Back to Journals » Journal of Multidisciplinary Healthcare » Volume 12
Assessment Of Ambient-Noise Exposure Among Female Nurses In Surgical Cardiac Intensive Care Unit
Authors Alduais SA, Salama KF
Received 11 July 2019
Accepted for publication 10 October 2019
Published 5 December 2019 Volume 2019:12 Pages 1007—1011
DOI https://doi.org/10.2147/JMDH.S222801
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Video abstract presented by Khaled F Salama.
Views: 100
Safa A Alduais,1 Khaled F Salama2
1Saud Albabtain Cardiac Center, Dammam, Saudi Arabia; 2Department of Environmental Health, College of Public Health, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
Correspondence: Khaled F Salama
Department of Environmental Health, College of Public Health, Imam Abdul Rahman Bin Faisal University, PO Box 1982, Dammam 31441, Saudi Arabia
Email [email protected]
Purpose: To measure noise levels in the Saud Albabtain Cardiac Center cardiac surgical intensive-care unit (CSICU) at different locations to find out the prevalence of noise-induced hearing loss among female nurses.
Methods: Ambient CSICU noise was measured using a sound-level meter and personal noise dosimeter during morning and night shifts (12 hours each) for 30 days. An audiometry test and questionnaire were used to test nursing responses to noise levels.
Results: Mean 12-hour average noise levels at the station during night shift were 60.3±7.1 dB(A) and inside rooms 62.48±8.02 dB(A). However, during morning shift 64.1±8.4 dB(A) in the rooms was recorded, while 68.8±8.2 dB(A) was recorded at the station, with a significant difference between the shifts (p<0.0001). ICU monitors recorded the highest noise-source levels of 82.7±5.3 dB(A). The lowest significant source was the suction machines, with an average of 67.1±12.5 dB(A). A significant correlation between decibel loss and nurse experience was observed.
Conclusion: Noise levels in the CSICU at Saud Albabtain Cardiac Center were higher than World Health Organization standards. CSICU nurses are exposed to noise levels that can affect their hearing capacity. Further research isneeded for effective medical device–alarm management.
Keywords: ambient noise, intensive-care unit, nurses, audiometry, hospital
Introduction
Exposure to ambient noise in hospital might have negative effects on nurses, patients, doctors, and other staff alike.1 In intensive-care units (ICUs), patients need a healthy, quiet environment to recover, as they are particularly vulnerable to the effects of multisource exposure to daily noise that might interfere with the their recovery.2,3 In many ICU-related professions, noise may have severe psychological impact, such as loss of concentration and missed communication, which can lead to significant fatigue. Moreover, with long working duration, it might lead to noise-induced hearing loss.4
In a hospital setting, medical staff are at risk of exposure to high levels of noise, and in some departments, eg, ICUs and emergency rooms, levels might exceed the widely recognized maximum daily dose over an 8-hour shift.5 The World Health Organization(WHO)-recommended acceptable noise levels for a hospital-care setting are 30 dB(A) at night and 35 dB(A) during the day.1 In ICUs, the purpose of alarms is to communicate a deviation from “normal” patient status, improving safety and staff attention. However, false alarms are a significant issue due to nurse desensitization, allowing less importance to be placed on alarms and thereby compromising patient safety.6
Hearing loss is rated as a common sensory impediment for individuals nowadays that can lead them to live a disabled life. Nonetheless, it is considered a preventable injury when produced by occupational noise.7 Recent Swedish studies found that noise levels in ICUs remain high and that only 10% of ICU staff decrease volumes on alarms, monitors and ventilators during the day8
Methods
Study Setting
The main aim of the present study was to determine levels of ambient noise and related health effects in the surgical cardiac ICU (CSICU) at Saud Albabtain Cardiac Center. The CSICU's capacity is ten beds (eight regular and two isolation beds), with a total of 35 nurses covering the unit. A cross-sectional study was conducted on two samples: one from the CSICU nurses and the other from female cardiac ward (FCW) nurses as an equivalent comparison group.
