Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Assessing the Effectiveness of an E-Coaching Intervention in Improving Family Support for Individuals with Mental Disorders: A Quasi-Experimental Approach
Authors Arifin M , Sekarwana N, Mediawati AS, Susilaningsih FS
Received 6 May 2023
Accepted for publication 26 July 2023
Published 17 August 2023 Volume 2023:16 Pages 2405—2415
DOI https://doi.org/10.2147/JMDH.S417685
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mokhamad Arifin,1,2 Nanan Sekarwana3 ,† Ati Surya Mediawati,4 Francisca Sri Susilaningsih4
1Doctoral Study Program, Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, 45363, Indonesia; 2Nursing Study Program, Faculty of Health Science, Universitas Muhammadiyah Pekajangan Pekalongan, Pekalongan, Central Java, Indonesia; 3Faculty of Medicine, Universitas Islam Bandung, Bandung, West Java, Indonesia; 4Nursing Study Program Universitas Padjadjaran, Bandung, West Java, 45363, Indonesia
†Late Nanan Sekarwana passed away before the completion of this article.
Correspondence: Mokhamad Arifin, Tel +62 816-677-711, Email [email protected]
Background: The increasing number of mental disorders (MDs) requires government, social, and family attention. The purpose of this study was to determine the effectiveness of an e-coaching empowerment application in improving families’ abilities to care for individuals with mental disorders (MDs).
Methods: A quasi-experimental design was used for this study. Totaling 122 individuals selected through purposive sampling from families with (MDs) in six selected community health centers that divided into two groups, intervention and regular mental healthcare. The data collected were analyzed using multiple linear regression. The independent variable was the provision of intervention using the e-coaching application with GROW (Goal, Reality, Option, Will) model, while the dependent variables were the family’s ability to recognize problems, make decisions, take care of people with MDs, modify the environment, and utilize health facilities. Further, multivariate tests were used to evaluate the effect of e-coaching empowerment on families’ ability to care for MDs.
Results: The results demonstrated a significant impact of e-coaching on the family’s ability to care for individuals with MDs (p< 0.01). Education also partially affected the family’s ability to care for individuals with MDs (p< 0.01). Additionally, age, gender, occupation, relationship with the individual MDs, and duration of care simultaneously did not significantly affect the family’s ability to care for individuals with MDs (p< 0.01). However, educationally background was significantly affect family ability in taking care for MD patients. Overall, e-coaching significantly improved the family’s ability to recognize problems, make decisions, care for patients with MDs, modify the environment, and utilize health facilities.
Recommendations: The e-coaching empowerment application for families can assist healthcare workers in enhancing the family’s ability to provide assistance for individuals with MDs at home. This application can improve mental health services in the broader location accessible via the internet and can be developed for other health fields. The application can be expanded into a simple game so that families can view their scores for their proficiency in each session to make it more entertaining.
Keywords: mental disorders, e-coaching, empowerment, family caregivers
Introduction
Our entirely health and well-being rest heavily on our mental health, which is also a basic human right. We may interact, function, cope, and thrive better when we are in good mental health. A complicated spectrum of mental health exists, with experiences ranging from a state of maximum well-being to crippling conditions of extreme suffering and emotional anguish. Although it is more common for those who have mental health issues to have lower levels of mental well-being, this is not always the case.1 Additionally, the prevalence of individuals suffering from MDs in Indonesia has increased significantly, rising from 1.7% in 2013 to 7% in 2018. The estimated number of people suffering from MDs in Indonesia is around 450 thousand.2 The government has provided specific laws to support people with MDs. The law states that mental health efforts in Indonesia are activities to create an optimal degree of mental health for every individual, family, and community. The activities include promotive, preventive, curative, and rehabilitative approaches that are carried out in a comprehensive, integrated, and sustainable manner by the government, local government, or the community.
