Back to Journals » International Journal of General Medicine » Volume 15
Assessment of COVID-19 Symptoms Distribution According to Tobacco Products Consumption and Khat Chewing: A Potential Antinociceptive Role of Nicotine Among COVID-19 Patients
Authors Gosadi IM , Abulqusim EM , Atiah AI , Ageeli BH , Alhazmi DA, Hamzi MA, Somaily SY
Received 22 June 2022
Accepted for publication 8 September 2022
Published 15 September 2022 Volume 2022:15 Pages 7299—7309
DOI https://doi.org/10.2147/IJGM.S379592
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ibrahim M Gosadi,1 Ebrahim M Abulqusim,2 Abdulrahman I Atiah,2 Bander H Ageeli,2 Doa’a A Alhazmi,2 Marwah A Hamzi,2 Sara Y Somaily2
1Department of Family and Community Medicine, Faculty of Medicine, Jazan University, Jazan, 82621, Saudi Arabia; 2Faculty of Medicine, Jazan University, Jazan, 82621, Saudi Arabia
Correspondence: Ibrahim M Gosadi, Faculty of Medicine, Jazan University, P.O. Box: 2349, Jazan, 82621, Saudi Arabia, Tel +966562137711, Email [email protected]
Purpose: To assess the distribution of COVID-19 symptoms according to the consumption of tobacco products and khat chewing among samples of Saudi Arabian individuals.
Methods: This retrospective cohort study was conducted in the Jazan region of Saudi Arabia. Data was collected online via a self-administered questionnaire. The questionnaire measured demographic variables, COVID-19 symptoms and vaccination, comorbidities history, tobacco product consumption, and khat chewing. In addition, logistic regression was performed to assess the association between the clinical presentation of COVID-19 with tobacco product consumption and khat chewing.
Results: A total of 1026 subjects were recruited. The mean age of the participants was 31 years, and more than half were male (53%). Among the reported tobacco product consumption, hookah smoking was more frequently reported as a currently consumed tobacco product (14.3%), followed by cigarette smoking (11.5%) and chewing tobacco (3.8%). Thirteen percent (134) were khat chewers at the time of recruitment. The odds of reporting five symptoms or more were higher among patients who have never been tobacco product consumers (OR: 1.6, 95% CI: 1.15– 2.35) while accounting for khat chewing, age, vaccination status, and history of comorbidities. Nonetheless, the difference in symptom distribution with khat chewing status was not statistically significant.
Conclusion: The findings of the current investigation suggest the presence of a potential impact of nicotine toxicity in masking pain among the subjects infected with COVID-19. Therefore, it is possible to hypothesize that, with the potential masking effect of nicotine, infected smokers may be less likely to suffer from the symptoms and seek official healthcare services, including diagnostic services.
Keywords: COVID-19, tobacco, khat, Jazan, Saudi Arabia
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or COVID-19 is a highly infectious new coronavirus strain reported at the end of 2019 in Wuhan, China.1 Since then, the incidence of COVID-19 has rapidly and persistently increased. According to the latest reports of the World Health Organization, the number of confirmed cases worldwide exceeded 386 million, with almost six million deaths by February 2022.2
COVID-19 is a respiratory viral disease that can influence the cardiovascular, renal, gastrointestinal tract, and nervous systems. Those infected with SARS-CoV-2 can experience asymptomatic, mild, moderate, or severe symptoms. The main symptoms of COVID-19 are fever, cough, sore throat, malaise, headache, muscle pain, nausea, vomiting, diarrhea, anosmia, dysgeusia, and in critical cases, acute respiratory failure.3
The clinical presentation, magnitude of severity, and persistence of symptoms among patients affected with COVID-19 can vary. In a review by Sanyaolu et al, the severity of COVID-19 infection has been indicated to be increased among patients with a history of respiratory illnesses such as asthma and chronic obstructive pulmonary disease and other conditions such as cardiovascular disease, diabetes, and hypertension.4 Furthermore, other demographic factors, such as aging, have been postulated to influence infection susceptibility and disease outcomes.5 In addition to variation in clinical presentation and complications of COVID-19 infection, variation in the persistence of symptoms was reported. In a systematic review including 45 studies with 9751 patients who were followed up to assess persistence of symptoms, it was concluded that 72.5% of the patients reported at least one symptom at day 60 or more after diagnosis, symptoms onset, or hospitalization; or day 30 after recovery from the acute phase or hospital discharge.6