Ambient-Noise Data Collection
Noise levels in the CSICU was measured using a sound-level meter (TES 1352A, EC Pub 651 type 2, ANSI S1.4 type 2) with a range of 30–130 dB and real-time measurement. It has a 1.27 cm electret condenser microphone and accuracy of ±1.5 dB (ref 94 dB@1KHz), with a battery life of about 30 hours.9
Personal Noise-Exposure Monitoring
A noise dosimeter was carried by the nurses in both the CSICU and FCW every day for 1 month. The dosimeter used was manufactured by Extech and has a measurement range of 70–140 dBA\0.1 dB. The device is ANSI S1.25 (1991) type 2, ISO-1999, BS 402 (1983). Its dimensions and weight are 106×64×34 mm and 227 g, including batteries. It comes with a 1.27 cm electret condenser microphone and a 79 cm cable.10
Audiometric Testing And Questionnaire Data
CSICU nurses were selected randomly to undergo audiometry in order to have a general idea of the condition of their hearing. Tests were conducted with the nurse in a soundproof room.
Questionnaire Data
A modified, structured, reliable, and validated questionnaire11 was given to the nurses to evaluate history, noise habits, and other psychological effects of noise exposure throughout the duration of their work.
Data Analysis
Significance was assessed with the independent t-tests and correlation analyses. Data were recorded, tabulated, and analyzed using SPSS 24.
Results
Sociodemographic characteristics of respondents are presented in Table 1. The mean age of the respondents was 33.4±4.8 years, while 22 (40%) were aged 20–30 years. Moreover, respondents’ median duration of working experience was 10 years, though over half (60%) had worked for 5–10 years. In addition, most respondents (67.2%) had bachelor’s degrees. However, the majority of nursing staff in the ICU were from South Asian countries (93.4%).
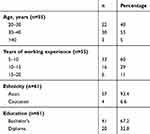 |
Table 1 Sociodemographic variables of ICU participants |
The mean 12-hour sound level during the night shift (inside the room) was 60.3±7.1 dB(A) and outside the room (nursing station) 62.48 ±8.02 dB(A). However, during the morning shift, readings inside and outside the room were 64.1±8.4 dB(A) and 68.8±8.2 dB(A), respectively. As shown in Table 2, there was a statistically significant difference between morning- and night-shift noise-levels readings (p<0.0001). Interestingly, maximum noise levels at the nursing station reached 89 dB(A) in the morning compared to 93.9 dB(A) at night.
 |
Table 2 Ambient-noise levels during night and morning shifts in ICU |
A noise-measurement chart was created for the CSICU devices. This showed that the highest levels were produced by monitors at the nursing stations, with noise levels of 82.7±5.3 dB(A), as shown Figure 1. The least significant source was the suction machine, with average levels of 67.1±12.5 dB(A). However, all noise sources exceeded the WHO standards, which represents a significant risk to patients and nurses who are exposed daily to this continuous noise.
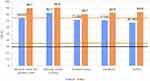 |
Figure 1 Average level of noise produced from apparatus in ICU. Note: The middle line in Figure 1 represents 40 dB which is the WHO-recommended noise level during the day, while the lowest line represents 35 dB, the WHO recommendation during the night. The highest line in the figure sits at 85 dB, which represents noise levels that have proven to be harmful to human hearing as per the American Conference of Governmental Industrial Hygienists. It is very clear that the noise produced by this equipment greatly surpasses the acceptable noise levels in the ICU. |
Table 3 shows the average personal-dosimeter noise levels during morning and night (12 hours each) shift in the FCW and CSICU. The data revealed that nurses in the CSICU were significantly exposed to ambient-noise sources higher than the FCW, with maximum noise levels in the CSICU of 74.3 dB(A) and 73.05 dB(A), respectively, while the maximum ambient noise exposure in the FCW was 74.2 and 68.9 during the morning and night shifts, respectively. There was a statistically significant difference between noise levels on the CSICU and FCW (p<0.0001) showing that the CSICU nurses are exposed to much higher noise levels during both shifts.
 |
Table 3 Independent-comparison t-tests between FCW and CSICU morning and night shifts |
Pearson correlation tests were conducted for audiometry results of decibel loss vs years of experience, as shown in Table 4.
 |
Table 4 Pearson correlations between audiometry dB(A) loss and years of experience |
There was a medium correlation (r=0.415) between ICU working years of experience and the dB loss of individuals (p=0.069). Pearson’s correlation coefficient was calculated to measure the strength of the correlation between dB loss and ICU-nurse experience. This demonstrated a near-moderate linear relationship (r=0.415). Since dB loss was correlated with ICU-nurse work duration, this could reflect a great and significant risk for nurses exposed to ambient noise that exceeds WHO standards.
