Back to Journals » Clinical Ophthalmology » Volume 17
Compared Methods for Reducing Stress in ROP Exams; Stake-Holding Examiner Perspective
Authors Cuddihee LJ, Giannulis P , Merriner S, Runge PE , Pringels V, McGill V, Johnson MA, Cobb LB, Arnold RW
Received 9 May 2023
Accepted for publication 3 July 2023
Published 12 July 2023 Volume 2023:17 Pages 1953—1965
DOI https://doi.org/10.2147/OPTH.S418150
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Supplementary video of "Care-giver sensation of ROP examination stress" [ID 418150].
Views: 107
Laney J Cuddihee,1 Peter Giannulis,1 Sarah Merriner,1 Paul E Runge,2 Victoria Pringels,3 Virginia McGill,3 Mary-Alice Johnson,3 Lindsey B Cobb,4 Robert W Arnold1
1Alaska Blind Child Discovery, Alaska Children’s EYE & Strabismus, Anchorage, AK, USA; 2International Retinal Consultant, Lakewood Ranch, FL, USA; 3Neonatal Intensive Care Unit, Providence Alaska Medical Center, Anchorage, AK, USA; 4Anesthesiology Department, Central Peninsula Hospital, Soldotna, AK, USA
Correspondence: Robert W Arnold, Alaska Blind Child Discovery, Alaska Children’s EYE & Strabismus, 3500 Latouche #280, Anchorage, AK, 99508, USA, Tel +1(907)561-1917, Fax +1(907)563-5373, Email [email protected]
Purpose: To better understand the sensory impact of retinal exam components typically experienced by infants undergoing various retinopathy of prematurity staging examinations, adults concerned for infant welfare and exam quality underwent similar exams to compare their perceived stress.
Patients and Methods: Adults directly involved with ROP exams and infant stress reduction had cardiac monitoring and concomitant ordinal self symptom-score (1– 10 Likert) during 15 components of the exam including lid speculum, various scleral depressors, indirect ophthalmoscopy, goniolens and direct ophthalmoscopy and retinal photography (Phoenix ICON) with or without topical anesthesia.
Results: Nine adults provided impressions and cardiac rhythm gathered supine over 15 minutes. Pain score for topical anesthetic 2 was less than for tropicamide 4. Lid specula numb scored a median 2 level (from 1 to 10) pain but without anesthetic scored 6. The goniolens numb scored 3. Scleral depression numb scored 3– 4 but increased to 7 without topical anesthesia. Direct ophthalmoscope scored 3 through the goniolens and the retinal camera scored 4 pain. Brightness with low 350 Lux indirect scored 6– 8 numb and 9 brightness without anesthetic. Full bright indirect, direct ophthalmoscope and the retinal camera all had Lux of 3000– 4000 and were scored brightness 9, 7 and 10, respectively. Adults had minimal oculocardiac reflex during on-globe retinal examination methods (range 98% to 102%).
Conclusion: Topical anesthesia provided a moderate reduction in pain during on-globe lid-speculum, scleral depressed indirect examination. There was a synergistic augmented sensory response between pain and brightness. Adults did not show the bradycardia typically elicited by retinal examinations in premature infants.
Keywords: retinopathy of prematurity, infant pain, bradycardia, scleral depression, imaging
Plain Language Summary
Nine NICU caregivers scored pain and brightness during 15 components typical for infant ROP staging examinations finding more pain if topical anesthesia withheld and elements of synergistic pain and brightness.
Introduction
There are different methods for staging examinations of the retina in patients screened and referred by their neonatologist for retinopathy of prematurity (ROP). Indirect ophthalmoscopy with lid speculum and scleral depression all the way anterior to the ora serrata is used by many ophthalmologists for retinal examination and also for peripherally ablative laser therapy. Abbreviated scleral depression may show portions of the retina consistent with diagnosis of threshold for therapy.1 Prior to widespread use of indirect ophthalmoscopy (before 1975), an infant contact lens and direct ophthalmoscopy were routinely used to afford a magnified, monocular, vertical image to the mid-periphery. Modern widefield, contact cameras can give a supine, in-NICU image to the mid periphery of the infant retina.2 The table-top, ultra-widefield, non-mydriatic camera can give a 200 degree retinal view in cooperative infants able to be held vertically.2 The relative pain and stress of each of these methods has not been directly compared, especially in adults.
