Back to Journals » Infection and Drug Resistance » Volume 16
Assessing the Knowledge, Attitudes, and Vaccination Practices Towards COVID-19 Vaccination Among Mainland Chinese Nursing Students and Interns: A Multicenter Cross-Sectional Study
Authors Qin Z, Ye X, Liu H , Tao Y, Zheng X , Zhong Y, Chen D, Ye W, Zhan C
Received 4 April 2023
Accepted for publication 12 July 2023
Published 20 July 2023 Volume 2023:16 Pages 4717—4728
DOI https://doi.org/10.2147/IDR.S415799
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Zhuzhu Qin,1,* Xinxin Ye,2,* Huanju Liu,3 Yining Tao,4 Xutong Zheng,1 Yanxia Zhong,5 Danfeng Chen,1 Wan Ye,6 Chenju Zhan7
1School of Nursing, Fujian University of Traditional Chinese Medicine, Fuzhou, Fujian, China; 2Department of Sports and Exercise Science, College of Education, Zhejiang University, Hangzhou, Zhejiang, China; 3Women’s Hospital and Institute of Genetics, Zhejiang University School of Medicine, Hangzhou, China; 4Department of Global Public Health, Karolinska Institute, Stockholm, Sweden; 5Department of Nursing, Shijiazhuang Medical College, Shijiazhuang, China; 6Department of Nursing, Xiamen Medical College, Xiamen, Fujian, China; 7Department of Nursing, Mindong Hospital Affiliated to Fujian Medical University, Ningde, China
*These authors contributed equally to this work
Correspondence: Wan Ye, Department of Nursing, Xiamen Medical College, Xiamen, Fujian, China, Tel +86 13806086169, Email [email protected] Chenju Zhan, Department of Nursing, Mindong Hospital Affiliated to Fujian Medical University, No. 89 HeShan Road, Fuan City, Fujian Province, 355000, China, Tel +86 13809562183, Email [email protected]
Objective: This study investigated factors influencing the knowledge, attitudes, practice profiles, and vaccination intentions among Chinese nursing students and nursing interns toward the coronavirus disease (COVID-19) vaccination.
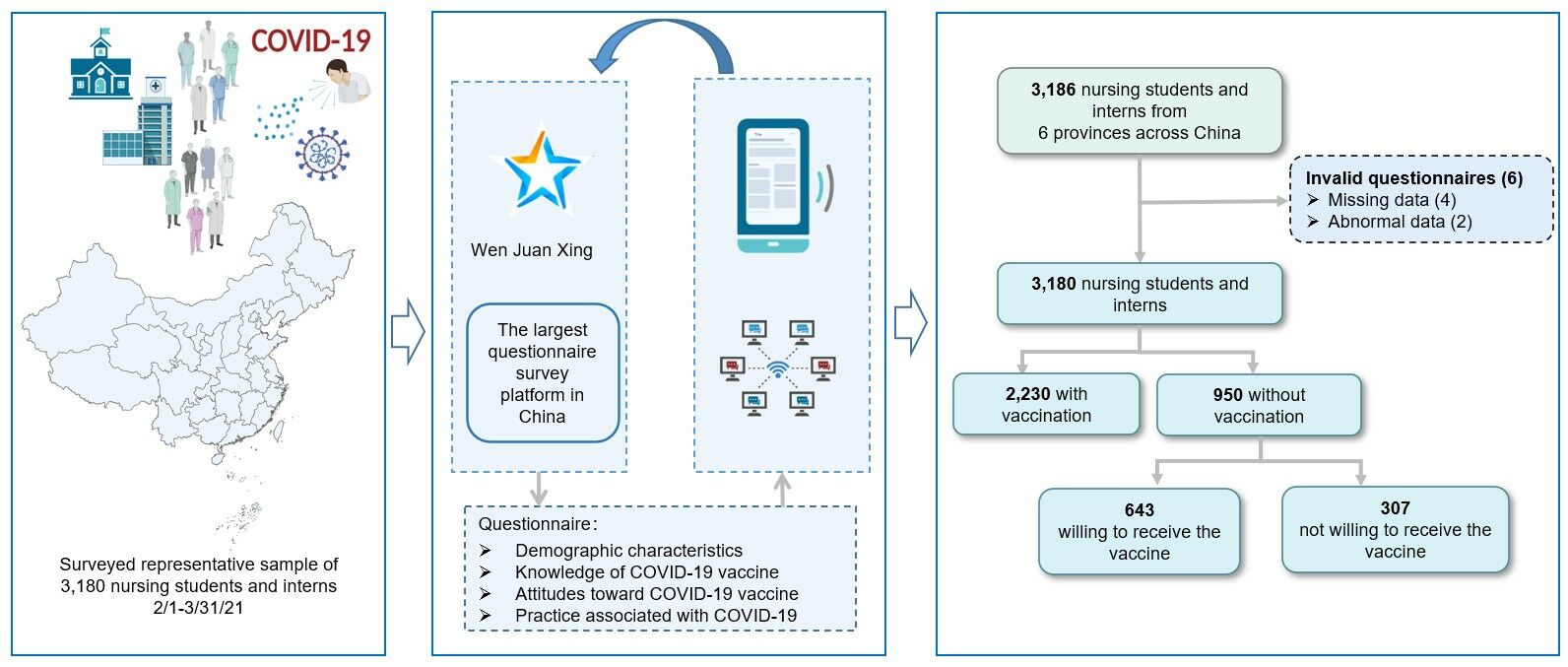
Materials and Methods: The multicenter cross-sectional study was based on a self-reported questionnaire collecting information among nursing students and nursing interns from three major geographic regions of China, and the sample was selected by consecutive sampling. The questionnaire was developed by knowledge, attitudes, and practice (KAP) theory. Univariate and multivariate logistic regression were used for statistical analysis.