Discussion
The complicated role of an ICU nurse is to ensure that ill patients receive optimal care through known duties, fulfilling ordered interventions, and acting as promoter for their patients.12 Ryherd et al's assessment of nursing total-noise dose received showed that nursing staff received a total noise dose in the range of 65–71 dBA.13 However, the WHO recommends noise levels in hospitals should be 40 dB(A) during the day and 35 dB(A) during the night shift.14 Nevertheless, most of the literature outlines that most ICUs exceed these recommended standards.15–17 Most of the ambient noise in ICUs might result from many sources, including equipment (eg, ventilators, pumps alarms, monitor alarms, and hospital staff).
In the present study, levels were very similar to Hsu et al, who found average noise levels of 77–81 dB(A) in a Taiwanese ICU.3 There was also similarity to other international findings that found ICU noise of 80–90 dB(A).18 Our data have shown that all the recorded ICU ambient noises were significantly higher than recommended levels, with means of 68.2–64.7 dB(A) and slight significant variation during morning and evening. Padmakkumar et al19 found that noise levels on one unit were 36.6 to 80 dB(A) and for another unit 40.6–86.2 dBA.19 These studies support our findings, and revealthat ambient noise in the ICU exceeds WHO guidelines.1,20 Though it has been shown that levels significantly exceeded the recommended standards, values were 40–60 dB(A) with no significant day/night-shift variation.8,21,22
There was a significant association between morning patient rounds and high ambient noise in this study. This in accordance with two similar studies in which higher activity in ICUs was associated with high ambient noise.23,24 Recent studies have identified equipment, including alarms, as the primary source of high and annoying noise levels,22,25 with the great challenge that control measures should be applied to minimize noise from monitors and ventilators. The findings of the present study are similar to those of Bayo et al,26 where recorded noise was 60–64 dB(A) during the morning and 55–59 dB(A) in the afternoon.
In ICUs, noise should be kept at lower levels as loud noise might lead to medical errors. Nevertheless, Berglund et alfound that impulse sounds like sudden alarms had a larger significant negative effect on nursing in ICUs.27 In our study, the maximum hearing loss was seen in ICU nurses with long experience of exposure to ambient noise, which is consistent with a similar study that revealed that duration of employment gives an additive effect to noise in causing noise-induced hearing loss.28 Deng, et al reported that most nurses in ICUs suggested acoustic control and minimization of alarms inside ICUs as protective tools for noise reduction.29 In the present study, many ICU nurses asked for serious improvement of the acoustic environment with sound-protective materials and space planning plus behavior modification.
Limitations
There was only one limitation to our study: it was difficult to quantify the hearing of nurses before their employement in the ICU because of an absence of hearing-examination records.
Conclusion
Nursing staff in the present study are at high risk of exposure to significant noise levels exceeding the WHO-recommended levels and might be at great risk, which can affect their hearing ability. Accurate early follow-up audiological evaluation for ICU nurses is always necessary due to the higher risk of sensorineural hearing loss. Monitors and staff activity represent the two major noise sources. Behavior modification by administrative and engineering control, as well as staff education, can be used as protective measures to reduce noise exposure effectively.
Ethical Statement
Data gathering and analysis was done following an evaluation and consent of Cardiac Surgery Intensive Care Unit directors and the approval of the Institutional Ethical and Review Board (IRB) at Saud Albabtain Cardiac Center (IRB-218-19) and with Imam Abdulrahman University IRB approval (PGS-2019-03-089). All participants signed written informed consent to confirm their willingness to participate after having the purpose of the study explained.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Berglund B
2. Goines L, Hagler L. Noise pollution: a modem plague. South Med J. 2007;100(3):287–294.
3. Hsu S-M, Ko W-J, Liao W-C, et al. Associations of exposure to noise with physiological and psychological outcomes among post-cardiac surgery patients in ICUs. Clinics (Sao Paulo). 2010;65(10):985–989. doi:10.1590/s1807-59322010001000011
4. Stansfeld SA, Matheson MP. Noise pollution: non-auditory effects on health. Br Med Bull. 2003;68:243–257.
5. Tizard CA. Health and safety in employment regulations 1995. (SR 1995/167); New Zealand: 1995;1995(May).
6. Konkani A, Oakley B, Bauld TJ, Bauid TJ. Reducing hospital noise: a review of medical device alarm management about the authors. Biomed Instrum Technol. 2012;46(6):478–487. doi:10.2345/0899-8205-46.6.478.
