Back to Journals » International Journal of Women's Health » Volume 15
Application of Copy Number Variation Sequencing Technology in 422 Foetuses with Abnormal Ultrasound Soft Markers
Authors Wang Y, Chai Y, Wang J, Gao M, Zang W, Chang Y
Received 5 July 2023
Accepted for publication 8 November 2023
Published 20 November 2023 Volume 2023:15 Pages 1791—1800
DOI https://doi.org/10.2147/IJWH.S429164
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Yanan Wang, Yuqiong Chai, Jieqiong Wang, Mingya Gao, Weiwei Zang, Yujie Chang
Department of Genetics and Prenatal Diagnosis, Luoyang Maternal and Child Health Hospital, Luoyang, 471000, People’s Republic of China
Correspondence: Yanan Wang, Department of Genetics and Prenatal Diagnosis, Luoyang Maternal and Child Health Hospital, No. 206 of Tongqu Street, Luolong District, Luoyang, 471000, People’s Republic of China, Tel +86-15896572343, Email [email protected]
Purpose: The application value of ultrasound soft indicators in prenatal diagnosis was evaluated by copy number variation sequencing (CNV-seq).
Methods: The authors conducted a retrospective analysis of 422 pregnant women who underwent CNV-seq testing at Luoyang Maternal and Child Health Hospital between January 2020 and November 2021. The women had presented with abnormal ultrasound soft markers; those identified as high-risk through non-invasive prenatal screening were excluded.
Results: A total of 43 abnormal cases were detected in 422 pregnant women, including 24 aneuploidy (including chimerism) and 19 pathogenic or likely pathogenic copy number variations (CNVs). Based on the characteristics of ultrasound soft indicators, pregnant women were divided into five groups: isolated nuchal translucency (NT) group, combined NT group, isolated soft indicators group, combined soft indicators group and combined non-NT group. The abnormality detection rates in the five groups were 12.38% (13/105), 36.11% (13/36), 3.74% (4/103), 3.08% (2/63) and 10.09% (11/109), respectively. Statistical tests showed that the detection rate in the NT thickening combined with other abnormalities group was significantly higher than the other four groups, while there was no statistical difference in the detection rate among the other four groups.
Conclusion: When NT thickening is combined with other abnormalities, it is more likely to indicate chromosome abnormalities or CNVs, so it should be regarded seriously upon finding, and pregnant women should be referred for prenatal diagnosis according to the examination results. In addition, NT thickening is an important indicator for prenatal diagnosis and should be considered regardless of whether it occurs independently. The authors recommend CNV-seq for prenatal diagnosis to prevent missing small fragments of CNVs during traditional karyotyping.
Keywords: ultrasound soft indicators, isolated type, combined type, amniotic fluid, CNV-seq
Introduction
Ultrasound soft markers refer to small nonspecific variations in foetal structure found in prenatal ultrasound that are often associated with abnormal chromosome number or pathogenic copy number variations (CNVs).1,2 Common ultrasound soft markers include nuchal translucency (NT) thickness, nuchal fold (NF) thickness, nasal bone dysplasia, choroid plexus cyst, intracardiac strong echo focus, intestinal echo enhancement, renal pelvis dilatation, single umbilical artery and short long bones.3,4 Clinically, the application value of single or combined ultrasound soft marker abnormalities in foetal chromosomal abnormalities needs to be clarified, as these can provide an essential basis for prenatal diagnosis and genetic counselling.
CNV sequencing (CNV-seq) technology, a prenatal diagnosis method based on high-throughput sequencing developed in recent years,5,6 can not only accurately detect chromosomal aneuploidy but also reduce the lower limit of fragment detection of CNVs to 0.1 megabases (Mb) compared to traditional karyotyping. