach’s α value of 0.92 for factor 1 (Anxiety) and of 0.90 for factor 2 (Fear). The AMICO scale has been validated in different population groups: the elderly,42 nurses,43 the general adult population,44 or the general adult population in United Kingdom.45
In this context, the scale for assessing fear and anxiety of COVID-19 in pregnant women (AMICO_Pregnant) was designed and validated in a previous study based on the Spanish version of the AMICO scale. The adaptation of AMICO to the population of pregnant women was carried out using the Delphi technique by a panel of 10 experts with an academic level of Doctor or Official Master’s Degree and whose areas of knowledge were obstetrics, public health, or psychology; one of the experts was also pregnant at 28 weeks of gestation.
Exploratory factor analysis obtained a two-dimensional structure of 16 items (anxiety and fear) that could explain 78.935% of the variance (KMO test=0.962; Bartlett's test X2=19,100.292; p<0.000).
The reliability study was carried out with both Cronbach’s Alpha and McDonald’s Omega coefficient estimates, giving values of 0.95 and 0.94, respectively.
The questionnaire contains 16 items with a Likert-type response scale from 1 to 10, where 1 expresses a very low level of fear and anxiety and 10 a very high level. The total score of the scale is obtained by calculating the mean score from the self-reported responses, and the value ranges from 1 to 10 points. A mean total score ≤3.06 indicates a low level of fear and anxiety; a mean total score between 3.07 and 6.53 is indicative of intermediate levels of fear and anxiety; and a mean total score ≥6.54 would suggest a clinically relevant level of fear and anxiety. The Mann–Whitney U statistic confirmed the significant differences between the different levels, with values of p=0.001.39
Participants
The number of births registered in Spain during 2021 amounted to 337,380 births.46 The required sample size was calculated considering a confidence level of 95%, for a maximum sampling error of 5%, and it amounted to 385 participants.47 A probabilistic snowball sampling was carried out. The research team carried out a process of identification of professional associations and health centres which were asked to collaborate in the dissemination, guaranteeing the confidentiality of the data. However, the final sample obtained was 978 pregnant women.
Variables
Sociodemographic variables included age, place of residence, marital and cohabitation status, level of education, occupation and employment sector, personal history, obstetric history, relationship with the disease, feeling of danger, and vaccination status against COVID-19.
Finally, the last section of the questionnaire included the AMICO_Pregnant scale with the aim of measuring fear and anxiety of COVID-19 disease. The final survey consisted of a total of 33 items.
Procedure
The data collection tool was designed using the GoogleFoms© software. The questionnaire was disseminated by mass mailing to residents throughout Spain by a free national magazine with content and newsletters related to pregnancy and childcare (Mi Bebé y Yo), and a link and QR code redirecting to the aforementioned GoogleForms form was distributed to subscribers who had agreed to participate in the research.
In turn, different organisations related to perinatal care, professional associations, obstetrics and gynaecology nurse training centres, primary care centres, as well as public and private hospitals in the national territory also collaborated in the dissemination of the survey. The researchers contacted the different organisations that were asked to collaborate in the dissemination. Some professionals belonging to the different contacted organisations collaborated in the dissemination of the questionnaire when the pregnant woman went to her prenatal check-up. The nurse specialist in obstetrics and gynaecology offered her the possibility to participate in the study by means of a QR code that redirected her to the online questionnaire.
Once the respondent accessed the form, information was displayed on the legal conditions, consent, and confidentiality of data, which they had to accept in order to access the questionnaire; the form also included a contact e-mail address to provide a reference for consultation and exercise of rights and duties in terms of data confidentiality, and to make enquiries about the study.
Data Analysis
Univariate and bivariate data analysis was performed using the Statistical Program for Social Sciences (SPSS) version 28.0 package. First, an analysis of the normality of the distribution of the AMICO_Pregnant score data was performed by calculating the Kolmogorov–Smirnov test, showing a significance level of p=0.000, which indicated an absence of normality.
For the bivariate analysis, different non-parametric tests were used based on the specific characteristics of the variables studied: Wilcoxon signed-rank test, Kruskal–Wallis test, Mann-Whitney U-test, and Spearman’s Rho, also estimated to analyse the correlation between two quantitative variables.
Ethical Aspects
The study was conducted in accordance with the Declaration of Helsinki 2013 by the World Medical Association and the European Union’s Good Clinical Practice Directive (Directive 2005/28/EC). The research protocol was presented and approved by the Biomedical Research Ethics Committee of the province. The research protocol was also approved.48 All participants were informed about the procedure and objectives of the study, and they gave their informed consent prior to the start of data collection.
Results
Descriptive Analysis
The questionnaire was answered by a total of 1013 pregnant women over 18 years of age and with a mean age of 33.38 years (SD=5.28). Of the total sample, 35 (3.5%) women completed the questionnaire partially, resulting in a complete sample of 978. 3.4% were in the first trimester of pregnancy, 13.6% in the second trimester, and 83% in the third trimester (M=37; SD=3.44). 30% were recruited at the antenatal clinic of the University Regional Hospital of Malaga, Maternity Hospital.
Responses were also obtained from all the Spanish provinces. 60.9% of the responses were from the province of Malaga, being the province with the highest response rate, followed by 5.7% from Madrid and 4.1% from Barcelona. The provinces of Seville and Valencia had participation rates between 3% and 5%. The rest of the 47 provinces in Spain showed a participation rate of less than 3% (Table 1).
 |
Table 1 Description of the Sample |
In terms of marital status, 89.1% declared themselves to be in a relationship and only 10.9% were single; 47.5% said they were married, 41.1% were in a stable relationship, and 10.4%, 0.7%, and 0.4% said they were single, divorced or widowed, respectively. In relation to the employment sector, 33.6% belonged to the service sector, 22.8% to auxiliary, technological, or financial activities, 20.8% to the health sector, 13.9% to education, and the remaining 6.9% were engaged in other activities. 2% were unemployed.
The highest level of education was university (35.3%), followed by upper secondary school or vocational training (28.7%), and Master’s degree or doctorate (16.1%). Primary and secondary studies were reported by 3.4% and 15.7%, respectively, and only 0.8% had no studies.
Obstetric history showed a representative sample in terms of nulliparity or multiparity, with 58.8% being pregnant for the first time and 41.2% having been pregnant two or more times. 98.7% were singleton pregnancies and 68.7% were spontaneous conception and wanted pregnancies. Personal history showed 73.8% of pregnant women with no history of clinical interest and the main complaints were respiratory diseases, bronchial asthma, or previous pneumonia in 7.4%, followed by autoimmune diseases in 4.2% or coagulation problems in 3.1%.
In relation to contact with COVID-19 disease, 48.7% of the pregnant women had had contact with the disease, 9.1% stated that a member of their family had had contact with COVID-19, and the remaining 42.3% stated that they had not had contact with the disease or only outside their family circle. In this regard, 93.9% reported having received at least one dose of the COVID-19 vaccine. In relation to the influence of the disease on their birth plans, 19.6% acknowledged having suffered changes in their birth plans due to the pandemic situation.
In relation to the self-perception of the pandemic danger situation with respect to the previous year (2020) in a range of 1 to 10, the mean was 4.89 points (SD=2.07), and in relation to the self-perception of the levels of fear and anxiety with respect to the previous year, in a range of 1 to 10 the mean was 4.75 points (SD=2.49).
The mean of the AMICO_Pregnant scale was 5.04 points (SD=2.36). The bivariate analysis showed statistically significant differences in the mean score of the scale and the following variables: weeks of gestation, contact with the disease, vaccination schedule, and changes in the birth plan (Table 1). Pregnant women with pregnancies closer to term showed lower levels of fear and anxiety than those at lower gestational weeks (37 wk;  =5.04 p=0.000). In addition, pregnant women who had experienced the disease showed lower levels of fear and anxiety (
=5.04 p=0.000). In addition, pregnant women who had experienced the disease showed lower levels of fear and anxiety ( =4.66) than those who had not had contact with the disease (
=4.66) than those who had not had contact with the disease ( =5.22) or the contact had been outside their family circle (
=5.22) or the contact had been outside their family circle ( =5.23). On the other hand, pregnant women who had received any dose of the COVID-19 vaccine showed similar levels of fear and anxiety, with no significant differences between the number of doses received (1 dose=5.26; 2 doses=4.90; 3 doses=5.11). However, those who had not received any doses showed significantly lower levels (
=5.23). On the other hand, pregnant women who had received any dose of the COVID-19 vaccine showed similar levels of fear and anxiety, with no significant differences between the number of doses received (1 dose=5.26; 2 doses=4.90; 3 doses=5.11). However, those who had not received any doses showed significantly lower levels ( =3.09 sig.=0.000). In relation to changes in their birth plan, pregnant women who had not experienced changes in their birth plan or who had no birth or delivery plan showed lower levels of fear and anxiety (
=3.09 sig.=0.000). In relation to changes in their birth plan, pregnant women who had not experienced changes in their birth plan or who had no birth or delivery plan showed lower levels of fear and anxiety ( =4.33) than those whose birth plans had been modified (
=4.33) than those whose birth plans had been modified ( =6.04).