7. Atzema C, Schull MJ, Borgundvaag B, Slaughter GRD, Lee CKALARMED. Adverse events in Low-risk patients with chest pain Receiving continuous electrocardiographic monitoring in the emergency department. A Pilot Study. Am J Emerg Med. 2006;24(1):62–67.
8. Kaur H, Rohlik GM, Nemergut ME, Tripathi S. Comparison of staff and family perceptions of causes of noise pollution in the pediatric intensive care unit and suggested intervention strategies. Noise Health. 2016;18(81):78–84.
9. TTES Electrical Electronic Corp. Sound level Meter analyzer Type 1350 A, User manual; Taiwan.
10. Dosimeter N, Interface PC. User ’ s guide noise dosimeter with PC interface model 407355. FLIR Syst Inc. 2013;3(407355):
11. Silva MC, Luz VB, Gil D. Ruído em hospital universitário: impacto na qualidade de vida TT - noise in the hospital setting: impact on quality of life. Audiol Commun Res. 2013;18(2):109–119. doi:10.1590/S2317-64312013000200009.
12. Sole M, Klein DMM. Introduction to critical care nursing. 6thed. Saunders. 33(2013):75–77 p.
13. Ryherd EE, Waye KP, Ljungkvist L. Characterizing noise and perceived work environment in a neurological intensive care unit. J Acoust Soc Am. 2008;123(2):747–756.
14. WHO. International program on chemical safety, environmental health criteria 150: benzene. ICPS. 1993. Available from: http://www.inchem.org/documents/ehc/ehc/ehc202.htm.
15. Toohill R, Berens RJ, Cheng EY, Weigle CGM, Akhtar S. Use of active noise cancellation devices in caregivers in the intensive care unit. Crit Care Med. 2003;28(4):1157–1160.
16. Bennett M. Sleep and rest in PICU. Paediatr Care. 2013;15(1):3–6.
17. Carno M-A, Connolly HV. Sleep and sedation in the pediatric intensive care unit. Crit Care Nurs Clin North Am. 2005;17(3):239–244.
18. Sen Z, Weitao Z, Zheng G. Investigation on the acoustic environment of General Hospital of Tianjin Medical University. 42nd Int Congr Expo Noise Control Eng 2013. INTER-NOISE 2013 Noise Control Qual Life. 2013;2(92):1173–1178. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84904468193&partnerID=40&md5=3a8f0fd0328b76857217612c44cdf16e.
19. Padmakumar AD, Bhasin V, Wenham TN, Bodenham AR. Evaluation of noise levels in intensive care units in two large teaching hospitals - A prospective observational study. J Intensive Care Soc. 2013;14(3):205–210.
20. Basner M, McGuire S. WHO environmental noise guidelines for the european region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health. 2018;15:3.
21. Kramer B, Joshi P, Heard C. Noise pollution levels in the pediatric intensive care unit. J Crit Care. 2016;36:111–115.
22. Shoemark H, Harcourt E, Arnup SJ, Hunt RW. Characterising the ambient sound environment for infants in intensive care wards. J Paediatr Child Health. 2016;52(4):436–440.
23. Morrison WE, Haas EC, Shaffner DH, Garrett ES, Fackler JC. Noise, stress, and annoyance in a pediatric intensive care unit. Crit Care Med. 2003;31(1):113–119.
24. Carvalho WB, Pedreira MLG, de Aguiar MAL. Noise level in a pediatric intensive care unit. J Pediatr (Rio J). 2005;81(6):495–498.
25. Kramer B, Joshi P, Heard C. Noise pollution levels in the pediatric intensive care unit. J Crit Care. 2016;36(1557–8615):111–115. doi:10.1016/j.jcrc.2016.06.029
26. M V B, García A DAMGP, Bay MV. Archives of environmental health : an international journal noise levels in an urban hospital and workers ’ subjective responses noise levels in an urban hospital and workers ’ subjective responses. 1995; 50(3):274–51.
27. Berglund B, Gidlof-Gunnarsson A, Nilsson ME, et al. An environmental health model for children exposed to aircraft and road-traffic noise. InterNoise. 2004:1–6. Available from: Berglund et al._2004.pdf.
28. Bandyopadhyay P, Bhattacharya SK, Kashyap SK. Assessment of noise environment in a major railway station in India. Ind Health 1994;32(3):187–91.
29. Deng Z, Xie H, Kang J Evaluation of medical staff and patients on the sound environment in a Chinese hospital based on a questionnaire survey.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
