Back to Journals » Cancer Management and Research » Volume 15
Asciminib in the Treatment of Philadelphia Chromosome-Positive Chronic Myeloid Leukemia: Focus on Patient Selection and Outcomes
Received 1 April 2023
Accepted for publication 24 July 2023
Published 23 August 2023 Volume 2023:15 Pages 873—891
DOI https://doi.org/10.2147/CMAR.S353374
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Nobuko Hijiya,1,* Michael J Mauro2,*
1Division of Pediatric Hematology, Oncology, and Stem Cell Transplantation, Columbia University Irving Medical Center, New York, NY, USA; 2Myeloproliferative Neoplasms Program, Leukemia Service, Memorial Sloan Kettering Cancer Center, New York, NY, USA
*These authors contributed equally to this work
Correspondence: Nobuko Hijiya, Columbia University Irving Medical Center, 161 Fort Washington Ave, HIP-7, New York, NY, 10032, USA, Tel +1 212 305 9770, Email [email protected]
Abstract: Tyrosine kinase inhibitors (TKIs) have significantly changed the treatment of chronic myeloid leukemia (CML) and improved outcomes for patients with CML in chronic phase (CML-CP) and accelerated phase (AP). Now armed with numerous effective therapeutic options, clinicians must consider various patient- and disease-specific factors when selecting the most appropriate TKI across lines of therapy. While most patients with CML expected to have a near-normal life expectancy due to the success of TKIs, emphasis has expanded beyond response and survival to include factors like quality of life, tolerability, and long-term toxicity management. Importantly, a subset of patients can achieve sustained deep molecular response and can attain treatment-free remission. Despite these successes, unmet needs remain related to CML treatment, including the persistent challenge of treatment resistance and intolerance, broadening treatment options for patients with resistance mutations or serious comorbidities, and focus on specific populations such as children and young adults. In particular, the only previously available treatments for patients with CML-CP with the T315I mutation were ponatinib, olverembatinib (exclusively approved for use in China at the time of this writing), omacetaxine, and hematopoietic stem cell transplantation. Asciminib has entered the CML treatment landscape as a new option for adult patients with CML-CP who have received ≥ 2 prior TKIs or those with the T315I mutation. Asciminib’s unique mechanism of action, Specifically Targeting the ABL Myristoyl Pocket, sets it apart from traditional adenosine triphosphate-competitive TKIs. While asciminib may overcome unmet needs for patients with CML-CP and continues to be studied in other novel settings, guidance on how to integrate asciminib in treatment algorithms is needed. This review focuses on clinical data and how asciminib can overcome current unmet needs, discusses how to individualize patient selection, and highlights future directions to investigate asciminib in earlier lines of therapy and in children and adolescents.
Keywords: asciminib, chronic myeloid leukemia, tyrosine kinase inhibitors, patient selection, pediatrics
Introduction
Chronic myeloid leukemia (CML) is a malignancy marked by uncontrolled clonal expansion of myeloid cells, with most patients presenting in the chronic phase (CP) of disease.1 Historically, CML was considered a fatal diagnosis with limited treatment options, such as interferon and hematopoietic stem cell transplantation (HSCT).2 With the advent of tyrosine kinase inhibitors (TKIs) introduced to clinical practice just over 20 years ago, the therapeutic landscape of CML was transformed.3
Traditional adenosine triphosphate (ATP)-competitive TKIs have been highly and durably successful, providing clinicians with a broad array of therapeutic options and allowing the majority of older adult patients the opportunity to have a normal life expectancy.2,4,5 Due to this increase in life expectancy afforded by TKIs, quality of life (QOL), tolerability, and the risk of long-term adverse events (AEs) have become a major focus of patient care, particularly in children and young adults diagnosed with CML possibly requiring decades of treatment.6 The deep and durable response of TKIs has also led to the investigation and realization of treatment-free remission (TFR) as a possibility for certain patients with CML to improve QOL and minimize toxicity.7 For younger patients facing longer treatment duration, the prospect of TFR is especially desirable.8,9
Despite growing progress in the treatment of CML-CP, many unmet needs related to treatment efficacy, tolerability, and decision-making remain, which may differ for patients in earlier vs later lines of therapy.10–14 One of the most critical challenges is how to individualize treatment selection and patient care based on the needs and characteristics of each patient to optimize clinical outcomes and tolerability. The expansion in focus beyond disease control and remission, to the goal of TFR, adds additional complexity to treatment optimization, monitoring, and management decisions in younger and older patients with CML.
Asciminib, a newer BCR::ABL1-targeted therapy, was approved in 2021 by the US Food and Drug Administration for the treatment of patients ≥18 years of age with CML-CP who have received ≥2 prior lines of therapy, as well as patients with the T315I mutation, and in 2022 by the European Medicines Agency for the treatment of patients with CML-CP who have received ≥2 prior lines of therapy, providing another effective option for patients not meeting milestones with other TKIs.15,16 Due to its distinct (myristoyl site) specificity, likely minimizing off-target effects and thus toxicity, as well as a distinct and seemingly more limited mutation profile vs ATP-competitive TKIs, asciminib has potential to overcome barriers to treatment with traditional ATP-competitive TKIs, such as resistance and intolerance.17 The goal of this review is to highlight the key unmet needs in the treatment of CML, future opportunities for asciminib in earlier lines of therapy and pediatric and young adult patients, and decision-making regarding patients who should be considered for asciminib based on the current evidence landscape.
Unmet Needs in the Treatment of CML
Across all lines of therapy for CML, failure to meet or loss of optimal disease response and treatment intolerance are major concerns requiring treatment modification or switching to another therapy.11,12,18,19 Sequential TKI therapy is associated with increasingly worse outcomes after each subsequent line of therapy, and failure after 2 prior TKIs is associated with higher rates of progression and death.20,21 Such realities underscore the unmet need to further address issues of resistance and intolerance to TKI therapy in CML.
Clinical resistance to TKI therapy can be divided into primary resistance (ie, lack of initial response leading to treatment failure) and secondary resistance (ie, loss of response). Overall, primary resistance manifests in approximately 4% of patients with CML treated with first-line (1L) imatinib not achieving a complete hematologic response (CHR) and up to 25% of patients not achieving landmark responses such as major cytogenetic response (MCyR) or complete cytogenetic response (CCyR) by specific time points.22–24 In 5-year analyses, imatinib and second-generation (2G) TKIs demonstrate variable rates of primary resistance when used in the 1L setting. Based on IRIS and trials where imatinib is used as a comparator to 2G TKIs, rates of primary resistance (including failure to achieve early molecular response) for imatinib vary widely, from 4% to 39.5%.13,25–27 Rates of primary resistance for 2G TKIs range from 3.5% to 20%.13,26,27 However, varying definitions, evolving guidelines, and differences in data reporting make exact estimates problematic. The mechanisms of primary resistance to TKIs are not fully understood, hard to predict, and thought to be, in part, related to mutations that increase drug metabolism.28
In terms of secondary resistance in the 1L setting, studies comparing 2G TKIs with imatinib demonstrate similar results with 5 years of follow-up. The ENESTnd trial demonstrated 6%, 7.3%, and 10% of patients in the nilotinib 300 mg twice daily (BID), nilotinib 400 mg BID, and imatinib treatment arms, respectively, had confirmed loss of first major molecular response (MMR).26 The DASISION trial demonstrated disease progression in 18 of 258 (6.9%) patients, with loss of CHR included in the definition for progression.13 In the BFORE trial, cumulative incidence of on-treatment progression was 6.7% and defined to include loss of key response thresholds (CCyR and CHR).27 It is difficult to determine the precise extent of secondary resistance due to differences in the way rates are reported across trials. Secondary resistance appears more strongly influenced by BCR::ABL1 gene amplification and development of kinase domain (KD) mutations.29
The incidence of treatment-acquired mutations in BCR::ABL1, associated with resistance to ATP-competitive TKIs, increases with sequential lines of therapy.20 Mutations identified in several regions of BCR::ABL1 may lead to overlapping patterns of resistance among ATP-competitive TKIs with similar binding requirements, reducing viable treatment options for patients resistant to their current therapy (multidrug-resistant CML).30,31 BCR::ABL1 KD mutations are the most common mechanisms of resistance to ATP-competitive TKIs, detected in up to 68% of patients with imatinib resistance and 2.2% to 26% of patients following 1L treatment with a 2G TKI (bosutinib, nilotinib, and dasatinib) who underwent mutational analysis for reasons such as suboptimal response and disease progression.32,33 Resistance increases with each subsequent line of therapy; up to 33% of patients who receive second-line (2L) dasatinib or nilotinib develop new BCR::ABL1 mutations.20,32 The BCR::ABL1 T315I mutation is commonly associated with resistance to both imatinib and the 2G TKIs nilotinib, dasatinib, and bosutinib.34 The reported frequency of T315I mutations is thought to be as high as 27% among patients with BCR::ABL1 mutations when sequencing is conducted at imatinib failure and up to 53% in 2L trials.32 Prior to asciminib, the only approved TKIs with sensitivity to the T315I mutation were the third-generation TKIs ponatinib and olverembatinib (exclusively approved for use in China at the time of this writing).20,35,36
In addition to resistance, intolerance of TKIs is a major issue affecting patient QOL, leading to suboptimal adherence and dosing, as well as treatment discontinuation; intolerance and resistance are often a combined challenge.37,38 While each TKI has a distinct AE profile, there are many common AEs such as gastrointestinal toxicities or fluid retention (edema/effusions), or, primarily in adult patients, more morbid risks such as cardiovascular events (CVEs), which pose a management challenge for prescribers.39–41 Treatment intolerance can also lead to sequential lines of therapy, potentially reducing treatment efficacy. In the IRIS trial, a modest 7% of patients discontinued imatinib by 10 years due to AEs; in other key clinical trials, 10.7% to 25% of patients who received therapy with 2G TKIs in the 1L setting discontinued therapy due to AEs by 5 years.13,26,27 Higher doses of certain TKIs may be required in 2L treatment and beyond with evident resistance to prior therapy, potentially contributing to discontinuation due to AEs, reportedly being higher in later lines.10,11,26,42–44 Studies of 2G TKIs used in the 2L setting demonstrate discontinuation rates due to AEs of 20.6% to 31%, with a follow-up period ranging from 4 to 9 years.11,43,44 The third-generation TKI ponatinib is approved for use in patients with resistance to or intolerance of prior TKIs. However, up to 21% of patients may discontinue treatment with ponatinib due to AEs.19 In addition, ponatinib is associated with a dose-dependent risk of vascular toxicity, likely impacted by pre-existing cardiovascular disease, limiting use in this population.45
Overlapping patterns of TKI resistance mutations and intolerance increase the challenges of patient care and minimize the success of sequential therapeutic strategies.3,31 Therefore, although switching TKIs is the recommended clinical approach when faced with resistance or intolerance, it does not guarantee successful clinical outcomes, underscoring the need for thoughtful and precautionary, yet response-optimized, individualized therapy selection in the management of CML.46 Based on key clinical trials of approved 1L TKIs, between 16% and 32% of patients discontinue 1L therapy and may require a switch to 2L therapy within 5 years, with only approximately one-third to one-half of 1L patients achieving deep molecular response (DMR) by 5 years on 1L therapy.13,25–27 DMR is a prerequisite to attempt TFR, an important treatment goal for patients with CML.42 In addition, in the aggregate, up to 78% of patients on 2L therapy do not achieve MMR by 2 years.47–49 Optimal response kinetics, wherein MMR is achieved by 1 year of primary therapy, is associated with a higher likelihood of DMR.42
In addition to limitations of CML treatment in adults, the management of pediatric CML presents both similar and unique challenges. Since CML in childhood is a rarer malignancy, accounting for <3% of pediatric leukemias, evidence-based guidelines for its management are lacking.42 CML in children and adolescents generally follows a more proliferative and often more aggressive disease course.50 Imatinib, dasatinib, and nilotinib are the only options currently approved for the treatment of CML in children.42 Of note, ponatinib is the only ATP-competitive TKI with activity against the T315I mutation. However, the use of ponatinib in pediatric CML-CP has not been thoroughly investigated, and an ongoing Phase 1 study is currently evaluating its use in this population.51 Issues regarding medication adherence, intolerance, and risks of long-term toxicities are critical considerations when treating pediatric patients with CML.42,50,52 The aforementioned limitations of current approved therapies for CML in adult and pediatric patients, in addition to the presence of common and age group-specific comorbidities, risk factors, and AEs impacts, described below, underscore the need for novel agents to treat CML in 1L and later line settings.
