Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 14
Are the Things Told to Care Providers Kept Confidential?: Perceived Breaches of Confidentiality and Associated Factors Among HIV/AIDS Clients on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021
Authors Bayisa L , Wakuma B , Abera T, Mulisa D , Mosisa G , Tolossa T , Turi E
Received 18 November 2021
Accepted for publication 30 December 2021
Published 15 January 2022 Volume 2022:14 Pages 1—12
DOI https://doi.org/10.2147/HIV.S350091
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Lami Bayisa,1 Bizuneh Wakuma,2 Tesfaye Abera,1 Diriba Mulisa,1 Getu Mosisa,1 Tadesse Tolossa,3 Ebisa Turi3
1Department of Nursing, School of Nursing and Midwifery, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 2Department of Pediatric Nursing, School of Nursing and Midwifery, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 3Department of Public Health, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
Correspondence: Lami Bayisa
Department of Nursing, School of Nursing and Midwifery, Institute of Health Sciences, Wollega University, PO Box 395, Nekemte, Ethiopia
Tel +251924318135
Email [email protected]
Introduction: HIV clients’ mistrust in providers’ handling of their medical information can be a reason for them not to utilize services. Compromised confidentiality of HIV clients can affect the entire community, as other people may become reluctant to seek HIV testing and counseling. In Ethiopia, there are few data on perceived breaches of confidentiality among HIV/AIDS clients. Thus, this study aimed to assess perceived breaches of confidentiality and associated factors among people living with HIV (PLHIV) on anti-retroviral therapy (ART) at Nekemte Specialized Hospital, Western Ethiopia.
Methods: A facility-based cross-sectional study was conducted among 423 HIV/AIDS clients at Nekemte Specialized Hospital from January 15 to February 20, 2021. Data were collected by an investigator-administered questionnaire. Collected data were entered into EpiData version 3.1, and Stata version 14.0 was used for analysis. Bivariable and multivariable logistic regression analyses were performed. Variables with a P-value of < 0.2 in the bivariable analysis were exported to the multivariable analysis. Adjusted odds ratios (AORs) with 95% confidence intervals (CIs) and P-values of < 0.05 were used to report significantly associated variables.
Results: A total of 423 PLHIV were included in the study. Nearly one-fourth of the respondents (23.60%) had perceived breaches of confidentiality (95% CI 19.8– 27.9%). Delayed ART start [(AOR 1.97) 95% CI (1.05– 3.71)], being female [(AOR 4.03) 95% CI (2.14– 7.59)], being widowed [(AOR 4.11) 95% CI (1.50– 11.20)], college education and above [(AOR 10.89) 95% CI (3.93– 30.14)], normal BMI [(AOR 2.72) 95% CI (1.06– 6.99)], substance use [(AOR 1.93) 95% CI (1.04– 3.58)], not knowing other ART user(s) [(AOR 2.89) 95% CI (1.53– 5.47)], and CD4 count ≤ 200 cells/mm3 [(AOR 2.63) 95% CI (1.22– 5.68)] were significantly associated variables.
Conclusion: One in four HIV/AIDS clients reported experiencing perceived breaches of confidentiality. Thus, early ART initiation, further HIV serostatus disclosure, and encouraging patients to decide on the type of care and information they want need to be strengthened in order to reduce breaches of confidentiality.
