Back to Journals » International Journal of Nanomedicine » Volume 18
Application of Single Extracellular Vesicle Analysis Techniques
Authors Zhu J, Wu F, Li C, Mao J, Wang Y, Zhou X, Xie H, Wen C
Received 15 May 2023
Accepted for publication 12 September 2023
Published 20 September 2023 Volume 2023:18 Pages 5365—5376
DOI https://doi.org/10.2147/IJN.S421342
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Anderson Oliveira Lobo
Junquan Zhu, Feifeng Wu,* Cuifang Li,* Jueyi Mao,* Yang Wang,* Xin Zhou,* Haotian Xie,* Chuan Wen
Department of Pediatrics, The Second Xiangya Hospital, Central South University, Changsha, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chuan Wen, Department of Pediatrics, The Second Xiangya Hospital, Central South University, 139 Renmin Middle Road, Changsha, Hunan, 410011, People’s Republic of China, Tel +86-13755191815, Email [email protected]
Abstract: Extracellular vesicles (EVs) are lipid containers that are actively released by cells and contain complex molecular cargoes. These cargoes include abundant material such as genomes and proteins from cells of origin. They are involved in intercellular communication and various pathological processes, showing excellent potential for diagnosing and treating diseases. Given the significant heterogeneity of EVs in complex physiopathological processes, unveiling their composition is essential to understanding their function. Bulk detection methods have been previously used to analyze EVs, but they often mask their heterogeneity, leading to the loss of valuable information. To overcome this limitation, single extracellular vesicle (SEV) analysis techniques have been developed and advanced. These techniques allow for analyzing EVs’ physical information and biometric molecules at the SEV level. This paper reviews recent advances in SEV detection methods and summarizes some clinical applications for SEV detection strategies.
Keywords: single extracellular vesicle analysis, heterogeneity, detection methods, disease diagnosis, new therapies
Introduction
Extracellular vesicles (EVs) are a generic term for encapsulated biomolecules released by cells into their surroundings, including exosomes, microvesicles, incomes, and apoptotic bodies, among other names.1 EVs are widely present in body fluids,2 including blood, urine, amniotic fluid, breast milk, semen, saliva, and malignant fluid, making them easily accessible for study.3 The plasma membrane structure of EVs enhances the stability of internal biomolecules, biofilm shuttle potential, and biocompatibility.4 Moreover, they have the unique capability to cross cellular barriers and enrich sensitive extracellular proteins, making them a valuable tool for remote intercellular communication in vivo.5 Consequently, EVs’ molecular composition is closely related to the physiological state of their cargo and parental cells and can serve as valuable biomarkers for various diseases.
However, studies of EVs have revealed that they were heterogeneous in size and molecular composition, which prompted the need to analyze single extracellular vesicle (SEV) to unravel their heterogeneity.6 Commonly techniques such as Western Blot and real-time PCR have been used to analyze the population of EVs rather than SEV.7,8 These analysis methods poorly characterize individual vesicles’ structure, composition, thereby potentially leading to biased results.9 Therefore, researchers have developed more than 20 new single-vesicle analysis techniques for more accurate subclassification and characterization of EVs.10 These techniques enable the analysis of physical morphology and specific biomolecules at the SEV level, better analyzing the heterogeneity of EVs and facilitating the understanding of the EVs’ role in disease development. Although these techniques helped us to understand SEV better, they require further refinement and development to overcome their limitations, such as insufficient resolution and low throughput.11 Recent advancements in the analysis of SEV, however, offer new opportunities to design new diagnostic devices for small sample sizes using non-invasive or minimally invasive methods. Based on these advancements, we will objectively evaluate the advantages and disadvantages of some methods for SEV and their potential applications.
Characterization Techniques for SEV
SEV Physical Characterization
The most prevalent method is a size-based classification of EVs.12 The International Society for Extracellular Vesicles (ISEV) guidelines for SEV characterization emphasize the importance of the physical properties of SEV.13 Hence, in single vesicle analysis, it is imperative to consider the physical parameters of individual vesicles, including their size, distribution, concentration, and morphology. To this end, techniques such as nanoparticle tracking analysis (NTA) have played a vital role in characterizing the physical parameters of SEV. This section provides a comprehensive overview of the principles behind several technologies and recent technological advancements (Table 1).
 |
Table 1 Summary of the SEV Characterization Techniques |
High-Resolution Microscopy Techniques
High-resolution microscopy techniques, including electron microscopy (EM) and atomic force microscopy (AFM), have enabled the direct visualization of EVs for morphological particle size characterization. EM operates by emitting a high-energy electron beam that interacts with the atoms in the sample to reveal fine internal structural details.14 This method includes various techniques broadly categorized into scanning electron microscopy (SEM) and transmission electron microscopy (TEM), with the latter being the most common for single vesicle analysis. However, sample preparation for these techniques requires heavy metal staining and fixation, which can compromise the structure and integrity of the EVs’ membranes.15,16 Cryogenic transmission electron microscopy (cryo-TEM) can overcome this challenge by eliminating the need for contrast agents or developers and the dehydration step. Although this approach yields low-resolution images, it shows the natural state of individual vesicles.17 Combining a second electron source into a low-energy electron microscope (LEEM) setup allowed for developing TEM at low energy for imaging and spectroscopy in transmission and reflection modes at nanometer (nm) resolution.18 This technique prevents high-energy electrons from damaging fragile biological samples and enables nondestructive imaging of biological samples at nanometer resolution. However, Rikkert et al found that operator subjectivity significantly affected the results, in addition to the different working protocols.19 Researchers recently proposed a software tool for the computer-aided assessment of SEV in TEM images.20 This algorithm can analyze SEV based on semi-automatic detection, which may be the first step in developing a standard protocol.
