Back to Journals » Infection and Drug Resistance » Volume 16
Application of Multiplex Fluorescence Polymerase Chain Reaction for Detecting Pathogenic Bacteria in Sputum Samples from Patients with Lower Respiratory Tract Infection
Authors Tan D, Han J, Sun Q, Cheng X, Liu J, Liu J, Li Q, Dai L
Received 19 July 2023
Accepted for publication 22 September 2023
Published 1 November 2023 Volume 2023:16 Pages 6999—7005
DOI https://doi.org/10.2147/IDR.S431425
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Deyong Tan,1– 4 Jianfeng Han,5 Qingzhi Sun,5 Xing Cheng,5 Juan Liu,5 Jia Liu,5 Qing Li,1– 4 Lizhong Dai5
1Department of Clinical Pharmacology, Xiangya Hospital, Central South University, Changsha, 410008 People’s Republic of China; 2Institute of Clinical Pharmacology, Central South University, Hunan Key Laboratory of Pharmacogenetics, Changsha, 410078 People’s Republic of China; 3Engineering Research Center of Applied Technology of Pharmacogenomics, Ministry of Education, Changsha, 410078 People’s Republic of China; 4National Clinical Research Center for Geriatric Disorders, Changsha, Hunan, 410008 People’s Republic of China; 5Sansure Biotech Inc, Changsha, Hunan Province, People’s Republic of China
Correspondence: Qing Li, Department of Clinical Pharmacology, Xiangya Hospital, Central South University, 87 Xiangya Road, Changsha, Hunan, People’s Republic of China, Tel +86 731 84805380, Fax +86 731-82354476, Email [email protected] Lizhong Dai, Sansure Biotech Inc, No. 680 Lusong Road, Changsha, Hunan, People’s Republic of China, Tel +86 73188883176, Email [email protected]
Objective: In this study, we conducted a multi-center research on six common lower respiratory tract pathogens using novel multiplex fluorescence quantitative polymerase chain reaction (PCR), and investigated the additional diagnostic value of this method, to provide a molecular diagnostic basis for clinical practice.
Methods: From March 2019 to October 2021, a total of 2047 respiratory sputum samples were collected from Hunan Provincial People’s Hospital (the First Affiliated Hospital of Hunan Normal University), Hunan Provincial Children’s Hospital, Jiangxi Provincial Children’s Hospital, and Wuhan Infectious Disease Hospital. The samples were analyzed using a novel multiplex fluorescence quantitative PCR method for Klebsiella pneumoniae, Streptococcus pneumoniae, Haemophilus influenzae, Pseudomonas aeruginosa, Legionella pneumophila, and Staphylococcus aureus. The results were compared to the results of bacterial culture and sequencing, as well as the results of third-party kits.
Results: Compared to the bacterial culture method, 2047 samples were detected with a sensitivity of 100%, a specificity of 72.22%, and an overall compliance rate of 81.91%. Compared to the sequencing method, the positive agreement percentage was 99.88%, the negative agreement percentage was 97.72%, and the overall agreement rate was 98.84%. Compared to similar control reagents, the positive agreement percentage was 100%, negative agreement percentage was 79.79%, and overall compliance rate was 96.19%.
Conclusion: The multiplex fluorescence PCR method has the advantages of simultaneously detecting multiple pathogenic bacteria and reducing the duration of pathogen culture identification. Combined detection can increase the detection rate, which has favorable performance and application prospects.
Keywords: bacterial infection, lower respiratory tract, melting curve, multiplex PCR, rapid diagnosis
Introduction
Respiratory tract infection is a common clinical infectious disease, and the COVID-19 epidemic has raised its awareness among the public, particularly that lower respiratory tract infection can easily cause bronchitis, pneumonia, and so on, which have a high incidence and mortality rate in the elderly and children.1,2 Respiratory tract infections have become a significant threat to people’s health—they play a significant role in the work of medical institutions, and timely and accurate diagnosis and treatment are crucial for reducing clinical antibiotic abuse and lowering the mortality rate with respect to respiratory infections.