Keywords: breaches of confidentiality, ART initiation, care providers, HIV/AIDS clients, PLHIV
Introduction
Despite the creation of awareness and public education about HIV/AIDS that has been undertaken for several decades, stigma and discrimination continue to shape much of society’s reactions toward people living with HIV (PLHIV).1,2 It is difficult to forecast how PLHIV will respond, or how their lives may change, if and when their HIV-related medical information becomes known by others.3 This is why all PLHIV have the right to decide and control where, when, how, and to whom their HIV-related medical information can be disclosed.4–6
However, some healthcare providers easily leak clients’ medical information, overlooking that this may lead to stigma. Besides, when accessing counseling, testing, and treatment services, HIV/AIDS clients are often concerned about the possibility of a breach of their HIV serostatus and the negative impacts that may follow. In the same way, HIV-positive individuals may experience two psychological conflicts: first, against relatives and friends who must not know their HIV serostatus; and second, against healthcare providers entrusted with confidential information. These factors can all lead to HIV-infected individuals becoming suspicious of their medical information and being a vulnerable group.7–9
Lack of trust by HIV clients in the healthcare providers’ handling of medical information related to their HIV serostatus can be a reason for them not to utilize HIV-related healthcare services. Thus, efforts to reduce HIV-related stigma need a significant change in the attitudes and practices of health facility staff, and the quality of care provided.10
The persistent stigma related to HIV infection makes it necessary for clients to devise strategies and secretly use counseling, testing, and treatment services.11 This may enable them to conceal their HIV status from some relatives and friends to avoid potential stigmatization. Therefore, clients need to be actors who can make the decision to use services in healthcare facilities in safety.
The consequences of compromising the confidentiality of PLHIV go beyond the individual. The harmful effects can be felt by an entire community; for instance, other community members will be more reluctant to be tested for HIV. If fewer people find out that they are HIV positive, the risk of further community HIV transmission is increased. In addition, breaches of confidentiality can create reasons for not seeking medical treatment or other services by people who need them.
In this study, a breach of confidentiality is defined as any divulgence of information by a healthcare provider without the express consent of the patient.12 To our best of the research knowledge, there are limited data regarding the perception of breaches of confidentiality among HIV-infected people on anti-retroviral therapy (ART) in Ethiopia, particularly in our study setting. However, such evidence is very important, to fill the information gap that exists and to improve the care provided to HIV/AIDS clients. Thus, this study aimed to assess perceived breaches of confidentiality and associated factors among PLHIV on ART at Nekemte Specialized Hospital.
Methods
Study Setting and Design
A facility-based cross-sectional study was conducted among 423 PLHIV on ART at Nekemte Specialized Hospital from January 15 to February 20, 2021. Nekemte Specialized Hospital is located in Nekemte town, the capital city of East Wollega Zone, Ethiopia. Nekemte town is located 328 km to the west of Addis Ababa. The hospital was established in 1940, and it started to provide ART services in 2005. Currently, about 2925 adult HIV-positive individuals are receiving ART services at the hospital.
Population and Sampling
The sample size was determined using a single population proportion formula considering the assumption of 95% confidence interval (CI), a margin of error of 5% (d=0.05), and taking 50% magnitude of perceived breach of confidentiality (P=0.5). The final sample size was 423 after a non-response rate (10%) was added. The source population comprised all HIV/AIDS clients attending the ART clinics at Nekemte Specialized Hospital. HIV/AIDS clients older than 15 years of age were eligible for the study. The study participants were recruited consecutively during their visit for follow-up, and data were obtained in a private room after they had finished their routine services.
Study Variables
The dependent variable was perceived breach of confidentiality.
Independent variables were: 1) socio-demographic characteristics (including age, sex, religion, residence, marital status, educational level, and occupation); 2) clinical characteristics (including baseline CD4 count, WHO clinical stage, functional status, body mass index [BMI], tuberculosis [TB]/HIV co-infection, baseline opportunistic infections, and HIV testing approach); 3) behavioral and social factors (use of traditional treatment, having a regular sexual partner, number of times tested for HIV, HIV disclosure status, level of social support, and knowing other ART user(s)).