Individuals with MD require specialized treatment to achieve a level of recovery. The recovery of mental disorder patients is influenced by medication adherence and is directly related to the support or assistance provided by their families. Family support and assistance make patients feel loved and valued.3 Also, it aids patients in preventing noncompliance and relapse in MD patients.4 Forms of family support and assistance for mental disorder patients include accompanying patients to medical appointments, handling administrative matters, providing information, and showing care.5 Furthermore, integrating a family approach to mental healthcare includes a multidisciplinary approach to treating the family as a whole since a family of mental illness patients who become caregivers for patients tends to have higher anxiety. A family-centered intervention program’s practicability, efficiency, and applicability may help reduce caregivers’ anxiety, depression, and stress. With a focus on caregiver empowerment, they could better handle their worries in the caregiving situation and develop more psychological power in the caring process. However, families with MD patients, especially those living in Indonesia, have some hindering factors in running their role to become a patient’s caregiver. In addition, earlier research found that caregivers face challenges due to a lack of understanding and limited access to information.6
According to experts, an integrated family approach to mental health care improves families by considering the many responsibilities, positions, and connections, implementing an adjustable complementary therapy program, and empowering professionals through multidisciplinary consultations.7 According to a study, persons who reported having more social support felt less of a desire for mental health services, implying that supportive connections can replace or even postpone seeking professional therapy. There may not be as much unmet need for psychiatric services as low service utilization rates among people with illnesses suggest.8
Evidence-based health and mental health promotion initiatives may be extended to include people in these non-clinical mental health settings by utilizing online and mobile technology. Data from Indonesia’s National Survey of Social and Economics show that the percentage of people who own a mobile phone increased from 59.59% in 2017 to 65.87% in 2021. As mobile phone ownership rises, so does the population’s use of mobile phones, rising from 68.59% in 2017 to 81.28% in 2021,9 support peer support training as an efficient way to increase compliance and results of online self-help programs, particularly when provided over the phone.10 Peers may be crucial in successfully assisting one another in using online resources for mental health and health information and gaining access to evidence-based technology interventions that support wellness and health goals.11 Digital mental health interventions (DMHI) can increase effectiveness, scope, and uniformity while lowering the price of mental health services. According to preliminary research, these technologies will increase the accessibility and effectiveness of evidence-based approaches.12
Several programs are available in Indonesia. Prevention efforts are carried out using various strategies, including empowering people with MDs and psychosocial disabilities. A brand-new approach for delivering evidence-based preventative interventions is called “family coaching”. Family coaching may be effective because of three recent developments in health promotion.13 Personalized feedback about intervention content or users’ mental health status is one engagement strategy made possible by e-coaching. Other engagement strategies include guidance about content and progress through e-coaching, social forums and peer interaction, content gamification, reminders, flexibility, and ease of use. Engagement with digital interventions for mental health promotion is encouraged by individualized intervention assistance, access to social support, and personalized feedback.14 However, shifting mental health care from professionals to digital apps could increase social isolation for those requiring human interaction. This essay makes the case that people are our society’s most magnificent resource and are just as pervasive as technology.15 This study aims to evaluate the impact of e-coaching on families’ ability to manage mental disorders patients at home.
Methods
Study Design
Researchers used a Quasi-Experimental Design to determine the extent of the influence of e-coaching on the ability of families to care for MDs. The study population consisted of families with members with MDs in a district with a total of 1647. The sample size calculation was performed using G-power, taking into account an effect size of 0.14, an alpha level of 0.05, a power of 0.90, two groups, and three repetitions. The calculation determined that a minimum of 110 respondents was needed. To account for potential dropouts, a reserve of 10% was added, resulting in a final rounded sample size of 122 respondents. The sample was taken from 6 health centers in Pekalongan District selected by the researchers. Documented review and approval from a formally constituted review board (Institutional Review Board or Ethics committee) is provided for this study, in accordance with the Declaration of Helsinki. We also provide informed consent for all participants. Furthermore, this study obtained ethical approval from the Ethics Committee of Padjadjaran University, Bandung, with the approval number 544/UN6.KEP/EC/2021.
Participants
The sampling was conducted using purposive sampling, and the inclusion criteria for respondents in this quantitative research are: 1) Families with members who have MDs, 2) willing to participate as respondents, 3) willing to complete the research process, 4) owning a smartphone, and 5) aged over 18 years. Meanwhile, the exclusion criteria are 1) families who have cared for people with MDs for less than three months and 2) not present during the research period.
There were 122 participants, split into two groups consisting of 61 respondents in the intervention group and 61 in the control group. While the control group received regular mental health care, the intervention group underwent therapy using an e-coaching program. In addition, to prevent contamination between the intervention and control groups, participants were physically or temporally separated to reduce the likelihood of interactions or information sharing between participants from different health centers, as well as clear instructions and monitoring to ensure participants followed the prescribed procedures.