=6.04).
The bivariate analysis of the correlation between quantitative variables showed statistically significant results. On the one hand, between the levels of fear and anxiety according to the AMICO_Pregnant scale and the self-perception of the level of danger of the pandemic situation with that of a year earlier using the Tau B correlation coefficient (0.556 p=0.000), ie, pregnant women who reported a low level of danger showed lower levels of fear and anxiety. On the other hand, self-reported levels of fear and anxiety in relation to the pandemic situation one year earlier showed a strong relationship with levels of fear and anxiety assessed with the AMICO_Pregnant scale according to the Tau B correlation coefficient (0.727 p=0.000), ie pregnant women who self-reported a decrease in levels of fear and anxiety compared to one year earlier showed lower levels of fear and anxiety on the scale. Finally, there was no significance between anxiety and fear levels and the age of the pregnant woman.
Regression Analysis
A categorical regression analysis was performed with the mean total score of the AMICO_Pregnant scale as the dependent variable and the categorical variables that had shown significant differences in the bivariate analysis, showing an adequate adjustment; 28% of the variance of the data was explained by this regression model, which made it possible to identify the variables that predicted high levels of fear and anxiety: administered vaccinations, contact with COVID-19 patients, and changes in the birth plan obtained p-values <0.05 (Table 2).
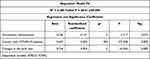 |
Table 2 Categorical Regression Model |
In this sense, the results showed that women who had received only one dose of vaccination had higher levels of fear and anxiety compared to those who had received a complete vaccination or even those who had not received any dose. Pregnant women who had not had contact with the disease within the family had higher levels of fear and anxiety, and finally, the existence of a birth plan that had undergone changes or the absence of any birth or delivery planning were shown to be events that increased the levels of fear and anxiety in pregnant women.
Discussion
This study attempts to indicate the effect that the COVID-19 pandemic has had on the levels of fear and anxiety in pregnant women as mediators of psychological well-being. This situation of special vulnerability with the presence of specific expectations and attitudes may have an impact on the ongoing pregnancy or become a determinant of the psycho-affective perception of the pregnant woman. However, when it comes to mental health in relation to the pandemic, it is difficult to find research that focuses exclusively on pregnant women despite being a particularly vulnerable group. Some authors have reported moderate levels of fear of the disease in pregnant women one year after the start of the pandemic.17
Fear during pregnancy may represent a relevant risk factor in the normal development of the current pregnancy; some authors point out an incidence between 45% and 77%.2,49,50 In this regard, there is research on the consequences that fear can have on infant psychophysiological development.23 Moreover, anxiety is an additional risk factor that intervenes in neonatal development in a number of ways.37,51–53
This research has shown the multiple circumstances that can have an impact on the levels of fear and anxiety of women with a pregnancy in progress, becoming determinants of their state of mind.
More specifically, the findings show that pregnant women show an intermediate level of fear and anxiety, in agreement with research carried out two years earlier, such as that by
Allande-Cussó et al,54 which assessed levels of fear and anxiety in the general population in Spain at the start of the pandemic, showing a psychological impact considered moderate. However, the work by Morgado-Toscano et al45 in the UK general population showed lower levels of psychological impact during the months of April to June 2021 in relation to both the studies by Allande-Cussó et al35 and the findings of the present study.