The first mass vaccination program for COVID-19 was initiated by the end of 2020.7 Vaccination against COVID-19 has been reported to minimize the risk of infection, reduce the severity of the disease, and hospitalization.8 Nonetheless, in addition to the influence of demography, comorbidity, and vaccination on the course of the disease, other lifestyle factors have been reported to influence COVID-19 outcomes.9
One of the lifestyle factors that may influence the outcomes of COVID-19 infection is tobacco product consumption. According to the World Health Organization, 22.3% of the world population used tobacco in 2020. Furthermore, tobacco product consumption has been reported to contribute to the death of eight million individuals worldwide yearly.10 Several investigations assessing the potential influence of tobacco product consumption on modifying COVID-19 infection outcomes have been reported. However, the identified studies reported conflicting evidence concerning the association between the consumption of tobacco products and COVID-19. In a study including 1688 navy aircraft carrier crewmembers, 1279 (76%) were diagnosed with COVID-19. The odds of COVID-19 infection were estimated according to smoking status (current smokers versus former and never smokers), revealing an odds ratio (OR) of 0.59 (95% confidence interval [CI] 0.45–0.78), suggesting a lower risk of infection among smokers.11 A similar notion was reported in a living evidence review aiming to assess the association of smoking status with COVID-19 infection, hospitalization, and mortality (version seven updated up to 25th of August 2020), which included 233 studies that concluded that current smokers were at lower risk of infection compared to never smokers (RR: 0.74 [95% Crl: 0.58–0.93]). However, it was indicated that former smokers were at increased risk of hospitalization compared to never smokers (RR: 1.20 [95% Crl: 1.03–1.44]).12 Nonetheless, other evidence was reported suggesting contradicting findings.
A systematic review and meta-analysis assessed the risk of adverse outcomes of COVID-19 according to smoking history. The meta-analysis, which included 40 studies, reported that current and former smokers were at higher risk of disease severity (OR=1.58; 95% CI: 1.16–2.15, and OR=2.48; 95% CI: 1.64–3.77). Similarly, a higher risk of death was detected among current and former smokers compared to never smokers (OR=1.35; 95% CI: 1.12–1.62; and OR=2.58; 95% CI: 2.15–3.09).13
Khat is a plant that contains cathinone, which has amphetamine-like pharmacological characteristics.14 The habit of khat chewing is widely practiced in eastern African countries such as Ethiopia,15 Southwestern regions of the Arabian peninsula, including Yemen,16 and the southwest of Saudi Arabia.17 Khat chewing has been reported to have a harmful impact on health18 and is commonly practiced with smoking.19 However, studies that assessed the effect of khat chewing on COVID-19 infection are limited to a review suggesting a higher risk of infection among khat chewers because khat chewing is commonly practiced during social gatherings in confined and poorly ventilated spaces and thus, increasing the risk of infection.20 Nonetheless, the impact of khat chewing on COVID-19 infection severity has not been investigated.
According to smoking history, contradictory findings have been reported concerning the association between COVID-19 infection susceptibility, severity, and persistence of symptoms. Additionally, the association between COVID-19 and khat chewing has not been reported. Therefore, in this investigation, we aimed to assess the association between COVID-19 symptoms distribution concerning tobacco product consumption and khat chewing among samples of Saudi Arabian individuals diagnosed with COVID-19.