Overview of Asciminib
Asciminib is the first BCR::ABL1 inhibitor to specifically target the ABL Myristoyl Pocket (STAMP), differentiating it from currently available ATP-competitive TKIs.53 Normally, the ABL N-terminus is myristoylated, allowing it to bind to the myristoyl pocket and resulting in autoinhibition of ABL kinase.54–56 In CML, the BCR::ABL1 fusion protein leads to loss of the ABL N-terminus, thereby disabling this autoregulatory mechanism and resulting in a constitutively active form of BCR::ABL1.53,55,56 Asciminib, an allosteric inhibitor, is able to bind to the myristoyl pocket, mimicking the normal configuration of the myristoylated N-terminus and restoring the inhibition of ABL.53
This unique mechanism of action of asciminib leads to improved specificity over ATP-competitive TKIs, which rely on binding to the ATP-binding site of BCR::ABL1 to produce their effect.57 The specificity of asciminib has the potential to reduce safety issues associated with off-target effects with ATP-competitive TKIs.17 Due to the unique binding site of asciminib, it can also overcome mutations conferring resistance to traditional TKIs such as T315I, which is localized to the ATP-binding site of BCR::ABL1.57
Asciminib may be administered at doses of 80 mg once daily (QD) or 40 mg twice daily (BID) for patients with non-T315I mutated CML-CP and requires a dose of 200 mg BID for T315I-mutated CML-CP.58 Approval of asciminib for use in adults with CML-CP previously treated with ≥2 TKIs was based on the efficacy and safety results from ASCEMBL, a multicenter, open-label, Phase 3 trial of asciminib vs bosutinib in patients with CML-CP who were previously treated with ≥2 TKIs.59 Approval for use in adult patients with T315I-mutated CML-CP was based on data from the multicenter, open-label, Phase 1 study, X2101, which demonstrated the efficacy of asciminib in heavily pretreated patients with CML who had resistance to or unacceptable side effects from currently available ATP-competitive TKIs and those with the T315I mutation.56 Of note, all studies mentioned in this review include only adult patients unless pediatric patients are specifically mentioned.
Clinical Trials Supporting the Initial Approval of Asciminib
X2101
X2101 is a Phase 1, dose-escalation study evaluating asciminib in patients with CML-CP and –accelerated phase (AP) who were previously treated with ≥2 TKIs. A total of 141 patients with CML-CP and 9 patients with CML-AP were enrolled and treated with asciminib QD or BID (dose range, 10–200 mg) during the enrollment period between May 2014 and September 2017. As of September 2017, 73% of patients were continuing treatment with asciminib.56 Patients with the T315I mutation were eligible for inclusion after ≥1 TKI and with no other therapeutic options. The primary endpoint was the maximum tolerated dose and/or the recommended dose for expansion of asciminib. Secondary outcomes included safety, efficacy, and pharmacokinetics.56
In patients with CML-CP without the T315I mutation who had resistance to or unacceptable side effects from prior ATP-competitive TKIs, asciminib demonstrated significant clinical activity. Rates of achieving or maintaining MCyR and CCyR were 77% and 70%, respectively, with a median follow-up of 72 weeks.56 MMR was achieved or maintained by 12 months in approximately half of heavily pretreated patients (>2 prior TKIs) and 57% of patients who discontinued prior ponatinib due to resistance or intolerance (Table 1).56 In patients without MMR at baseline, this response was achieved in 47% of ponatinib-naive patients and 40% of ponatinib-pretreated patients by 12 months.56 A subanalysis was performed on patients with a baseline BCR::ABL1IS ≤1% and considered to be intolerant of or resistant to their most recent TKI. Treatment with asciminib resulted in >40% of evaluable patients not in MR4 or MR4.5 at baseline achieving MR4 or MR4.5 overall by week 48.60
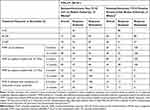 |
Table 1 Efficacy of Asciminib by Months 6 and 12 |
Safety was evaluated in all 150 patients, including those with the T315I mutation and those with CML-AP, demonstrating an overall manageable safety profile of asciminib. The most common all-grade treatment-emergent adverse events were fatigue (29.3%), headache (28.0%), and elevated lipase (26.7%).56 Of note, clinical pancreatitis occurred in 3% of evaluable patients, all of whom were receiving higher doses of asciminib (>40 mg BID), and all cases resolved within 5 to 10 days of asciminib discontinuation. A maximum tolerated dose of asciminib was not reached, and most AEs were grade 1 or 2.56
Long-term data from X2101 continued to demonstrate the durable efficacy of asciminib with high cumulative rates of MMR and DMR by 4 years. Cumulative MMR continued to increase over time irrespective of line of therapy or baseline disease characteristics.61 Additionally, most patients (69.6%) remained on asciminib during this timeframe, and no new safety signals were reported. Importantly, no increase in the frequency or severity or arterio-occlusive events (AOEs) was observed. Most all-grade AEs occurred in year 1 of treatment and were grade 1 or 2, reflecting the favorable safety profile of asciminib with longer follow-up.61
Asciminib was also clinically active in patients with CML-CP with the T315I mutation (Table 1). Rates of achieving or maintaining MCyR and CCyR were 60% and 44%, respectively, with a median follow-up of 37 weeks. Molecular responses correlated to number of prior TKIs; by 12 months, rates of MMR were 44% for patients treated with ≤2 prior TKIs and 11% for more heavily pretreated patients, defined as prior treatment with >2 TKIs.56 MMR was achieved in 17% of patients with prior resistance or intolerance of ponatinib, suggesting modest clinical activity of asciminib in this patient group.56 For patients with the T315I mutation, higher molecular response rates correlated with higher dosing schedules (>150 mg BID). This latter finding is consistent with in vitro studies demonstrating that higher concentrations of asciminib are necessary to reach half the maximum inhibitory concentration in T315I-mutated cell lines.56
An analysis of 48 patients with CML with the T315I mutation receiving a starting dose of asciminib 200 mg BID in the X2101 study demonstrated that 48.9% of patients achieved MMR by week 96, with ≥50% of patients who achieved MMR also achieving MR4 or MR4.5.62 MMR rates for ponatinib-naive and ponatinib-pretreated patients receiving asciminib were 57.9% and 30.8%, respectively, by week 24 and 68.4% and 34.6%, respectively, by week 96, and corresponding rates of BCR::ABL1IS ≤1% were 62.5% and 33.3%, by week 24, respectively, and 81.3% and 47.6% by week 96, respectively.62 Response rates to asciminib in CML with a T315I mutation were thus substantial and supported US Food and Drug Administration approval. In this analysis, the most frequent AEs were increased lipase and fatigue (29.2%) and nausea (27.1%), with limited increases in AEs over time. Of note, AOEs occurred in 8.3% of patients, none of which led to dose adjustment or death. Only 4 patients discontinued asciminib due to AEs.62 This analysis thus revealed favorable efficacy and safety of higher-dose asciminib in patients with CML-CP with the T315I mutation.