The results may have been influenced by several factors: first, the timing of data collection and the pandemic situation; during the data collection period of this research, vaccination coverage in Spain was above 92% in the population over 12 years of age, more than 92% of those over 60 years of age had received a booster dose, and the main indicators for monitoring the pandemic were at a low risk level in most parts of Spain.28
On the other hand, sex, especially if we compare a female-only population group with a group of both sexes, should be taken into account. It seems to be a determinant in the levels of fear and anxiety, and it may have contributed to intermediate levels despite the low risk situation of the pandemic at the time. Indeed, different studies have always shown higher levels in women compared to men.29
Uncertainty in relation to pregnancy or delivery plans, clinical variability, uncertainty in relation to contagiousness in their environment, the lack of a complete vaccination schedule and, consequently, uncertainty in relation to the disease and its effects on both mother and newborn have shown to be factors underlying these increases in the levels of fear and anxiety in pregnant women during the pandemic, according to the data collected. The group of women who had not been infected with COVID-19 showed higher levels of fear and anxiety when compared to the group of women who had been infected with COVD-19 or whose contact with the disease was limited to outside their family circle. These results support the data obtained in other research on the general population or on vulnerable population groups such as the elderly.42,54
A closer examination of the findings and conclusions of the authors cited above suggests that the uncertainty caused by an unexpected circumstance considered a threat to health, in this case a pandemic situation, can generate emotions of fear and anxiety in pregnant women55–57 as they do not know how to deal with a circumstance that alters their expectations and doubt their ability to adapt to the new circumstance, thus producing fear and mistrust towards the near future.58 On the other hand, the findings of this research in relation to the variables related to individual health do not show significant differences in the evaluation of the levels of fear and anxiety in relation to personal history, type of conception, type of prenatal control, number of embryos or number of previous pregnancies. In this sense, in agreement with other research, despite the situation of special vulnerability on a physiological level due to the changes that pregnancy produces in the woman and despite the fact that the health of the woman is fundamental for a state of well-being of the foetus, the woman prioritises the health of the pregnancy or of the baby over her own; this is a psychological approach linked to an innate attitude of protection of the offspring.27,37,59 However, the pandemic situation may have exacerbated this protective attitude and generated a response by increasing levels of fear and anxiety in women.33 In addition, multiparity has been considered by some authors as a protective factor against levels of anxiety and fear in relation to pregnancy or childbirth,34 probably due to the experience of having had a previous birth. However, the findings do not show significant differences between primigravidae and multigestation, which may be explained by the specificity of the questions asked in the data collection on fear and anxiety related to COVID-19 disease.
In relation to age or marital support as influential factors in the levels of fear and anxiety, the descriptive analysis used in the interpretation of the data shows a homogeneous sample in terms of age, which justifies the absence of significant differences, and on the other hand, a sample with 89.1% in a couple situation justifies the absence of significant differences in this sense.
In addition, social variables such as employment sector or level of education might have been particularly affected by the timing of the research, which was carried out with hardly any employment restrictions, which would justify the absence of significant differences.
Finally, pregnant women’s perceptions of danger may vary depending on multiple factors such as the information they receive, their experiences within their family circle, their social or work environment, and the way they feel about their pregnancy.23,49 Although the pandemic has brought about changes in lifestyle, in relationships with others, or with the healthcare system,60 when analysing the results obtained in this study, pregnant women who understood the pandemic situation to be better than in the past, which may suggest that they had adapted to living with the new normality, showed greater emotional resilience in the face of the present situation, reporting lower levels of fear and anxiety.
Therefore, the findings are consistent with current thinking on the emotional consequences of a pandemic.1,2,49,50,61 The pregnant woman, at first, tends to show negative feelings about the potential threat posed by the pandemic during pregnancy, with positive emotions emerging secondary to circumstances such as the vaccination schedule, weeks of gestation, maintenance of her birth plans, or previous experiences with the disease. This evolves into a state of ambiguity that is common in pregnant women due to feelings of vulnerability against which they do not feel prepared, but nevertheless, they face the threat thanks to their coping mechanisms and the support of their social circle.