Methods
Study Context
This investigation was a retrospective cohort study in the Jazan region, southwest Saudi Arabia, between June and July 2021. The Standing Committee for Scientific Research Ethics, Jazan University, granted ethical approval to conduct the study (approval number REC42/1/149 dated June 2021). Data was collected online, targeting subjects living in the Jazan region diagnosed with COVID-19. The current investigation complies with the Declaration of Helsinki and informed consent was obtained before the participation of the targeted subjects. Khat chewing is common in Jazan, where the current available prevalence studies reported that cigarette smoking, hookah smoking, and khat chewing were 10.16%,21 15.3%,22 and 33.2%.17
Data Collection
After consulting the literature, a self-administered questionnaire was developed and composed of the following sections. The first section contained questions measuring patients’ demographics such as age, gender, social status, residence, educational level, and occupation. The second section was developed to assess the presence of symptoms after COVID-19 infection, where question items were dependent on a review by Cascella et al.3 Finally, the third section was designed to measure tobacco product consumption and khat chewing practice, where items measuring consumption were retrieved from previous investigations measuring smoking consumption and khat chewing in the Jazan region.17,21,22 A consultant in epidemiology assessed the content of the questionnaire, and piloting of the study instrument was performed on 15 male and female participants to test the face validity of the instrument, clarity of the questions, and time needed to complete the questionnaire.
Researchers targeted adult patients living in the Jazan region diagnosed with COVID-19 since the pandemic’s start until data collection time to achieve the research objectives. The investigation included any adult who was a confirmed COVID-19 patient by a standard healthcare facility in the region. Subjects under 18 years old and those who were not confirmed cases of COVID-19 were excluded.
Recruitment of the participants was performed electronically. The developed questionnaire was converted to an online survey enabling completion by the participants, and distributed to the targeted population online via social media. A screening question was presented at the beginning to ensure that participants met the inclusion criteria. Data collection was anonymous, and participation in the survey was voluntary. Non-random snowball sampling was utilized, where participants who completed the questionnaire were requested to share the survey link with other potential participants.
Sample size estimation was based on the findings of Gülsen et al, where the odds of higher COVID-19 severity for smokers was 2.16 (95% CI: 1.37–3.46).23 A sample of 879 was estimated via StatCal function of EpiInfo by utilizing the Unmatched Cohort and Cross-section Studies option according to the following parameters: Assuming 95% two-sided confidence level, power of 80%, exposure ratio of 2, the proportion of outcome in unexposed of 10.7%, and proportions of outcome in exposed of 20.6% and an OR of 2.16.
Data Analysis
The statistical package for the social sciences (version 25) was used to analyze the data. The summary of study variables was presented using descriptive statistics, including mean, frequency counts, and percentages for binary and categorical variables. A symptom severity index was calculated by summing the number of reported symptoms or complications where binary classification of severity was performed. The median number of reported symptoms was five. This point was used to group patients with fewer than five symptoms and patients with five or more symptoms together. Multivariate logistic regression was used to assess the association between tobacco product consumption or khat chewing with the distribution of the symptoms, where the symptoms were presumed as the outcome, and tobacco product consumption or khat chewing was presumed as independent factors while accounting for patients’ characteristics. A p value of < 0.05 was considered a statistically significant value for the applied statistical tests.
Results
A total of 1044 individuals diagnosed with COVID-19 in Jazan were identified, of whom 18 were excluded due to not meeting the inclusion criteria. Table 1 describes the demographic characteristics, tobacco product consumption, and khat chewing among the included participants. The mean age of the participants was 31 years, and more than half were males (53%). The majority of the participants were Saudis (96.3%), and more than half were married (51.7%) and were living in rural areas (51.7%). In addition, most participants reported having a university-level education (73.8%), 46.2% reported having a monthly income of less than 5000 Saudi Arabian Riyal (SAR), and 20% described themselves as unemployed.