Results: A total of 3180 nursing students and interns (effective rate: 99.8%) from six Chinese provinces were polled. The vaccine hesitation rate was 9.65% (307/3180), 2230 participants (70.1%) had gotten at least one dose of the vaccine, and 643 participants (67.7%) had indicated a readiness to be vaccinated. The results showed that older age, higher academic background, perfect vaccine management, others’ recommendations, influenza vaccination history, epidemic under control, knowledge of vaccines or intervals, and vaccine knowledge training were associated with higher vaccination rates. Conversely, vaccine hesitancy was caused by a perceived lack of physical need, uncertainty about vaccination requirements, and fear of vaccination.
Conclusion: This study provided population-based estimates of COVID-19 vaccine uptake intention among mainland Chinese nursing students and interns. Factors such as age, education, vaccine knowledge, and attitudes influence COVID-19 vaccine behaviour. Relevant authorities should understand the barriers to COVID-19 vaccination from knowledge, attitude and practice, which is significant for formulating effective response strategies in future global public health crises.
Keywords: COVID-19, vaccine, knowledge, attitudes, practice, nursing students and interns
Graphical Abstract:
Introduction
As of June 24, 2023, the cumulative number of confirmed COVID-19 infections worldwide surpassed 760 million and caused approximately 6.94 million deaths.1 The explosive growth in the number of cases has posed intense physical and mental pressure on medical personnel. Meanwhile, the shortage of personal protective equipment has also increased the probability of infection among medical personnel. Studies have found that the proportion of health workers infected ranged from 2–35% across countries during COVID-19 period.2 These have brought a strong shock to the healthcare system.3 Therefore, protecting healthcare providers is essential in responding to the pandemic. Studies have indicated that healthcare workers’ reluctance to accept COVID-19 vaccination increases the risk of virus transmission to patients and reduces the likelihood of patients being encouraged to vaccinate.4 In addition, direct contact between nursing interns and patients increases the chances of infection, and it is necessary to promote their active vaccination to protect themselves and others.5,6 Schools play a crucial role in epidemic prevention and control because students’ density and mobility raise the risk of infection. As a particular group among many students, nursing students receive systematic medical knowledge education in school, one of the essential links to promoting health work smoothly.7 Nursing students may be able to provide information regarding vaccinations to their families, friends, or the community in their future careers. They may also inspire other students to actively participate in the vaccination team by demonstrating a positive attitude and practice toward the vaccination.8 Therefore, assessing nursing students’ knowledge, attitude, willingness, and the factors influencing vaccination behaviour is significant and should be considered.
Previous studies have demonstrated that people’s willingness to vaccinate varies significantly among different populations, countries, and settings.9,10 Favourable factors influencing vaccination include scientific sources of information,11 previous influenza vaccination history,12 increased education,12 and fear of spreading the disease to family members.13 Concerns about the side effects of the vaccine,14 and the spread of worrying information on the Internet15 may have led to varying degrees of vaccine hesitation among the vaccinated population. According to relevant studies, the more comprehensive the knowledge of vaccines, the more positive the attitude towards vaccination, and the attitude towards vaccines also influenced the degree of vaccine acceptance.16,17 Researchers found that 43.8% of nursing students in seven European countries were willing to receive vaccination against COVID-19.18 A cross-sectional study of different majors students’ attitudes and intentions toward COVID-19 vaccination in China found that medical students (65.3%) were more aware of vaccines than non-medical students (53.6%).19
The knowledge-attitude-practice (KAP) theory is a health behavior model widely used in medicine to explain how personal knowledge and attitudes affect changes in health practice.20,21 Numerous researchers have applied this theory to explore vaccination of different populations during epidemics,22 cancer patients,23 and medical students.24 However, most studies have focused on vaccination intentions, while the impact of COVID-19 vaccine knowledge and attitudes among nursing students and nursing interns on vaccination intentions has been ignored to varying degrees. This study aimed to understand nursing students’ and nursing interns’ knowledge, attitude, and practice on the COVID-19 vaccine through a large-scale multicenter study in China and to explore the factors influencing their willingness to vaccinate.
Materials and Methods
Study Design and Participants
This study was designed as a multicenter, cross-sectional, population-based on questionnaire. Nurse students and nursing interns were conducted using a self-assessment questionnaire through the online platform Wen Juan Xing (https://www.wjx.cn) from February 1 to March 31, 2021. Potential study participants were recruited from nursing schools in three major geographical regions of China, including Fujian, Hebei, Anhui, Shanxi, Gansu and Qinghai provinces, using the convenience sampling method. First, the project leader of this study reached cooperation with the dean of the school of Nursing through communication. Then, with the help of the dean, the project leader contacted the class teachers caring for students’ daily study and life in each class. These teachers were responsible for sending the generated QR code posters or links to students through Wechat or QQ (two of the most commonly used social media platforms in China) for filling in. Participants were informed that their participation was voluntary and that their anonymous data would only be used for this study without being disclosed.
Inclusion criteria: (1) Nursing students and nursing interns; (2) Have sufficient ability to read, understand, and complete online questionnaires. All participants provided informed consent and indicated voluntary participation in the survey.
Exclusion criteria: Individuals who faced challenges utilizing mobile phones or computers.
Questionnaire
The preliminary questionnaire entries were developed through a systematic review of relevant literature, followed by a pre-survey of ten individuals selected from different schools.25–28 Based on the pilot test results, the experts of the research group discussed and refined the items of the questionnaire, and finally formed the questionnaire named “Knowledge, attitude, Practice and vaccination intention of nursing students and nursing interns on COVID-19 vaccine”, which consists of the following four parts:
- Demographic characteristics: Age, education level, ethnicity, religion, monthly household income, health status, area of residence, and current status.
- Knowledge of COVID-19 vaccine: Familiarity with COVID-19 vaccine knowledge, knowledge acquisition channels, vaccination intervals (correct option: 28 days, incorrect option: 7 or 14 days), vaccine protection time (correct option: half a year and above, incorrect option: three months and above or lifelong immunization) and whether personal protection should still be done after vaccination.
- Attitudes toward COVID-19 vaccine: This section included participants’ perceptions of the currently controlled epidemic, whether vaccination of the seasonal flu virus is necessary to protect the family during the epidemic, and reasons affecting vaccination.
- Practice associated with COVID-19: This section aimed to assess the condition and willingness of COVID-19 or seasonal influenza vaccine. We asked whether participants received regular seasonal influenza vaccination or participated in the COVID-19 vaccine training, whether they proactively consulted a doctor about COVID-19 to avoid infection or sought help from medical professionals when they had suspected symptoms, and whether they could stay healthy by getting vaccinated. We also asked participants if they had or were willing to receive the COVID-19 vaccine. We categorized participants who received or expressed willingness to receive the vaccine into the “vaccine acceptance” group, and we placed those who did not receive the vaccine or were unwilling to receive the vaccine into the “vaccine hesitancy” group.
Statistical Methods
Frequency and percentage were used to analyze demographic characteristics. Pearson chi-square test or Fisher’s exact test was used to compare the two groups. Univariate and multivariate logistic regression were used to assess the relationship between participants’ demographic characteristics, knowledge, attitudes, and practices related to COVID-19 and willingness to vaccinate in the “vaccine acceptance” and “vaccine hesitancy” groups. A multivariate logistic regression model was established to analyze the decisive factors affecting vaccination. The forward stepwise multivariate regression method was used to analyze the decisive factors affecting vaccination. P-values<0.05 was considered as statistically significant. The results of multivariate logistic regression analyses were presented in forest plots with the comparative odds ratio (OR) and 95% confidence intervals (CIs). All analyses were performed using SPSS26.0 (IBM Corporation, New York, NY, United States).
Ethical Statements
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Medical Ethics Committee of Xiamen Medical College and the audit of the Chinese Clinical Trial Registration Center (Registration number: ChiCTR2100042804). All participants gave their consent to participate in this study. This includes participants under 18 years of age, whom the Ethics Committee also approved.
Results
Participant Demographic Characteristics and COVID-19 Vaccination Status
From February 1 to March 31, 2021, 3186 nursing students and nursing interns were recruited from 6 provinces nationwide. Six participants were excluded due to either a response time of less than 30 seconds or incomplete baseline data. Thus, 3180 participants with an overall validity rate of 99.8% were included in the statistical analysis. As shown in Figure 1A, a total of 2230 (70.1%) of the 3180 participants had received at least one dose of the vaccine, while 643 (67.7%) of the 950 (29.9%) participants who had not received the vaccine said they were willing to accept it. Additionally, 307 (32.3%) were not willing to receive the COVID-19 vaccine, resulting in a vaccine hesitancy rate of 9.65% (307/3180). The results of the demographic characteristics showed statistically significant differences between the vaccine acceptance and vaccine hesitation groups (Table 1). Those in the “vaccine acceptance” group appeared to be older, more educated or had higher average monthly family income (all P < 0.05).
 |
Table 1 Comparison of Demographic Characteristics and Vaccine Acceptance |
 |
Figure 1 COVID-19 vaccination status and intention (A) and sources of vaccine information (B). |
Participant Knowledge, Attitudes, and Practice Outcomes of COVID-19 Vaccine
As shown in Figure 1B, the knowledge sources about the COVID-19 vaccine among participants were online news (89.3%), WeChat (83.2%), other (71.0%), television (69.3%), cell phone text messages (63.2%), microblogging (61.4%), government announcements (54.2%), community village vaccination pamphlet bulletin board activities (informed by others (43.0%), workplace (18.3%), and radio (10.3%). Table 2 compares the knowledge, attitudes, and practices adopted by the two groups of subjects in regard to the COVID-19 vaccine. Results showed significant differences between the two groups of participants on knowledge, attitudes, and practices (P < 0.05). In terms of knowledge, only 213 (6.7%) participants were unaware of the vaccine; 1766 (55.5%) names were aware of the vaccination interval, and more than half of participants were unaware or uncertain about the duration of protection from vaccination. 2991 (94.1%) participants were willing to wearing masks after vaccination.
 |
Table 2 Comparison of Subjects’ Knowledge, Attitudes, and Practice Regarding the COVID-19 Vaccine |
In terms of attitudes, participants who believed that the current outbreak was under control were confident in future protection. Factors that influenced participants’ willingness to receive the COVID-19 vaccine included recommendations from the national government, news media publicity, recommendation by medical experts, recommendations by people around them to reduce the spread of COVID-19, high-risk and priority groups, well-managed vaccine, adequate vaccine supply in the region, effective vaccine against variant viruses, a perceived need for vaccination, clear location of vaccination, without afraid of needle, frequent travel and need for vaccination, and sufficient time for vaccination. No contraindications appeared to be more likely to receive the vaccine or more willing to receive the COVID-19 vaccine (P < 0.05). In terms of practice, participants who regularly received the flu vaccine and had participated in vaccine knowledge training were more willing to receive the COVID-19 vaccine (all P < 0.05).
Factors Influencing Vaccination Practice and Willingness to Vaccinate
As shown in Figure 2, Participants who were relatively older (18–20 years vs <18 years, OR=0.485, 95% CI=0.298–0.789) and more educated (college vs high school or under, OR=0.141, 95% CI=0.092–0.217; bachelor or above vs high school or under, OR=0.285, 95% CI=0.105–0.771), knew a lot about COVID-19 vaccine (OR =0.236, 95% CI=0.089–0.626), clearly understood the interval between vaccinations (OR=0.524, 95% CI=0.361–0.761), the epidemic is under control (OR=0.518, 95% CI=0.292–0.917), accepted recommendations from people around them (OR=0.202, 95% CI=0.116–0.351), perfect vaccine management (agreement vs disagreement, OR=0.171, 95% CI=0.054–0.547; uncertain vs disagreement, OR=0.249, 95% CI=0.077–0.805), receiving regular seasonal influenza vaccination (OR=0.445, 95% CI=0.295–0.699) and having participated in training on COVID-19 vaccine (OR =0.586, 95% CI=0.411–0.836) were more likely to receive COVID-19 vaccine. Conversely, participants who did not think they physically needed or were unsure about the need for vaccination (agree vs disagree, OR=2.990, 95% CI=1.890–4.730; unsure vs disagree, OR =3.294, 95% CI = 2.301–4.715), and those who were afraid of the shot (OR=1.611, 95% CI=1.130–2.297) were significant factors contributing to participants’ hesitation. The multivariate logistic regression showed a good model fit superiority (χ2 = 4.606, df = 8, p = 0.799).