Data Collection Instrument and Procedure
Data were collected using an interviewer-administered questionnaire. The questionnaire was developed from the national ART guideline, ART intake forms, and the comprehensive HIV Testing and Counseling format. The questionnaire contains both closed-ended questions and open-ended questions. The questionnaire was prepared in English and translated into the local language, Afaan Oromoo, for data collection, and then translated back to English to maintain its consistency. Each patient’s chart was retrieved by using their registration number from the database. Patients were interviewed to obtain their socio-demographic characteristics. Relevant medical history and laboratory parameters were taken from the ART intake form and follow-up care form. One supervisor (BSc Public Health) and two data collectors (Clinical Nurses) participated in the data collection program. Quality of data was ensured through training and supervising the data collectors.
Data Management and Analysis
Collected data were entered into EpiData version 3.1, cleaned, and exported to Stata version 14.0 for analysis. Patient characteristics were reported as counts or percentages for categorical factors. Bivariable and multivariable logistic regression analyses were conducted to identify associated factors with perceived breaches of confidentiality. Those variables with a P-value of <0.2 in the bivariable analysis were exported to multivariable analysis. Adjusted odds ratios (AORs) with 95% confidence intervals (CIs) and P-values of <0.05 were used to select and report the factors significantly associated with perceived breaches of confidentiality in the final results.
Ethical Considerations
Ethical clearance was obtained from the Institutional Review Board of the Institute of Health Sciences, Wollega University. A formal letter of permission was obtained from the Medical Director of Nekemte Specialized Hospital. Study participants were recruited only after informed consent had been obtained from all of them. All obtained data were preserved confidentially and this study was conducted in accordance with the Declaration of Helsinki.
Definition of Terms
A perceived breach of confidentiality was defined as any divulgence of information by a healthcare provider without the express consent of the patient.12
Delayed ART initiation was defined as starting ART after 7 days following a confirmed positive HIV diagnosis.13
Traditional healing refers to knowledge, approaches, and health practices, incorporating plant, animal, and mineral-based medicines, spiritual therapies, manual techniques, and exercises, applied singularly or in combination to treat, diagnose, and prevent illnesses or maintain well-being.14
Results
Socio-Demographic Characteristics of the Study Participants
This study was conducted on a total of 423 HIV/AIDS clients on ART. Of all respondents, the majority of them (81.85%) were in the category 18–40 years of age. More than half of the respondents were female (54.61%) and more than half were Protestant in their religion (53.9%). More than two-thirds of respondents were urban dwellers (69.74%) and almost half of the respondents (49.65%) were married. Regarding educational status, over one-fourth of the respondents (26.24%) had attended college and above, and regarding occupation, 32.15% of respondents were housewives (Table 1).
 |
Table 1 Socio-Demographic Characteristics of HIV/AIDS Clients on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Clinical Characteristics of the Study Participants
Less than half of respondents (44.21%) had a baseline CD4 cell count of >500 cells/mm3. Nearly two out of five respondents (37.5%) were classified under WHO clinical stage I. The majority of respondents (80%) were diagnosed with a working level of functional status; almost all respondents (90%) did not report TB/HIV co-infections and very few respondents (<1%) were diagnosed with baseline opportunistic infections other than TB. More than half (57.92%) of respondents had been tested for HIV via provider-initiated HIV testing and counseling (PITC) and about one-third of them were delayed in starting ART (Table 2).
 |
Table 2 Clinical Characteristics of HIV/AIDS Clients on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Behavioral and Social Characteristics of the Study Participants
Among all respondents, almost two in three (65.72%) reported having a regular sexual partner, and the majority of respondents (70.45%) had been tested for HIV only once. Nearly three out of four (73.76%) respondents had disclosed their HIV serostatus. About three out of five respondents (58.87%) reported a history of substance use and practiced traditional healing (60.28%). Less than half (41.84%) of the respondents knew other ART user(s), and only a few of them had a strong level of social support (7.09%) and reported the presence of communication barriers during the HIV test (7.09%) (Table 3).
 |
Table 3 Behavioral and Social Characteristics of HIV/AIDS Clients on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Magnitude of Perceived Breaches of Confidentiality
Nearly one out of four HIV/AIDS clients had perceived breaches of confidentiality concerning their HIV-related medical information in the study area. Of 100 respondents who perceived breaches of confidentiality, nearly half (48%) of them had a history of delayed ART initiation and the majority (72%) of them were female (Figure 1).