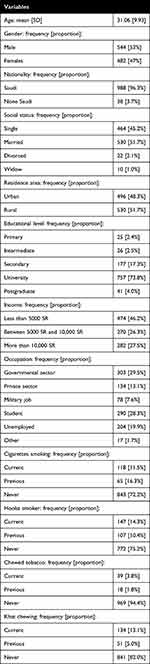 |
Table 1 Demographic Characteristics, Tobacco Products Consumption and Khat Chwing Among 1026 Individuals from Jazan, Saudi Arabia, Whom Were Diagnosed with COVID-19 |
Among the reported tobacco product consumption, hookah smoking was more frequently reported as a currently consumed tobacco product (14.3%) compared to cigarette smoking (11.5%) and chewing tobacco (3.8%). When observing the ever-consumed tobacco product, it can be noted that chewing tobacco was the least frequently reported compared to other tobacco products. Finally, 134 (13.1%) participants reported being current khat chewers at the time of recruitment.
Table 2 describes the clinical presentation, history of morbidity, and receipt of COVID-19 vaccination of the recruited sample. Among the assessed symptoms, the most frequently reported symptom was fever (66.3%), followed by headache (64.9%), and muscle ache (63.7%). Among the identified histories of comorbidities, asthma was more frequently reported (14.7%). Finally, more than half the participants reported receipt of a COVID-19 vaccine at the time of the recruitment (54.3%).
 |
Table 2 Clinical Presentation, History of Comorbidity, and Receipt of COVID-19 Vaccination Among 1026 Individuals from Jazan, Saudi Arabia, Whom Were Diagnosed with COVID-19 |
When asked about anosmia, 56.5% of subjects reported a loss of sense of smell. Similarly, 36.8% of subjects reported ageusia. The median duration for the persistence of loss of smell was 14 days since infection and varied between one day to 510 days. Additionally, the median duration for the persistence of loss of taste was 11 days since infection and varied between two days to 370 days.
Table 3 illustrates the distribution of COVID-19 symptoms according to tobacco and khat consumption status. When observing the frequency of reporting the symptoms concerning tobacco product consumption, it can be noted that the proportion of patients who were current tobacco product consumers reported experiencing fewer symptoms compared to previous or never consumers of tobacco products. This notion applies to all reported symptoms, of which differences concerning reporting of cough, myalgia, and headache were statistically significant (p values < 0.05). A similar notion can also be seen among the khat chewers, but with less variation, where fever and myalgia were less frequently reported among current khat chewers compared to previous or never khat chewers (p values < 0.05).
 |
Table 3 Distribution of COVID-19 Symptoms Among 1026 Individuals from Jazan, Saudi Arabia, Whom Were Diagnosed with COVID-19 and Classified According to Tobacco Products Consumption and Khat Chewing |
Assessment of the distribution of the symptoms revealed that 626 patients (61%) reported having five or more symptoms. As illustrated in Table 3, the number of patients who reported suffering from five or more COVID-19 symptoms was higher among patients who reported previous or never tobacco product consumption (p value of 0.002). Nonetheless, the difference in symptom distribution according to khat chewing status groups was not statistically significant.
In Table 4, multivariate logistic regression was performed to assess the association between tobacco product status and khat chewing status with the odds of reporting five symptoms or more. It was noted that the odds of reporting five symptoms or more were higher among patients who have never been tobacco product consumers (OR: 1.6) and patients who were diagnosed with asthma (1.7), and the odds were lower among males (0.6) with statistically significant values (p values < 0.05) while controlling for khat chewing, age, COVID-19 vaccination status, history of diabetes, hypertension, and cardiac diseases.
Discussion
This investigation was a cross-sectional study that targeted individuals from Jazan diagnosed with COVID-19 and assessed the distribution of the disease symptoms according to tobacco product consumption and khat chewing. The investigation findings indicate that consumers of tobacco products suffered fewer COVID-19 symptoms compared to those who were not consumers. The association between khat chewing and symptoms distribution was less apparent than the findings related to tobacco product consumption.