ASCEMBL
ASCEMBL is a Phase 3, randomized, open-label, multicenter study comparing the efficacy and safety of asciminib vs bosutinib in adults with CML-CP previously treated with ≥2 TKIs and with treatment failure or intolerance of the most recent TKI as defined in the European LeukemiaNet (ELN) 2013 Recommendations (Figure 1). A total of 233 patients were randomized 2:1 to receive asciminib 40 mg BID or bosutinib 500 mg QD and were stratified by baseline MCyR.59 The primary analysis was conducted at week 24, with follow-up and additional endpoints performed and reported at weeks 48 and 96.59,63 Of note, based on known bosutinib resistance, patients with a known T315I or V229L mutation at any time before the study and those with significant cardiac disease were excluded from this study.59,64
 |
Figure 1 ASCEMBL study design. Abbreviations: ABL1, Abelson tyrosine kinase 1; BCR, breakpoint cluster region; CML-CP, chonic myeloid leukemia in chronic phase; ELN, European LeukemiaNet; IS, International Scale; MCyR, major cytogenetic response; CCyR, complete cytogenetic response rate; MMR, major molecular response (BCR::ABL1IS ≤0.1%); TKI, tyrosine kinase inhibitor. Notes: aMust meet lack of efficacy criteria based on the 2013 ELN recommendations for second-line TKI therapy. bPatients who discontinued bosutinib treatment due to intolerance or any reason other than lack of efficacy were not allowed to switch to asciminib. Adapted from Blood, volume 138, Rea D, Mauro MJ, Boquimpani et al A Phase 3, open-label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs. Page numbers: 2031–2041, copyright 2021, with permission from Elsevier.59 |
The primary endpoint for this study was MMR at week 24, with MMR at week 96 as a key secondary endpoint.59,63 At week 24, the MMR of asciminib (25.5%) was superior to bosutinib (13.2%) and met the primary study endpoint.59 Investigators performed a multivariate analysis to evaluate effects of treatment after controlling for disease features and demographics between treatment cohorts. MMR at week 96 results favor asciminib compared with bosutinib in patients who discontinued their last TKI due to lack of efficacy or intolerance and regardless of BCR::ABL1 levels at baseline. A consistent MMR benefit for asciminib vs bosutinib was preserved across all major demographic and prognostic subgroups assessed in the week 24 and 96 analyses, including line of therapy (Figure 2). This effect was durable, and MMR remained consistently better with asciminib with rates of 37.6% vs 15.8% with asciminib and bosutinib, respectively, at week 96.59,63,65,66
 |
Figure 2 Risk difference (95% CI) for MMR at week 96 from subgroup analyses. Abbreviations: ABL1, Abelson tyrosine kinase 1; BCR, breakpoint cluster region; CI, confidence interval; IS, international scale; TKI, tyrosine kinase inhibitor. Notes: aPatients with T315I and V299L BCR::ABL1 mutations or a nonevaluable mutation assessment were excluded from the subgroup analysis. Reproduced from Hochhaus A, Rea D, Boquimpani et al Asciminib vs bosutinib in chronic-phase chronic myeloid leukemia previously treated with at least two tyrosine kinase inhibitors: longer-term follow-up of ASCEMBL. Leukemia. Mar 2023;37(3):617–626. Creative Commons.63 |
The week 24 analysis of ASCEMBL also demonstrated a favorable safety profile for asciminib with some tolerability advantages over bosutinib continuing upon subsequent analyses, including lower rates of grade ≥3 AEs in the asciminib arm (50.6%) than in the bosutinib arm (60.5%).59 The most common AEs experienced in the asciminib arm were thrombocytopenia (28.8%), neutropenia (21.8%), and headache (16%). In contrast, the most common AEs in the bosutinib arm were diarrhea (71.1%), nausea (46.1%), and increased alanine aminotransferase (27.6%).59 Gastrointestinal AEs were markedly more frequent with bosutinib.59 The favorable safety profile of asciminib vs bosutinib is further evidenced and supported by discontinuation rates due to AEs that were lower with asciminib (5.8%) vs bosutinib (21.1%) (Table 2).59
 |
Table 2 Most Frequent Adverse Events (≥10% of Patients in Any Treatment Arm) by Week 24 |
At week 96, discontinuations due to AEs continued to be low, at 7.7% with asciminib vs 26.3% with bosutinib. With longer exposure, safety and tolerability of asciminib continued to be more favorable than those of bosutinib, with no new or worsening safety signals reported in the week 96 analysis.63,65,66 The risk of CVEs limits use of some TKIs, particularly in patients with underlying risk factors. Regarding the important question of CVEs relative to asciminib, in ASCEMBL the frequency of AOEs was 5.1% with asciminib and 1.3% with bosutinib by week 96; however, patients treated with asciminib vs bosutinib had a longer median duration of exposure (23.7 months vs 7.0 months).59,63 Reassuringly, the exposure-adjusted AOE rate (per 100 patient-years) with asciminib was 3.3 and 3.0 in the primary analysis and week 96 analysis, respectively. Available data to date thus demonstrate low rates of AOEs, and no apparent increased risk was seen with asciminib over time.63,65,66 Future studies of asciminib in newly diagnosed patients will help to clarify the safety profile of asciminib, including the important question of AOEs without the confounding impact of prior TKI exposure. Using validated questionnaires assessing symptom burden in CML-CP, asciminib showed advantages over bosutinib and was more likely to improve or maintain baseline QOL.67 As such, this may suggest an advantage of asciminib vs bosutinib in regard to adherence.
The X2101 and ASCEMBL studies provided critical data supporting asciminib as a novel, safe, and highly effective new treatment option for patients with CML-CP that is able to address a high unmet need, including those who had previously received ≥2 other lines of therapy or who are harboring the T315I mutation.56,59 This latter finding is of particular importance as the only other widely approved TKI with activity against the T315I resistance mutation is ponatinib, which is often limited due to its cardiovascular risks.56 In addition, X2101 demonstrated that a subset of patients with resistance to or intolerance of ponatinib achieved MMR with asciminib. Asciminib may therefore benefit patients with CML-CP with very limited treatment options, including those with no options other than HSCT.56 The above data demonstrating the MMR benefit of asciminib in ponatinib-naive vs ponatinib-pretreated patients suggest that treatment with asciminib prior to ponatinib may produce higher response rates. Additional ongoing studies in patients with CML-CP across lines of therapy will continue to generate more data to build the profile of asciminib and help aid in patient selection.
Future Directions for Asciminib in CML
Given the demonstrated efficacy and safety of asciminib as a therapeutic option for adult patients with CML in later lines of therapy, there is a keen interest in investigating asciminib in other clinical scenarios, including in earlier lines of therapy, in patients with comorbidities, and combined with ATP-competitive TKIs to improve efficacy, minimize toxicity, delay resistance, and facilitate TFR (Table 3). In addition, given the unique challenges for managing pediatric patients with CML, evaluating the use of asciminib in this population represents an exciting frontier in the advancement of CML treatment.42
 |
Table 3 Ongoing Trials of Asciminib in CML |
Currently, asciminib is being evaluated in several earlier-line studies, including in adult patients with newly diagnosed CML-CP. ASC4FIRST (NCT04971226) is a Phase 3, open-label, multicenter study investigating 1L asciminib vs all currently approved ATP-competitive TKIs. This is the first trial comparing a novel agent to all TKIs approved for the treatment of CML in 1L and will provide much needed comparative data between asciminib and ATP-competitive TKIs using MMR at week 48 as its primary endpoint.79 ASC4START (NCT05456191) is a Phase 3b study evaluating the safety of asciminib vs nilotinib in the 1L setting for the treatment of adults with CML-CP. Outcome measures for this study will be time to discontinuation of study treatment due to AEs as a primary outcome, with secondary outcomes related to efficacy.80 ASC2ESCALATE (NCT05384587) is a Phase 2 study evaluating patients with CML-CP treated with asciminib in the 2L setting and will provide data on whether these patients can benefit from asciminib dose escalation if not meeting certain response milestones.82 Collectively, the above studies will provide critical data supporting the use of asciminib in earlier lines of therapy.
Trials such as FASCINATION (NCT03906292) are assessing combination therapies with asciminib for the treatment of adults with CML-CP in the 1L setting.78 The goal of combination therapy is to increase the number of patients meeting clinical milestones, increase depth of response to improve long-term outcomes, and offer the possibility of TFR.83 Preclinical and in vitro studies have demonstrated that combining asciminib with an ATP-competitive TKI may reduce the likelihood of treatment resistance due to mutations in either the ATP-binding site or myristoyl pocket.84 With regard to safety, in vitro modeling suggests that combinations with asciminib may permit lower drug dosages, improving tolerability.85 X2101 investigated a safe and tolerable dosing schedule for asciminib in combination with imatinib, dasatinib, or nilotinib in adult patients treated with ≥2 prior TKIs.71 Preliminary efficacy results from this study are promising and demonstrate, for example, that combining asciminib with imatinib produced rates of CCyR and MMR of 50% and 42%, respectively, by week 48 in patients without this level of response at baseline.86 This combination also revealed a generally favorable safety profile.86 These collective in vitro and early clinical data further support the potential of combination therapies with asciminib, warranting ongoing investigation to determine a safe and tolerable dosing schedule for asciminib in combination with imatinib, dasatinib, or nilotinib in adult patients treated with ≥2 prior TKIs.71
Given the unmet need in pediatric patients, including resistance, intolerance, magnified concern over long-term toxicity, and population-specific concerns such as growth retardation reported with currently approved ATP-competitive TKIs, a Phase 1/2 trial of asciminib has been initiated to assess safety and efficacy of asciminib in children.87 ASC4KIDS (NCT04925479) is an open-label, 3-part, multicenter study investigating dosage, safety, and pharmacokinetics of asciminib monotherapy in pediatric patients with CML-CP following treatment with ≥1 prior TKI. The primary objective of this trial is to characterize the pharmacokinetics of asciminib in pediatric patients with the goal of identifying the pediatric formulation dose of asciminib in the fed state comparable to the adult dose of 40 mg BID in the fasted state. The dose determined in part 1 will be administered in parts 2 and 3, evaluating BID and QD regimens in this population, respectively.73 Lifelong TKI exposure could significantly impact adherence, and long-term consequences of TKI therapy remain largely unknown; therefore, providing opportunity to stop treatment and attempt TFR is a particularly worthwhile goal in pediatric patients.88 Deep and sustained responses seen with asciminib in adults with CML raises the possibility that such benefits could extend to pediatric patients and provide the opportunity of TFR.59,65,66 Importantly, adolescents and young adults (AYA) with CML may have a higher tumor burden at diagnosis, and some studies have reported poorer response to treatment and outcomes in this population.89 Nonadherence is estimated to impact up to 60% of AYA patients with cancer and is associated with poorer outcomes.89 AYA are also expected to have extended periods of treatment, thereby experiencing similar challenges and survivorship issues to pediatric patients.90,91 Additionally, fertility is an important clinical consideration in AYA patients making the prospect of stopping treatment and attempting TFR attractive.91 As such, the aforementioned benefits of asciminib may extend to AYA patients.