AFM is another method that characterizes the overall physical attributes of a sample through the interaction between a nano-tip probe and the immobilized sample by aggregating readings of individual vesicles to obtain images of the mechanical properties of the subpopulation.20 The fluidic AFM combines ordinary AFM with microchannel and pressure control into a complete complex, enabling the resolution of EVs secreted in individual cells. A recent paper describes the SEV analysis technique under optical microscopy - peak force knockdown (PFT) mode.21 This method immobilizes EVs in a microfluidic chamber for immunostaining and imaging, reducing the signal-to-noise ratio when the vesicles are in solution or floating freely in flow conditions. However, the low throughput is one of the most significant drawbacks of this technique. Ridolfi et al developed AFM analysis software that can analyze hundreds of EVs in less than an hour using a general AFM device to address this challenge.22 Recently, Gazze et al have also developed AFM analysis software to help researchers with their analysis, and the analysis data can be shared to build a common database.23 Nevertheless, the current research comparing these applications needs to be improved. Furthermore, the high cost of instrumentation and stringent technical requirements (eg, high sample concentration required, complex pre-processing of samples) limit the application of microscopic imaging techniques for SEV characterization. Additionally, the low throughput of these techniques poses challenges for the rapid characterization of SEV.
Nanoparticle Tracking and Tunable Resistive Pulse Sensing Analysis
NTA and tunable resistive pulse sensing (TRPS) are commonly used to estimate the size distribution and density of EVs. NTA is a rapid analysis technique based on the Brownian motion of suspended particles, enabling determining EV size distribution and concentration.24 The technique irradiates the particles by scattering and tracking the recorded laser beam, subsequently capturing photographs and traces and analyzing the Brownian motion trajectory of the EVs. The diffusion coefficient is then calculated to obtain the hydrated particle size of the EVs using the Stokes-Einstein equation. The concentration of EVs can be calculated from the number of particles observed within the field of view. However, it should be noted that NTA devices, such as NanoSight NS300 and ZetaView, can differ significantly in terms of hardware and software, affecting measurement results.25 In particular, ZetaView has been found to provide more accurate and reproducible detection of EV concentrations, while NanoSight NS300 provides higher resolution size measurements. Furthermore, NTA technology can be used in fluorescent mode to quantify specific proteins and nucleic acids of EVs by introducing fluorescent markers such as membrane dyes and immunofluorescent antibodies.26,27 Despite these advantages, NTA particle size measurements may be more extensive than actual values, and the particle size distribution can be more comprehensive than the accurate distribution.
TRPS is a technique that utilizes the Coulter effect to determine the particle size distribution and concentration of EVs in solution.28 TRPS detects a transient drop in ionic current as the EVs pass through the nanopores of a polyurethane membrane. The current drop’s magnitude correlates with the EVs’ particle size, enabling the determination of the particle size distribution. Nevertheless, it is essential to note that TRPS is vulnerable to nanopore clogging and background noise caused by non-EV particles,29 necessitating further optimization and calibration of system parameters.30
SEV Biochemical Characterization
EVs consist mainly of transmembrane or lipid-bound extracellular and cytoplasmic proteins from their parental cells, resulting in different protein compositions of SEV subpopulations.31,32 Therefore, the protein fractions of EVs are the significant bearers of single vesicle functioning and transmitting information. Furthermore, previous studies have shown that nucleic acids in EVs exhibit significant diversity and correlate with the type and staging of disease.33,34 Hence, biomolecular analysis of SEV is a stepping stone to a deeper understanding of single vesicles and holds promise for diagnosing many diseases (especially cancer), predicting and monitoring therapeutic responses, and real-time assessment of disease progression. Here we present some of the widely used techniques for biomolecular analysis (Table 1).
Flow Cytometry
Flow cytometry (FCM) is an advanced technique widely used in clinical and scientific research for the rapid characterization, quantitative analysis, or sorting of cells. It has also been used for the single-particle multi-parameter quantification of EVs.35 Pol et al reported that the scattered light signal of most small particle-size EVs was drowned out by the background signal when EVs were analyzed by FCM.36 Researchers found that fluorescent triggering had a higher signal-to-noise ratio than scattering triggering and that labeling EVs with lipid film dyes or immunofluorescent antibodies improves FCM function.37 However, FCM based on signal amplification lacks a universal fluorescent probe for selectively labeling EVs. It does not enable quantitative analysis of individual EVs’ low-copy proteins, nucleic acids, etc. To address these issues, Shen et al established a signal amplification-based flow cytometry protocol that employs a nucleic acid aptamer to identify specific antigens on the surface of EVs.38 The aptamer triggers a hybridization chain reaction (HCR), which expands the particle size of individual EVs to 500 nm and combines a large number of fluorescent probes to achieve simultaneous amplification of the scattering and fluorescence signals of individual EV. The nano-flowcytometry (nFCM), developed by Prof. Yan Xiaomei’s group, combines Rayleigh light scattering with sheath flow single-molecule fluorescence detection technology, significantly improving the sensitivity of both scattering and fluorescence detection compared to conventional FCM.39 The instrument enables multi-parameter quantitative analysis of SEV down to 40 nm particle size, with analysis rates of up to 10,000 particles per minute.40 Nevertheless, the clinical application of FCM is limited by the need for highly sophisticated instrumentation and expertise.
Droplet Digital Analysis
Droplet digital analysis (DDS) methods mostly use microdrop microfluidics to randomly assign SEV to individual microdroplets and perform absolute quantification of EV biomolecules based on enzyme-linked immunosorbent assay (ELISA) or DNA calculation techniques. Liu et al have developed a microdroplet-based digital detection platform called ExoELISA,41 which can detect up to five EVs per µL based on the ELISA principle. Yang et al have developed the digital extracellular vesicle screening technology (DEST),42 which incorporated microdroplet generation, processing, and analysis to increase detection throughput to over 100 times that of conventional droplet microfluidics, with a start-to-finish analysis time of fewer than two hours and the ability to process hundreds of samples per day. These techniques hold great promise for accurately quantifying rare subpopulations of EVs in complex environments, thereby demonstrating the significant potential for clinical application in disease diagnosis and prognosis. Moreover, Li’s team has developed a thermophoresis-mediated DNA computation technique that identifies single exosome bimolecularmarkers.43 In this method, two aptamer probes hybridize to the same linked probe, and fluorescence is exhibited when both target molecules are present on the EVs. Proximity barcoding assay (PBA) is a newly developed digital method that enables the simultaneous characterization of multiple proteins on SEV.44 This technique involves coupling a different DNA-encoded tag to each antibody, followed by an enzyme-linked hybridization reaction and PCR amplification, resolving protein information contained in the DNA sequence-generation sequencing technology. The sequence information can then be translated into protein information for individual EVs. PBA can enable the simultaneous characterization of over 30 protein molecules on a single EV and significantly improve the diagnosis of diseases by sequencing multiple proteins at the single vesicle level on digital microfluidic. Nevertheless, the above methods require intricate experimental designs and operational procedures, including tasks such as sample processing, labeling, reactions, and analysis. These processes may be highly specialized and time and resource intensive.
Fluorescence Microscopy Imaging Techniques
Fluorescence microscopy is a widely used technique for characterizing EVs regarding their secretion pathways, transport processes, and uptake mechanisms. Total internal reflection fluorescence microscopy (TIRF) is the most commonly used single-molecule fluorescence imaging technique for the characterization of proteins and nucleic acids of EVs.45,46 Cui’s team developed a method that combined the TIRF platform with DNA dot accumulation nanoscale topography imaging to quantify specific SEV proteins using complementary strand transient hybridization and dissociation processes accompanied by fluorescence “scintillation” times.47 Their innovation involves using machine learning algorithms for cancer typing detection, achieving an accuracy of up to 100%. The high-throughput nano-biochip integrated system for liquid biopsy (HNCIB) developed by Zhou et al enables the simultaneous characterization of surface proteins and internal mRNA/miRNA of EVs on a TIRF imaging platform.48
Super-resolution microscopy (SRM) is a fluorescence microscopy technique based on the optical principles of classical optical microscopy. SRM techniques are divided into excitation-patterning methods and single-molecule localization methods,10,49 depending on the operation mechanism, with the latter being more widely used. Single-molecule localization methods, such as direct stochastic optical reconstruction microscopy (d-STORM) and photoactivation localization microscopy (PALM), have successfully achieved single-molecule fluorescence imaging of EVs. PALM has been implemented for single-molecule fluorescence imaging of EVs. Single-molecule localization methods can be combined with TIRF to improve the signal-to-noise ratio and shorten the imaging time.50 However, super-resolution fluorescence microscopy requires sophisticated instrumentation and powerful data processing software, often with low throughput. Despite the pivotal role played by the fluorescence microscopy techniques discussed above in exploring EV secretion and characterization and uptake mechanisms, fluorescent markers may interfere with their localization, activity, and function. Additionally, lipid markers may be non-specific for labeling or dye aggregation.51
Raman Spectroscopy Analysis
Raman tweezer microspectroscopy (RTM) utilizes inelastic scattering to characterize the chemical bonds present within a substance and obtain information on the constituent biomolecules. This technique analyzes subgroups’ concentration and density based on SEV components’ biomolecular composition. Previous studies have confirmed that laser tweezers raman spectroscopy (LTRS) can distinguish EVs from normal and cancer cells. These differences mainly arise from the relative levels of phospholipids and cholesterol.52,53 However, the working principle of RTM has two main drawbacks.53 Firstly, the chemical bond composition within matter is similar, leading to low resolution. Secondly, the scattering efficiency usually could be much higher in a relatively low level of Raman signal information. To overcome these limitations, researchers have proposed the Raman spectroscopy metabolic labeling technique, which changes the composition of matter isotopes to increase RTM resolution.54 However, this technique must address the disadvantage of slow RTM imaging speed. A recent study described a new generation of automated single-particle raman capture analysis (SPARTA).55 This SPARTA system is optimized for analysis and provides a more convenient and comprehensive comparison of multiple EVs’ spectroscopy methods. Notably, this method achieves high throughput with a limit of only 10 seconds to complete the information acquisition and analysis.
Surface Plasma Resonance Technology
The surface plasmon resonance (SPR) technique can record the oscillation of electrons caused by the binding of a recording target to a substrate under incident light irradiation and analyze the spectral shift and intensity change for label-free detection. This technique has been refined and applied to the analytical characterization of EV proteins and nucleic acids.29,56 The nanoplasmon-enhanced scattering (nPES) platform developed by Liang et al enables the analysis of SEV in only 1 μL of plasma samples to achieve good differentiation between healthy individuals, patients with pancreatic cancer, and patients with pancreatitis.57 The nPLEX platform replaces the total internal reflection of incident light with light transmission through periodic nanopores, another SPR technology.58 nPLEX offers significantly higher detection sensitivity, and they have designed ligand-functionalized channel arrays for the simultaneous detection of SEV protein markers in microfluidic chips. nPLEX has a minimum detection limit of 3000 EVs in less than 30 minutes. Based on the nPLEX platform, Shao et al developed an amplified plasma exosome platform to increase detection sensitivity to 200 EVs.59 However, it is important to note that the challenging aspect of mitigating the drawbacks of SPR is the interference of non-specific bindings on the outcome signals.
Interference Correlation Microscopy
The single particle interferometric reflectance imaging sensor (SP-IRIS) is a technique that utilizes the interference signal of two reflected beams of light from a substrate and a nanoparticle source to achieve real-time imaging of nanoparticles.60 It enables the detection of SEV-enhanced scattering signals for particle size and concentration characterization analysis.61 Nano View Biosciences has developed ExoView, a fully automated exosome fluorescence detection and analysis system based on SP-IRIS in fluorescence mode, which enables fluorescence co-localization analysis of multiple proteins on the SEV.62,63 This system can accurately count and differentiate individual vesicles. However, Arab et al pointed out that SP-IRIS does not provide an accurate quantitative analysis of EV concentration compared to single-particle characterization techniques such as NTA.63 This could be attributed to the lateral resolution of the microscope (~400 nm), which can accommodate several small vesicles that may be mistaken for a giant vesicle, particularly in highly concentrated samples.