There are similarities in techniques for retinal examination between adults and infants, for instance the same indirect ophthalmoscope and condensing lens are used independent of age. However, there are also remarkable differences between infant and adult eye examinations. Scleral depression on cooperative adults is usually done without a lid speculum and with the depressor on the external surface of the eyelids. In contrast, scleral depression of NICU infants is usually done with a lid speculum and with the depressor inside the eyelids and directly on the eyeball. Adults can usually deliberately direct their gaze so different quadrants can be viewed while an infant usually requires instrument redirection of the globe. The adult eye is often longer than 22 mm while the premature infant eye may be less than 18 mm.
Lid specula and scleral depressors have been fashioned to adapt to smaller infant eye configuration out of paper clips, cataract lens irrigating vectis or other similar tools or custom generated for small eyes.3–8 Gonioscopic lenses similar in shape to the Koeppe lens were modified to fit infant eyes by Shaeffer and Richardson and Leyden and can allow a view of the mid-periphery with direct ophthalmoscope.9,10
Pain and stress in premature infants is often quantified with measures like the Premature Infant Pain Profile (PIPP), which is calculated from heart rate, oxygen saturation and facial actions.11 Pain in most aspects of an infant’s body produces tachycardia whereas lid-speculum scleral depression in premature infants often produces bradycardia.12 Therefore, pain scales associated with an ROP examination may have altered meaning and yielded limited precision. To improve precision in infants, additional measures of autonomic nervous activity such as skin conduction may also be monitored.13 The briskness of facial expression with exposure to bright light is used to determine visual acuity in alert, premature infants.14 Alert adults, on the other hand, can give reliable, self-determined Likert score levels for various sensory stimuli including discriminating between pain and brightness.
For more than two decades, pain during ROP staging exams has been noted with encouragement of further study to reduce stress.15 Kara et al compared Premature Infant Pain Profile with topical dilating drops for follow-up outpatient retinal exams in infants noting no difference compared to controls but gradually decreasing scores with repeat administration in both groups.16 Topical tropicamide plus neosynephrine produced a moderate increase in PIPP.17 In some situations, topical anesthetic and oral sucrose did not improve PIPP during staging ROP exams.18 However, through meta analysis, multisensory modalities like topical anesthetic, oral sweet liquid and non-nutritive sucking may have the most pain reduction impact during ROP exams.19,20 In a single-blind study, topical proparacaine 0.5% reduced PIPP during ROP staging exams in 22 premature patients.21 Oral paracetamol modestly reduced PIPP during ROP exams.22 Handheld Optical Coherence Tomography has less stress than indirect ophthalmoscopy for ROP examination.23 Avoiding lid speculum and globe indentation has been recommended to reduce stress.24 Avoiding routine scleral depression reduced PIPP and Bernese Pain Scale if quick speculum-free exams did not suggest “severe” ROP for which speculum and scleral depress was presumed diagnostically better.25 Exam to zone 3 was improved with scleral indent.1
Non-pharmacologic methods have been used to reduce pain in ROP exams. In a review, both oral glucose and sucrose helped, but breast milk did not reduce Premature Infant Pain Profile,26,27 but any of these may be considered insufficient to satisfactorily reduce substantial pain with exams.28 Others found breast milk helpful before ROP exam stress.29 Breast milk may be more soothing than oral sucrose.27 Positioning the infant in Reverse Kangaroo Mother Care reduced stress for infants and mothers during ROP exams.30 Gentle touch during exams can be helpful.31
Randomly prescribed 0.5% proparacaine marginally decreased infant pain scores from 65% to 27% at the time during ROP exams.32 Topical anesthesia for ROP treatments resulted in more cardiorespiratory instability but general fentanyl anesthesia had cases difficult to wean off the ventilator up to 24 hours after surgery.33 Topical proparacaine 0.5% and oral sucrose had similar Premature Infant Pain Profile scores 15.5±2.6 and then 14±2.4 proparacaine versus 14.2 ± 1.8 and 14.9 ± 2.5 (p = 0.48).18 Oral sucrose and withholding feeds had no benefit, whereas pacifier and nesting helped exam comfort the worst of which was lid speculum, and topical anesthesia had marginal benefit.34 Younger infants (31 weeks) had brief benefit from topical anesthesia during eye exams.35
Topical anesthesia after strabismus surgery had either no impact, or a worsening in young children undergoing strabismus surgery.36
From one NICU to another, protocols regarding ROP examinations, photography, type of scleral depressors and use of topical anesthetics are not uniform. It is not clear whether topical anesthetic favorably influences the ROP exam in all situations. Adding topical anesthesia to each ROP eye exams adds time, cost and complexity to the process. However, if adult examiners agree that proparacaine were proven better for them, then protocols for infant eye exams in the NICU would have more precise evidence, and therefore may be encouraged, funded and adopted.