Regarding the limitations of this research, it should be noted that 60.9% of the sample was collected from the city of Malaga. However, this province constitutes 3.6% of the country’s population and the sample collection process was not probabilistic. On the other hand, a high proportion of educated women participated, which is common in research, as educated women are the ones who participate the most in research.35 In this sense, therefore, the results obtained are not entirely extrapolable to the entire Spanish population despite the sample size, and besides, the pandemic situation has evolved differently in each geographical area. Another limitation is that none of the participants informed of mental health disorders, which may be attributed to the participants’ fear of reporting them.
Furthermore, the results obtained are in the context of the COVID-19 disease. However, despite the above limitations, the research has generated interesting results for the nursing clinical practice that may be applied in the context of other respiratory infectious diseases affecting a particularly vulnerable group such as pregnant women, as well as for the scientific community interested in the field of mental health.
Conclusion
The results of this research show certain characteristics of pregnant women who, despite a pandemic situation in a state of remission, reported intermediate levels of fear and anxiety. Pregnant women who were close to term, without previous close contact with the disease, without a complete vaccination schedule, and who had undergone changes in their pregnancy or birth expectations were more likely to report negative experiences in terms of levels of fear and anxiety. Given the potential consequences of untreated high levels of fear and anxiety during gestation,32,57,62 identifying women who are more immersed in their expectations of pregnancy and childbirth by working proactively to help manage greater flexibility towards the different deviations that may occur in pregnancy and childbirth can help moderate fear and anxiety if pregnancy and childbirth do not proceed according to their expectations. Mental health prevention and treatment in the antenatal period helps to mitigate the effects of high levels of fear and anxiety at a time of particular mental health vulnerability.
Funding
This research has not received any public or private funding.
Disclosure
Francisco Javier Muñoz-Vela and Regina Allande-Cussó are co-first authors for this study. The authors of this research have no conflicts of interest, and the research findings are the product of the analysis of the results obtained.
References
1. Tuncer SK, Yilmaz FA, Karakurt P, Ciltas NY. The Relationship between the Fear of Childbirth and Anxiety during the Covid-19 Pandemic. Galician Medical J. 2022;29(2):E202222. doi:10.21802/gmj.2022.2.2
2. Yesilcinar I, Guvenc G, Kinci MF, Pardes BB, Kok G, Knowledge SAA. Fear, and Anxiety Levels Among Pregnant Women During the COVID-19 Pandemic: a Cross-Sectional Study. Clin Nurs Res. 2022;31(4):758–765. doi:10.1177/10547738221085662
3. Tajalli S, Imani A. Tokophobia in Iranian women during the COVID-19 pandemic. Int J Reprod Biomed. 2021;19(11):1025–1026. doi:10.18502/ijrm.v19i11.9918
4. Du RH, Liang LR, Yang CQ, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5):2000524. doi:10.1183/13993003.00524-2020
5. Dashraath P, Wong JLJ, Lim MXK, et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222(6):521–531. doi:10.1016/j.ajog.2020.03.021
6. Eastin C, Eastin T. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;58(4):711.
7. DeBolt CA, Bianco A, Limaye MA, et al. Pregnant women with severe or critical coronavirus disease 2019 have increased composite morbidity compared with nonpregnant matched controls. Am J Obstet Gynecol. 2021;224(5):510.e1–510.e12. doi:10.1016/j.ajog.2020.11.022