E-Coaching Assessment
The independent variable is the provision of intervention using the e-coaching application with GROW (Goal, Reality, Option, Will) model. The specialty of this GROW Model does not require psychological training and psychotherapeutic background, the coaches can come from the functional field, and personal development can be done through cooperation with others; this GROW model corresponds to organizational cooperation, simple and used by many parties.16 The dependent variables are the family’s ability to recognize problems, make decisions, take care of people with MDs, modify the environment, and utilize health facilities. The E-coaching application, SIPANDAWA, can be accessed at https://sipandawa.com (Figure 1).
 |
Figure 1 Application e-coaching SIPANDAWA preview. |
Evaluating the effectiveness of e-coaching by using a 20-question questionnaire which has been validated on the family’s capacity for caring for MDs, which includes six questions on the family’s capacity for problem-solving, two questions on the family’s capacity for decision-making, six questions on the family’s capacity for caring for patients with MDs, three questions on the family’s capacity for environment modification, and three questions on the family’s capacity for using medical facilities (Supplementary 1). Additionally, each question has been assessed and validated by three experts with PhD qualification (Supplementary 2). Age, gender, education, occupation, relationship with the person with MD, and the duration served to care for the person with MD are confounding factors in this study.
Furthermore, to validate the questionnaire, we followed a rigorous process. Firstly, we conducted a pilot study with a small group of participants to assess the clarity and comprehensibility of the questionnaire items. Based on their feedback, we made necessary revisions to improve the questionnaire’s clarity. Subsequently, we approached three experts in the relevant field and shared the revised questionnaire with them. These experts have extensive experience and knowledge in our research area. We asked for their evaluation of the questionnaire’s quality, focusing on its relevance, appropriateness, and comprehensiveness. In addition, we conducted a final review of the questionnaire to ensure its consistency and coherence. We double-checked for any ambiguous or overlapping items, and made necessary adjustments for a more robust instrument.
Statistical Analysis
The authors performed analysis of covariance (ANCOVA) by using SPSS 28 (Statistical Package for the Social Sciences) to investigate the impact of e-coaching on families’ capacity to care for MDs.
Results
In order to assess the effectiveness of e-coaching, we employed the GROW approach, which involved measuring various factors including the family’s capacity to identify issues, make decisions, provide care for individuals with mental disorders (MDs), adapt the environment, and utilize healthcare resources.
Characteristics of Respondents
Table 1 demonstrates the characteristics of respondents in the intervention and control groups.
 |
Table 1 Participant Characteristics |
Table 1. Illustrates that the intervention group predominantly comprises females at 70.5%, while in the control group, it is 63.9%. Regarding the educational level, most participants in the intervention group have completed junior high school, accounting for 47.6%, whereas, in the control group, it is 65.6%. Concerning occupation, most participants in the intervention group work in the domestic sector, accounting for 62.3%, while in the public sector, it is 37.5%. Regarding the relationship with the person affected by mental illness, the majority of participants in the intervention group are siblings at 62.2%, while in the control group, it is parents at 31.1%.
An E-Coaching Application Intervention’s Effects
Family abilities were evaluated three times in this study: once before the intervention (pre-tests), two weeks after the intervention (post-test 1), and again two weeks later (post-test 2). The results of measuring the average ability of families to care for MDs are shown in Table 2.
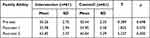 |
Table 2 Family Ability Evaluation |
Table 2 demonstrates the average family ability during pre-tests of 50.26 in the intervention group and 50.44 in the control group. Analysis of the average difference in family ability between groups during pre-tests showed no difference with a value of ρ=0.698. At post-test 1, the average family ability was 54.90 in the control group and 55.98 in the intervention group. At a p-value of =0.070, analysis of the average gap in family capacities across groups at post-test 1 revealed no difference. In post-test 2, the average family ability in the intervention group was 63.85, while it was 60.84 in the control group. Analysis of the average difference in family abilities between groups at post-test 2 showed a difference with the ρ<0.05, indicating that e-coaching influences the family’s ability to take care of MDs. The relationship of e-coaching and variables to family abilities The effect of e-coaching on the family’s ability to care for MDs also needs to consider the existence of a role variable.
A Confounding Variable’s Significance
The variables estimated as confounding in this study are age, gender, occupation, education, relationship with MDs, and length of care. The effects of confounding can be seen in Table 3.