 |
Figure 2 Forest plots for multivariate logistic regression analysis of vaccination behavior and intention. |
Discussion
This study explored the knowledge, attitudes, and behaviors of nursing students and nursing interns towards the COVID-19 vaccine in six provinces of China and the factors influencing their decision to get vaccinated. The study included 3180 participants, of whom 70.1% were vaccinated. This result indicated that higher vaccination rates were associated with participants demographics (older age, higher literacy), knowledge (greater familiarity with vaccine knowledge, clear understanding of vaccination intervals), attitudes (accepting recommendations from peers and perfect vaccine management), and personal practices (influenza vaccination history, COVID-19 vaccine-related training).9.65% of the participants surveyed were reluctant to get vaccinated. Vaccine resistance was associated with a perception that their body did not need or was unsure if they needed the vaccine and a fear of getting the shot.
The study show that older participants (18–20 years old) had more positive vaccination profiles than younger participants (< 18 years old), possibly due to an increased ability to acquire and assimilate knowledge with age and a greater understanding of COVID-19-related conditions. However, inconsistent with previous study,29 our study did not conclude that the vaccination rate increased with age, which may be related to the small percentage of participants in the older than 20 years old group. Additionally, this study found that a lower level of education may be an influencing factor for vaccine hesitation, similar to the results of an international study.30 This can be explained by the fact that educational status can strongly predict knowledge stock.31 Before the implementation of wide-reaching vaccination campaigns, educators can use a variety of methods, including the creation of educational videos, dissemination of informative leaflets, and organization of expert lectures, to expand students’ understanding and encourage vaccine acceptance.
In terms of knowledge, our study found that compared with the vaccine hesitancy group, people in the vaccine acceptance group were more familiar with knowledge related to vaccination, such as the interval between vaccinations and the protection time after vaccination. This may be because participants who knew more about the vaccine were more aware of its importance for pandemic control and thus protect themselves and those around them through vaccination. Previous studies32 found a high association between people’s willingness to vaccinate and their knowledge of the COVID-19 vaccine. However, there were still a large number of nursing students and nursing interns who answered incorrectly about the interval between vaccinations (44.5%) and the protective time of the vaccine (51.1%), which may be the deficiencies that the government and relevant departments should pay attention to in the process of promoting vaccines in the future. 94.1% of the participants knew that they should still wear masks after vaccination, which indicates that nursing students and interns have a strong sense of self-protection and health awareness under the influence of the social environment in China.33
In addition, in our study, social media (online news, WeChat) was the primary source of COVID-19 vaccine information for participants. With the widespread use of the Internet and mobile devices, young people have easy access to various sources of information through the Internet and social media.34 On the other hand, it should be noted that online media sometimes spread alarming disinformation,35 which can negatively influence those who are already hesitant about vaccination decisions. In this regard, the government should make full use of social media to spread vaccination information, accurately monitor relevant information published on social media, crack down on platforms spreading false news, and act as “gatekeepers” for the public to receive correct information. Consistent with a study conducted in Saudi Arabia,36 our univariate analysis showed that government recommendations and medical experts were the most trusted sources of vaccination information in China. To improve vaccination rates, in the future, efforts could be directed at the younger generation to disseminate evidence-based medical knowledge and speed up vaccination.37 Medical workers can also use their professional knowledge to communicate with the public through social media platforms. By addressing concerns about vaccines, clarifying false information, and increasing public confidence in vaccination,38 they can help accelerate efforts to contain this significant global public health event.
According to the KAP theory, knowledge is the foundation for change, while attitudes are the driving force behind behavior change. Therefore, improving positive attitudes towards vaccination is critical to optimizing vaccination programs. Once a robust and positive attitude develops, it will likely translate into vaccination practice. In our study, 95.2% of nursing students and interns in the “vaccine acceptance” group expressed strong confidence in the vaccine. Previous studies39–41 have shown a large body of research exploring the differences between nurses and physicians regarding COVID-19 or seasonal influenza vaccination, with nurses showing more hesitancy than physicians. The findings of this study indicate that a majority (69.5%) of nursing students and trainees did not receive regular influenza vaccination. Nursing students and nursing interns, being potential reserves for future medical institutions, may engage in more frequent patient interaction during their clinical practice than doctors. They hold a crucial position in shaping patients’ attitudes towards vaccination. Therefore, it is critical for them to provide better information about the risk of infection and the availability of documentation on the safety and effectiveness of newly developed vaccines.