8. Sattari M, Bashirian S, Masoumi SZ, et al. Evaluating Clinical Course and Risk Factors of Infection and Demographic Characteristics of Pregnant Women with COVID-19 in Hamadan Province, West of Iran. J Res Health Sci. 2020;20(3):e00488. doi:10.34172/jrhs.2020.22
9. Kajdy A, Sys D, Pokropek A, et al. Risk factors for anxiety and depression among pregnant women during COVID-19 pandemic - results of a web-based multinational cross-sectional study. Int J Gynaecol Obstet. 2022;160(1):167–186. doi:10.1002/ijgo.14388
10. Karimi-Zarchi M, Neamatzadeh H, Dastgheib SA, et al. Vertical Transmission of Coronavirus Disease 19 (COVID-19) from Infected Pregnant Mothers to Neonates: a Review. Fetal Pediatr Pathol. 2020;39(3):246–250. doi:10.1080/15513815.2020.1747120
11. Kotlyar AM, Grechukhina O, Chen A, et al. Vertical transmission of coronavirus disease 2019: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224(1):35. doi:10.1016/j.ajog.2020.07.049
12. Mullins E, Hudak ML, Banerjee J, et al. Pregnancy and neonatal outcomes of COVID-19: coreporting of common outcomes from PAN-COVID and AAP-SONPM registries. Ultrasound Obstet Gynecol. 2021;57(4):573–581. doi:10.1002/uog.23619
13. Doncarli A, Araujo-Chaveron L, Crenn-Hebert C, et al. Impact of the SARS-CoV-2 pandemic and first lockdown on pregnancy monitoring in France: the COVIMATER cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1). doi:10.1186/s12884-021-04256-9.\
14. Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547. doi:10.1016/S2215-0366(20)30168-1
15. Gómez-Salgado J, Andrés-Villas M, Domínguez-Salas S, Díaz-Milanés D, Ruiz-Frutos C. Related Health Factors of Psychological Distress During the COVID-19 Pandemic in Spain. Int J Environ Res Public Health. 2020;17(11):3947. doi:10.3390/ijerph17113947
16. Motrico E, Domínguez-Salas S, Rodríguez-Domínguez C, Gómez-Gómez I, Rodríguez-Muñoz MF, Gómez-Baya D. The Impact of the COVID-19 Pandemic on Perinatal Depression and Anxiety: a Large Cross-sectional Study in Spain. Psicothema. 2022;34(2):200–208. doi:10.7334/psicothema2021.380
17. Mamuk R, Ş A, Erdoğan A. Evaluation of the association between fear of COVID-19 and pregnancy distress. Afr Health Sci. 2023;23(1):59–71. doi:10.4314/ahs.v23i1.8
18. Leung GM, Lam TH, Ho LM, et al. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. 2003;57(11):857. doi:10.1136/jech.57.11.857
19. Latendresse G, Wong B, Dyer J, Wilson B, Baksh L, Hogue C. Duration of Maternal Stress and Depression: predictors of Newborn Admission to Neonatal Intensive Care Unit and Postpartum Depression. Nurs Res. 2015;64(5):331–341. doi:10.1097/NNR.0000000000000117
20. Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2000;50(5):275–285. doi:10.1097/00006199-200109000-00004
21. Guvenc G, Yesilcinar İ, Ozkececi F, et al. Anxiety, depression, and knowledge level in postpartum women during the COVID-19 pandemic. Perspect Psychiatr Care. 2021;57(3):1449–1458. doi:10.1111/ppc.12711
22. Mcalonan GM, Lee AM, Cheung V, et al. Immediate and Sustained Psychological Impact of an Emerging Infectious Disease Outbreak on Health Care Workers. Canadian J Psychiatry. 2007;52(4):241–247. doi:10.1177/070674370705200406
23. Matsushima M, Horiguchi H. The COVID-19 pandemic and mental well-being of pregnant women in Japan: need for Economic and Social Policy interventions. Disaster Med Public Health Prep. 2020;16(2):449–454. doi:10.1017/dmp.2020.334
24. Amparo B, Bonifacio S. Ramos Campos Francisco. Manual de psicopatología. 2020.
25. Piqueras Rodríguez JA, Ramos Linares V, Martínez González AE, Oblitas Guadalupe LA. Emociones negativas y su impacto en la salud mental y física. Suma Psicológica. 2009;16(2):85–112.