Our multivariate logistic regression findings suggest that male patients and patients who are current tobacco consumers are less likely to report COVID-19 symptoms than females and patients who are never tobacco consumers. Similarly, patients with a history of asthma are more likely to suffer from COVID-19 symptoms. Although studies assessing the association between smoking and COVID-19 severity are variable and conflicting, the findings of our investigation can be compared to similar literature.
An Italian study by Prinelli et al analyzed the data of 6857 individuals, where 1691 cases were confirmed with COVID-19 via nasopharyngeal swab. Prinelli et al assessed the distribution of symptoms according to the subjects’ smoking status. It was noted that the reporting of fever, myalgia, loss of smell or taste, cough, or pneumonia was less frequent among current smokers compared to never smokers or former smokers (p values < 0.05), which is similar to the findings of our study. In addition, their multivariate logistic regression findings indicate lower odds of reporting disease symptoms among current smokers compared to never smokers among the 1691 confirmed cases.24
Nonetheless, other literature provided contradicting evidence, especially concerning the influence of smoking on COVID-19 severity. A systematic review and meta-analysis were conducted involving 47 eligible studies with a total of 32,849 hospitalized patients, of whom 1501 were current smokers. The severity of COVID-19 was based on the presence of respiratory distress, oxygen saturation level, and arterial partial pressure of oxygen. It was concluded that current smokers had an increased risk of severe COVID‐19 (risk ratios [RR]: 1.80; 95% [CI]: 1.14‐2.85; P = 0.012), and severe or critical COVID‐19 (RR: 1.98; CI: 1.16‐3.38; P = 0.012).25 A UK study recruited users of the Zoe COVID-19 Symptom Study app around the UK, resulting in the recruitment of 401,982 participants with a smoking prevalence of 11%. Among their sample, 7123 COVID-19 patients were included, where the symptoms were assessed according to several characteristics, including smoking status, and suggested a higher risk of developing a fever, persistent cough, and shortness of breath among the current smokers of the standard users of the app (OR [95% CI] = 1.14 [1.10 to 1.18]). However, their study did not identify a pattern suggesting higher reporting of individual symptoms when comparing smokers to non-smokers among those diagnosed with COVID-19.26
Another hospital-based investigation assessed the association between inflammatory and hematological biomarkers among hospitalized patients with COVID-19 infection and classified samples of 200 patients according to their smoking status. Current smokers had higher neutrophil counts, NLR values, and CRP levels than never smokers, suggesting a poorer prognosis of COVID-19 among hospitalized smokers than hospitalized never smokers.27 Another UK Biobank-based study identified 1649 COVID-19 infections that reported higher odds of hospitalization (OR 1.80, 95% CI 1.26 to 2.29) among current smokers compared to never smokers.28 Another smaller-scale systematic review and meta-analysis suggested similar findings.23
Despite the evidence suggesting higher severity and mortality among smokers infected with COVID-19, other studies indicate less frequent reporting of COVID-19 symptoms among smokers. A systematic review and meta-analysis involving 30 retrospective observational studies with 6515 patients diagnosed with COVID-19 with a low prevalence of current smoking among hospitalized patients were concluded. Additionally, the review reported higher odds of adverse infection outcomes among former smokers than current smokers suggesting a potential influence of smoking-related toxicity on COVID-19 symptoms.29
After observing the conflicting findings concerning the association between smoking and COVID-19, it can be concluded that most studies assessing the association between smoking and COVID-19 infection indicate a worsening impact of smoking on the prognosis of patients and a higher tendency for hospitalization and mortality. However, studies that assessed symptom distribution according to smoking status, including our current investigation, suggest that smokers are less likely to report suffering fever, headache, and muscle pain than never smokers. This notion suggests a potential impact of nicotine toxicity on masking pain among the infected subjects. A review by Shi et al reported the pathophysiology and clinical implications of smoking on pain sensation and detailed physiological changes induced by nicotine exposure. In addition, several animal-based and human studies suggested analgesic properties of nicotine via affecting central and peripheral nicotine acetylcholine receptors and indicate that chronic exposure to smoking may alter pain perception among smokers compared to non-smokers.30
Our investigation was limited to patients diagnosed with COVID-19 and did not include individuals with no history of the disease. The review by Simons et al12 and the study by Paleiron et al11 suggest that smokers were at a lower risk of contracting COVID-19. Although our investigation did not assess the risk of contracting the infection, we detected a lower frequency of COVID-19 symptoms among current smokers. Therefore, it is possible to postulate that, with the potential masking effect of nicotine, infected smokers may be less likely to suffer from the symptoms and seek official healthcare services, including diagnostic services.