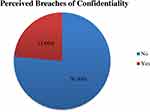 |
Figure 1 Perceived breaches of confidentiality among HIV/AIDS clients on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021. |
Perceived Breaches of Confidentiality: Brief Explanation
Those respondents who perceived breaches of confidentiality were given the chance to discuss or explain how and where they experienced the breaches of their HIV-related medical information. Accordingly, most of the respondents gave their reflection and these reflections were summarized into three main categories to answer the questions of “where” and “how” the breaches of confidentiality were experienced, and then applied to the way that they perceived the breaches of confidentiality (Table 4).
 |
Table 4 Concepts Raised by HIV/AIDS Clients at Different Working Units of the Hospital, With Explanation and Application to Perceived Breaches of Confidentiality |
Regarding areas where the respondents experienced breaches of confidentiality in the Nekemte Specialized Hospital, six potential areas were identified. Respondents mentioned these breaches and explained them briefly from their point of view. Consequently, the ART clinic‘s open location, inpatient/ward admission, provider approaches, medication refilling area, the way that clients transferred/linked, and the laboratory request form were issues raised by the respondents. In particular, a large number of respondents (88) complained about the ART clinic’s open location, while many other respondents (63) complained about the care providers’ approach (Figure 2).
 |
Figure 2 Areas where breaches of confidentiality were perceived among HIV/AIDS clients on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021. |
Factors Associated with Perceived Breaches of Confidentiality
Bivariable Analysis
Binary logistic regression model analysis was computed to identify potential factors. Accordingly, 17 potential independent variables were found to be associated with the outcome variable at a P-value of <0.2 and were considered as candidates for the multivariable logistic regression model (Table 5).
 |
Table 5 Results of Bivariable Analysis and Factors Associated with Breaches of Confidentiality Among HIV/AIDS Clients on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Multivariable Analysis
The multivariable logistic regression analysis was conducted on the 17 candidate variables. Eight variables (sex, marital status, educational level, delayed ART start, baseline CD4 count, nutritional status, and substance use) remained significantly and independently associated with perceived breaches of confidentiality among HIV/AIDS clients at a P-value of <0.05.
Accordingly, respondents with a delayed ART start had a two-fold higher perceived breach of confidentiality compared to their counterparts [(AOR 1.97) 95% CI (1.05–3.71)]. Female respondents were four times more likely to have perceived breaches of confidentiality compared to male respondents [(AOR 4.03) 95% CI (2.14–7.59)]. Widowed respondents were four times more likely to have perceived breaches of confidentiality compared to those who were married [(AOR 4.11) 95% CI (1.50–11.20)].
Respondents who had completed primary school, secondary school, and college and above were eight, 16, and 11 times more likely to have perceived breaches of confidentiality [(AOR 7.89) 95% CI (2.92–21.33), (AOR 16.37) 95% CI (5.57–48.08), and (AOR 10.89) 95% CI (3.93–30.14), respectively] compared to respondents with no formal education.
Respondents with normal BMI were three times more likely to have perceived breaches of confidentiality compared to underweight respondents [(AOR 2.72) 95% CI (1.06–6.99)]. Respondents who had ever used substances were two-fold more likely to have perceived breaches of confidentiality than non-users [(AOR 1.93) 95% CI (1.04–3.58)]. Respondents who did not know other ART user(s) were three times more likely to have perceived breaches of confidentiality compared to their counterparts [(AOR 2.89) 95% CI (1.53–5.47)]. The odds of a perceived breach of confidentiality were two-fold higher among participants with a baseline CD4 count of ≤200 cells/mm3 compared to those with >500 cells/mm3 [(AOR 2.63) 95% CI (1.22–5.68)] (Table 6).