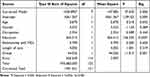 |
Table 3 Confounding Impact Analysis Using ANCOVA |
The outcomes of the ANCOVA conducted on the data are displayed in Table 3. For each variable in the model, the table indicates the type III sum of squares, degrees of freedom, mean square, F-statistic, and significance level. The corrected model, which includes all the predictor variables, was found to be statistically significant (F(7, 114) =37,.025, p < 0.001), indicating that the model as a whole was a good fit for the data. The adjusted R-squared value of 0.676 suggests that the model explains a substantial amount of the variance in the outcome variable.
The intercept term was highly significant (F(1, 114) = 1.091E3, p < 0.001), indicating that the outcome variable had a significant baseline value. Only education, group, and the corrected model were substantial predictors of the outcome variable among the predictor variables. The variables of age, gender, occupation, relationship with MDs, and length of care were not significant predictors of the outcome variable. Overall, the multivariate test results suggest that the e-coaching empowerment application significantly affected families’ ability to care for individuals with mental disorders, even after controlling for other variables.
E-Coaching Results Overview
The family’s ability in the care of MDs is assessed based on 5 family tasks in the treatment of MDs consisting of task 1: recognize the problem; task: 2 make decisions; task: 3 taking care of MDs patient; task 4: modify the environment and tasks: 5 utilize health facilities. The Figure 2 demonstrated an overview of changes in family abilities in the treatment of MDs in the intervention group that occurred before e-coaching and after e-coaching.
 |
Figure 2 Family ability in taking care of MDs. |
Overall, there was an improvement in the ability to care for individuals with MDs with regards to the variables of Recognizing the Problem, Making a Decision, Taking Care the Patient, Modifying the Environment, and Utilizing Health Facilities. It is clear that e-coaching significantly improved several of these variables.
Discussion
Patients with pulmonary tuberculosis can increase their self-efficacy and preventative behaviors, such as knowledge, attitude, and behavior, by receiving health coaching based on the health promotion framework. Although the research is conducted in different areas, the critical essence is using the same method, which is coaching.17 Studies show that personalized support during the intervention, access to social support, and personalized feedback seem to encourage engagement with digital interventions for mental health promotion, so there is still room for improvement in the development of coaching for mental health through digital media. These findings should be interpreted cautiously because the included studies are diverse, often have small sample sizes, and generally do not highlight engagement as the primary outcome. Although user participation is essential for the success of digital treatments, little attention has been paid to this topic. The effectiveness of different user engagement facilitation tactics for digital interventions for mental health promotion requires further study.18 The effects of coaching practices on well-being might last up to six months following involvement. Coaching must be institutionalized to enhance the well-being of digital technology users who experience health issues.19
This study used the Coaching GROW method in four stages on 5 cases of managing Aggression/Violent Behavior, Hallucinations, Withdrawal, Low Self-Esteem, and Deficit/Self-Care. When effectively used in the mentoring process, the coaching model positively impacts the organization and individuals within it, ultimately resulting in better patient care.20 According to this study, combining coaching GROW with Zoom media can enhance school administrators’ well-being. The study’s findings also demonstrate the GROW technique as an effective treatment for subjective well-being in various mental health issues.21
Education level and involvement in employment and education are positively correlated. This study contends that these aspects of socioeconomic inequality grow as people age and emphasizes the significance of involving workers with less education in initiatives to promote lifelong learning.22 Considering inter-individual variables, such as education level, when examining the impact of proactive personality and locus of control on job satisfaction is crucial because education can have beneficial and detrimental effects on reducing stress.23 Students in senior high school have higher health literacy levels than those in junior high school, and those who have completed health-related courses have even higher health literacy levels. Preventing and treating infectious diseases is the most sought-after health information, and students are increasingly using new media to learn about health.24 In all provinces, patient education materials are still written beyond the recommended Grade Reading Level (GRL), and provincial institutions vary greatly regarding patient education capacity, quality, and comprehension. It offers a chance to improve the materials’ effectiveness, assuring a more thorough audience knowledge and raising patients’ health literacy.25 Anyone who wants to learn more can do so, even classroom teachers. By actively participating in initiatives to raise students’ mental health literacy, they can significantly raise their awareness of and attitudes toward psychological issues, making up for the absence of full-time mental health teachers in schools. Future efforts should focus on improving students’ mental health literacy and developing evidence-based intervention research. In addition, we can raise kids’ mental health knowledge by addressing delays and preventing bad mental health.26
Social inequality in 2018 has been growing over time and is influenced by factors other than gender, including education level, age, job, salary, and place of birth.27 The degree to which certain job pathways are believed to require verbal or numerical skills is correlated with the distribution of gender in education and employment. The large discrepancies in professional results between men and women can only be attributed to gender differences in academic achievement, even though gender is only moderately related to people choosing decisions that are in line with their academic abilities.28
Even in brain deterioration, older people can preserve cognitive function by working in jobs that stimulate cognitive performance and include, more important social engagement.29 Contrarily, there is no correlation between medication compliance and the following factors: BMI, occupation, comorbidities, disease duration, age, gender, marital status, or degree of education.