Methods
This comparison of clinical diagnostic tests had institutional review board approval from WCG IRB (Study number 1345195) and complies with the Declaration of Helsinki. All participants gave written consent for the study and images and were invited to become co-authors. Inclusion criteria were adults with interest in infant ROP exam comfort while exclusions were cardiac arrythmias, retinal detachment, enucleation or exenteration, pregnancy or allergy to topical anesthetic or dilating drops.
Each subject was reminded the Likert score responses from 1 to 10 and was examined after eating a meal in an evening between February and March 2023. One drop of tropicamide 1% was instilled to dilate each eye at least 30 minutes before the remainder of data collection (designated “T”). Each subject was supine in a reclining eye exam chair. A small, portable, Blue-Tooth adhesive electrocardiac monitor (VivaLNK, Campbell, California) was placed in the mid-sternal area according to manufacturer guidelines and the real-time cardiac activity was transmitted to an iPhone or iPad (Apple Computer, Cupertino, CA). All eye examinations were performed by experienced ophthalmologists (PER and RWA). The brightness of the examination equipment was monitored with a Dr.Meter photometer. Figure 1 shows many of the instruments used for the various eye exam methods. A Video of the retinal examination process can be viewed.
 |
Figure 1 Instrumentation for various methods of ROP examinations. |
For each of the designated exam methods, time, heart rate before, heart rate during and also pain level (1–10) and brightness level (1–10) were recorded. One drop of proparacaine 0.5% (designated P) was placed in the right eye. An Alfonso lid speculum (Storz E4112) was placed in the numbed (n) right eye (designated An). The indirect ophthalmoscope (Heine Omega 500 CE) was set at ¼ knob-turn (350 Lux by Dr.Meter model LX1330B at the level of the eye under the 20 diopter condensing lens). The right eye was then rotated and indented directly on the bulbar conjunctival surface for indirect retinal exam with the See-Through scleral depressor (designated CTn).37 Then the same right eye was rotated and indented with the metal Runge scleral depressor (designated Rn).3 Then the Heine indirect was set at full brightness (4000 lux) and the right, numb eye was rotated and indented with the See-Through scleral depressor (CTFB). The Alfonso lid speculum was then removed from the right eye and the Heine indirect was returned to 350 lux for the remainder of testing.
The left eye acted as control and received no topical anesthetic so was still feeling (f). The Alfonso lid speculum was then placed in the left eye (designated Af). The left eye was then rotated and indented for exam with the See-Through scleral depressor (designated CTf). Then, the left eye was rotated and indented with the metal Runge scleral depressor (designated Rf). Then, the Alfonso lid speculum was removed from the left eye.
A Moria wire lid speculum (Moria ROP exam kit W/WS-L reference#17257X10, Anton France) was placed in the right eye (M). The right eye was then examined with the globe rotated and indented with the accompanying Moria lens vectis-style scleral depressor (designated MSd). Then the right eye was examined with rotation and indenting by the Runge 3D-printed plastic scleral depressor (MRp). The Moria speculum was then removed.
One additional drop of proparacaine 0.5% was placed in the right eye. A Koeppe gonioscopy lens was placed in the numb right eye (designated Gn). Artificial tear solution was irrigated to remove bubbles. Then the mid-periphery of the right eye was examined with a Welch Allyn 3.5-V direct ophthalmoscope (model 11720) on 3000 lux on full brightness (designated GD). The Koeppe lens was then removed.