Currently, bacterial culture and drug susceptibility tests are common methods for identifying pathogens of respiratory bacterial infections, particularly in primary medical facilities. However, there are issues with bacterial culture, including a lengthy culture cycle, a low positive rate, and the difficulty of cultivating certain bacteria. Therefore, the development of more rapid, accurate, and convenient identification methods is of vital importance for the accurate diagnosis and treatment of clinical lower respiratory tract infections. Nucleic acid detection technology has undergone rapid clinical development and popularization in recent years, and it was adopted and utilized extensively during the COVID-19 epidemic. Multiplex PCR uses multiple pairs of primers to amplify multiple pathogens simultaneously, with the advantages of rapid, sensitive, precise, and easy operation.3,4
In this study, a novel multiplex fluorescence PCR technique was used to detect six common respiratory tract infections,5 namely, Klebsiella pneumoniae, Streptococcus pneumoniae, Haemophilus influenzae, Pseudomonas aeruginosa, Legionella pneumophila, and Staphylococcus aureus. The results were compared to those of bacterial culture, sequencing method, and comparable nucleic acid detection reagents to determine consistency and application effect. Through multicenter clinical studies, we provide an easy-to-use method for detecting lower respiratory tract infections in clinical applications.
Materials and Methods
Sample Sources
From March 2019 to October 2021, a total of 2047 sputum samples were collected from patients hospitalized with lower respiratory tract infections at the Hunan Provincial People’s Hospital (the First Affiliated Hospital of Hunan Normal University), Hunan Provincial Children’s Hospital, Jiangxi Provincial Children’s Hospital, and Wuhan Infectious Disease Hospital. All the sputum samples were identified using VITEK® MS, an automated mass spectrometry microbial identification system (BioMérieux France).
This study was conducted with approval from the Ethics Committee of Hunan Provincial People’s Hospital (the First Affiliated Hospital of Hunan Normal University), Ethics Committee of Hunan Provincial Children’s Hospital, Ethics Committee of Jiangxi Provincial Children’s Hospital, and Ethics Committee of Wuhan Infectious Disease Hospital. This study was conducted in accordance with the declaration of Helsinki. Since the patient data of this study used was kept confidential throughout, and it would not cause any harm to patients, so the informed consent was waived.
Reagents and Instruments
Nucleic acid extraction or purification kit (Sansure Biotech Inc.), Multiple respiratory pathogen nucleic acid diagnostic kit (Multiplex PCR-Fluorescence Probing) (Sansure Biotech Inc.), SLAN-96P PCR amplification instrument (Shanghai Hongshi Medical Technology Co., Ltd.), Respiratory Pathogens Sequencing Reagents Kit (Sansure Biotech Inc.), Respiratory Pathogens Nucleic Acid Detection Kit (Isothermal Amplification on Disk Chip), (CapitalBio Technology Inc.), Legionella Pneumophila Real Time PCR Kit (Shanghai ZJ Bio-Tech Co., Ltd.).
Sample Processing
The same volume of sterile normal saline was added to the sample, which was then thoroughly mixed and allowed to stand for 30 minutes until completely liquefied. For samples that were difficult to liquefy, the same volume of 4% sodium hydroxide solution was added and centrifuged at high speed for 3 minutes. After discarding the supernatant, the sample was resuspended in 1 mL of normal saline. The sample was centrifuged for 3 minutes at high speed, the supernatant was discarded, and then the sample was resuspended in normal saline. Nucleic acid was extracted from the sample after liquefaction.
Nucleic Acid Extraction
Nucleic acid was extracted using the magnetic bead method with Nucleic acid extraction or purification kit. A total of 200 μL of liquified sample was added to a new centrifuge tube, nucleic acid extraction was performed as per the instructions, and 50 μL of eluate was added to each tube of nucleic acid for later use.