Family interactions are essential in determining the psychological status of adolescents. However, the impact of father-child connections differs depending on the father’s living situation. The results also emphasize the importance of considering context when analyzing how family interactions affect adolescents’ well-being.30 Qualitative methods are the most effective way to study family dynamics and relationships. There are four benefits: (1) learning what family members mean when they talk about family interactions and relationships; (2) learning what they think about how the family interacts and interacts with one another; (3) examining families within their contexts; and (4) giving voice to excluded family members and family members.31
In addition, economic concerns are crucial inside families. Higher socioeconomic level individuals have greater psychosocial coping mechanisms to handle psychosocial challenges. Besides those with the highest incomes, jobs may be a psychological burden and a source of stress for all workers, suggesting that a person’s stress levels may be lowered by having a higher income.32 Although it is negligible, there is a connection between emotional-focused family burden and ineffective family coping mechanisms. Therefore, social support and practical coping skills instruction for those who care for people with chronic schizophrenia and bipolar disorder can lessen their perception of the care’s burden.33 Programs for psychoeducation may lessen the strain of communication and enhance carers’ mental health, according to an earlier study. These initiatives can enhance the quality of life for aphasic people and their families who reside in rural locations and deal with severe social stigma and heavy caregiving responsibilities.34
Timely access to inpatient care is required to shorten the length of stay for individuals with mental health conditions. This can be accomplished, in part, by making inpatient psychiatric care insurance more widely available and removing pointless mental health requirements for placement authorization.35 MDs who live in rural areas, take drugs, and have emotional issues are more likely to have prolonged hospital stays. The chance of a mental disorder linked to childhood trauma relapsing is increased by working and having experienced parental childhood trauma. Treatment emphasizing early trauma lowers the chance of relapse and reduces hospital stays.36
Based on multiple regression analysis, the R Square value is 0.692 or equivalent to 69.2%. This number indicates that the variables of the group, age, gender, occupation, education, relationship with people with MDs, and length of care together influence the family’s ability to care for people with MDs by 69.2%. Meanwhile, the remaining (100–69.2% = 30.8%) is influenced by other variables outside this regression equation or that have not been studied.
Some other potential confounding variables that have not been studied include support systems, economic status, marital status, and insurance ownership.37 Family support has more sway in nations with more power disparity or less individualism (where social norms and culture may be less advantageous). It implies that family support is a replacement mechanism in these nations that encourages entrepreneurial behavior.38 In rural areas, low family income predicts poor long-term results for people with schizophrenia. When developing mental health policies and offering community-based mental health services, the financial situation of the person’s family should be considered.39 Low-income individuals have a disproportionately high likelihood of being male, single, unable to support themselves outside of the home, lacking family carers, having fewer family members, and being mentally ill. Poor workability, earlier onset age, never-treated status, and low-income family economic status are significant risk variables linked to patients’ poor mental health. Early detection, care, and patient recovery should be enhanced through culturally appropriate community-based interventions and focused programs to reduce poverty.40
Female participants report more depressive symptoms and unmarried households are more likely to have careers for their parents. Both marital status and caregiving status are proportional predictors of depression; however, the effect of caregiving status on depression is not supported by marital status. Significant differences in depression symptoms, proportional to marital status and gender, are caused by caregiving status.41 The working-age population’s suicide rate is influenced both separately and together by marital status, educational level, and employment situation. Particularly among young adults, divorce, unemployment, and economic inactivity for adults, all increase the risk of suicide. Suicide prevention for young adults should consider monitoring and intervention.42
Aspects of finances and insurance are another confusing factor associated with family capacity. Even after correcting for these variables initially and other confounders, financial stability and financial competence are positively connected to self-reported physical and mental health indicators, while financial challenges are adversely related. Based on data from health insurance claims, financial status is also linked to a lower likelihood of depression. Anxiety is also linked to financial stability. To improve population health, policymakers may consider implementing more potent measures to guarantee favorable financial conditions.