The Phoenix ICON Go portable camera was set up according to manufacturer guidelines. The settings were default and not specifically for dark fundi, and white balance was calibrated. The right eye had the Alfonso lid speculum placed. Clear hydroxypropyl methylcellulose gel (Hypromellose) was placed on the right cornea. Then the Phoenix ICON Go (gain 6.0, intensity 5.5) was used to visualize the posterior pole and mid-periphery on the right eye (designated Ph). The Alfonso lid speculum was then removed to complete eye exam data collection. Each subject then had the ViviLNK monitor removed from the chest. Then two other common pain experiences between subjects were assessed to determine uniformity. Pain level with VivaLNK removal was queried. Each subject also then estimated the pain level of a “Brain Freeze” when cold liquid like a milk shake was ingested too quickly.
A sample size estimate was made assuming normal distribution of perceived levels of pain or brightness with a standard deviation of 2, and alpha of 0.5 and a beta of 0.8, to detect a true difference of 2 it would require a sample size of 9.
Results
Nine adult subjects aged 23–77 completed all 15 aspects of the retinal examinations. There were 3 premedical students, one occupational therapist, one physical therapist, one neonatologist, one pediatric anesthesiologist, one pediatric ophthalmologist and one retinal specialist. Raw data can be accessed here: https://www.abcd-vision.org/references/ROP-Stress-DeID.pdf
Table 1 shows each ROP exam method or component and their abbreviations in the order they were performed with the actual mean and standard deviation time in minutes from the initial instilling of a numbing drop in the right eye, with the time following dilation of each eye. Table 1 also gives grouped data on oculocardiac reflex (OCR) as a percent of the pre-maneuver heart rate, and medial plus intra-quartile range for perceived pain scores and brightness scores. None of our adults had heart rate change reaching a common definition of oculocardiac reflex as a 20% heart rate drop.
 |
Table 1 Values for 15 ROP Exam Components |
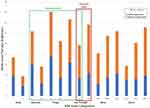
Figure 2 gives distributions of pain scores for all nine subjects and Figure 3 gives Brightness scores (photo).
 |
Figure 2 Pain score distributions for various ROP exam methods. |
 |
Figure 3 Brightness score distributions for various ROP exam methods in 9 adults. |
Each of 15 ROP exam method groups of data for the 9 subjects was subjected to Shapiro–Wilk test and the consistent trend was normal distribution. As such, pain scores, brightness scores and oculocardiac were compared using t-Test and ANOVA. Figure 4 presents a table of comparison between all 15 aspects of examinations studied with t-Test scores and levels of probability for perceived pain and brightness scores for all subjects. The individual aspects are ranked by increasing pain scores in rows and increasing brightness scores in columns.
The oculocardiac reflex defined as the exam heart rate with greatest change divided by the pre-heart rate ranged from 99% for Moria lid speculum insertion numb to 102% for direct exam through the gonio lens numb and insertion of the Alfonso lid speculum without topical anesthesia. The average OCR did not vary across the 15 exam methods (F(14120) = 1.39, p = 0.17). The distribution of oculocardiac reflex for all nine subjects and all 15 maneuvers is shown in Figure 5.
 |
Figure 5 Oculocardiac reflex (exam heart rate/pre-exam heart rate) distributions for various exam methods in 9 adults. |
Tropicamide 1% was used in the study while Cyclomydril is typically used in premature infants. To estimate comparability of these drops, on a subsequent day, three subjects separately scored comfort level for tropicamide in one eye 3, 4, and 4 while Cyclomydril in the other eye 2, 2 and 3. All 9 subjects scored tropicamide 1% as 3.6 ± 0.9 pain level.
The Phoenix ICON Go camera after topical anesthetic and Alfonso lid speculum scored pain level 3.7 ± 1.5 and brightness 9.3 ± 1.3 which was similar to numb scleral depression with 4000 LUX indirect ophthalmoscope scored as 4.4 ± 1.4 pain and brightness 9.3 ± 0.7 (p = 0.28 and p = 1.0).
A view to the ora serrata was feasible utilizing the indirect ophthalmoscope and scleral depression (all 4 instruments), but the ora was not visualized with the direct ophthalmoscope or the fundus camera.