Moreover, the results show that the two themes promoting vaccination behaviour/intention are: recommended by around people and improved vaccine management, consistent with the current reported findings.42,43 People are more or less influenced by their surroundings, and if their family members or friends want them vaccinated, their willingness to be vaccinated becomes much higher. Although high-risk groups, such as medical workers, may be prioritized for vaccination,44 the growing availability of various vaccines and the promotion of herd immunity initiatives have made vaccination a common need for people worldwide. The distribution, storage, transportation of vaccines, and the monitoring of adverse reactions after vaccination are crucial to ensure the smooth implementation of mass vaccination.45 Additionally, vaccine hesitation was higher among participants who did not think they physically needed the vaccine and those who were afraid of the shot. To increase vaccination rates, health promotion lectures focusing on the risks to oneself and the surrounding population when infected with the virus and the benefits of vaccination can be conducted.
Regarding the relevant behaviors, participants who had attended the training on the COVID-19 vaccine showed more active vaccination behaviors. After systematic training by relevant institutions and departments, those with a deeper understanding of vaccination can be more motivated to join the vaccination team.5 A research demonstrated that a history of influenza vaccination has a favorable effect on COVID-19 vaccination intentions.12 Our study also found that past behavior may be one of the important factors influencing vaccination behavior. Following the publication of the COVID-19 vaccination policy, participants who received a regular dose of seasonal influenza vaccination reported more positive behaviors. Recent data indicates that China’s influenza vaccination rate for the 2021–2022 season stands at a mere 2.47%,46 significantly lower than other countries worldwide, such as England (48.0%).47 Vaccination can be viewed as an expression of personal habit,48 as it involves proactively protecting oneself from infectious diseases. Public health organizations should promote influenza vaccination as part of preventive health practices. This may reduce resistance to future group vaccination programs.
This study has some limitations that should be further considered. First, our study participants consisted of nursing students, and nursing interns cannot be generalized to all healthcare workers. Additionally, this cross-sectional design means causality could not be inferred from the results. Although participants reported acquiring more knowledge about the vaccine during the pandemic, we could not compare changes in their KAP over time. Therefore, further longitudinal studies are warranted. Despite these limitations, the present study based on substantial data and a considerable sample size pertaining to vaccination acceptance among nursing students and interns concerning their knowledge, attitudes, and practices (KAP). These findings may contribute valuable insights to assist educational institutions and relevant authorities in developing rapid and practical strategies to increase student vaccination rates in the event of similar future public health crises.
Conclusion
Our study revealed that students’ overall acceptance of the COVID-19 vaccine was high, but there is still room for improvement. We found that personal characteristics, attitudes, practices, and knowledge of vaccines influenced the acceptance of vaccines. In order to promote vaccination, relevant education departments should actively use multiple channels to disseminate knowledge about COVID-19 vaccine, increase the confidence of nursing students and nursing interns in vaccination, and improve vaccination coverage.
Data Sharing Statement
If necessary, data can be obtained from e-mail: [email protected]
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. WHO Coronavirus (COVID-19) dashboard. Available from: https://covid19.who.int.
2. World Health Organization. Prevention, identification and management of health worker infection in the context of COVID-19. Available from: https://www.who.int/publications-detail-redirect/10665-336265.
3. Sun S, Xie Z, Yu K, Jiang B, Zheng S, Pan X. COVID-19 and healthcare system in China: challenges and progression for a sustainable future. Global Health. 2021;17:14. doi:10.1186/s12992-021-00665-9
4. Biswas N, Mustapha T, Khubchandani J, Price JH. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021;46(6):1244–1251. doi:10.1007/s10900-021-00984-3