Additionally, policies can promote wise financial management practices and comprehension of the long-term effects of financial decisions, as these factors may be extremely important to health outcomes. Although the most conservative limits for friction and double inference corrections render it statistically insignificant, insurance may have a “peace of mind” effect. Health insurance could ease anxiety.43 The insurance coverage in Indonesia’s eastern provinces is still significantly lower than in its western provinces. Health insurance ownership, education, household economic status, and regional characteristics exhibit favorable insurance utilization correlations. After the National Health Insurance program was implemented, there was still inequity in insurance usage across socioeconomic status and geography differences. This circumstance highlights the requirement for the government and associated parties to make efforts to equalize insurance utilization, particularly for National Health Insurance in all regions of Indonesia.44
Furthermore, despite e-coaching having shown significant differences in improving family ability to care for individuals with MDs, this study has several limitations. The quasi-experimental design of this study, which lacks randomization and may result in disparities in baseline characteristics between the intervention and control groups, is one possible weakness that could restrict its ability to produce reliable results. Self-report measures used in the study have the risk of introducing subjectivity bias, erroneous answers, or memory distortion. The delivery of the intervention by an e-coach may have an impact on how the family members react and how much assistance they report giving. Controlling outside elements that can affect family support, such as climatic changes, family dynamics, or unmanaged stressors, is difficult.
Conclusion
The study on integrating the GROW approach and e-coaching application demonstrates how the e-coaching application affects the family’s capacity to care for MDs. This program can enhance mental health services in a larger area that is reachable online and can be created for other medical specialties. Furthermore, the educational background of the family significantly affected their capacity to care for MD patients.
Acknowledgments
We would like to express our gratitude to Universitas Padjadjaran and Universitas Muhammadiyah Pekajangan Pekalongan for their support in providing facilities and funding for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. World mental health report: transforming mental health for all. Geneva: World Health Organization; 2022. Available from: https://apps.who.int/iris/handle/10665/356119.
2. Kementrian Kesehatan RI [Indonesian Ministry of Health]. Infodatin Situasi Kesehatan Jiwa Di Indonesia. Indonesia: Pusat Data dan informasi Kemenkes RI [Infodata on Mental Health Situation in Indonesia. Indonesia: Data and information center of the Indonesian Ministry of Health] ; 2019 https://pusdatin.kemkes.go.id/download.php?file=download/pusdatin/infodatin/InfoDatin-Kesehatan-Jiwa.pdf.
3. Damayantie N, Rusmimpong R, Elly A. Hubungan pengetahuan dan dukungan keluarga dengan kepatuhan kontrol berobat pasien skizofrenia di poli jiwa RSJD Provinsi Jambi Tahun 2018 [The relationship of knowledge and family support with schizophrenia patient medication compliance control in RSJD Jambi province 2018]. J Bahana Kesehat Masy. 2019;2019:1. Indonesian. doi:10.35910/jbkm.v3i1.161.
4. Keliat BA, Pawirowiyono A. Keperawatan Jiwa Terapi Aktivitas Kelompok [Psychiatric Nursing Group Activity Therapy].
5. Suryenti V. Dukungan dan Beban Keluarga dengan Kemampuan Keluarga Merawat Pasien Resiko Perilaku Kekerasan di Klinik Jiwa Rumah Sakit Jiwa Provinsi Jambi Tahun 2017 [Family Support and Burden with Family Ability to Caring for Patients at Risk for Violent Behavior at Mental Clinics Mental Hospital Jambi Province in 2017]. J Psikologi Jambi. 2017;2017:2. Indonesian. doi:10.22437/jpj.v2i2.4795
6. Agustina NW, Handayani S. Kemampuan Keluarga Dalam Merawat Pasien Skizofrenia Dengan Gejala Halusinasi [Family Ability in Caring for Schizophrenic Patients with Hallucination Symptoms]. URECOL. 2017;2017:439–444. Indonesian.
7. Stolper H, van Doesum K, Steketee M. Integrated family approach in mental health care by professionals from adult and child mental health services: a qualitative study. Front Psychiatry. 2022;13:781556. doi:10.3389/fpsyt.2022.781556
8. Thoits PA. Perceived social support and the voluntary, mixed, or pressured use of mental health services. Soc Ment Health. 2011;1:4–19. doi:10.1177/2156869310392793
9. Sutarsih T, Wulandari VC, Untari R, Kusumatrisna AL, Hasyyati AN. Telecommunication Statistics in Indonesia 2021. Indonesia: BPS-Statistics Indonesia; 2021.