With topical anesthetic, all scleral depress methods scored a similar amount of pain (Runge metal 3.2.±1.8, Moria 3.4 ± 1.7, See-Through 3.6 ± 1.1 and Runge Plastic 3.9 ± 1.9) with corresponding Brightness scores when the indirect was at 350 LUX; 7.0 ± 1.7, 8.0 ± 1.2, 6.4 ± 1.4 and 8.1 ± 1.4. See-Through Scleral depressor brightness 8.0 ± 1.4 with the feeling eye was scored greater than the 6.4 ± 1.4 with topical anesthesia (T(16)=2.5, p = 0.02). The pain score with exact same See-Through depressor numb at 350 LUX indirect was 3.6 ± 1 and seemed to increase to 4.4 ± 1.4 with numb, full bright 4000 LUX but not statistically different (T(16)=1.5 p = 0.16). Combined pain and brightness scores for each exam method are shown in Figure 6.
At the end of testing, the 9 subjects had similar scores of their memory of a “Brain Freeze” which can follow a quick ingestion of too much ice-cream, milk-shake with a pain score of 5.6 ± 1.7. Removal of the adhesive strip for the VivaLNK cardiac monitor produced a pain score of 3.3 ± 1.3.
Discussion
Through this prospective study of adults selected for their concern about stress in premature infants, we confirmed the moderate benefit of topical anesthesia for on-globe scleral depressed retinal exam as is typically done for ROP staging examinations. We also detected a synergistic sensory stress augmentation between pain and brightness. In contrast to the bradycardia typical in premature infants, minimal heart rate change occurred with adults as a result of on-globe, scleral depressed retinal exam.
Retinopathy of prematurity is “screened” by neonatologists based on regionally agreed levels of gestational age, birthweight and other risk factors. The uniform application of guidelines and resultant exam timing can be facilitated by software like ROP Check (Neolight, Phoenix, Arizona).38 As such, utilizing the correct nomenclature, ROP screening produces no physiological stress to the infant. However, once an infant meets ROP screening criteria and is referred, the ROP “staging” examination(s) can produce substantial stress for that infant, stress that is readily apparent to caregivers who have a stake in reducing stress including nurses, physical and occupational therapists, neonatologists, pediatric anesthesiologists, ophthalmologists and, of course, parents. The scleral-depressed, indirect ophthalmoscope ROP staging exam is often incorrectly and colloquially called an ROP “screening” exam.39
The thorough infant retinal examination is not easy for the examining ophthalmologist or for the patient. The infant may have puffy eyes with or without nasolacrimal discharge, there may be supplemental oxygen by intubation or nasal continuous positive airway pressure (CPAP), often infants are isolated with communicable diseases, and tiny infants are prone to dramatic apnea and bradycardia with even gentle ocular manipulation. The instrumentation for premature infant eye examinations represents more than just a miniaturization of adult tools. The anatomy of the infant fornix makes non-invasive, posterior reach of a cryo-probe very difficult.40 The Arnold See-Through scleral depressor allows cryotherapy to zone 1 without conjunctival incision.37,41 Additional lid specula and scleral depressors have been adapted to tiny eyes. Efforts should be made to reduce infant stress and keep the risk of nosocomial infection down.42 Following a stressful ROP staging examination, infants may have disrupted eating, sleep, prolonged apnea and bradycardia, and temporary indentation of the eyelids and subconjunctival hemorrhage.
There are similarities between adult and premature infant eye examinations: instruments to open and move the eye, luminosity, and documentation with various imaging techniques and cameras. However, there are also differences between adult subjects and premature infant eye exams: the size of eye and lid, bradycardia with exam, ability to voluntarily direct gaze, softness of globe, systemic dilution of drops, infants might be resisting eye rotation while adults encouraged to assist. Infant pain profiles that rely on heart rate can have confounded implications with eye pain during scleral depression because the ROP exam often elicits profound bradycardia whereas pain elsewhere typically results in tachycardia. Adults compared to infants are better able to separate their perception of brightness and of pain.
We detected a trend toward synergistic stress with various noxious stimuli in retinal exam with direct globe contact (Figure 6). Brightness from the same light source was scored higher when more pain was sensed, and there was a statistically underpowered trend for more pain scored with brighter examination. When topical anesthesia was not used, subjects with robust Bells phenomena had higher pain scores than those who kept the eye gazing away from the lid speculum.