Multiplex PCR Detection
Selection of Pathogen Targets
Pathogens tested were bacteria commonly associated with lower respiratory tract infections, such as K. pneumoniae, S. pneumoniae, H. influenzae, P. aeruginosa, L. pneumophila, and S. aureus. Primers were designed for the aforementioned pathogen-conserved regions, and the forward and reverse primers and probes of all detection targets were combined to form a PCR primer mix (Multiple PCR mix) (Table 1).
 |
Table 1 Primer and Probe Design Information |
Fluorescence Quantitative PCR Amplification
The PCR reaction system was as follows: total reaction volume of 50 μL, containing 5 μL of the above extracted DNA template, 44 μL of multiplex PCR mix, and 1 μL of enzyme mix. The PCR reaction conditions were:
UDGase reaction, 50°C, 2 min, 1 cycle; UDGase stands for Uracil-DNA Glycosylase, an enzyme used to prevent contamination by degrading any uracil-containing DNA. The reagent replaces dTTP with dUTP, so the PCR products are all “DNA” strands containing dU. UDG enzyme effectively hydrolyzes uracil on single- or double-stranded DNA, resulting in pyrimidine-deficient sites that are easily hydrolyzed and broken at high temperatures or high pH. The enzyme is inactive against RNA and is mainly used to prevent contamination of PCR amplification products.
Pre-denaturation, 94°C for 3 min, 1 cycle; This step helps to denature the DNA, separating the double-stranded DNA into single strands, which will serve as templates for the subsequent PCR amplification.
Amplification Cycles (Total of 45 cycles): Denaturation, 94°C for 10s, Annealing, 60°C for 20s, Extension, 72°C for 20s. Primer extension is generally performed at 72°C (Taq enzyme optimal temperature). And it can effectively reduce the non-specific extension in the multiplex PCR reaction, further improve the efficiency of multiplex reaction, so that the sensitivity and specificity of reagent detection is higher. At the same time, in order to match the amplification of subfragments, the Tm value of the probe we designed was optimized to glow only at the 72°C.
The melting temperature (Tm) range was 62–75°C, and the fluorescence was continuously collected until the end of the procedure. The results were interpreted and analyzed using the SLAN 8.2.2 analysis software included with the instrument.
Evaluation of Fluorescence Real-Time PCR Results
Result interpretation: The negative result should be consistent with no melting curve in the detection of FAM, HEX, ROX, and CY5 channels, with no amplification curve (No Ct) or Ct value >37. The positive results should conform to obvious S-type amplification curves in the detection of FAM, HEX (or VIC), ROX, and CY5 channels, Ct < 37. Also, characteristic peaks of the melting curve were observed in the four channels, and the Tm were FAM (68.8–71.3°C), HEX (65.8–68.5°C), ROX (68.5–71.0°C), and CY5 (66.8–70.0°C).
Statistical Analysis
SPSS 24.0 statistical software was used for data analysis. Counting data are expressed as percentages, and the chi-squared test was applied to compare between-group differences. P < 0.05 was considered a statistically significant difference.
Results
The results of multiplex PCR nucleic acid test results of 2047 samples were counted, including 311 cases in the K. pneumoniae (KPN) positive group, 341 cases in the S. pneumoniae (SP) positive group, 292 cases in the H. influenzae (HI) positive group, 241 cases in the P. aeruginosa (PA) positive group, 65 cases in the L. pneumophila (LP) positive group, 244 cases in the S. aureus (SA) positive group, and 838 cases in the negative group.
Comparison of Multiplex PCR Test Results with Bacterial Culture Results
Compared with the bacterial culture results, the multiplex PCR test results of the six bacteria had a sensitivity of 100% (95% CI: 99.32–100.00%), specificity of 72.22% (95% CI: 69.35–74.97%), and total consistency of 81.91% (95% CI: 79.90–83.80%) (Table 2).
 |
Table 2 Comparison of Multiplex PCR Detection and Bacterial Culture Results |
The primary reason for the inconsistency between multiplex PCR and bacterial culture results is the difference in sensitivity between the two methods. Also, the test performed after drug administration may also have a substantial impact on culture positivity. There were 261 samples with positive pathogen culture results which had inconsistently positive targets, primarily because the culture results were positive for a single target while the multiplex nucleic acid test revealed mixed infection. If the sample contains a low concentration of the corresponding target, the target signal detected by the melting curve may be weak.
Comparison of Multiplex PCR Test Results and Sequencing Results
Compared with the sequencing results, the multiplex PCR results of the six bacteria had a sensitivity of 99.88% (95% CI: 99.31–100.00%), a specificity of 97.72% (95% CI: 96.37–98.66%), and total consistency of 98.84% (95% CI: 98.17–99.31%) (Table 3).