Considerations for Patient Selection for Asciminib
Prior to approval of asciminib in the third line and beyond (3L+) setting, effective 3L+ therapeutic options for CML were limited, and sequential treatment with 2G TKIs were associated with decreasing clinical response. For these patients, ponatinib may be an option, which demonstrated clinical efficacy but carries significant cardiovascular risks.92 While availability of asciminib gives a broader range of patients a new option for later-line therapy, this choice also brings new challenges with respect to treatment planning on an individual patient basis. Identifying appropriate patient candidates, timing of treatment initiation or dose adjustment, and consideration of numerous patient factors, including disease risk, molecular factors, efficacy and tolerability of prior treatments, patient age, comorbidities, and individual patient goals, are all crucial.93
Molecular Response Milestones and Patient Goals
Current ELN recommendations and National Comprehensive Cancer Network (NCCN) guidelines discuss molecular monitoring and response goals by line of therapy.42,46 The ELN 2020 recommendations state that the definition of response to 2L treatment should be the same as for 1L treatment with BCR::ABL1IS ≤10%, ≤1%, and ≤0.1% at 3, 6, and 12 months, respectively, defined as optimal response milestones. Although the precise definition of an acceptable response in patients with ≥2 prior TKIs is not formalized, a BCR::ABL1IS >1% or response less than CCyR is considered insufficient for optimal survival.46 NCCN guidelines recommend switching to a 2G TKI for patients with disease resistant to imatinib, although there is no clear evidence that switching improves long-term outcomes in 2L, and although dose escalation of imatinib has demonstrated some benefit in these patients, duration of responses have been short. However, there is some evidence that early molecular response (BCR::ABL1IS ≤10% at 3 and 6 months) after 2L therapy with dasatinib or nilotinib is associated with improved PFS and OS. It is currently recommended that patients in 2L therapy and beyond not achieving cytogenetic and molecular responses at 3, 6, and 12 months should be evaluated for alternative therapies or HSCT. Failure after ≥2 prior TKIs is not associated with durable responses when patients are switched to an alternate 2G TKI, and the NCCN recommends treatment with ponatinib or asciminib or enrollment in a clinical trial for these patients.42
Now, data from the Phase 1 X2101 and Phase 3 ASCEMBL trials show DMRs are possible with asciminib not previously expected for patients in later lines of therapy.62,63,65,66 These data also suggest that safety and tolerability of asciminib may permit longer use, making achievement of molecular responses more feasible.63,65,66 Having another option for patients may facilitate treatment switch decisions in later lines of therapy with greater odds of longer-term tolerability and response.
Mutation Status
As previously noted, mutations in the BCR::ABL1 KD confer resistance to many TKIs, and each TKI has a somewhat unique resistance profile.32,42 Molecular testing for mutations is important at a number of points during treatment, especially for patients not meeting milestones. The T315I mutation is one of the most common KD mutations, and availability of asciminib gives patients with this mutation another option beyond ponatinib.32 It is unclear if asciminib is superior to ponatinib in this setting regarding efficacy, as there are no direct randomized clinical trials comparing the 2 drugs. In the OPTIC trial, 60% of patients with the T315I mutation achieved BCR::ABL1IS ≤1% by 12 months with ponatinib when administered at a dose of 45 mg QD. In this trial, patients in the 45- and 30-mg cohorts reduced their dose to 15 mg QD upon achievement of this response, and most of those who lost response upon dose reduction had the T315I mutation at baseline.45 In patients with the T315I mutation, X2101 demonstrated that BCR::ABL1IS ≤1% was achieved by 45.9% of patients without this level of response at baseline with asciminib at a dose of 200 mg BID by week 24, with a higher rate of 62.2% seen by week 96.62
More data are needed to establish the efficacy of asciminib among patients with non-T315I KD mutations. In ASCEMBL, a small number of patients had baseline BCR::ABL1 KD mutations other than T315I and V299L. Therefore, no conclusions could be drawn in regard to impact of mutations on efficacy.59 While little is known about the mechanisms of resistance to asciminib, certain mutations such as A337T and P465S that impact the myristoyl pocket may play a role.42,53 As such, the most recent NCCN guidelines have added these mutations as contraindications to asciminib therapy; however, availability to test for these mutations in routine clinical practice is lacking.42 Studies evaluating asciminib plus an ATP-competitive TKI are ongoing to evaluate the potential of combination therapy to overcome resistance to an acquired mutation or compound mutations associated with either therapy.71,75,78
Prior TKI Exposure
Patients treated with asciminib achieved BCR::ABL1IS ≤1% and MMR by week 96 regardless of last TKI received and reason for discontinuation. Responses also continued to deepen over time in this heavily pretreated population.63,94 Although X2101 demonstrated that a higher proportion of patients with a baseline BCR::ABL1IS ≤1% achieved MMR by 1 year compared with patients with BCR::ABL1IS >1% at baseline, ASCEMBL revealed that more patients treated with asciminib than with bosutinib achieved molecular responses, irrespective of baseline BCR::ABL1 levels.56,59 Furthermore, asciminib may be selected for treatment of CML-CP for patients with prior treatment with ≥2 TKIs, including prior ponatinib. However, real-world evidence and data from X2101 demonstrate that patients with CML-CP without prior ponatinib exposure may demonstrate better global outcomes with asciminib relative to ponatinib-pretreated patients. Further investigation is needed to determine the differential impact of prior resistance vs intolerance to ponatinib on responses to asciminib.62,95
Tolerability and Comorbidities
The presence of comorbidities, such as cardiovascular risk factors, diabetes, gastrointestinal disorders, and pulmonary issues, also creates a management challenge when prescribing TKIs for patients with CML. Different management options for 1L TKI therapy have been suggested for common comorbidities, but are not absolute. Below, we describe common comorbidities that can pose a challenge when selecting treatment for patients with CML.
CVEs, including AOEs, have been associated, at varying degrees, with several TKIs.39,96 Risk of CVEs on treatment appears lower in patients with minimal or no pretreatment risk factors; risk of on-treatment events increases with the number of baseline cardiovascular risk factors.97 It is estimated, however, that 30% of patients with CML have baseline cardiovascular risk factors such as hypertension and obesity, with more than 10% having diabetes.98,99 Quantifying risk of CVEs with each TKI is challenging given the heterogeneity in data reporting from different studies and different patient populations. Among approved TKIs, both ponatinib and nilotinib have cardiovascular warnings in their labels.98,100,101
In the PACE trial, serious AOEs occurred in 26% of patients treated with ponatinib.19 By contrast, rates of AOEs were 3.2%, 5.3%, and 9.6% in the 15-, 30-, and 45-mg QD cohorts, respectively, in the OPTIC dose-ranging study.45 Although both trials evaluated ponatinib in heavily pretreated patients with CML, including those with the T315I mutation, important differences in recognition and management of AOEs, and, in OPTIC, dose exposure, should be considered.19,45 Notably, the starting dose of ponatinib in PACE was 45 mg QD and allowed for dose reductions in response to AEs. In OPTIC, patients were randomly assigned to treatment with either 45, 30, or 15 mg QD of ponatinib, and half of patients in the 45-mg cohort underwent planned dose reduction after 3.4 months up achieving BCR::ABL1IS ≤1%.45 Also, the median duration of follow-up with PACE was nearly twice that of OPTIC at the time of data reporting.19,45
The OPTIC trial demonstrated exposure-adjusted AOE rates of 2.1%, 3.6%, and 5.6% for the 15-, 30-, and 45-mg cohorts.45 In PACE, exposure-adjusted incidence rates decreased over time from 15.8% to 4.9% in years 1 and 5, respectively.19 ASCEMBL evaluated risk of AOEs with asciminib and demonstrated an exposure-adjusted AOE rate of 3.3 per 100 patient-years at week 24 that remained similar to slightly lower, at 3.0 per 100 patient-years by week 96.63,65,66 This is important to consider given that prior to asciminib, ponatinib was the only widely approved TKI for patients harboring the T315I mutation, although it carries a significant risk of AOEs.56 Importantly however, unlike PACE and OPTIC, the ASCEMBL trial, by design, needed to exclude patients with the T315I mutation, and due to differences in patient populations and study designs, results from these trials cannot be directly compared.19,45,59 ENESTnd investigated nilotinib compared with imatinib in 1L and is the only trial following newly diagnosed patients with CML-CP treated with a 2G TKI for ≥10 years.102 Nilotinib has been historically associated with high cardiovascular risk and ENESTnd found an overall risk of CVEs of 7.5% and 13.4% with nilotinib 300 mg BID and 400 mg BID, respectively, in 1L treatment of patients with CML-CP by 5 years; this risk increased to 16.5% and 23.5%, respectively, by 10 years.26,41,102 Importantly, this study also explored frequency of CVEs in patients with pre-existing cardiac risk and found risk of CVEs was higher in those with high cardiovascular risk.26 This is notable since patients in ASCEMBL were heavily pretreated (≥2 prior TKIs) and, of the 8 patients with AOEs in the asciminib arm reported by week 96, 7 had prior nilotinib exposure, 3 had prior ponatinib exposure, and most had cardiovascular risk factors at screening.63,65,66 Overall, based on available evidence, asciminib may be associated with a lower risk of AOEs than ponatinib and nilotinib, perhaps providing an alternative for patients with 2 or more prior TKIs and the T315I mutation irrespective of cardiovascular risk factors. However, longer-term follow-up and more data, particularly in less heavily treated or previously untreated patients, are needed to fully evaluate cardiovascular risks associated with asciminib.