The retinal exam technique of direct ophthalmoscope through a goniolens has been thought to be less stressful.43 Some infants are capable of resuming sleeping by this technique. We noted similar levels of brightness and lid-opening pain with this direct/gonio method and lid speculum/indirect exam. The addition of scleral depression adds a continuously varying pressure and prodding sensation which may not allow an infant to resume sleep with the scleral indentation component. Once inserted, the Shaffer-Richardson goniolens may not need to be touched to allow retinal exam to the mid-periphery. Retinal examination with a non-contact camera can show less stress than typical indirect ophthalmoscopy.44
The PIPP is not a perfect indicator of stress in every circumstance.13,45 An infant may cry and wince for a similar exam component that an adult would judge Likert pain or brightness level 5 and have a similar wince and cry up to an adult perceived level 10. Tachycardia can be elicited by pain, whereas bradycardia can be elicited by manipulation of periocular tissues. As such infant pain scores incorporating phonation, avoidance behavior and cardiac rhythm may have limited precision. Even though an adult might sit still and externally tolerate a pain or brightness score of 6 similarly to a 9, most would prefer to avoid the 9.
Heart rate change during ROP examinations has been observed for decades. Javorka in 197846 and Clarke in 198547 reported excessive bradycardia during ROP examinations. Bradycardia that can be more profound than the oculocardiac reflex induced by strabismus surgery is frequently associated with lid speculum, scleral depressed ROP staging examinations.12 However, in this study of on-globe scleral depressed retinal examination in 9 adults, minimal heart rate change was observed. We found cardiac monitoring with the VivaLNK system to be elegant, reliable and not cumbersome.
A weakness of this study was quantifying the pain level of a short-acting dilating drop instead of the dilute cyclopentolate/phenylephrine drop typically used in the NICU. We used similar sized lid specula in adults as would be used in the infants, but we used a larger goniolens for the adults. This study did not assess the qualitative difference of retinal vessel staging by these various exam techniques. The order of exam was fixed and therefore any element of sensory adaptation or augmentation was not controlled. The sample size was just sufficient to detect a 2-scoring level difference in Likert score for pain and brightness. The majority of Likert scores for pain and brightness, and the heart rate responses had normal distributions and therefore we employed t-Test for comparison of all comparisons instead of non-parametric for some. A strength of the study was relatively short 15-minute overall data gathering duration so each adult could compare various components, however we studied shorter examples of the exam methods with persistent stress induction which might individually last minutes for the complex examination of a tiny infant at risk of lifetime blindness from ROP. No short-term or long-term adverse effects were reported by all 9 subjects.
Conclusion: This study employing sensory perceptions during a retinal exam method using direct contact with the globe, which is atypical in the adults but typical for infants, favors the judicious use of topical anesthetic and limited ophthalmoscope brightness when possible. Topical dilating drops produce substantial discomfort. The sensation of wire lid specula and gonioscopic lenses is similar and mild, but brightness from indirect and direct ophthalmoscopy and retinal photography can be intense. There appears some synergistic impact between pain and brightness during retinal examinations.
Abbreviations
Gonioscopy (gonio), model of portable Phoenix retinal camera ICON Go; IQR, Inter-quartile range; NICU, neonatal intensive care unit; OCR, Oculocardiac reflex; PIPP, Premature Infant Pain Profile; ROP, retinopathy of prematurity; SD, standard deviation; Please see Table 1.
Data Sharing Statement
Data Access: https://www.abcd-vision.org/references/ROP-Stress-DeID.pdf.
Funding
There is no funding to report.
Disclosure
Dr Arnold is a board member of PDI Check, PEDIG, and Glacier Medical Software which owns a Phoenix ICON GO camera. Dr Robert W Arnold is a coordinator for Alaska Blind Child Discovery, during the conduct of the study; consultant for Neolight, outside the submitted work; In addition, Dr Robert W Arnold has patent Systems and Methods for Eye Evaluation and Treatment issued to Robert Arnold and Alex Damarjian; Drs Runge and Arnold have designed instruments for ROP examination, but receive no royalties. The authors report no other conflicts of interest in this work.
References
1. Dhillon B, Wright E, Fleck BW. Screening for retinopathy of prematurity: are a lid speculum and scleral indentation necessary? J Pediatr Ophthalmol Strabismus. 1993;30(6):377–381.
2. Arnold RW, Grendahl RL, Kevin Winkle R, Jacob J. Outpatient, wide-field, digital imaging of infants with retinopathy of prematurity. Ophthalmic Surg Lasers Imaging Retina. 2017;48(6):494–497.