Clinical Application of SEV
Precision medicine advocates for the implementation of personalized molecular diagnostic and treatment methods in clinical practice. EVs, due to their heterogeneity and key role in disease diagnosis and treatment, have prompted researchers to explore their potential as a new star in molecular detection in precision medicine.64 The detection of SEV has been proven helpful for early disease diagnosis, especially for tumor classification and staging (Table 2). On the other hand, EVs as tools for disease treatment have become a new hot spot. This section outlines recent attempts at the clinical application of single vesicle analysis.
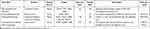 |
Table 2 Summary of Diagnosis of Diseases |
Diagnosis of Diseases
Colorectal cancer continues to pose a significant health threat with high mortality rates worldwide.65 There is a need for better acceptance of available screening and diagnostic methods.66 Recently, researchers have developed a new single microbead fluorescent aptamer sensor that incorporates DNA aptamers capable of explicitly binding SEV surface proteins and individual microbeads capable of immunosorbent EVs.67 This technique allows for the rapid and straightforward detection of 4.9×104 vesicles per microliter sample without further signal amplification reactions. Clinical trials have demonstrated the ability of this method to directly detect exosomes from 2 μL plasma samples, showing that the level of CD63, EpCAM double-positive exosomes are higher in cancer patients than in healthy controls. This assay is sensitive, reliable, requires a small sample, and has excellent potential for developing simple diagnostic tools for clinical applications. Another study reported that high-sensitivity FCM established using improved FCM found significantly higher levels of CD147-positive EVs of rectal cancer origin as a potential marker.40 The advantage of this technique is the ability to demonstrate the proportion of EVs with positive specific protein markers for further quantitative analysis.
Breast cancer is a major health concern and a leading cause of mortality in women worldwide. Due to the high heterogeneity of breast cancer, identifying the receptor status of breast cancer cells is crucial for effective treatment strategies and prognosis.68 In a recent study, Chunchen Liu et al developed a droplet digital ExoELISA method to detect GPC-1(+) exosomes in clinical samples from healthy individuals, patients with benign breast disease, breast cancer patients, and post-breast cancer patients.41 The results showed that GPC-1 expression was significantly higher in tumor-derived exosomes compared to normal and benign breast disease samples, and breast cancer patients had a higher level of GPC-1(+) exosomes than healthy controls and benign breast disease patients. The droplet digital ExoELISA method demonstrated unprecedented accuracy and high specificity in exosome quantification, with a detection limit of at least ten exosomes per microliter. In another study, researchers developed a thermophoresis-mediated DNA algorithm for the bimolecular detection of secretory exosomes in breast cancer cells using two markers with high selectivity and affinity for HER2, the DNA aptamer of EpCAM.43 The results showed high accuracy in classifying breast cancer versus healthy individuals and HER2+BC versus HER2-BC, with 97% and 90% accuracy, respectively. These findings indicate the potential of exosome-based diagnostics for breast cancer detection and monitoring.
Pancreatic cancer is a highly aggressive and lethal disease with a high mortality rate.69 Current diagnostic methods are limited, and further exploration of more accurate and convenient detection methods is needed to improve patient outcomes. In this regard, Yang et al employed a novel ultrasensitive digital extracellular vesicle screening technique (DEST) to identify potential biomarkers of EVs secreted by cell lines derived from patients with intraductal papillary mucinous neoplasms.42 Their study identified MUC5AC as a potential biomarker that showed significantly higher levels in high-grade lesions (82% specificity, 100% sensitivity) compared to other EV markers, such as MUC1 and MUC2. These findings were further validated in a separate cohort, indicating the potential of MUC5AC as a reliable biomarker for pancreatic cancer diagnosis. To improve the accuracy of EV detection, the researchers used an amplification strategy of bivalent cholesterol-modified RNA-DNA double-stranded nucleic acid (AbMB-biChol) labeling, which effectively converted the EV signal into an amplified RNA signal.70 The EVs secreted by pancreatic cancer were recognized by four independent AbMB-biChol antibodies modified with EGFR, EpCAM, GPC1, and EphA2, respectively. The results showed that the combination of the four labeled proteins had superior accuracy (AUC=0.909) compared to the isolated platform bound to a single antibody or the commonly used serum biomarker CA19-9 (AUC=0.714). However, no significant differences were observed in these four markers’ plasma protein expression levels between pancreatic cancer patients and healthy donors. This novel technique has a limit of detection (LOD) of 10 particles per microliter. These results suggest the potential of the combination of MUC5AC and AbMB-biChol labeling as a diagnostic tool for pancreatic cancer.
Potential for Treatment
Researchers have observed an elevated secretion of exosomes during drug-induced angiogenesis, indicating the potential therapeutic value of exosomes in this context.71 And the clinical efficacy of EVs obtained from different sources has been demonstrated.72,73 However, the practical application of EVs in clinical settings remains challenging due to the heterogeneity and low yield. Nevertheless, the unique ability of EVs to traverse biological barriers, evade immune clearance, and be targeted makes them promising tools for drug delivery.74–76 Excitingly, studies have shown that drug-loaded vesicles can effectively combat cancer.77 Nonetheless, the need for nano-characterization techniques hampers this process since vesicle preparation often results in heterogeneity. SEV analysis can analyze nanoparticle cargo at the individual particle level, which aids in the quality assessment of their clinical application. Researchers have employed automated SPARTA to demonstrate that this technology can accurately characterize single-vesicle cargo information and determine whether SEV is loaded with active ingredients.78 Additionally, another study introduced a high-throughput method for the absolute quantification of liposomal nanomedicine particle size, drug content, drug encapsulation fraction, and particle concentration at the single-particle level using nFCM.79 Utilizing single-vesicle technology is crucial for producing and evaluating therapeutic EVs, but further studies are still needed to explore its potential fully.
Another promising idea is the discovery of new therapeutic targets at SEV. The involvement of EVs in various diseases, especially tumors, has been extensively studied.80 Studies have shown that drugs targeting EVs occurrence can reduce tumor growth or metastasis.81,82 However, these drugs are non-specific and may also block beneficial vesicle communication, leading to adverse effects. So far, no research has identified drugs that can act specifically at the level of SEV. Utilizing SEV analysis techniques can be instrumental in analyzing EVs’ heterogeneity at the single-vesicle level. This approach may lead to discovering new targets for a novel therapeutic approach. Researchers can identify more precise and effective therapeutic strategies by understanding the cargo and functions of individual vesicles.