Hyperglycemia has also been reported with several TKIs. Safety from the X2101 trial showed that grade ≥3 hyperglycemia occurred in 2% of patients with asciminib; currently, no warnings or precautions exist related to use of asciminib in diabetic patients.56,58 Hypertension should be carefully monitored in patients taking asciminib as it emerged in 11.5% of patients in ASCEMBL and nearly 20% of patients in X2101, but medically controlled hypertension does not preclude asciminib as a therapeutic option.56,58,59
A history of pancreatitis, although not a contraindication to asciminib, should prompt more frequent monitoring for pancreatic toxicity in patients receiving asciminib.58 Although no cases of pancreatitis were reported in either the asciminib or bosutinib arm of ASCEMBL, pancreatitis occurred in 3% of patients who received asciminib in X2101, albeit exclusively at doses of >40 mg BID.56
Pulmonary issues have been reported with TKIs, particularly dasatinib.8,13 In the ASCEMBL and X2101 studies, pulmonary issues or pleural effusions with asciminib have been uncommon.58 In X2101, 6% of patients with CML-CP/AP experienced a pleural effusion with asciminib; in this study, doses of up to 200 mg BID were used and a majority of patients were previously treated with dasatinib.56 Therefore, baseline pulmonary issues and prior exposure to TKIs with pulmonary toxicity do not appear to be significant barriers to treatment with asciminib.
Gastrointestinal (GI) AEs, such as nausea, diarrhea, abdominal pain, and vomiting, are a common class effect across BCR::ABL-targeted therapies. However, the incidence of GI AEs with asciminib is lower than bosutinib in the ASCEMBL study.59 Nausea and vomiting are associated with nonadherence and play a substantial role in patients’ ability to stay on treatment at an optimal dose.103 Therefore, asciminib may confer some advantages with respect to GI tolerability.
Taken together, the above safety factors are important to patient selection given that long-term TKI therapy nonadherence is a recognized issue in the population of patients treated for CML and can impact a majority of patients. Such nonadherence can adversely impact survival and increase healthcare resource utilization.104 Management of toxicity such as GI AEs are important to consider as they can reduce a patient’s QOL and further decrease long-term adherence.40,103,105 The safety of asciminib, although still under investigation, appears to have a favorable profile that may positively impact adherence and preserve QOL.
Patient Age
Patient age is an important factor when selecting a TKI as the rate of relevant comorbidities tends to increase, and patients may present contraindications to certain treatments and may be at a higher risk for intolerance or more serious AEs with increasing age.46,98,106,107 According to a retrospective study of commercially insured and Medicare enrollees with CML, older age (≥55 years) is associated with multiorgan system AEs with TKIs.108 Trial data supports a similar concern; in the DASISION trial, median age of patients who developed a pleural effusion with dasatinib was 15 years older than those who did not.109 In the ASCEMBL study, 19% of patients were ≥65 years of age, and notably, no differences in efficacy were observed between these patients and younger patients. However, the sample size of patients ≥75 years of age was insufficient to draw conclusions related to differences in efficacy or safety.59 Therefore, it is unknown if advanced age has a significant impact on efficacy and/or safety of patients with CML treated with asciminib. Importantly, patients with CML who are <50 years old are expected to live more than 30 years.8 In these patients, long-term treatment can result in AEs that adversely impact QOL.110 As patients develop comorbidities with age, they are at higher risk for developing AEs.98 Therefore, tolerability becomes increasingly important with long-term treatment in this population.
Drug–Drug Interactions
Asciminib is an inhibitor of CYP3A4, CYP2C9, and CYP2C8 and can increase plasma concentration of medications metabolized by these enzymes, thereby increasing the risk of AEs associated with these concomitant medications.57,58 In addition, asciminib is also a CYP3A4 substrate, and coadministration of asciminib with a strong inhibitor of CYP3A4 can increase risk of asciminib toxicity.58 For patients taking substrates of CYP3A4, it is recommended that AEs from these substrates are carefully monitored and such substrates be avoided with higher doses of asciminib (ie 200 mg BID for patients with the T315I mutation).58 It is advised that asciminib not be used at all in patients taking CYP2C9 substrates with a narrow therapeutic window.58 If coadministration is unavoidable, the dose of CYP2C9 substrates should be reduced and alternatives be considered for patients requiring higher doses of asciminib.58 In all given clinical scenarios, risks and benefits of asciminib vs the concomitant medication must be carefully weighed.
Factors Influencing Pediatric Patient Selection
Although many oncologists have adopted treatment guidelines for adults to utilize in the pediatric population due to a paucity of pediatric-specific guidelines, there are patient factors of greater significance to consider in this population.42 Imatinib, dasatinib, and nilotinib are the only currently approved TKIs for children for the treatment of CML.42 Roughly 30% of 1L pediatric patients with CML treated with imatinib experienced unsatisfactory response or intolerance.87,111 CVEs have not been observed in studies of nilotinib in pediatric patients. However, cumulative MMR rates are lower in patients with prior resistance to or intolerance of imatinib or dasatinib.87,112 Therefore, as with adults, molecular response rates are lower with subsequent lines of therapy.20 This, in addition to fewer available treatment options in the pediatric population compared with adults, underscores the importance of pediatric patient selection for TKIs.42,87 Furthermore, there are some overlapping and distinct treatment goals and considerations for treatment selection for pediatric patients.
The goals of CML treatment in pediatric patients are similar to those in adults and include remission, improving survival, and preventing disease progression.42 However, unlike adults, pediatric patients are expected to, in theory, have more years in treatment, exposing them to an increased risk of long-term health consequences.88 A potential need for lifelong therapy also makes certain factors more important such as tolerability and ease of administration to support adherence.6
Nonadherence is common in teenagers and often increases after a favorable response to TKI therapy has been obtained during the first year.52 Increased risk-taking behaviors in adolescence may also make adherence difficult.6 The QD with food drug schedule for imatinib and with/without food with dasatinib can make these treatments easier to adhere to.6,113,114 Nilotinib is given on a BID schedule with avoidance of food recommended 2 hours before and 1 hour after each dose. Such restrictions may be difficult for teenagers and young children to adhere to.6,101 This experience is important to consider when evaluating asciminib as a future treatment option as BID dosing under food restrictions mirrors the adult formulation of asciminib. Therefore, ASC4KIDS (NCT04925479) is evaluating the food-restrictive adult formulation in patients at study entry against a pediatric formulation of mini-tablets taken with food. This study is also evaluating a QD dosing schedule for asciminib in the pediatric population, which would simplify administration.73 If approved, this new formulation may improve adherence in pediatric patients with CML-CP who are prescribed asciminib.
In addition, adherence and QOL are greatly influenced by toxicities. Currently approved ATP-competitive TKIs target BCR::ABL1, but their nonspecific activity may influence other signaling pathways affecting bone development.90 Children with CML are prescribed TKIs during an active phase of growth, and growth retardation has been reported with approved ATP-competitive TKIs in pediatric patients.90 Hypothyroidism and pubertal delay may also occur as demonstrated in pediatric CML literature.52 The specificity and unique mechanism of action of asciminib has been shown to demonstrate fewer off-target effects, making it a promising candidate for treating CML in pediatric patients where minimizing toxicity is particularly important given longer expected duration of exposure.17,52
Prior to use of TKIs for the treatment of pediatric CML, HSCT was the only treatment option offering the possibility of cure. Effectiveness of TKIs in treating pediatric CML has limited indications for HSCT.6,52 Although children with CML-CP fare better with HSCT than adults, early morbidities and mortality associated with the procedure make TKIs preferred.6,52 As more therapeutic options become available to pediatric patients with CML, with potentially greater ability to facilitate TFR, indications for HSCT should continue to become more limited.
Conclusions
Although TKIs have greatly improved QOL and outcomes for those with CML, many unmet needs remain.11–13,26,115 Resistance and intolerance remain significant issues with current approved ATP-competitive TKIs.11,12,19,102 Limited treatment options for patients with CML harboring the T315I mutation and the prospect of long-term toxicity in pediatric patients also present distinct challenges.20,42,88 With approval of asciminib for later-line therapy, physicians are seeking guidance on how to incorporate this new option into their treatment decision-making process and how to select patients for treatment. Clinical data from X2101 and ASCEMBL demonstrated that asciminib is highly effective for patients who received ≥2 prior TKIs and for patients with T315I-mutated CML and has potential safety advantages over other standard of care treatment options.56,58,59 These data show that asciminib has broad applicability for patients who have received ≥2 prior TKIs and may need alternatives. Longer-term follow-up of these trials along with ongoing trials of asciminib monotherapy (eg, ASC4FIRST, ASC4START, ASC2ESCALATE) or combination therapy (eg, FASCINATION) in earlier lines and in pediatric patients (ASC4KIDS) will further elucidate the clinical efficacy and safety profile of asciminib in patients with CML.73,74,78–80,82
Acknowledgments
Medical writing support was provided by Christopher DiMaio, MD (Nucleus Global, Inc) and was funded by Novartis Pharmaceuticals Corporation. This manuscript was developed in accordance with Good Publication Practice (GPP3) guidelines. Authors had full control of the content and made the final decision on all aspects of this publication.