3. Pflugrath AE, Runge PE. New scleral depressor for retinopathy of prematurity. Retina. 2022;42(4):822–823.
4. Morizane Y, Takasu I, Mohri S, Ohtsuki H. A new scleral depressor for premature infants. Retina. 2005;25(8):1118.
5. Karaki T. A new scleral depressor for extremely premature infants. J Pediatr Ophthalmol Strabismus. 1994;31(4):267.
6. Kumar KS, Gopal L, Badrinath SS, Nethralaya S. Infant scleral depressor. Retina. 1992;12(4):376.
7. Spaide RF. A scleral depressor for infants. Ophthalmic Surg. 1987;18(7):544.
8. Katz NN, Przybyla VA
9. Hindle NW. Cryotherapy for retinopathy of prematurity to prevent retrolental fibroplasia. Can J Ophthalmol. 1982;17(5):207–212.
10. Szewczyk TS. Retrolental fibroplasia; etiology and prophylaxis. Am J Ophthalmol. 1952;35(3):301–311.
11. Stevens BJ, Gibbins S, Yamada J, et al. The premature infant pain profile-revised (PIPP-R): initial validation and feasibility. Clin J Pain. 2014;30(3):238–243.
12. Schumacher AC, Ball M, Arnold AW, Grendahl RL, Winkle RK, Arnold RW. Oculocardiac reflex during ROP exams. Clin Ophthalmol. 2020;14:4263–4269.
13. Onuagu V, Gardner F, Soni A, Doheny KK. Autonomic measures identify stress, pain, and instability associated with retinopathy of prematurity ophthalmologic examinations. Front Pain Res. 2022;3:1032513.
14. Arnold RW. Digital values for alpha acuities. JPOS. 2021;58(2):132–135.
15. Belda S, Pallas CR, De la Cruz J, Tejada P. Screening for retinopathy of prematurity: is it painful? Biol Neonate. 2004;86(3):195–200.
16. Kara C, Petricli IS, Uzlu SE, Cuni BT. Effect of topical anesthesia on reducing pain associated with mydriatic eye drops during retinopathy of prematurity screening. Ophthalmologica. 2022;245(5):487–494.
17. Cohen AM, Cook N, Harris MC, Ying GS, Binenbaum G. The pain response to mydriatic eyedrops in preterm infants. J Perinatol. 2013;33(6):462–465.
18. Nesargi SV, Nithyanandam S, Rao S, Nimbalkar S, Bhat S. Topical anesthesia or oral dextrose for the relief of pain in screening for retinopathy of prematurity: a randomized controlled double-blinded trial. J Trop Pediatr. 2015;61(1):20–24.
19. Disher T, Cameron C, Mitra S, Cathcart K, Campbell-Yeo M. Pain-relieving interventions for retinopathy of prematurity: a meta-analysis. Pediatrics. 2018;142(1):8768.
20. Francis K. What is best practice for providing pain relief during retinopathy of prematurity eye examinations? Adv Neonatal Care. 2016;16(3):220–228.
21. Marsh VA, Young WO, Dunaway KK, et al. Efficacy of topical anesthetics to reduce pain in premature infants during eye examinations for retinopathy of prematurity. Ann Pharmacother. 2005;39(5):829–833.
22. Kabatas EU, Dursun A, Beken S, Dilli D, Zenciroglu A, Okumus N. Efficacy of Single Dose Oral Paracetamol in Reducing Pain During Examination for Retinopathy of Prematurity: a Blinded Randomized Controlled Trial. Indian J Pediatr. 2016;83(1):22–26.
23. Mangalesh S, Sarin N, McGeehan B, et al. Preterm Infant Stress During Handheld Optical Coherence Tomography vs Binocular Indirect Ophthalmoscopy Examination for Retinopathy of Prematurity. JAMA Ophthalmol. 2021;139(5):567–574.
24. Kirchner L, Jeitler V, Pollak A, et al. Must screening examinations for retinopathy of prematurity necessarily be painful? Retina. 2009;29(5):586–591.
25. Mataftsi A, Lithoxopoulou M, Seliniotaki AK, et al. Avoiding use of lid speculum and indentation reduced infantile stress during retinopathy of prematurity examinations. Acta Ophthalmol. 2022;100(1):e128–e134.