Outlook
Significant advancements have been achieved in SEV analysis techniques. However, despite using the same SEV analysis technique in various studies, significant discrepancies are apparent in the results across these different research endeavors. This divergence in outcomes poses challenges in assessing and comparing differential results, impeding SEV research’s broader adoption. Consequently, while refining SEV analysis techniques, a crucial focus should be placed on addressing the vital research concern of standardization.
EVs, serving as vehicles for cell communication, can be likened to a language that reflects the body’s condition. Consequently, alterations in EVs can serve as indicators for diagnosing diseases. The availability of extracellular vesicles from various bodily fluids has paved the way for developing diagnostic techniques centered around SEV analysis, facilitating precision medicine.83 This approach leverages longitudinal sampling of individuals over time to provide valuable insights into the dynamic evolution of disease states. The impact of SEV on disease diagnosis has been empirically demonstrated to offer heightened accuracy and sensitivity compared to conventional methods.84 However, it is essential to highlight that these detection techniques still necessitate robust clinical data support to establish their reliability.
EVs are carriers of material exchange, facilitating the transport of beneficial and harmful substances. Numerous efforts have been made to increase EVs production for therapeutic purposes, using them to deliver substances with health benefits or as drug carriers.85 However, what needs to be considered is the potential harm caused by the overproduction of these EVs. A study has shown that cells that inhibit autophagy secrete more EVs, which may be due to the need for excessive production of EVs to transport cellular waste.86 In addition, another study has shown that increased EV secretion under inflammatory conditions raises concerns about whether increased EV production may trigger an inflammatory response.87 SEV analysis techniques must effectively identify these potentially harmful substances before they can be used clinically. However, limited studies apply SEV analysis techniques to ensure quality control of therapeutic EVs. Addressing this knowledge gap is critical to ensuring the safety and efficacy of EV-based therapies.
In conclusion, this article provides an overview of the cutting-edge advancements in SEV analysis. The evolution of SEV technologies has elucidated distinct molecular attributes within cell-specific EVs, encompassing a range of physical and biological characteristics such as vesicle size, origin, and content. Through the SEV analysis, diseases can be diagnosed and treated, thereby fostering the pioneering clinical utilization of EVs.
Abbreviations
EVs, extracellular vesicles; SEV, single extracellular vesicle; NTA, nanoparticle tracking analysis; AFM, atomic force microscopy; SEM, scanning electron microscopy; TEM, transmission electron microscopy; cryo-TEM, cryogenic transmission electron microscopy; TRPS, tunable resistive pulse sensing; FCM, flow cytometry; nFCM, nano-flowcytometry; DDS, droplet digital analysis; DEST, digital extracellular vesicle screening technology; PBA, Proximity barcoding assay; TIRF, total internal reflection fluorescence microscopy; SRM, super-resolution microscopy; d-STORM, direct stochastic optical reconstruction microscopy; PALM, photoactivation localization microscopy; RTM, raman tweezer microspectroscopy; LTRS, laser tweezers raman spectroscopy; SPARTA, single-particle raman capture analysis; SPR, surface plasmon resonance; nPES, nanoplasmon-enhanced scattering; SP-IRIS, single particle interferometric reflectance imaging sensor.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 82070758), Hunan Provincial Key R&D Program Project (No. 2020SK2084).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Kontopoulou E, Strachan S, Reinhardt K, et al. Evaluation of dsDNA from extracellular vesicles (EVs) in pediatric AML diagnostics. Ann Hematol. 2020;99(3):459–475. doi:10.1007/s00277-019-03866-w
2. Colombo M, Raposo G, Thery C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Dev Biol. 2014;30:255–289. doi:10.1146/annurev-cellbio-101512-122326
3. Nanou A, Mol L, Coumans FAW, Koopman M, Punt CJA, Terstappen L. Endothelium-derived extracellular vesicles associate with poor prognosis in metastatic colorectal cancer. Cells. 2020;9(12):2688. doi:10.3390/cells9122688
4. Agarwal V, Yadav SS, Kumar S, et al. Evaluating the role of extracellular vesicles as a biomarker under transmission electron microscope in prostate cancer and benign prostate hyperplasia patients. Urologia. 2022;89(2):210–215. doi:10.1177/03915603211018677
5. Kanada M, Bachmann MH, Hardy JW, et al. Differential fates of biomolecules delivered to target cells via extracellular vesicles. Proc Natl Acad Sci USA. 2015;112(12):E1433–42. doi:10.1073/pnas.1418401112
6. Martinez MC, Andriantsitohaina R. Extracellular vesicles in metabolic syndrome. Circ Res. 2017;120(10):1674–1686. doi:10.1161/CIRCRESAHA.117.309419
7. Tkach M, Kowal J, Thery C. Why the need and how to approach the functional diversity of extracellular vesicles. Philos Trans R Soc Lond B Biol Sci. 2018;373(1737):20160479. doi:10.1098/rstb.2016.0479