26. O’Connell MA, Leahy-Warren P, Khashan AS, Kenny LC, O’Neill SM. Worldwide prevalence of tocophobia in pregnant women: systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2017;96(8):907–920. doi:10.1111/aogs.13138
27. Akgor U, Fadıloglu E, Soyak B, et al. Anxiety, depression and concerns of pregnant women during the COVID-19 pandemic. Arch Gynecol Obstet. 2021;304(1):125–130. doi:10.1007/s00404-020-05944-1
28. Sitras V, Šaltytė Benth J, Eberhard-Gran M. Obstetric and psychological characteristics of women choosing epidural analgesia during labour: a cohort study. PLoS One. 2017;12(10):e0186564. doi:10.1371/journal.pone.0186564
29. Lukasse M, Schroll AM, Karro H, et al. Prevalence of experienced abuse in healthcare and associated obstetric characteristics in six European countries. Acta Obstet Gynecol Scand. 2015;94(5):508–517. doi:10.1111/aogs.12593
30. Lara-Cinisomo S, Zhu K, Fei K, Bu Y, Weston AP, Ravat U. Traumatic events: exploring associations with maternal depression, infant bonding, and oxytocin in Latina mothers. BMC Women's Health. 2018;18(1). doi:10.1186/s12905-018-0520-5
31. Sheen K, Slade P. Examining the content and moderators of women’s fears for giving birth: a meta-synthesis. J Clin Nurs. 2018;27(13–14):2523–2535. doi:10.1111/jocn.14219
32. Dencker A, Nilsson C, Begley C, et al. Causes and outcomes in studies of fear of childbirth: a systematic review. Women and Birth. 2019;32(2):99–111. doi:10.1016/j.wombi.2018.07.004
33. Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–627. doi:10.1016/S2215-0366(20)30203-0
34. Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288.
35. Sylvers P, Lilienfeld SO, LaPrairie JL. Differences between trait fear and trait anxiety: implications for psychopathology. Clin Psychol Rev. 2011;31(1):122–137. doi:10.1016/j.cpr.2010.08.004
36. Van Den Bergh BRH, Mulder EJH, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev. 2005;29(2):237–258. doi:10.1016/j.neubiorev.2004.10.007
37. Jeličić L, Sovilj M, Bogavac I, et al. The Impact of Maternal Anxiety on Early Child Development During the COVID-19 Pandemic. Front Psychol. 2021;12. doi:10.3389/fpsyg.2021.792053
38. Lin CY. Social reaction toward the 2019 novel coronavirus (COVID-19). Social Health Behav. 2020;3(1):1. doi:10.4103/SHB.SHB_11_20
39. Munoz-Vela FJ, Gómez-Salgado J, Rodriguez-Diaz L, Allande-Cussó R, Vazquez-Lara JM, Fagundo-Rivera J. Adaptación y estudio psicométrico de la escala para la medición del miedo y la ansiedad a la enfermedad COVID-19 en la mujer gestante. Front Public Health. 2023;11. doi:10.3389/fpubh.2023.1225822
40. Gómez-Salgado J, Allande-Cussó R, Domínguez-Salas S, García-Iglesias JJ, Coronado-Vázquez V, Ruiz-Frutos C. Design of fear and anxiety of covid-19 assessment tool in Spanish adult population. Brain Sci. 2021;11(3):1–9. doi:10.3390/brainsci11030328
41. Gómez-Salgado J, Allande-Cussó R, Rodríguez-Domínguez C, et al. Development and criterion validity of the COVID-19 anxiety and fear assessment scale: a cross sectional study. Sci Prog. 2021;104(4):003685042110502. doi:10.1177/00368504211050291
42. Vélez-Morón A, Andújar-Barroso RT, Allande-Cussó R, García-Iglesias JJ, Aquino-Cárdenas G, Gómez-Salgado J. Measuring anxiety and fear of Covid-19 among older people: psychometric properties of anxiety and fear of Covid-19 scale (AMICO) in Spain. BMC Public Health. 2022;22(1):1–11. doi:10.1186/s12889-022-13960-w
43. Morgado-Toscano C, Allande-Cussó R, Fagundo-Rivera J, et al. Initial Psychometric Development of the Fear and Anxiety to COVID-19 Scale in Nursing Professionals. An Occupational Health Assessment Tool. 2022. doi:10.2147/RMHP.S384080
44. Allande-Cussó R, Linares Manrique M, Gómez-Salgado J, et al. Anxiety and fear related to coronavirus disease 2019 assessment in the Spanish population: a cross-sectional study. Sci Prog. 2020;104(3):67.
45. Morgado-Toscano C, Gómez-Salgado J, Fagundo-Rivera J, et al. Anxiety and fear of COVID-19 in the UK general population: a cross-sectional study. Medicine. 2023;102(10):e33045. doi:10.1097/MD.0000000000033045
46. INEbase / Demografía y población /Fenómenos demográficos /Estadística de nacimientos. Movimiento natural de la población / Últimos datos. Available from: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736177007&menu=ultiDatos&idp=1254735573002.