26. Ercelik ZE, Yilmaz D. Nonpharmacological applications during the retinopathy of prematurity examination and their effects on pain control: a systematic review and meta-analysis. J Perinat Neonatal Nurs. 2022;36(3):297–304.
27. Sener Taplak A, Erdem E. A comparison of breast milk and sucrose in reducing neonatal pain during eye exam for retinopathy of prematurity. Breastfeed Med. 2017;12:305–310.
28. Turan O, Akkoyun I, Ince DA, Doganay B, Tugcu AU, Ecevit A. Effect of breast milk and sucrose on pain and perfusion index during examination for retinopathy of prematurity. J Matern Fetal Neonatal Med. 2021;34(7):1138–1142.
29. Rosali L, Nesargi S, Mathew S, Vasu U, Rao SP, Bhat S. Efficacy of expressed breast milk in reducing pain during ROP screening--a randomized controlled trial. J Trop Pediatr. 2015;61(2):135–138.
30. Padhi TR, Sareen D, Pradhan L, et al. Evaluation of retinopathy of prematurity screening in reverse Kangaroo Mother Care: a pilot study. Eye. 2015;29(4):505–508.
31. Sun Y, Zhang J, Chen X, et al. Effectiveness of gentle human touch for pain control during examination for retinopathy of pre-maturity: a randomized controlled trial. Front Pediatr. 2020;8:608378.
32. Cogen MS, Parker JS, Sleep TE, Elsas FJ, Metz TH
33. Jiang JB, Strauss R, Luo XQ, et al. Anaesthesia modalities during laser photocoagulation for retinopathy of prematurity: a retrospective, longitudinal study. BMJ Open. 2017;7(1):e013344.
34. Kandasamy Y, Smith R, Wright IM, Hartley L. Pain relief for premature infants during ophthalmology assessment. J AAPOS. 2011;15(3):276–280.
35. Mehta M, Mansfield T, VanderVeen DK. Effect of topical anesthesia and age on pain scores during retinopathy of prematurity screening. J Perinatol. 2010;30(11):731–735.
36. Arnold RW, Bond AN. Does topical proparacaine improve postoperative comfort after strabismus surgery? Clin Ophthalmol. 2019;13:2279–2283.
37. Arnold RW. Posterior retinopathy of prematurity cryotherapy from a limbal reference. J Pediatr Ophthalmol Strabismus. 1994;31:303–305.
38. Arnold RW, Jacob J, Matrix Z. Toward Achieving 100% Adherence for Retinopathy of Prematurity Screening Guidelines. J Pediatr Ophthalmol Strabismus. 2017;54(6):356–362.
39. Wilson JM, Jungner YG. Principles and practice of mass screening for disease. Bol Oficina Sanit Panam. 1968;65(4):281–393.
40. Schulenburg WE, Yang YF, Parikakis E, Bydder GM. Cryotherapy for retinopathy of prematurity: a MRI study of the surgical-anatomical relationship of the neonatal conjunctival fornices to the globe. Eye. 2001;15(Pt 5):587–590.
41. Palmer EA. Posterior retinopathy of prematurity cryotherapy for a limbal reference: discussion. J Pediatr Ophthalmol Strabismus. 1994;31(5):306.
42. Hered RW, Gyland EA. The retinopathy of prematurity screening examination: ensuring a safe and efficient examination while minimizing infant discomfort. Neonatal Netw. 2010;29(3):143–151.
43. Hindle NW. Retinopathy of prematurity. Arch Ophthalmol. 1985;103(7):894–895.
44. Prakalapakorn SG, Stinnett SS, Freedman SF, Wallace DK, Riggins JW, Gallaher KJ. Non-contact retinal imaging compared to indirect ophthalmoscopy for retinopathy of prematurity screening: infant safety profile. J Perinatol. 2018;38(9):1266–1269.
45. Witt N, Coynor S, Edwards C, Bradshaw H. A guide to pain assessment and management in the neonate. Curr Emerg Hosp Med Rep. 2016;4:1–10.
46. Javorka K, Zavarska L. Oculocardiac reflex in premature infants. Cesk Pediatr. 1978;33(3):138–140.
47. Clarke WN, Hodges E, Noel LP, Roberts D, Coneys M. The oculocardiac reflex during ophthalmoscopy in premature infants. Am J Ophthalmol. 1985;99(6):649–651.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.