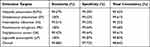 |
Table 3 Comparison of Multiplex PCR Detection and Sequencing Results |
The primary reasons for the inconsistency between multiplex PCR detection and sequencing results are as follows: the samples contained a low concentration of the corresponding target and the target signal detected by the melting curve was weak; the sample was at a weak positive or a critical positive concentration level; the target gene sequence was mutated, which decreased the accuracy or sensitivity; and there was additional interference or PCR inhibitors, which would render the bacteria undetectable by the sequencing method.
Comparison of Multiplex PCR Test Results with Similar Reagent Results
Compared with the test results of similar reagents, the multiplex PCR test results of the six bacteria had a sensitivity of 100% (95% CI: 99.09–100%), a specificity was 79.79% (95% CI: 70.25–87.37%), and total consistency of 96.19% (95% CI: 94.12–97.69%) (Table 4).
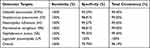 |
Table 4 Comparison of Multiplex PCR Detection and Similar Reagents |
The primary reasons for the inconsistency between multiplex PCR detection and the test results of similar reagents are as follows: it is possible that the samples contained a low concentration of the corresponding target, which belongs to the weak positive or critical positive concentration level; the target gene sequence detected by the control reagent had mutated, resulting in poor accuracy or sensitivity; there was additional interference or PCR inhibitors, which would render the bacteria undetectable by the control reagents.
Discussion
Respiratory tract infection is a common clinical condition that is typically classified according based on the site of infection as upper or lower respiratory tract infection. Normally, it is caused by bacteria, viruses, fungi, and other pathogens. Upper respiratory tract infections are primarily caused by viruses, whereas lower respiratory tract infections are primarily caused by bacteria. Empirically, there is widespread use of antibiotics due to failure of on-time and accurate diagnosis of infectious pathogens, thus in recent years drug-resistant bacteria resulting from antibiotic abuse have become an important pathogen of clinical respiratory tract infections.6
A bacterial examination has significant guiding significance for the diagnosis and treatment of lower respiratory tract infection pathogens.7 Although pathogenic bacteria culture is the gold standard for laboratory testing and identification, its detection results are easily influenced by factors such as specimen collection and culture conditions.8 Some special pathogenic bacteria, such as L. pneumophila, are more difficult to detect by culture because they require special culture conditions, and the detection rate is low due to limited conditions in certain hospitals.9 Metagenomics sequencing technology is a novel technology recently developed that has the advantage of covering a broad range of pathogens and has a high clinical application value for the identification of rare infections and the diagnosis of pathogens that are difficult to detect using conventional methods. However, it has drawbacks such as a lack of recognized interpretation standards, unclear interpretation of sequencing results, and a high cost.10 Due to the similar characteristics of clinical infections caused by pathogenic bacteria of the lower respiratory tract, differential diagnosis cannot be performed effectively using only clinical symptoms and conventional methods. Therefore, high sensitivity and high specificity methods are necessary to quickly identify pathogenic bacteria and provide a solid foundation for clinical diagnosis. Multiplex PCR technology offers a potent solution to this issue. It is improved and developed based on conventional PCR technology, and multiple primer probes are mixed into the same reaction solution, enabling simultaneous detection and identification of multiple pathogens in a single reaction.3,11 In this study, novel multiplex PCR technology was used to detect pathogenic bacteria nucleic acid in the samples collected from patients with lower respiratory tract infections in different hospitals, and the application performance of this method and the detection reagent was clinically validated, providing a basis for the rapid supplementary clinical diagnosis of lower respiratory tract infectious diseases.