 |
Table 6 Results of Multivariable Analysis and Factors Associated with Breaches of Confidentiality Among HIV/AIDS Clients on ART at Nekemte Specialized Hospital, Western Ethiopia, 2021 |
Discussion
The right to privacy or confidentiality is a fundamental human right in every country in the world. It is also the fundamental determinant of healthcare-seeking behavior of patients/clients who have an illness leading to social isolation, discrimination, and stigma. In this regard, HIV/AIDS is among the medical illnesses known to cause discrimination and stigma not only in the community but also in the healthcare setting.15 Basically, maintaining confidentiality can create an ethical dilemma between respecting the autonomy of the patient and endangering the life of the community at large. Research has shown that maintaining confidentiality is a cornerstone of successful ART through improving the adherence to ART of PLHIV.16,17 On the contrary, breach of confidentiality is the leading cause of low healthcare-seeking behavior among HIV-positive patients, low ART adherence, and traveling long distances to access ART.16,18 Moreover, it may also be the leading cause of an increased incidence of HIV infection and HIV-related mortality and morbidity in Ethiopia. This is the most cited reason for HIV patients receiving HIV-related care from a health facility which is located far from their place of residence.19 Therefore, this study aimed to determine the level of perceived breaches of confidentiality and their associated factors among HIV-positive patients attending the ART clinic of Nekemte Specialized Hospital.
According to the present study, nearly one-fourth of the participants had perceived a breach of confidentiality. This result echoes the finding of a study from the Islamic Republic of Iran.20 In addition, patients’ medical information being breached by physicians or nurses was mentioned in HIV-related studies from Zambia, Malawi, and Senegal.3,21,22 Furthermore, congruent with the current study findings, a study from Indonesia showed that confidentiality is poorly taught and systematically breached in practice.23 However, in contrast to the current study, a study from South Africa revealed that participants believed that their HIV status was kept confidential.24 The observed discrepancy may be due to socio-cultural variations among the populations of interest, and bureaucratic differences in breaching confidentiality.
The present study also found important factors affecting perceived breaches of confidentiality among PLHIV. Accordingly, the likelihood of a perceived breach of confidentiality was two-fold higher among PLHIV who experienced delayed ART initiation compared to their counterparts. This may be attributed to a fear of stigma related to a confidentiality breach, which further leads to delayed ART initiation, low ART adherence, opportunistic infections, and poor clinical outcomes. This is a major health system challenge which must be resolved to prevent and control HIV infection in the community. In addition, the odds of a perceived breach of confidentiality were four times higher among female patients compared to their male counterparts. This may be explained by a biological difference between females and males in terms of their psychological/emotional reaction to a given circumstance. Likewise, widowed women were four times more likely to have perceived a breach of confidentiality compared to married women. This may be due to widowed women being more worried about their future life, such as marrying, childbearing, and social relations. Besides, widowed women are already stigmatized and discriminated against in the community, so that their perception of confidentiality being breached is high.
Furthermore, patients with a baseline CD4 cell count ≤200 cells/mm3 were 2.63 times more likely to have perceived a breach of confidentiality compared to those with a baseline CD4 cell count >500 cells/mm3. A possible reason is that an abnormal CD4 cell count of 200 or fewer indicates an advanced stage of the disease (AIDS) and a high risk of life-threatening opportunistic infections.25 These patients lose physical strength, with weight loss and decreased muscle mass, have repeated skin infections, are frequently absent from work, and may have an increased number of hospital visits. During their hospital visits, they may observe and notice the hospital environment more, as well as the providers’ approach, including the care they provide. The current study also found that the literacy status of the HIV/AIDS clients had an influence on their level of perceiving breaches of confidentiality of HIV-related medical information. Accordingly, the more educated patients were more likely to perceive a breach of confidentiality compared to those who had a low educational level. This may be due to educated people being able to acquire or gather information from multiple sources during their medication follow-up.26,27 They may hear different languages, and read leaflets, laboratory requests, radiology examination requests, medication prescriptions, medical registration charts, and information on open desktop computers. So, in cases where they hear or see HIV-related medical information on themselves and/or on other patients, they become more suspicious about the handling of the information.