10. Klimczak KS, Twohig MP, Peacock GG, Levin ME. Using peer-support coaching to improve adherence to online ACT self-help for college mental health: a randomized controlled trial. Behav Res Ther. 2023;160:104228. doi:10.1016/j.brat.2022.104228
11. Aschbrenner KA, Naslund JA, Grinley T, Bienvenida JCM, Bartels SJ, Brunette M. A survey of online and mobile technology use at peer support agencies. Psychiatr Q. 2018;89:539–548. doi:10.1007/s11126-017-9561-4
12. Khanna MS, Carper M. Digital mental health interventions for child and adolescent anxiety. Cogn Behav Pract. 2022;29:60–68. doi:10.1016/j.cbpra.2021.05.003
13. Rotheram-Borus MJ, Swendeman D, Rotheram-Fuller E, Youssef MK. Family Coaching as a delivery modality for evidence-based prevention programs. Clin Child Psychol Psychiatry. 2018;23:96–109. doi:10.1177/1359104517721958
14. Saleem M, Kühne L, De Santis KK, Christianson L, Brand T, Busse H. Understanding engagement strategies in digital interventions for mental health promotion: scoping review. JMIR Ment Health. 2021;8:e30000. doi:10.2196/30000
15. Rudd BN, Beidas RS. Digital mental health: the answer to the global mental health crisis? JMIR Ment Health. 2020;7:e18472. doi:10.2196/18472
16. Whitmore J. Business coaching international: unlocking the secrets and the power. Coaching. 2009;2:176–179. doi:10.1080/17521880903102332
17. Sitanggang YA, Amin M, Sukartini T. Health coaching berbasis health promotion model terhadap peningkatan efikasi diri dan perilaku pencegahan penularan pada pasien tb paru [Health coaching based on a health promotion model to increase self-efficacy and transmission prevention behavior in pulmonary TB patients]. J Penelit Kesehatan Suara Forikes. 2017;2017:7. Indonesian. doi:10.33846/sf8402
18. Keessen P, van Duijvenbode IC, Latour CH, et al. Design of a remote coaching program to bridge the gap from hospital discharge to cardiac rehabilitation: intervention mapping study. JMIR Cardio. 2022;6:e34974. doi:10.2196/34974
19. Phaekwamdee M, Darakorn Na Ayuthaya S, Kiattisin S. The effects of coaching techniques on well-being of digital-technology users. JOItmC. 2022;8:170. doi:10.3390/joitmc8040170
20. Nathwani S, Rahman N. GROWing in dentistry: mentoring the dental professional. Br Dent J. 2022;232:261–266. doi:10.1038/s41415-022-3979-2
21. Okorie CO, Ogba FN, Amujiri BA, et al. Zoom-based GROW coaching intervention for improving subjective well-being in a sample of school administrators: a randomized control trial. Internet Interv. 2022;29:100549. doi:10.1016/j.invent.2022.100549
22. Bjursell C, Nystedt P, Björklund A, Sternäng O. Education level explains participation in work and education later in life. Educ Gerontol. 2017;43:511–521. doi:10.1080/03601277.2017.1357397
23. Loleka BY, Ogawa K. Influence of the level of education on women’s knowledge, attitude, and practices to control the transmission of COVID-19 in the Democratic Republic of the Congo. Sci Afr. 2022;17:e01299. doi:10.1016/j.sciaf.2022.e01299
24. Guo Y, Jiang D, Dong J, et al. A Study on the Comparison and Enhancement of Health Literacy of College Students in Guangdong Province in 2020 and 2022. SHS Web of Conferences; 2023 155:01002. doi:10.1051/shsconf/202315501002
25. van Ballegooie C, Heroux D, Hoang P, Garg S. Assessing the functional accessibility, actionability, and quality of patient education materials from Canadian cancer agencies. Curr Oncol. 2023;30:1439–1449. doi:10.3390/curroncol30020110
26. Liao Y, Ameyaw MA, Liang C, Li W. Research on the effect of evidence-based intervention on improving students’ mental health literacy led by ordinary teachers: a meta-analysis. IJERPH. 2023;20:949. doi:10.3390/ijerph20020949
27. Brattlöf F, Gustafsson PE, San Sebastián M. Prevalence and change in social inequalities in physical activity before and during the COVID-19 pandemic in Sweden. Int J Equity Health. 2023;22:21. doi:10.1186/s12939-023-01835-4