5. AL-Rawajfah OM, Al-Mugeed KA, Alaloul F, Al-Rajaibi HM, Al Omari O. COVID-19 knowledge, attitude, and precautionary practices among health professional students in Oman. Nurse Educ Pract. 2021;52:103041. doi:10.1016/j.nepr.2021.103041
6. Al‐Mugheed K, Al Rawajfah O, Bani‐Issa W, Rababa M. Acceptance, attitudes, and barriers of vaccine booster dose among nursing students: a multicounty survey. J Nurs Manag. 2022;30(7):3360–3367. doi:10.1111/jonm.13791
7. Manning ML, Gerolamo AM, Marino MA, Hanson-Zalot ME, Pogorzelska-Maziarz M. COVID-19 vaccination readiness among nurse faculty and student nurses. Nurs Outlook. 2021;69(4):565–573. doi:10.1016/j.outlook.2021.01.019
8. Jiang N, Wei B, Lin H, Wang Y, Chai S, Liu W. Nursing students’ attitudes, knowledge and willingness of to receive the coronavirus disease vaccine: a cross-sectional study. Nurse Educ Pract. 2021;55:103148. doi:10.1016/j.nepr.2021.103148
9. Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi:10.1038/s41591-020-1124-9
10. Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39(15):2024–2034. doi:10.1016/j.vaccine.2021.02.005
11. Mo PK, Luo S, Wang S, et al. Intention to receive the COVID-19 vaccination in China: application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines. 2021;9(2):129. doi:10.3390/vaccines9020129
12. Wang K, Wong ELY, Ho KF, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38(45):7049–7056. doi:10.1016/j.vaccine.2020.09.021
13. Szmyd B, Bartoszek A, Karuga FF, Staniecka K, Błaszczyk M, Radek M. Medical students and SARS-CoV-2 vaccination: attitude and behaviors. Vaccines. 2021;9(2):128. doi:10.3390/vaccines9020128
14. Kreps S, Dasgupta N, Brownstein JS, Hswen Y, Kriner DL. Public attitudes toward COVID-19 vaccination: the role of vaccine attributes, incentives, and misinformation. NPJ Vaccines. 2021;6(1):73. doi:10.1038/s41541-021-00335-2
15. Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccines. 2022;10(1):110. doi:10.3390/vaccines10010110
16. Brown DL, Cowdery JE. College students’ knowledge and attitudes toward clinical trials and their relationship with willingness to participate in COVID-19 trials or vaccines. J Am Coll Health. 2021;1–3. doi:10.1080/07448481.2021.1947840
17. Qiao S, Tam CC, Risk Exposures LX. Risk perceptions, negative attitudes toward general vaccination, and COVID-19 vaccine acceptance among college students in south Carolina. Am J Health Promot. 2022;36(1):175–179. doi:10.1177/08901171211028407
18. Patelarou E, Galanis P, Mechili EA, et al. Factors influencing nursing students’ intention to accept COVID-19 vaccination: a pooled analysis of seven European countries. Nurse Educ Today. 2021;104:105010. doi:10.1016/j.nedt.2021.105010
19. Gao L, Su S, Du N, et al. Medical and non-medical students’ knowledge, attitude and willingness towards the COVID-19 vaccine in China: a cross-sectional online survey. Hum Vaccin Immunother. 2022;18(5):2073757. doi:10.1080/21645515.2022.2073757
20. Li L, Zhang J, Qiao Q, Wu L, Chen L. Development, reliability, and validity of the “knowledge-attitude-practice” questionnaire of foreigners on traditional Chinese medicine treatment. Evid Based Complement Alternat Med. 2020;2020:8527320. doi:10.1155/2020/8527320
21. Oshima T, Siah KTH, Kim YS, et al. Knowledge, attitude, and practice survey of gastroparesis in Asia by Asian neurogastroenterology and motility association. J Neurogastroenterol Motil. 2021;27(1):46–54. doi:10.5056/jnm20117
22. Elhadi M, Alsoufi A, Alhadi A, et al. Knowledge, attitude, and acceptance of healthcare workers and the public regarding the COVID-19 vaccine: a cross-sectional study. BMC Public Health. 2021;21:955. doi:10.1186/s12889-021-10987-3
23. Hong J, Xu XW, Yang J, et al. Knowledge about, attitude and acceptance towards, and predictors of intention to receive the COVID-19 vaccine among cancer patients in Eastern China: a cross-sectional survey. J Integr Med. 2022;20(1):34–44. doi:10.1016/j.joim.2021.10.004
24. Orok E, Ndem E, Daniel E. Knowledge, attitude and perception of medical students on COVID-19 vaccines: a study carried out in a Nigerian University. Front Public Health. 2022;10:942283. doi:10.3389/fpubh.2022.942283
25. Rahman MM, Chisty MA, Alam MA, et al. Knowledge, attitude, and hesitancy towards COVID-19 vaccine among university students of Bangladesh. PLoS One. 2022;17(6):e0270684. doi:10.1371/journal.pone.0270684
26. Saiful Islam M, Bakkar Siddique A, Akter R, et al. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: a cross-sectional community survey in Bangladesh. BMC Public Health. 2021;21(1):1851. doi:10.1186/s12889-021-11880-9