The novel multiplex fluorescence PCR technology used in this study combines melting curve analysis. The detection reagent used is the first in China to use multiplex fluorescence PCR technology to detect six types of bacteria in a single tube and is an innovative product for molecular diagnostics. The results revealed that the pathogens of lower respiratory tract infection obtained from clinical studies conducted in multiple centers were K. pneumoniae, S. pneumoniae, and H. influenzae, consistent with the results of clinical epidemiological investigation in Southwest China. For example, the distribution of pathogenic bacteria among hospitalized children and adults from 2015 to 2020 in Chongqing General Hospital were mainly gram-negative bacilli. The pathogenic bacteria in lower respiratory tract infections in children were mainly S. pneumoniae (21.9%) and H. influenzae (19.4%), while they were mainly Acinetobacter baumannii (25.3%) and K. pneumoniae (24.5%) in adults.12 The distribution of isolated bacteria in patients with lower respiratory tract infection in Guizhou Regional General Hospital from 2014 to 2019 revealed that gram-negative bacteria accounted for the main proportion (75.66%), and the top three bacteria were S. pneumoniae 14.64% (3742/23718), H. influenzae 14.03% (3327/23718), and K. pneumoniae 12.78% (3030/23718).13
Bacterial resistance has always been an important concern in clinical medical work, and the isolation and distribution of 114,033 respiratory strains in China by the China Bacterial Resistance Surveillance Network (CHINET) in 2020 revealed that K. pneumoniae, A. baumannii, P. aeruginosa, S. aureus, H. influenzae, and S. pneumoniae ranked 1 to 6, respectively.14 An analysis published in a Lancet article on bacterial resistance in 2022 revealed that an estimated 4.95 million deaths in 2019 were linked to antimicrobial resistance (AMR), of which 1.27 million deaths were attributable to AMR. As for disease types, lower respiratory tract infections associated with antimicrobial resistance were the most severe, resulting in more than 1.5 million deaths. The six main pathogens associated with drug-resistant deaths include Escherichia coli, S. aureus, K. pneumoniae, S. pneumoniae, A. baumannii, and P. aeruginosa.15 Therefore, it is necessary for the detection and monitoring of these widespread cases of drug resistance, because pathogenic results can be obtained rapidly through multiplex PCR to assist further clinical diagnosis and drug treatment.
In this study, a novel rapid detection method, multiplex PCR, was adopted for lower respiratory tract pathogens, which aimed at six common respiratory tract infection pathogens, with high sensitivity, good specificity, and high consistency with the culture method, sequencing method, and similar nucleic acid detection reagents. Furthermore, the method was not hindered by the use of antibacterial drugs, and the overall amplification reaction time was kept under 2 hours; this meant that the method could satisfy the need for timely clinical test reports and give doctors a solid basis for making diagnoses and treatment. The national medical device registration batch number of the kit used in this study is 20223400597. This innovative bacterial detection method provides a practical means for the rapid detection and identification of lower respiratory tract infections. In clinical applications, multiplex PCR technology can be used in combination with bacterial culture and susceptibility testing, to improve the accuracy of diagnosis, reduce antibiotic abuse, and provide guidance for precision medicine in clinical settings.
The limitation of this study is that the use of antibiotics in clinical patients may affect the sensitivity of pathogen detection results, but combining multiplex PCR technology with bacterial culture and drug sensitivity can improve the accuracy of auxiliary diagnosis and provide a basis for clinical precise drug use.
Conclusion
In recent years, with the rapid development of nucleic acid amplification technology, multiplex PCR based on the TaqMan probe has become an important pathogen detection tool and has been implemented in clinical practice. Broad-spectrum respiratory pathogen nucleic acid detection has become a novel development direction. We conducted a multi-centre study of six common lower respiratory tract pathogens using novel multiplex fluorescence quantitative polymerase chain reaction (PCR) to investigate the added diagnostic value of the method, to provide a molecular diagnostic basis for clinical practice.
Compared to traditional detection methods, the multiplex PCR detection technology for respiratory pathogens is quick, sensitive, and simple, with a wide detection area and greater detection efficiency. It can effectively identify the bacteria of common respiratory tract infections, and provide guidance for the auxiliary diagnosis of patients with lower respiratory tract infections and the use of therapeutic drugs. Rapid and accurate screening methods are conducive to accurate clinical diagnosis and guidance for rational drug use, and should be promoted in clinical practice.