Author Contributions
MJM and NH were involved in the conception of the initial draft of this manuscript, substantially revised and critically reviewed the manuscript, made the decision to submit it for publication, agreed on the journal to which the article will be submitted, and contributed to subsequent drafts. All authors agree to take responsibility and be accountable for the contents of this article.
Funding
This manuscript was sponsored by Novartis Pharmaceuticals Corporation. Financial support for medical editorial assistance was also provided by Novartis. The sponsor was not involved in the writing of this review.
Disclosure
NH reports consultancy or an advisory role for Stemline Therapeutics; honoraria from Incyte and Stemline Therapeutics; and research funding from Pfizer and Novartis. MJM reports consultancy for Novartis, Bristol Myers Squibb, Takeda, Pfizer, Sun Pharma/SPARC, and Abbvie; honoraria from Novartis, Bristol Myers Squibb, Takeda, and Pfizer; and research funding from Novartis, Bristol Myers Squibb, Takeda, and Sun Pharma/SPARC. The authors report no other conflicts of interest in this work.
References
1. Minciacchi VR, Kumar R, Krause DS. Chronic myeloid leukemia: a model disease of the past, present and future. Cells. 2021;10:117. doi:10.3390/cells10010117
2. Santos FP, Kantarjian H, Quintás-Cardama A, Cortes J. Evolution of therapies for chronic myelogenous leukemia. Cancer J. 2011;17:465–476. doi:10.1097/PPO.0b013e31823dec8d
3. Isfort S, Brümmendorf TH. Bosutinib in chronic myeloid leukemia: patient selection and perspectives. J Blood Med. 2018;9:43–50. doi:10.2147/JBM.S129821
4. Sasaki K, Strom SS, O’Brien S, et al. Relative survival in patients with chronic-phase chronic myeloid leukaemia in the tyrosine-kinase inhibitor era: analysis of patient data from six prospective clinical trials. Lancet Haematol. 2015;2:e186–e193. doi:10.1016/S2352-3026(15)00048-4
5. Bower H, Björkholm M, Dickman PW, Höglund M, Lambert PC, Andersson TM. Life expectancy of patients with chronic myeloid leukemia approaches the life expectancy of the general population. J Clin Oncol. 2016;34:2851–2857. doi:10.1200/JCO.2015.66.2866
6. Hijiya N, Suttorp M. How I treat chronic myeloid leukemia in children and adolescents. Blood. 2019;133:2374–2384. doi:10.1182/blood.2018882233
7. Atallah E, Sweet K. Treatment-free remission: the new goal in CML therapy. Curr Hematol Malig Rep. 2021;16:433–439. doi:10.1007/s11899-021-00653-1
8. Ciftciler R, Haznedaroglu IC. Tailored tyrosine kinase inhibitor (TKI) treatment of chronic myeloid leukemia (CML) based on current evidence. Eur Rev Med Pharmacol Sci. 2021;25:7787–7798. doi:10.26355/eurrev_202112_27625
9. Castagnetti F, Binotto G, Capodanno I, et al. Making treatment-free remission (TFR) easier in chronic myeloid leukemia: fact-checking and practical management tools. Target Oncol. 2021;16:823–838. doi:10.1007/s11523-021-00831-4
10. Hochhaus A, Gambacorti-Passerini C, Abboud C, et al. Bosutinib for pretreated patients with chronic phase chronic myeloid leukemia: primary results of the Phase 4 BYOND study. Leukemia. 2020;34:2125–2137. doi:10.1038/s41375-020-0915-9
11. Shah NP, Rousselot P, Schiffer C, et al. Dasatinib in imatinib-resistant or -intolerant chronic-phase, chronic myeloid leukemia patients: 7-year follow-up of study CA180-034. Am J Hematol. 2016;91:869–874. doi:10.1002/ajh.24423
12. Hochhaus A, Larson RA, Guilhot F, et al. Long-term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med. 2017;376:917–927. doi:10.1056/NEJMoa1609324
13. Cortes JE, Saglio G, Kantarjian HM, et al. Final 5-year study results of DASISION: the dasatinib versus imatinib study in treatment-naive chronic myeloid leukemia patients trial. J Clin Oncol. 2016;34:2333–2340. doi:10.1200/JCO.2015.64.8899
14. Hochhaus A, Rosti G, Cross NC, et al. Frontline nilotinib in patients with chronic myeloid leukemia in chronic phase: results from the European ENEST1st study. Leukemia. 2016;30:57–64. doi:10.1038/leu.2015.270
15. Deeks ED. Asciminib: first approval. Drugs. 2022;82:219–226. doi:10.1007/s40265-021-01662-3
16. Asciminib moves toward EU approval for Ph+ CML in chronic phase. Available from: https://www.onclive.com/view/asciminib-moves-toward-eu-approval-for-ph-cml-in-chronic-phase.
17. Manley PW, Barys L, Cowan-Jacob SW. The specificity of asciminib, a potential treatment for chronic myeloid leukemia, as a myristate-pocket binding ABL inhibitor and analysis of its interactions with mutant forms of BCR-ABL1 kinase. Leuk Res. 2020;98:106458. doi:10.1016/j.leukres.2020.106458
18. Kantarjian HM, Hughes TP, Larson RA, et al. Correction to: long-term outcomes with frontline nilotinib versus imatinib in newly diagnosed chronic myeloid leukemia in chronic phase: ENESTnd 10-year analysis. Leukemia. 2021;35:2142–2143. doi:10.1038/s41375-021-01306-1
19. Cortes JE, Kim DW, Pinilla-Ibarz J, et al. Ponatinib efficacy and safety in Philadelphia chromosome-positive leukemia: final 5-year results of the phase 2 PACE trial. Blood. 2018;132:393–404. doi:10.1182/blood-2016-09-739086
20. Cortes J, Lang F. Third-line therapy for chronic myeloid leukemia: current status and future directions. J Hematol Oncol. 2021;14:44. doi:10.1186/s13045-021-01055-9
21. Bosi GR, Fogliatto LM, Costa TE, et al. What happens to intolerant, relapsed or refractory chronic myeloid leukemia patients without access to clinical trials? Hematol Transfus Cell Ther. 2019;41:222–228. doi:10.1016/j.htct.2018.11.005
22. Loscocco F, Visani G, Galimberti S, Curti A, Isidori A. BCR-ABL independent mechanisms of resistance in chronic myeloid leukemia. Front Oncol. 2019;9:939. doi:10.3389/fonc.2019.00939
23. Bhamidipati PK, Kantarjian H, Cortes J, Cornelison AM, Jabbour E. Management of imatinib-resistant patients with chronic myeloid leukemia. Ther Adv Hematol. 2013;4:103–117. doi:10.1177/2040620712468289
24. Shah NP. Medical management of CML. Hematology Am Soc Hematol Educ Program. 2007;:371–375. doi:10.1182/asheducation-2007.1.371
25. Druker BJ, Guilhot F, O’Brien SG, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355:2408–2417. doi:10.1056/NEJMoa062867
26. Hochhaus A, Saglio G, Hughes TP, et al. Long-term benefits and risks of frontline nilotinib vs imatinib for chronic myeloid leukemia in chronic phase: 5-year update of the randomized ENESTnd trial. Leukemia. 2016;30:1044–1054. doi:10.1038/leu.2016.5
27. Brümmendorf TH, Cortes JE, Milojkovic D, et al. Bosutinib (BOS) versus imatinib for newly diagnosed chronic phase (CP) chronic myeloid leukemia (CML): final 5-year results from the BFORE trial. Blood. 2020;136:41–42. doi:10.1182/blood-2020-137393
28. Jabbour E, Parikh SA, Kantarjian H, Cortes J. Chronic myeloid leukemia: mechanisms of resistance and treatment. Hematol Oncol Clin North Am. 2011;25:981–995. doi:10.1016/j.hoc.2011.09.004
29. Zhang WW, Cortes JE, Yao H, et al. Predictors of primary imatinib resistance in chronic myelogenous leukemia are distinct from those in secondary imatinib resistance. J Clin Oncol. 2009;27:3642–3649. doi:10.1200/JCO.2008.19.4076
30. Patel AB, O’Hare T, Deininger MW. Mechanisms of resistance to ABL kinase inhibition in chronic myeloid leukemia and the development of next generation ABL kinase inhibitors. Hematol Oncol Clin North Am. 2017;31:589–612. doi:10.1016/j.hoc.2017.04.007
31. Alves R, Gonçalves AC, Rutella S, et al. Resistance to tyrosine kinase inhibitors in chronic myeloid leukemia-from molecular mechanisms to clinical relevance. Cancers (Basel). 2021;13:4820. doi:10.3390/cancers13194820
32. Soverini S, Branford S, Nicolini FE, et al. Implications of BCR-ABL1 kinase domain-mediated resistance in chronic myeloid leukemia. Leuk Res. 2014;38:10–20. doi:10.1016/j.leukres.2013.09.011
33. Brümmendorf TH, Cortes JE, Milojkovic D, et al. Bosutinib versus imatinib for newly diagnosed chronic phase chronic myeloid leukemia: final results from the BFORE trial. Leukemia. 2022;36:1825–1833. doi:10.1038/s41375-022-01589-y
34. Liu J, Yang H, Xu X, Yi S, Meng L. Mutations in the BCR-ABL1 kinase domain in patients with chronic myeloid leukaemia treated with TKIs or at diagnosis. Oncol Lett. 2020;20:1071–1076. doi:10.3892/ol.2020.11650
35. Dhillon S. Olverembatinib: first approval. Drugs. 2022;82:469–475. doi:10.1007/s40265-022-01680-9
36. Jiang Q, Li Z, Qin Y, et al. Olverembatinib (HQP1351), a well-tolerated and effective tyrosine kinase inhibitor for patients with T315I-mutated chronic myeloid leukemia: results of an open-label, multicenter phase 1/2 trial. J Hematol Oncol. 2022;15:113. doi:10.1186/s13045-022-01334-z
37. Hehlmann R, Cortes JE, Zyczynski T, et al. Tyrosine kinase inhibitor interruptions, discontinuations and switching in patients with chronic-phase chronic myeloid leukemia in routine clinical practice: SIMPLICITY. Am J Hematol. 2019;94:46–54. doi:10.1002/ajh.25306
38. Efficace F, Cannella L. The value of quality of life assessment in chronic myeloid leukemia patients receiving tyrosine kinase inhibitors. Hematology Am Soc Hematol Educ Program. 2016;2016:170–179. doi:10.1182/asheducation-2016.1.170
39. Steegmann JL, Baccarani M, Breccia M, et al. European LeukemiaNet recommendations for the management and avoidance of adverse events of treatment in chronic myeloid leukaemia. Leukemia. 2016;30:1648–1671. doi:10.1038/leu.2016.104
40. Mohanavelu P, Mutnick M, Mehra N, et al. Meta-analysis of gastrointestinal adverse events from tyrosine kinase inhibitors for chronic myeloid leukemia. Cancers (Basel). 2021;13:1643. doi:10.3390/cancers13071643
41. Cirmi S, El Abd A, Letinier L, Navarra M, Salvo F. Cardiovascular toxicity of tyrosine kinase inhibitors used in chronic myeloid leukemia: an analysis of the FDA Adverse Event Reporting System Database (FAERS). Cancers (Basel). 2020;12:826. doi:10.3390/cancers12040826
42. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Chronic Myeloid Leukemia. V1; 2023.