Strengths and Limitations
This study has multiple areas of strengths and limitations. The main strengths of the current study are related to its ability to reach a sample of subjects diagnosed with COVID-19 and assess their tobacco consumption and khat chewing practice. Furthermore, the study targeted the general population diagnosed with COVID-19 with demographic and clinical characteristics variations, which relatively enabled the generalization of the study findings. However, the study’s limitations are related to the potential selection bias resulting from the inability to reach subjects who are not social media users, including illiterate individuals. Moreover, a limitation is related to the inability to assess the dose-response relationship concerning tobacco product consumption and khat chewing with the distribution of COVID-19 symptoms.
Conclusion
The current investigation findings suggest the presence of analgesic properties of nicotine among consumers of tobacco products. This may explain the lower frequency of COVID-19 symptoms among the current tobacco products consumers compared to those who have never used tobacco products. In addition, khat chewing practice did not seem to be associated with variation in reporting COVID-19 symptoms. Our investigation suggests a need for further research on the pathophysiology of nicotine among smokers and its impact on the development of symptoms.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi:10.1056/NEJMoa2001316
2. World Health Organization. WHO coronavirus disease (COVID-19) dashboard; 2020. Available from: https://covid19.who.int/.
3. Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). In: StatPearls. Treasure Island (FL): StatPearls Publishing. Copyright © 2022, StatPearls Publishing LLC; 2022.
4. Sanyaolu A, Okorie C, Marinkovic A, et al. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. 2020;2(8):1069–1076. doi:10.1007/s42399-020-00363-4
5. Bajaj V, Gadi N, Spihlman AP, Wu SC, Choi CH, Moulton VR. Aging, immunity, and COVID-19: how age influences the host immune response to coronavirus infections? Front Physiol. 2020;11:571416. doi:10.3389/fphys.2020.571416
6. Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA network open. 2021;4(5):e2111417. doi:10.1001/jamanetworkopen.2021.11417
7. World Health Organization. Coronavirus disease (COVID-19): vaccines; 2022.
8. CDC. Possibility of COVID-19 illness after vaccination; 2021. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/effectiveness/why-measure-effectiveness/breakthrough-cases.html.
9. Li S, Hua X. Modifiable lifestyle factors and severe COVID-19 risk: a Mendelian randomisation study. BMC Med Genomics. 2021;14(1):38. doi:10.1186/s12920-021-00887-1
10. World Health Organization. Tobacco; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/tobacco#:~:text=Over%2080%25%20of%20the%20world%27s,(WHO%20FCTC)%20in%202003.
11. Paleiron N, Mayet A, Marbac V, et al. Impact of tobacco smoking on the risk of COVID-19: a large scale retrospective cohort study. Nicotine Tob Res. 2021;23(8):1398–1404. doi:10.1093/ntr/ntab004
12. Simons D, Shahab L, Brown J, Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7). Addiction. 2021;116(6):1319–1368. doi:10.1111/add.15276
13. Umnuaypornlert A, Kanchanasurakit S, Lucero-Prisno DEI, Saokaew S. Smoking and risk of negative outcomes among COVID-19 patients: a systematic review and meta-analysis. Tob Induc Dis. 2021;19:09. doi:10.18332/tid/132411
14. Halbach H. Medical aspects of the chewing of khat leaves. Bull World Health Organ. 1972;47(1):21–29.
15. Rather RA, Berhanu S, Abaynah L, Sultan M. Prevalence of Khat (Catha edulis) chewing and its determinants: a respondent-driven survey from Hossana, Ethiopia. Subst Abuse Rehabil. 2021;12:41–48. doi:10.2147/SAR.S324711
16. Hassan NA, Gunaid AA, Murray-Lyon IM. Khat (Catha edulis): health aspects of khat chewing. Eastern Mediterr Health j. 2007;13(3):706–718.