Funding
Hunan Science and Technology Department: Hunan Innovative Province Construction Special Focus Area R&D Program. [Development of Precise, Intelligent and Portable Molecular Diagnostic Equipment System (2019SK2231)]; National Natural Science Foundation (NNSF) of China (82373963).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Troeger C, Blacker B, Khalil IA; GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18(11):1191–1210. PMID: 30243584; PMCID: PMC6202443. doi:10.1016/S1473-3099(18)30310-4
2. Allinson JP, Chaturvedi N, Wong A, et al. Early childhood lower respiratory tract infection and premature adult death from respiratory disease in Great Britain: a national birth cohort study. Lancet. 2023;401(10383):1183–1193. Erratum in: Lancet. 2023 May 6;401(10387):1498. PMID: 36898396. doi:10.1016/S0140-6736(23)00131-9
3. Yang J, Li D, Wang J, Zhang R, Li J. Design, optimization, and application of multiplex rRT-PCR in the detection of respiratory viruses. Crit Rev Clin Lab Sci. 2022;59(8):555–572. PMID: 35559711. doi:10.1080/10408363.2022.2072467
4. Huang SJ, Yao YH, Chao PL. Application of multiple fluorescent PCR to the detection of pathogenic bacteria in lower respiratory tract infection. China Health Stand Manage. 2015;6(29):155–158. Chinese.
5. Noor Nik Zuraina NM, Hasan H, Mohamad S, Suraiya S. Diagnostic detection of intended bacteria associated with respiratory tract infections among Kelantanese Malaysian Hajj pilgrims by a ready-to-use, thermostable multiplex PCR assay. Saudi J Biol Sci. 2022;29(8):103349. PMID: 35800141; PMCID: PMC9253910. doi:10.1016/j.sjbs.2022.103349
6. Ho J, Ip M. Antibiotic-resistant community-acquired bacterial pneumonia. Infect Dis Clin North Am. 2019;33(4):1087–1103. PMID: 31668192. doi:10.1016/j.idc.2019.07.002
7. Lee SH, Ruan SY, Pan SC, Lee TF, Chien JY, Hsueh PR. Performance of a multiplex PCR pneumonia panel for the identification of respiratory pathogens and the main determinants of resistance from the lower respiratory tract specimens of adult patients in intensive care units. J Microbiol Immunol Infect. 2019;52(6):920–928. PMID: 31806539; PMCID: PMC7185395. doi:10.1016/j.jmii.2019.10.009
8. Guo LM. Laboratory diagnosis and clinical significance of lower respiratory tract infection. J Pract Med Tech. 2018;25(03):276–277. Chinese.
9. Eble D, Gehrig V, Schubert-Ullrich P, Köppel R, Füchslin HP. Comparison of the culture method with multiplex PCR for the confirmation of Legionella spp. and Legionella pneumophila. J Appl Microbiol. 2021;131(5):2600–2609. PMID: 33847421; PMCID: PMC9292777. doi:10.1111/jam.15103
10. Liu H, Zhang Y, Yang J, Liu Y, Chen J, Szymczak WA. Application of mNGS in the etiological analysis of lower respiratory tract infections and the prediction of drug resistance. Microbiol Spectr. 2022;10(1):e0250221. PMID: 35171007; PMCID: PMC8849087. doi:10.1128/spectrum.02502-21
11. Lin CY, Hwang D, Chiu NC, et al. Increased detection of viruses in children with respiratory tract infection using PCR. Int J Environ Res Public Health. 2020;17(2):564. PMID: 31952364; PMCID: PMC7013517. doi:10.3390/ijerph17020564
12. Han F, Zhang SS. Comparative analysis of pathogenic bacteria distribution and drug resistance of lower respiratory tract infection in children and adults in general hospital. Hainan Med J. 2021;32(17):2212–2216. Chinese.
13. Chen R, Xu YJ, Luo XR, et al. Distribution and drug resistance of pathogenic bacteria in lower respiratory tract infections in a hospital in Guizhou from 2014 to 2019. World Notes Antibiot. 2021;42(04):241–246. Chinese. doi:10.13461/j.cnki.wna.005403
14. Hu FP, Guo Y, Zhu DM, et al. 2020 CHINET China bacterial resistance monitoring. Chin J Infect Chemother. 2021;21(04):377–387. Chinese. doi:10.16718/j.1009-7708.2021.04.001
15. Murray CJL, Ikuta KS, Sharara F; Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. Erratum in: Lancet. 2022 Oct 1; 400(10358):1102.PMID: 35065702; PMCID: PMC8841637. doi:10.1016/S0140-6736(21)02724-0
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