8. Willms E, Cabanas C, Mager I, Wood MJA, Vader P. Extracellular vesicle heterogeneity: subpopulations, isolation techniques, and diverse functions in cancer progression. Front Immunol. 2018;9:738. doi:10.3389/fimmu.2018.00738
9. Mathiasen S, Christensen SM, Fung JJ, et al. Nanoscale high-content analysis using compositional heterogeneities of single proteoliposomes. Nat Methods. 2014;11(9):931–934. doi:10.1038/nmeth.3062
10. Panagopoulou MS, Wark AW, Birch DJS, Gregory CD. Phenotypic analysis of extracellular vesicles: a review on the applications of fluorescence. J Extracell Vesicles. 2020;9(1):1710020. doi:10.1080/20013078.2019.1710020
11. Shao H, Im H, Castro CM, Breakefield X, Weissleder R, Lee H. New technologies for analysis of extracellular vesicles. Chem Rev. 2018;118(4):1917–1950. doi:10.1021/acs.chemrev.7b00534
12. Bordanaba-Florit G, Royo F, Kruglik SG, Falcon-Perez JM. Using single-vesicle technologies to unravel the heterogeneity of extracellular vesicles. Nat Protoc. 2021;16(7):3163–3185. doi:10.1038/s41596-021-00551-z
13. Thery C, Witwer KW, Aikawa E, et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7(1):1535750. doi:10.1080/20013078.2018.1535750
14. Pascucci L, Scattini G. Imaging extracellular vesicles by transmission electron microscopy: coping with technical hurdles and morphological interpretation. Biochim Biophys Acta Gen Subj. 2021;1865(4):129648. doi:10.1016/j.bbagen.2020.129648
15. Jeppesen DK, Fenix AM, Franklin JL, et al. Reassessment of exosome composition. Cell. 2019;177(2):428–445 e18. doi:10.1016/j.cell.2019.02.029
16. Kim G, Kim M, Lee Y, Byun JW, Hwang DW, Lee M. Systemic delivery of microRNA-21 antisense oligonucleotides to the brain using T7-peptide decorated exosomes. J Control Release. 2020;317:273–281. doi:10.1016/j.jconrel.2019.11.009
17. Zabeo D, Cvjetkovic A, Lasser C, Schorb M, Lotvall J, Hoog JL. Exosomes purified from a single cell type have diverse morphology. J Extracell Vesicles. 2017;6(1):1329476. doi:10.1080/20013078.2017.1329476
18. Neu PS, Geelen D, Thete A, Tromp RM, van der Molen SJ. Complementary LEEM and eV-TEM for imaging and spectroscopy. Ultramicroscopy. 2021;222:113199. doi:10.1016/j.ultramic.2020.113199
19. Rikkert LG, Nieuwland R, Terstappen L, Coumans FAW. Quality of extracellular vesicle images by transmission electron microscopy is operator and protocol dependent. J Extracell Vesicles. 2019;8(1):1555419. doi:10.1080/20013078.2018.1555419
20. Kotrbová A, Štěpka K, Maška M, et al. TEM ExosomeAnalyzer: a computer-assisted software tool for quantitative evaluation of extracellular vesicles in transmission electron microscopy images. J Extracell Vesicles. 2019;8(1):1560808. doi:10.1080/20013078.2018.1560808
21. Li MI, Xu X, Xi N, Wang W, Xing X, Liu L. Multiparametric atomic force microscopy imaging of single native exosomes. Acta Biochim Biophys Sin. 2021;53(3):385–388. doi:10.1093/abbs/gmaa172
22. Ridolfi A, Brucale M, Montis C, et al. AFM-based high-throughput nanomechanical screening of single extracellular vesicles. Anal Chem. 2020;92(15):10274–10282. doi:10.1021/acs.analchem.9b05716
23. Gazze SA, Thomas SJ, Garcia-Parra J, et al. High content, quantitative AFM analysis of the scalable biomechanical properties of extracellular vesicles. Nanoscale. 2021;13(12):6129–6141. doi:10.1039/d0nr09235e
24. Szatanek R, Baj-Krzyworzeka M, Zimoch J, Lekka M, Siedlar M, Baran J. The methods of choice for Extracellular Vesicles (EVs) characterization. Int J Mol Sci. 2017;18(6). doi:10.3390/ijms18061153
25. Bachurski D, Schuldner M, Nguyen PH, et al. Extracellular vesicle measurements with nanoparticle tracking analysis - An accuracy and repeatability comparison between NanoSight NS300 and ZetaView. J Extracell Vesicles. 2019;8(1):1596016. doi:10.1080/20013078.2019.1596016
26. Kwon Y, Park J. Methods to analyze extracellular vesicles at single particle level. Micro Nano Syst Lett. 2022;10(1):14. doi:10.1186/s40486-022-00156-5
27. Sun L, Meckes DG. Methodological approaches to study extracellular vesicle miRNAs in Epstein–Barr virus-associated cancers. Int J Mol Sci. 2018;19(9):2810. doi:10.3390/ijms19092810
28. Vogel R, Coumans FA, Maltesen RG, et al. A standardized method to determine the concentration of extracellular vesicles using tunable resistive pulse sensing. J Extracell Vesicles. 2016;5:31242. doi:10.3402/jev.v5.31242
29. Akers JC, Ramakrishnan V, Nolan JP, et al. Comparative analysis of technologies for quantifying Extracellular Vesicles (EVs) in Clinical Cerebrospinal Fluids (CSF). PLoS One. 2016;11(2):e0149866. doi:10.1371/journal.pone.0149866
30. Weatherall E, Willmott GR. Applications of tunable resistive pulse sensing. Analyst. 2015;140(10):3318–3334. doi:10.1039/c4an02270j
31. Kowal J, Arras G, Colombo M, et al. Proteomic comparison defines novel markers to characterize heterogeneous populations of extracellular vesicle subtypes. Proc Natl Acad Sci USA. 2016;113(8):E968–77. doi:10.1073/pnas.1521230113
32. van Niel G, D’Angelo G, Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat Rev Mol Cell Biol. 2018;19(4):213–228. doi:10.1038/nrm.2017.125
33. Veziroglu EM, Mias GI. Characterizing extracellular vesicles and their diverse RNA contents. Front Genet. 2020;11:700. doi:10.3389/fgene.2020.00700