43. Giles FJ, le Coutre PD, Pinilla-Ibarz J, et al. Nilotinib in imatinib-resistant or imatinib-intolerant patients with chronic myeloid leukemia in chronic phase: 48-month follow-up results of a phase II study. Leukemia. 2013;27:107–112. doi:10.1038/leu.2012.181
44. Cortes J, Brümmendorf TH, Goh YT, et al. Bosutinib for chronic phase chronic myeloid leukemia after imatinib failure: >8-year update of a phase 1/2 study.
45. Cortes J, Apperley J, Lomaia E, et al. Ponatinib dose-ranging study in chronic-phase chronic myeloid leukemia: a randomized, open-label phase 2 clinical trial. Blood. 2021;138:2042–2050. doi:10.1182/blood.2021012082
46. Hochhaus A, Baccarani M, Silver RT, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34:966–984. doi:10.1038/s41375-020-0776-2
47. Gambacorti-Passerini C, Brümmendorf TH, Kim DW, et al. Bosutinib efficacy and safety in chronic phase chronic myeloid leukemia after imatinib resistance or intolerance: minimum 24-month follow-up. Am J Hematol. 2014;89:732–742. doi:10.1002/ajh.23728
48. Shah NP, Kim DW, Kantarjian H, et al. Potent, transient inhibition of BCR-ABL with dasatinib 100 mg daily achieves rapid and durable cytogenetic responses and high transformation-free survival rates in chronic phase chronic myeloid leukemia patients with resistance, suboptimal response or intolerance to imatinib. Haematologica. 2010;95:232–240. doi:10.3324/haematol.2009.011452
49. Kantarjian HM, Giles FJ, Bhalla KN, et al. Nilotinib is effective in patients with chronic myeloid leukemia in chronic phase after imatinib resistance or intolerance: 24-month follow-up results. Blood. 2011;117:1141–1145. doi:10.1182/blood-2010-03-277152
50. Carofiglio F, Lopalco A, Lopedota A, et al. Bcr-Abl tyrosine kinase inhibitors in the treatment of pediatric CML. Int J Mol Sci. 2020;21:4469. doi:10.3390/ijms21124469
51. ClinicalTrials.gov. Safety and efficacy of ponatinib for treatment of pediatric recurrent or refractory leukemias, lymphomas or solid tumors. Available from: https://ClinicalTrials.gov/show/NCT03934372.
52. Athale U, Hijiya N, Patterson BC, et al. Management of chronic myeloid leukemia in children and adolescents: recommendations from the Children’s Oncology Group CML Working Group. Pediatr Blood Cancer. 2019;66:e27827. doi:10.1002/pbc.27827
53. Schoepfer J, Jahnke W, Berellini G, et al. Discovery of asciminib (ABL001), an allosteric inhibitor of the tyrosine kinase activity of BCR-ABL1. J Med Chem. 2018;61:8120–8135. doi:10.1021/acs.jmedchem.8b01040
54. Colicelli J. ABL tyrosine kinases: evolution of function, regulation, and specificity. Sci Signal. 2010;3:re6. doi:10.1126/scisignal.3139re6
55. Hantschel O. Structure, regulation, signaling, and targeting of abl kinases in cancer. Genes Cancer. 2012;3:436–446. doi:10.1177/1947601912458584
56. Hughes TP, Mauro MJ, Cortes JE, et al. Asciminib in chronic myeloid leukemia after ABL kinase inhibitor failure. N Engl J Med. 2019;381:2315–2326. doi:10.1056/NEJMoa1902328
57. Hoch M, Sengupta T, Hourcade-Potelleret F. Pharmacokinetic drug interactions of asciminib with the sensitive cytochrome P450 probe substrates midazolam, warfarin, and repaglinide in healthy participants. Clin Transl Sci. 2022;15:1406–1416. doi:10.1111/cts.13252
58. SCEMBLIX (asciminib). Prescribing information. Novartis; 2021.
59. Rea D, Mauro MJ, Boquimpani C, et al. A phase 3, open-label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs. Blood. 2021;138:2031–2041. doi:10.1182/blood.2020009984
60. Hughes T, Mauro MJ, Kim D, et al. Asciminib in heavily pretreated patients (pts) with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia in chronic phase (CML-CP) sensitive to tyrosine kinase inhibitor (TKI) therapy.
61. Mauro MJ, Hughes T, Kim D, et al. Asciminib monotherapy in patients with CML-CP without BCR::ABL1 T315I mutations treated with at least two prior TKIs: 4-year phase 1 safety and efficacy results. Leukemia. 2023;37:1048–1059. doi:10.1038/s41375-023-01860-w
62. Hughes T, Cortes J, Rea D, et al. Asciminib provides durable molecular responses in patients with chronic myeloid leukemia in chronic phase (CML-CP) with the T315I mutation: updated efficacy and safety data from a phase I trial.
63. Hochhaus A, Rea D, Boquimpani C, et al. Asciminib vs bosutinib in chronic-phase chronic myeloid leukemia previously treated with at least two tyrosine kinase inhibitors: longer-term follow-up of ASCEMBL. Leukemia. 2023;37(3):617–626. doi:10.1038/s41375-023-01829-9
64. ClinicalTrials.gov. Study of efficacy of CML-CP patients treated with ABL001 versus bosutinib, previously treated with 2 or more TKIs. Available from: https://ClinicalTrials.gov/show/NCT03106779.
65. Rea D, Mauro MJ, Hochhaus A, et al. Efficacy and safety results from ASCEMBL, a phase 3 study of asciminib vs bosutinib in patients with chronic myeloid leukemia in chronic phase after ≥2 prior tyrosine kinase inhibitors: week 96 update.
66. Rea D, Hochhaus A, Mauro MJ, et al. Efficacy and safety results from ASCEMBL, a phase 3 study of asciminib vs bosutinib in patients with chronic myeloid leukemia in chronic phase after ≥2 prior tyrosine kinase inhibitors: week 96 update.
67. Mauro MJ, Boquimpani C, Rea D, et al. CML-417: ASCEMBL phase 3 health-related quality of life (HRQL) comparison of asciminib and bosutinib for patients with chronic myelogenous leukemia in chronic phase (CML-CP), previously treated with 2 or more tyrosine kinase inhibitors (TKI). Clin Lymphoma Myeloma Leuk. 2021;21(Suppl 1):S336. doi:10.1016/S2152-2650(21)01785-7
68. ClinicalTrials.gov. ABL001 for the treatment of chronic myeloid leukemia in patients who are on therapy with tyrosine kinase inhibitor. Available from: https://ClinicalTrials.gov/show/NCT04216563.
69. ClinicalTrials.gov. Asciminib in monotherapy for Chronic Myeloid Leukemia in Chronic Phase (CML-CP) with and without T315I mutation. Available from: https://ClinicalTrials.gov/show/NCT04666259.
70. ClinicalTrials.gov. Study of efficacy and safety of CML-CP patients treated with asciminib versus best available therapy, previously treated with 2 or more tyrosine kinase inhibitors. Available from: https://ClinicalTrials.gov/show/NCT04795427.
71. ClinicalTrials.gov. A phase I study of oral ABL001 in patients with CML or Ph+ ALL. Available from: https://ClinicalTrials.gov/show/NCT02081378.
72. ClinicalTrials.gov. Asciminib treatment optimization in ≥ 3rd line CML-CP. Available from: https://ClinicalTrials.gov/show/NCT04948333.
73. ClinicalTrials.gov. Study to determine the dose and safety of asciminib in pediatric patients with chronic myeloid leukemia. Available from: https://ClinicalTrials.gov/show/NCT04925479.
74. ClinicalTrials.gov. Asciminib monotherapy, with dose escalation, for 2nd line chronic myelogenous leukemia. Available from: https://ClinicalTrials.gov/show/NCT05384587.
75. ClinicalTrials.gov. Study of efficacy and safety of asciminib in combination with imatinib in patients With Chronic Myeloid Leukemia in Chronic Phase (CML-CP). Available from: https://ClinicalTrials.gov/show/NCT03578367.
76. ClinicalTrials.gov. Treatment free remission after combination therapy with asciminib (ABL001) plus imatinib in Chronic Phase Chronic Myeloid Leukemia (CP-CML) patients who relapsed after a prior attempt at TKI discontinuation. Available from: https://ClinicalTrials.gov/show/NCT04838041.