27. Shirui L, Gao Z, Zhong M, Zhujun Y, Jianan L, Haoran B. Chinese University students’ awareness and acceptance of the COVID-19 vaccine: a cross-sectional study. Risk Manag Healthc Policy. 2022;15:845–864. doi:10.2147/RMHP.S360274
28. Li XH, Chen L, Pan QN, et al. Vaccination status, acceptance, and knowledge toward a COVID-19 vaccine among healthcare workers: a cross-sectional survey in China. Hum Vaccin Immunother. 2021;17(11):4065–4073. doi:10.1080/21645515.2021.1957415
29. Jiang N, Gu P, Liu K, Song N, Jiang X. Acceptance of COVID-19 vaccines among college students: a study of the attitudes, knowledge, and willingness of students to vaccinate. Hum Vaccin Immunother. 2021;17(12):4914–4924. doi:10.1080/21645515.2021.2013077
30. Bono SA, E FDMV, Siau CS, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low- and middle-income countries. Vaccines. 2021;9(5):515. doi:10.3390/vaccines9050515
31. Singh DR, Sunuwar DR, Karki K, Ghimire S, Shrestha N. Knowledge and perception towards universal safety precautions during early phase of the COVID-19 outbreak in Nepal. J Community Health. 2020;45(6):1116–1122. doi:10.1007/s10900-020-00839-3
32. Maraqa B, Nazzal Z, Rabi R, Sarhan N, Al-Shakhra K, Al-Kaila M. COVID-19 vaccine hesitancy among health care workers in Palestine: a call for action. Prev Med. 2021;149:106618. doi:10.1016/j.ypmed.2021.106618
33. Bai Z, Ma Z, Jing L, et al. Estimation and sensitivity analysis of a COVID-19 model considering the use of face mask and vaccination. Sci Rep. 2023;13(1):6434. doi:10.1038/s41598-023-33499-z
34. Jain J, Saurabh S, Kumar P, et al. COVID-19 vaccine hesitancy among medical students in India. Epidemiol Infect. 2021;149:e132. doi:10.1017/S0950268821001205
35. Huang Y, Su X, Xiao W, et al. COVID-19 vaccine hesitancy among different population groups in China: a national multicenter online survey. BMC Infect Dis. 2022;22(1):153. doi:10.1186/s12879-022-07111-0
36. Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657–1663. doi:10.2147/JMDH.S276771
37. Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16(11):2586–2593. doi:10.1080/21645515.2020.1780846
38. Jones AM, Omer SB, Bednarczyk RA, Halsey NA, Moulton LH, Salmon DA. Parents’ source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Adv Prev Med. 2012;2012:932741. doi:10.1155/2012/932741
39. Fakonti G, Kyprianidou M, Toumbis G, Giannakou K. Attitudes and acceptance of COVID-19 vaccination among nurses and midwives in Cyprus: a cross-sectional survey. Front Public Health. 2021;9:656138. doi:10.3389/fpubh.2021.656138
40. Gagneux-Brunon A, Detoc M, Bruel S, et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021;108:168–173. doi:10.1016/j.jhin.2020.11.020
41. Oruç MA, Öztürk O. Attitudes of health care professionals towards COVID-19 vaccine - a sequence from Turkey. Hum Vaccin Immunother. 2021;17(10):3377–3383. doi:10.1080/21645515.2021.1928462
42. Ng N, Vaithilingam S, Nair M, Hwang LA, Musa KI. Key predictors of COVID-19 vaccine hesitancy in Malaysia: an integrated framework. PLoS One. 2022;17(5):e0268926. doi:10.1371/journal.pone.0268926
43. Papini F, Grassi N, Guglielmi G, et al. Covid-19 vaccine management (Comirnaty and mRNA-1273 moderna) in a teaching hospital in Italy: a short report on the vaccination campaign. Environ Health Prev Med. 2021;26:99. doi:10.1186/s12199-021-01018-z
44. Yamey G, Schäferhoff M, Hatchett R, Pate M, Zhao F, McDade KK. Ensuring global access to COVID-19 vaccines. Lancet. 2020;395(10234):1405–1406. doi:10.1016/S0140-6736(20)30763-7
45. Weintraub RL, Subramanian L, Karlage A, Ahmad I, Rosenberg J. COVID-19 vaccine to vaccination: why leaders must invest in delivery strategies now. Health Aff. 2021;40(1):33–41. doi:10.1377/hlthaff.2020.01523
46. Zhao HT, Peng ZB, Ni ZL, et al. Investigation on influenza vaccination policy and vaccination situation during the influenza seasons of 2020–2021 and 2021–2022 in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2022;56(11):1560–1564. doi:10.3760/cma.j.cn112150-20220810-00802
47. Oakley S, Bouchet J, Costello P, Parker J. Influenza vaccine uptake among at-risk adults (aged 16–64 years) in the UK: a retrospective database analysis. BMC Public Health. 2021;21(1):1734. doi:10.1186/s12889-021-11736-2
48. Lin CJ, Nowalk MP, Toback SL, et al. Importance of vaccination habit and vaccine choice on influenza vaccination among healthy working adults. Vaccine. 2010;28(48):7706–7712. doi:10.1016/j.vaccine.2010.07.009
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