This study also found that patients who use substances were two-fold more likely to have perceived a breach of confidentiality compared to non-users. This may imply that individuals who practice substance use (smoking, drinking alcohol, chewing chat, etc) from the beginning have low societal acceptance.28 Though, when their underlying conditions are exacerbated or doubly burdened by HIV/AIDS, they may have doubts about the way in which services are provided and the providers’ approaches. In addition, patients who did not know other ART user(s) were three times more likely to have perceived a breach of confidentiality compared to those who knew other ART user(s). The only possible way to know another ART user is through a patient disclosing their HIV-positive serostatus. Disclosing one’s own HIV-positive serostatus can have positive consequences for the health and lives of PLHIV. They may receive strong social support, improve their adherence to medication, and increase the health-seeking behavior of other individuals and their trust in the services being provided.29 Hence, patients who do not know other ART user(s) may lack information on how much their HIV-related medical information will be kept confidential and be apprehensive toward the providers’ approach and services delivered. Moreover, the odds for a perceived breach of confidentiality were three-fold higher in patients with normal nutritional status (BMI 18.5–24.9 kg/m2) compared to underweight patients. Patients with normal nutritional status may have conserved their immunity and may not be clinically ill, which may be reflected by poor adherence to provided care and counseling.30,31 As they may feel healthy, since their body defenses are still competent and protecting them from invading pathogens, they may even doubt the effectiveness of ART drugs. So, they may not want to be seen or known as HIV-infected individuals, and to overcome these challenges they suspect that care providers may expose their HIV-related medical information.
Limitations
Although this is a prime area of interest, there is limited literature to compare and contrast with the present study findings. As this is a cross–sectional study, it is difficult to determine temporal relationships. It would have been better if the quantitative findings had been supplemented by qualitative findings.
Conclusion
In general, the magnitude of perceived breaches of confidentiality among PLHIV was high in the study area. The study found that delayed ART initiation, being female, being a widowed woman, and having a low CD4 count (≤200 cells/mm3) were independent determinants of perceived breaches of confidentiality. Therefore, there is a need to develop clear and comprehensive guidelines and policies that enhance the protection of privacy and confidentiality in order to reduce breaches of confidentiality. Moreover, there is a need for increased awareness in PLHIV on the procedures of keeping information secret and conditional circumstances demanding a breach of confidentiality. In addition, future researchers should undertake a mixed study design to underpin the quantitative study findings, and care providers’ perspectives need to be incorporated.
Abbreviations
AIDS, acquired immune deficiency syndrome; AOR, adjusted odds ratio; ART, anti-retroviral therapy; BMI, body mass index; CD4, cluster of differentiation 4; CI, confidence interval; HIV, human immunodeficiency virus; OI, opportunistic infection; PITC, provider-initiated testing and counseling; PLHIV, people living with human immunodeficiency virus; TB, tuberculosis; VCT, voluntary counseling and testing; WHO, World Health Organization.
Data Sharing Statement
All datasets used and analyzed in the present study are included in this manuscript.
Ethical Approval and Consent to Participants
Ethical endorsement was gained from the Institutional Review Board of the Institute of Health Sciences, Wollega University. A formal permission letter was obtained from the administrative body of Nekemte Specialized Hospital. Informed consent was taken from each study participant before the data collection started. All data were collected anonymously and maintained with confidentiality. All the procedures of data collection were conducted according to the principles of the Declaration of Helsinki.
Acknowledgments
We are thankful to the study participants for their cooperation and to the data collectors.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was obtained for this research article.
Disclosure
The authors declare that they have no competing interests.