28. Dekhtyar S, Weber D, Helgertz J, Herlitz A. Sex differences in academic strengths contribute to gender segregation in education and occupation: a longitudinal examination of 167,776 individuals. Intelligence. 2018;67:84–92. doi:10.1016/j.intell.2017.11.007
29. Curreri C, Trevisan C, Grande G, et al. The influence of occupation type and complexity on cognitive performance in older adults. Psychiatry Res. 2022;326:111542. doi:10.1016/j.pscychresns.2022.111542
30. Liu Y, Ge T, Jiang Q. Changing family relationships and mental health of Chinese adolescents: the role of living arrangements. Public Health. 2020;186:110–115. doi:10.1016/j.puhe.2020.06.026
31. Ganong L, Coleman M. Qualitative research on family relationships. J Soc Pers Relat. 2014;31:451–459. doi:10.1177/0265407514520828
32. Paoletti J, Chen MA, Wu-Chung EL, et al. Employment and family income in psychological and immune outcomes during bereavement. Psychoneuroendocrinology. 2023;150:106024. doi:10.1016/j.psyneuen.2023.106024
33. Abbaslou T, Farsham A, Bidaki R, Bozorg B. The relationship between coping styles and family burden in chronic schizophrenic and bipolar type I patients’ caregivers. Egypt J Neurol Psychiatry Neurosurg. 2023;59:7. doi:10.1186/s41983-023-00609-7
34. Tatsumi H, Nakaaki S, Satoh M, Yamamoto M, Chino N, Hadano K. Relationships among communication self-efficacy, communication burden, and the mental health of the families of persons with aphasia. J Stroke Cerebrovasc Dis. 2016;25:197–205. doi:10.1016/j.jstrokecerebrovasdis.2015.09.018
35. Stephens RJ, White SE, Cudnik M, Patterson ES. Factors associated with longer length of stay for mental health emergency department patients. J Emerg Med. 2014;47:412–419. doi:10.1016/j.jemermed.2014.04.040
36. Vivalya BMN, Vagheni MM, Piripiri AL, et al. Prevalence and factors associated with relapse and long hospital stay among adult psychiatric patients with a history of childhood trauma. Psychiatry Res. 2022;316:114745. doi:10.1016/j.psychres.2022.114745
37. Li Y, Vo A, Randhawa M, Fick G. Designing utilization-based spatial healthcare accessibility decision support systems: a case of a regional health plan. Decis Support Syst. 2017;99:51–63. doi:10.1016/j.dss.2017.05.011
38. Maleki A, Moghaddam K, Cloninger P, Cullen J. A cross-national study of youth entrepreneurship: the effect of family support. Int J Entrepreneurship Innov. 2023;24:44–57. doi:10.1177/14657503211054284
39. Ran M-S, Yang LH, Liu Y-J, et al. The family economic status and outcome of people with schizophrenia in Xinjin, Chengdu, China: 14-year follow-up study. Int J Soc Psychiatry. 2017;63:203–211. doi:10.1177/0020764017692840
40. Zhao X, Y-H Y, Peng -M-M, et al. Change of poverty and outcome of persons with severe mental illness in rural China, 1994–2015. Int J Soc Psychiatry. 2021;67:315–323. doi:10.1177/0020764020951234
41. Provenzano AM, Stearns MA, Nadorff DK. The influence of caregiving on the relation between marital status and psychological health in a grandparent sample. Int J Aging Hum Dev. 2021;92:411–430. doi:10.1177/0091415020920000
42. Choi M, Sempungu JK, Lee EH, Chang -S-S, Lee YH. Single and combined effects of marital status, education attainment, and employment status on suicide among working-age population: a case-control study in South Korea. SSM Population Health. 2022;19:101246. doi:10.1016/j.ssmph.2022.101246
43. Bialowolski P, Weziak-Bialowolska D, Lee MT, Chen Y, VanderWeele TJ, McNeely E. The role of financial conditions for physical and mental health. Evidence from a longitudinal survey and insurance claims data. Soc Sci Med. 2021;281:114041. doi:10.1016/j.socscimed.2021.114041
44. Nasution SK, Mahendradhata Y, Trisnantoro L. Can a national health insurance policy increase equity in the utilization of skilled birth attendants in Indonesia? A secondary analysis of the 2012 to 2016 national socio-economic survey of Indonesia. Asia Pac J Public Health. 2020;32:19–26. doi:10.1177/1010539519892.394
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