47. Fox N, Hunn A, Mathers N. Sa m pling a nd Sa m ple Size Calculation The NIHR Research Design Service for York Shire & the Humber The NIHR RDS for the East Midla nds / York Shire & the Humber. 2009.
48. Centro Provincial de Málaga – comité de Ética de la Investigación – bioética Andalucía. Available from: https://www.bioetica-andalucia.es/3-comites-de-etica/3-3-comites-etica-investigacion-ceis/3-3-5-mapa-de-los-ceis/centro-provincial-de-malaga-comite-de-etica-de-la-investigacion/.
49. Cigaran RG, Botezatu R, Mineca EM, et al. The Psychological Impact of the COVID-19 Pandemic on Pregnant Women. HEALTHCARE. 2021;9(6):725. doi:10.3390/healthcare9060725
50. Fan HSL, Choi EPH, Rwt K, et al. COVID-19 related fear and depression of pregnant women and new mothers. Public Health Nurs. 2022;39(3):562–571. doi:10.1111/phn.13035
51. Robertson Blackmore E, Gustafsson H, Gilchrist M, Wyman C, O’connor TG. Pregnancy-Related Anxiety: evidence of Distinct Clinical Significance from a Prospective Longitudinal Study HHS Public Access. J Affect Disord. 2016;197:251–258. doi:10.1016/j.jad.2016.03.008
52. Huizink AC, Mulder EJH, De Medina PG R, Visser GHA, Buitelaar JK. Is pregnancy anxiety a distinctive syndrome? Early Hum Dev. 2004;79(2):81–91. doi:10.1016/j.earlhumdev.2004.04.014
53. Tandon P, O’Connor K, Nguyen G, Maxwell C, Huang V. The COVID-19 Pandemic Significantly Impacts Pregnancy Planning and Mental Health of Women With Inflammatory Bowel Disease. J Clin Gastroenterol. 2022.
54. Allande-Cussó R, Linares Manrique M, Gómez-Salgado J, et al. Anxiety and fear related to coronavirus disease 2019 assessment in the Spanish population: a cross-sectional study. Int J Med. 2021;104(3).
55. Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020;277:5. doi:10.1016/j.jad.2020.07.126
56. Han L, Bai H, Lun B, Li Y, Wang Y, Ni Q. The Prevalence of Fear of Childbirth and Its Association With Intolerance of Uncertainty and Coping Styles Among Pregnant Chinese Women During the COVID-19 Pandemic. Front Psychiatry. 2022;13:935760. doi:10.3389/fpsyt.2022.935760
57. Muñoz-Vela FJ, Rodríguez-Díaz L, Gómez-Salgado J, et al. Fear and Anxiety in Pregnant Women During the COVID-19 Pandemic: a Systematic Review. Int J Public Health. 2023;68.
58. Shakarami A, Mirghafourvand M, Abdolalipour S, Jafarabadi MA, Iravani M. Comparison of fear, anxiety and self-efficacy of childbirth among primiparous and multiparous women. BMC Pregnancy Childbirth. 2021;21(1). doi:10.1186/s12884-021-04114-8
59. Ravaldi C, Wilson A, Ricca V, Homer C, Vannacci A. Pregnant women voice their concerns and birth expectations during the COVID-19 pandemic in Italy. Women and Birth. 2021;34(4):335–343. doi:10.1016/j.wombi.2020.07.002
60. Liu CH, Koire A, Erdei C, Mittal L. Unexpected changes in birth experiences during the COVID-19 pandemic: implications for maternal mental health. Arch Gynecol Obstet. 2022;306(3):687. doi:10.1007/s00404-021-06310-5
61. Dymecka J, Gerymski R, Iszczuk A, Bidzan M. Fear of Coronavirus, Stress and Fear of Childbirth in Polish Pregnant Women during the COVID-19 Pandemic. Int J Environ Res Public Health. 2021;18(24):13111. doi:10.3390/ijerph182413111
62. Liu J, Liu S. The management of coronavirus disease 2019 (COVID-19). J Med Virol. 2020;92(9):1484–1490. doi:10.1002/jmv.25965
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