References
1. Neuman M, Obermeyer CM. Experiences of stigma, discrimination, care and support among people living with HIV: a four country study. AIDS Behav. 2013;17(5):1796–1808. doi:10.1007/s10461-013-0432-1
2. Twinomugisha B, Ottemöller FG, Daniel M. Exploring HIV-related stigma and discrimination at the workplace in Southwestern Uganda: challenges and solutions. Adv Public Health. 2020;2020:e8833166. doi:10.1155/2020/8833166
3. Dapaah JM, Senah KA. HIV/AIDS clients, privacy and confidentiality; the case of two health centres in the ashanti region of Ghana. BMC Med Ethics. 2016;17(1):41. doi:10.1186/s12910-016-0123-3
4. Todd A. Mandatory HIV status disclosure for students in Illinois: a deterrent to testing and a violation of the Americans with disabilities act, 10. Nw. J. L. & Soc. Pol’y; 2015:426. Available from: http://scholarlycommons.law.northwestern.edu/njlsp/vol10/iss2/4.
5. Smith JJ, Berlin L. The HIV-positive patient and confidentiality. Am. J. Roentgenol. 2001;176(3):599–602. doi:10.2214/ajr.176.3.1760599
6. Joint United Nations Programme on HIV/AIDS(2006).Guidelines on protecting the confidentiality and security of HIV information: proceedings from a workshop. Available from: https://refworld.org/pdfid/467f8cfc2.pdf.
7. Prabhas Maurya. Editorial note on HIV stigma in the world. J AIDS Clin Res 12 (2020):831.Available from https://www.hilarispublisher.com/open-access/hiv-stigma.pdf
8. Aquino C, Secker MJ, Wood N. HIV/AIDS-related ethical dilemma of confidentiality. Availabe from https://www.tc.columbia.edu/publications/gsjp/gsjp-volumes-archive/gsjp-volume-11-2009/11333 V11Article7.pdf.
9. Khac Hai N, Lawpoolsri S, Jittamala P, Thi Thu HP, Kaewkungwal J. Practices in security and confidentiality of HIV/AIDS patients’ information: a national survey among staff at HIV outpatient clinics in Vietnam. PLoS One. 2017;12(11):e0188160. doi:10.1371/journal.pone.0188160
10. Carr, D., R. Kidd, M. Fitzgerald, and L. Nyblade. 2015.Achieving a Stigma-free Health Facility and HIV Services: ISBN:978-1-59560-095-0. Available from: https://www.healthpolicyproject.com/pubs/281 SDAdminitratorGuide.pdf.
11. Fido NN, Aman M, Brihnu Z. HIV stigma and associated factors among antiretroviral treatment clients in Jimma town, Southwest Ethiopia. HIVAIDS - Res Palliat Care. 2016;8:183–193. doi:10.2147/HIV.S114177
12. Iwuagwu S, Durojaye E, Oyebola B, Oluduro B, Ayankogbe O. HIV/AIDS and human rights in Nigeria. -UNESCO HIV and health education publication. policy- center for the rights to health for policy project; 2003.
13. Bayisa L, Tadesse A, Reta MM, Gebeye E. Prevalence and factors associated with delayed initiation of antiretroviral therapy among people living with HIV in Nekemte Referral Hospital, Western Ethiopia. HIVAIDS Auckl NZ. 2020;12:457–465.