17. Mahfouz MS, Rahim BE, Solan YM, Makeen AM, Alsanosy RM. Khat chewing habits in the population of the Jazan Region, Saudi Arabia: prevalence and associated factors. PLoS One. 2015;10(8):e0134545. doi:10.1371/journal.pone.0134545
18. Al-Motarreb A, Baker K, Broadley KJ. Khat: pharmacological and medical aspects and its social use in Yemen. Phytother Res. 2002;16(5):403–413. doi:10.1002/ptr.1106
19. Al-Sanosy RM. Pattern of khat abuse and academic performance among secondary school and college students in Jazan region, kingdom of Saudi Arabia (ksa). J Family Community Med. 2009;16(3):89–95.
20. Yousuf A, Musa R, Isa M, Arifin SR. Vaping and Khat (Catha edulis Forsk) Chewing during COVID-19 pandemic. SSRN Electronic J. 2020. doi:10.2139/ssrn.3733764
21. Algabbani A, Almubark R, Althumiri N, Alqahtani A, BinDhim N. The prevalence of cigarette smoking in Saudi Arabia in 2018. Food Drug Regul Sci J. 2018;1:1. doi:10.32868/rsj.v1i1.22
22. Quadri MF, Saleh SM, Alsanosy R, et al. Effectiveness of an intervention program on knowledge of oral cancer among the youth of Jazan, Saudi Arabia. Asian Pac J Cancer Prev. 2014;15(5):1913–1918. doi:10.7314/APJCP.2014.15.5.1913
23. Gülsen A, Yigitbas BA, Uslu B, Drömann D, Kilinc O. The effect of smoking on COVID-19 symptom severity: systematic review and meta-analysis. Pulm Med. 2020;2020:7590207. doi:10.1155/2020/7590207
24. Prinelli F, Bianchi F, Drago G, et al. Association between smoking and SARS-CoV-2 infection: cross-sectional study of the EPICOVID19 internet-based survey. JMIR Public Health Surveill. 2021;7(4):e27091. doi:10.2196/27091
25. Reddy RK, Charles WN, Sklavounos A, Dutt A, Seed PT, Khajuria A. The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. J Med Virol. 2021;93(2):1045–1056. doi:10.1002/jmv.26389
26. Hopkinson NS, Rossi N, El-Sayed Moustafa J, et al. Current smoking and COVID-19 risk: results from a population symptom app in over 2.4 million people. Thorax. 2021;76(7):714–722. doi:10.1136/thoraxjnl-2020-216422
27. Çetin Kargin N. The effect of smoking on COVID-19-linked biomarkers in hospitalized patients with COVID-19. J Clin Lab Anal. 2021;35(10):e23983. doi:10.1002/jcla.23983
28. Clift AK, von Ende A, Tan PS, et al. Smoking and COVID-19 outcomes: an observational and Mendelian randomisation study using the UK Biobank cohort. Thorax. 2022;77(1):65–73. doi:10.1136/thoraxjnl-2021-217080
29. Farsalinos K, Barbouni A, Poulas K, Polosa R, Caponnetto P, Niaura R. Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis. Ther Adv Chronic Dis. 2020;11:2040622320935765. doi:10.1177/2040622320935765
30. Shi Y, Weingarten TN, Mantilla CB, Hooten WM, Warner DO. Smoking and pain: pathophysiology and clinical implications. Anesthesiology. 2010;113(4):977–992. doi:10.1097/ALN.0b013e3181ebdaf9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