34. Tsering T, Li M, Chen Y, et al. EV-ADD, a database for EV-associated DNA in human liquid biopsy samples. J Extracell Vesicles. 2022;11(10):e12270. doi:10.1002/jev2.12270
35. Choi D, Montermini L, Jeong H, Sharma S, Meehan B, Rak J. Mapping subpopulations of cancer cell-derived extracellular vesicles and particles by nano-flow cytometry. ACS Nano. 2019;13(9):10499–10511. doi:10.1021/acsnano.9b04480
36. Cheung CK, Rajasekaran A, Barratt J, Rizk DV. An update on the current state of management and clinical trials for IgA nephropathy. J Clin Med. 2021;10(11):2493. doi:10.3390/jcm10112493
37. Parveen S, Misra R, Sahoo SK. Nanoparticles: a boon to drug delivery, therapeutics, diagnostics and imaging. Nanomedicine. 2012;8(2):147–166. doi:10.1016/j.nano.2011.05.016
38. Shen W, Guo K, Adkins GB, et al. A single Extracellular Vesicle (EV) flow cytometry approach to reveal EV heterogeneity. Angew Chem Int Ed Engl. 2018;57(48):15675–15680. doi:10.1002/anie.201806901
39. Zhu S, Ma L, Wang S, et al. Light-scattering detection below the level of single fluorescent molecules for high-resolution characterization of functional nanoparticles. ACS Nano. 2014;8(10):10998–11006. doi:10.1021/nn505162u
40. Tian Y, Ma L, Gong M, et al. Protein profiling and sizing of extracellular vesicles from colorectal cancer patients via flow cytometry. ACS Nano. 2018;12(1):671–680. doi:10.1021/acsnano.7b07782
41. Liu C, Xu X, Li B, et al. Single-exosome-counting immunoassays for cancer diagnostics. Nano Lett. 2018;18(7):4226–4232. doi:10.1021/acs.nanolett.8b01184
42. Yang KS, Ciprani D, O’Shea A, et al. Extracellular vesicle analysis allows for identification of invasive IPMN. Gastroenterology. 2021;160(4):1345–1358 e11. doi:10.1053/j.gastro.2020.11.046
43. Li Y, Deng J, Han Z, et al. Molecular identification of tumor-derived extracellular vesicles using thermophoresis-mediated DNA computation. J Am Chem Soc. 2021;143(3):1290–1295. doi:10.1021/jacs.0c12016
44. Lin B, Tian T, Lu Y, et al. Tracing tumor-derived exosomal PD-L1 by dual-aptamer activated proximity-induced droplet digital PCR. Angew Chem Int Ed Engl. 2021;60(14):7582–7586. doi:10.1002/anie.202015628
45. He D, Ho SL, Chan HN, et al. Molecular-recognition-based DNA nanodevices for enhancing the direct visualization and quantification of single vesicles of tumor exosomes in plasma microsamples. Anal Chem. 2019;91(4):2768–2775. doi:10.1021/acs.analchem.8b04509
46. He D, Wang H, Ho SL, et al. Total internal reflection-based single-vesicle in situ quantitative and stoichiometric analysis of tumor-derived exosomal microRNAs for diagnosis and treatment monitoring. Theranostics. 2019;9(15):4494–4507. doi:10.7150/thno.33683
47. Chen C, Zong S, Liu Y, et al. Profiling of exosomal biomarkers for accurate cancer identification: combining DNA-PAINT with machine- learning-based classification. Small. 2019;15(43):e1901014. doi:10.1002/smll.201901014
48. Zhou J, Wu Z, Hu J, et al. High-throughput single-EV liquid biopsy: rapid, simultaneous, and multiplexed detection of nucleic acids, proteins, and their combinations. Sci Adv. 2020;6(47). doi:10.1126/sciadv.abc1204
49. Huang B. Super-resolution optical microscopy: multiple choices. Curr Opin Chem Biol. 2010;14(1):10–14. doi:10.1016/j.cbpa.2009.10.013
50. Groveman BR, Orru CD, Hughson AG, et al. Rapid and ultra-sensitive quantitation of disease-associated alpha-synuclein seeds in brain and cerebrospinal fluid by alphaSyn RT-QuIC. Acta Neuropathol Commun. 2018;6(1):7. doi:10.1186/s40478-018-0508-2
51. Nienhaus K, Nienhaus GU. Where do we stand with super-resolution optical microscopy? J Mol Biol. 2016;428(2 Pt A):308–322. doi:10.1016/j.jmb.2015.12.020
52. Su J. Label-free single exosome detection using frequency-locked microtoroid optical resonators. ACS Photonics. 2015;2(9):1241–1245. doi:10.1021/acsphotonics.5b00142
53. Smith ZJ, Lee C, Rojalin T, et al. Single exosome study reveals subpopulations distributed among cell lines with variability related to membrane content. J Extracell Vesicles. 2015;4:28533. doi:10.3402/jev.v4.28533
54. Horgan CC, Nagelkerke A, Whittaker TE, et al. Molecular imaging of extracellular vesicles in vitro via Raman metabolic labelling. J Mater Chem B. 2020;8(20):4447–4459. doi:10.1039/d0tb00620c
55. Penders J, Nagelkerke A, Cunnane EM, et al. Single particle automated raman trapping analysis of breast cancer cell-derived extracellular vesicles as cancer biomarkers. ACS Nano. 2021;15(11):18192–18205. doi:10.1021/acsnano.1c07075
56. Joshi GK, Deitz-McElyea S, Liyanage T, et al. Label-free nanoplasmonic-based short noncoding RNA Sensing at attomolar concentrations allows for quantitative and highly specific assay of microRNA-10b in biological fluids and circulating exosomes. ACS Nano. 2015;9(11):11075–11089. doi:10.1021/acsnano.5b04527
57. Liang K, Liu F, Fan J, et al. Nanoplasmonic quantification of tumor-derived extracellular vesicles in plasma microsamples for diagnosis and treatment monitoring. Nat Biomed Eng. 2017;1:21. doi:10.1038/s41551-016-0021
58. Im H, Shao H, Park YI, et al. Label-free detection and molecular profiling of exosomes with a nano-plasmonic sensor. Nat Biotechnol. 2014;32(5):490–495. doi:10.1038/nbt.2886
59. Lim CZJ, Zhang Y, Chen Y, et al. Subtyping of circulating exosome-bound amyloid beta reflects brain plaque deposition. Nat Commun. 2019;10(1):1144. doi:10.1038/s41467-019-09030-2