14. Birhan W, Giday M, Teklehaymanot T. The contribution of traditional healers’ clinics to public health care system in Addis Ababa, Ethiopia: a cross-sectional study. J Ethnobiol Ethnomedicine. 2011;7(1):39. doi:10.1186/1746-4269-7-39
15. Capon DJ, Ward RH. The CD4-gp120 interaction and AIDS pathogenesis. Annu Rev Immunol. 1991;9(1):649–678. doi:10.1146/annurev.iy.09.040191.003245
16. Mengiste M, Ahmed MH, Bogale A, Yilma T. Information-seeking behavior and its associated factors among patients with diabetes in a resource-limited country: a cross-sectional study. Diabetes Metab Syndr Obes Targets Ther. 2021;14:2155. doi:10.2147/DMSO.S289905
17. Biswas S, Syiemlieh J, Nongrum R, Sharma S, Siddiqi M. Impact of educational level and family income on breast cancer awareness among college-going girls in Shillong (Meghalaya), India. Asian Pac J Cancer Prev. 2020;21(12):3639. doi:10.31557/APJCP.2020.21.12.3639
18. Belete H, Ali T, Mekonen T, Fekadu W, Belete T. Perceived stigma and associated factors among adults with problematic substance use in Northwest Ethiopia. Psychol Res Behav Manag. 2021;14:637. doi:10.2147/PRBM.S301251
19. Exavery A, Charles J, Barankena A, et al. Accelerating caregivers’ HIV status disclosure to community-based lay social welfare volunteers in Tanzania. AIDS Res Ther. 2021;18(1) doi:10.1186/s12981-021-00332-4
20. Association of body mass index with immune recovery, virological failure and cardiovascular disease risk among people living with HIV - Han - 2021 - HIV Medicine. Wiley Online Library. Available from: https://onlinelibrary.wiley.com/doi/10.1111/hiv.13017.
21. Olawepo JO, Pharr JR, Cross CL, et al. Changes in body mass index among people living with HIV who are new on highly active antiretroviral therapy: a systematic review and meta-analysis. AIDS Care. 2021:33:326–336.
22. Chambers LA, Rueda S, Baker DN, et al. Stigma, HIV and health: a qualitative synthesis. BMC Public Health. 2015;15(1):1–17. doi:10.1186/s12889-015-2197-0
23. Smurzynski M, Leone PA, Miller WC. Confidentiality concerns, perceived staff rudeness, and other HIV testing barriers; 2008. Available from: http://jeholine.org/vol1 1/JEH-FORD Article 2.pdf. Accessed January 23,2021
24. Nixon SA, Cameron C, Hanass‐Hancock J, et al. Perceptions of HIV‐related health services in Zambia for people with disabilities who are HIV‐positive. J Int AIDS Soc. 2014;17(1):18806. doi:10.7448/IAS.17.1.18806
25. World Health Organization. Towards universal access: scaling up priority HIV; 2009.
26. Moradi G, Mohraz M, Gouya M, et al. Problems of providing services to people affected by HIV/AIDS: service providers and recipients perspectives. East Mediterr Health J. 2015;21(1):20–28. doi:10.26719/2015.21.1.20
27. Kruse GR, Chapula BT, Ikeda S, et al. Burnout and use of HIV services among health care workers in Lusaka District, Zambia: a cross-sectional study. Hum Resour Health. 2009;7(1):1–10. doi:10.1186/1478-4491-7-55
28. Bemelmans M, Van Den Akker T, Pasulani O, et al. Keeping health staff healthy: evaluation of a workplace initiative to reduce morbidity and mortality from HIV/AIDS in Malawi. J Int AIDS Soc. 2011;14(1):1–7. doi:10.1186/1758-2652-14-1
29. Soumah M, Ouédraogo M, Dia S, Ndiaye M, Fall M, Sow M. Secret médical et VIH/sida au Sénégal: connaissances, pratiques, aspects éthiques et perspectives. Rev Med Leg. 2010;1(3–4):100–108. doi:10.1016/j.medleg.2010.11.001
30. Butt L. Can you keep a secret? Pretences of confidentiality in HIV/AIDS counseling and treatment in Eastern Indonesia. Med Anthropol. 2011;30(3):319–338. doi:10.1080/01459740.2011.560585
31. Tsame O. Keeping patient HIV status confidential: the experiences and perceptions of community members in a public clinic; 2016. Available from:https://openaidsjournal.com/VOLUME/ 12/PAGE/150/PDF/. Accessed: February 20, 2021
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