77. ClinicalTrials.gov. Asciminib used in consolidation with imatinib vs. imatinib to achieve TFR in CP-CML. Available from: https://ClinicalTrials.gov/show/NCT05413915.
78. ClinicalTrials.gov. Frontline asciminib combination in chronic phase CML. Available from: https://ClinicalTrials.gov/show/NCT03906292.
79. ClinicalTrials.gov. A study of oral asciminib versus other TKIs in adult patients with newly diagnosed Ph+ CML-CP. Available from: https://ClinicalTrials.gov/show/NCT04971226.
80. ClinicalTrials.gov. A study to investigate tolerability and efficacy of asciminib (oral) versus nilotinib (oral) in adult participants (≥18 years of age) with newly diagnosed Philadelphia chromosome positive chronic myelogenous leukemia in chronic phase (Ph+ CML-CP) (ASC4START). Available from: https://ClinicalTrials.gov/show/NCT05456191.
81. ClinicalTrials.gov. Asciminib as initial therapy for patients with chronic myeloid leukemia in chronic phase. Available from: https://ClinicalTrials.gov/show/NCT05143840.
82. Sasaki K, Mauro M, Levy MY, et al. ASC2ESCALATE: a phase 2, single-arm, dose-escalation study of asciminib monotherapy in patients (Pts) with Chronic Myeloid Leukemia in Chronic Phase (CML-CP) previously treated with 1 prior Tyrosine Kinase Inhibitor (TKI). Blood. 2022;140(1):6784–6786. doi:10.1182/blood-2022-167044
83. Mu H, Zhu X, Jia H, et al. Combination therapies in chronic myeloid leukemia for potential treatment-free remission: focus on leukemia stem cells and immune modulation. Front Oncol. 2021;11:643382. doi:10.3389/fonc.2021.643382
84. Eide CA, Zabriskie MS, Savage Stevens SL, et al. Combining the allosteric inhibitor asciminib with ponatinib suppresses emergence of and restores efficacy against highly resistant BCR-ABL1 mutants. Cancer Cell. 2019;36:431–443.e5. doi:10.1016/j.ccell.2019.08.004
85. Lindström HJG, Friedman R. The effects of combination treatments on drug resistance in chronic myeloid leukaemia: an evaluation of the tyrosine kinase inhibitors axitinib and asciminib. BMC Cancer. 2020;20:397. doi:10.1186/s12885-020-06782-9
86. Cortes J, Lang F, Kim D, et al. Combination therapy using asciminib plus imatinib (IMA) in patients (pts) with chronic myeloid leukemia (CML): results from a phase 1 study.
87. Hijiya N, Maschan A, Rizzari C, et al. Phase 2 study of nilotinib in pediatric patients with Philadelphia chromosome-positive chronic myeloid leukemia. Blood. 2019;134:2036–2045. doi:10.1182/blood.2019000069
88. Hijiya N, Schultz KR, Metzler M, Millot F, Suttorp M. Pediatric chronic myeloid leukemia is a unique disease that requires a different approach. Blood. 2016;127:392–399. doi:10.1182/blood-2015-06-648667
89. Nishiyama-Fujita Y, Nakazato T, Iriyama N, et al. Outcomes of adolescents and young adults with chronic-phase chronic myeloid leukemia treated with tyrosine kinase inhibitors. Ann Med. 2022;54:1244–1254. doi:10.1080/07853890.2022.2069280
90. Ford M, Mauro M, Aftandilian C, Sakamoto KM, Hijiya N. Management of chronic myeloid leukemia in children and young adults. Curr Hematol Malig Rep. 2022;17:121–126. doi:10.1007/s11899-022-00673-5
91. Pemmaraju N, Kantarjian H, Shan J, et al. Analysis of outcomes in adolescents and young adults with chronic myelogenous leukemia treated with upfront tyrosine kinase inhibitor therapy. Haematologica. 2012;97:1029–1035. doi:10.3324/haematol.2011.056721
92. Lipton JH, Bryden P, Sidhu MK, et al. Comparative efficacy of tyrosine kinase inhibitor treatments in the third-line setting, for chronic-phase chronic myelogenous leukemia after failure of second-generation tyrosine kinase inhibitors. Leuk Res. 2015;39:58–64. doi:10.1016/j.leukres.2014.10.005
93. Ono T. Which tyrosine kinase inhibitors should be selected as the first-line treatment for chronic myelogenous leukemia in chronic phase? Cancers (Basel). 2021;13:5116. doi:10.3390/cancers13205116
94. Hughes T, Rea D, Boquimpani C, et al. Dynamics of response and response factors in patients (pts) with chronic myeloid leukemia in chronic phase (CML-CP) after ≥2 prior tyrosine kinase inhibitors (TKIs) in the phase 3 ASCEMBL study. Blood. 2022;140(Suppl 1):6757–6759. doi:10.1182/blood-2022-169110
95. Luna A, Pérez-Lamas L, Boque C, et al. Real-life analysis on safety and efficacy of asciminib for ponatinib pretreated patients with chronic myeloid leukemia. Ann Hematol. 2022;101:2263–2270. doi:10.1007/s00277-022-04932-6
96. Aghel N, Delgado DH, Lipton JH. Cardiovascular toxicities of BCR-ABL tyrosine kinase inhibitors in chronic myeloid leukemia: preventive strategies and cardiovascular surveillance. Vasc Health Risk Manag. 2017;13:293–303. doi:10.2147/VHRM.S108874
97. Baggio D, Tan S, Porch K, Shortt J, Ko B. Prediction of cardiovascular events in patients with chronic myeloid leukaemia using baseline risk factors and coronary artery calcium scoring. Intern Med J. 2021;51:1736–1740. doi:10.1111/imj.15517
98. Cortes J. How to manage CML patients with comorbidities. Hematology Am Soc Hematol Educ Program. 2020;2020:237–242. doi:10.1182/hematology.2020006911
99. Coutinho AD, Makenbaeva D, Farrelly E, Landsman-Blumberg PB, Lenihan D. Elevated cardiovascular disease risk in patients with chronic myelogenous leukemia seen in community-based oncology practices in the United States. Clin Lymphoma Myeloma Leuk. 2017;17(10):676–683. doi:10.1016/j.clml.2017.06.011
100. ICLUSIG (ponatinib). Prescribing information. Takeda; 2022.
101. TASIGNA (nilotinib). Prescribing information. Novartis; 2021.
102. Kantarjian HM, Hughes TP, Larson RA, et al. Long-term outcomes with frontline nilotinib versus imatinib in newly diagnosed chronic myeloid leukemia in chronic phase: ENESTnd 10-year analysis. Leukemia. 2021;35(2):440–453. doi:10.1038/s41375-020-01111-2
103. Lee PM, Chang CT, Yusoff ZM. Adherence to tyrosine kinase inhibitors among adult chronic myeloid leukemia patients in a Malaysia hospital. Int J Clin Pharm. 2021;43:46–54. doi:10.1007/s11096-020-01070-9
104. Tan BK, Bee PC, Chua SS, Chen LC. Monitoring and improving adherence to tyrosine kinase inhibitors in patients with chronic myeloid leukemia: a systematic review. Patient Prefer Adherence. 2021;15:2563–2575. doi:10.2147/PPA.S269355
105. Guerin A, Chen L, Ionescu-Ittu R, et al. Impact of low-grade adverse events on health-related quality of life in adult patients receiving imatinib or nilotinib for newly diagnosed Philadelphia chromosome positive chronic myelogenous leukemia in chronic phase. Curr Med Res Opin. 2014;30(11):2317–2328. doi:10.1185/03007995.2014.944973
106. Saydam G, Ali R, Demir AM, et al. The effect of comorbidities on the choice of tyrosine kinase inhibitors in patients with chronic myeloid leukemia. Int J Hematol Oncol. 2022;11(1):IJH38. doi:10.2217/ijh-2021-0010
107. Jabbour E, Makenbaeva D, Lingohr-Smith M, Lin J. Use of real-world claim databases to assess prevalence of comorbid conditions relevant to the treatment of chronic myelogenous leukemia based on national comprehensive network treatment guidelines. Clin Lymphoma Myeloma Leuk. 2015;15(12):797–802. doi:10.1016/j.clml.2015.09.008
108. Chow EJ, Doody DR, Wilkes JJ, et al. Adverse events among chronic myelogenous leukemia patients treated with tyrosine kinase inhibitors: a real-world analysis of health plan enrollees. Leuk Lymphoma. 2021;62:1203–1210. doi:10.1080/10428194.2020.1855340
109. Cortes J. How to manage CML patients with comorbidities. Blood. 2020;136:2507–2512. doi:10.1182/blood.2020006911
110. Flynn KE, Atallah E. Quality of life and long-term therapy in patients with chronic myeloid leukemia. Curr Hematol Malig Rep. 2016;11:80–85. doi:10.1007/s11899-016-0306-5
111. Suttorp M, Bornhauser M, Metzler M, Millot F, Schleyer E. Pharmacology and pharmacokinetics of imatinib in pediatric patients. Expert Rev Clin Pharmacol. 2018;11(3):219–231. doi:10.1080/17512433.2018.1398644
112. Hijiya N, Maschan A, Rizzari C, et al. A phase 2 study of nilotinib in pediatric patients with CML: long-term update on growth retardation and safety. Blood Adv. 2021;5(14):2925–2934. doi:10.1182/bloodadvances.2020003759
113. SPRYCEL (dasatinib). Prescribing information. Bristol Myers Squibb; 2021.
114. GLEEVAC (imatinib mesylate). Prescribing information. Novartis; 2020.
115. Lipton JH, Brümmendorf TH, Gambacorti-Passerini C, et al. Long-term safety review of tyrosine kinase inhibitors in chronic myeloid leukemia - What to look for when treatment-free remission is not an option. Blood Rev. 2022;56:100968. doi:10.1016/j.blre.2022.100968
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