60. Trueb J, Avci O, Sevenler D, Connor JH, Unlu MS. Robust visualization and discrimination of Nanoparticles by interferometric imaging. IEEE J Sel Top Quantum Electron. 2017;23(2):6900610. doi:10.1109/JSTQE.2016.2639824
61. Daaboul GG, Gagni P, Benussi L, et al. Digital detection of exosomes by interferometric imaging. Sci Rep. 2016;6:37246. doi:10.1038/srep37246
62. Li M, Soder R, Abhyankar S, et al. WJMSC-derived small extracellular vesicle enhance T cell suppression through PD-L1. J Extracell Vesicles. 2021;10(4):e12067. doi:10.1002/jev2.12067
63. Gori A, Romanato A, Bergamaschi G, et al. Membrane‐binding peptides for extracellular vesicles on-chip analysis. J Extracell Vesicles. 2020;9(1):1751428. doi:10.1080/20013078.2020.1751428
64. Cheng L, Hill AF. Therapeutically harnessing extracellular vesicles. Nat Rev Drug Discov. 2022;21(5):379–399. doi:10.1038/s41573-022-00410-w
65. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
66. Kanth P, Inadomi JM. Screening and prevention of colorectal cancer. BMJ. 2021;374:n1855. doi:10.1136/bmj.n1855
67. Wang F, Zhang Y, Chen D, Zhang Z, Li Z. Single microbead-based fluorescent aptasensor (SMFA) for direct isolation and in situ quantification of exosomes from plasma. Analyst. 2021;146(10):3346–3351. doi:10.1039/d1an00463h
68. Polyak K. Heterogeneity in breast cancer. J Clin Invest. 2011;121(10):3786–3788. doi:10.1172/jci60534
69. Tanaka M, Fernandez-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17(5):738–753. doi:10.1016/j.pan.2017.07.007
70. Li P, Wang J, Gao M, Wang J, Ma Y, Gu Y. Membrane feature-inspired profiling of extracellular vesicles for pancreatic cancer diagnosis. Anal Chem. 2021;93(28):9860–9868. doi:10.1021/acs.analchem.1c01712
71. Feghhi M, Rezaie J, Akbari A, et al. Effect of multi-functional polyhydroxylated polyhedral oligomeric silsesquioxane (POSS) nanoparticles on the angiogenesis and exosome biogenesis in human umbilical vein endothelial cells (HUVECs). Mater.Des. 2021;197. doi:10.1016/j.matdes.2020.109227
72. Kordelas L, Rebmann V, Ludwig AK, et al. MSC-derived exosomes: a novel tool to treat therapy-refractory graft-versus-host disease. Leukemia. 2014;28(4):970–973. doi:10.1038/leu.2014.41
73. Sprooten J, Ceusters J, Coosemans A, et al. Trial watch: dendritic cell vaccination for cancer immunotherapy. Oncoimmunology. 2019;8(11):e1638212. doi:10.1080/2162402X.2019.1638212
74. Rana S, Zöller M. Exosome target cell selection and the importance of exosomal tetraspanins: a hypothesis. Biochem Soc Trans. 2011;39(2):559–562. doi:10.1042/bst0390559
75. Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJA. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol. 2011;29(4):341–345. doi:10.1038/nbt.1807
76. Kamerkar S, LeBleu VS, Sugimoto H, et al. Exosomes facilitate therapeutic targeting of oncogenic KRAS in pancreatic cancer. Nature. 2017;546(7659):498–503. doi:10.1038/nature22341
77. Ahmadi M, Mahmoodi M, Shoaran M, Nazari-Khanamiri F, Rezaie J. Harnessing normal and engineered mesenchymal stem cells derived exosomes for cancer therapy: opportunity and challenges. Int J Mol Sci. 2022;23(22). doi:10.3390/ijms232213974
78. Saunders C, Foote JEJ, Wojciechowski JP, et al. Revealing population heterogeneity in vesicle-based nanomedicines using automated, single particle raman analysis. ACS Nano. 2023;17(12):11713–11728. doi:10.1021/acsnano.3c02452
79. Chen C, Zhu S, Wang S, Zhang W, Cheng Y, Yan X. Multiparameter quantification of liposomal nanomedicines at the single-particle level by high-sensitivity flow cytometry. ACS Appl Mater Interfaces. 2017;9(16):13913–13919. doi:10.1021/acsami.7b01867
80. Becker A, Thakur BK, Weiss JM, Kim HS, Peinado H, Lyden D. Extracellular vesicles in cancer: cell-to-cell mediators of metastasis. Cancer Cell. 2016;30(6):836–848. doi:10.1016/j.ccell.2016.10.009
81. Bobrie A, Krumeich S, Reyal F, et al. Rab27a supports exosome-dependent and -independent mechanisms that modify the tumor microenvironment and can promote tumor progression. Cancer Res. 2012;72(19):4920–4930. doi:10.1158/0008-5472.CAN-12-0925
82. Luzio JP, Hackmann Y, Dieckmann NM, Griffiths GM. The biogenesis of lysosomes and lysosome-related organelles. Cold Spring Harb Perspect Biol. 2014;6(9):a016840. doi:10.1101/cshperspect.a016840
83. Bano R, Ahmad F, Mohsin M. A perspective on the isolation and characterization of extracellular vesicles from different biofluids. RSC Adv. 2021;11(32):19598–19615. doi:10.1039/d1ra01576a
84. Yu S, Huang M, Wang J, Zheng Y, Xu H. Extracellular vesicles in tumor diagnosis: a mini-review. Curr Mol Med. 2021;21(7):596–606. doi:10.2174/1573405616666201209103154
85. Rezaie J, Nejati V, Mahmoodi M, Ahmadi M. Mesenchymal stem cells derived extracellular vesicles: a promising nanomedicine for drug delivery system. Biochem Pharmacol. 2022;203:115167. doi:10.1016/j.bcp.2022.115167
86. Hassanpour M, Rezaie J, Darabi M, Hiradfar A, Rahbarghazi R, Nouri M. Autophagy modulation altered differentiation capacity of CD146(+) cells toward endothelial cells, pericytes, and cardiomyocytes. Stem Cell Res Ther. 2020;11(1):139. doi:10.1186/s13287-020-01656-0
87. Almohammai A, Rahbarghazi R, Keyhanmanesh R, Rezaie J, Ahmadi M. Asthmatic condition induced the activity of exosome secretory pathway in rat pulmonary tissues. J Inflamm. 2021;18(1):14. doi:10.1186/s12950-021-00275-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
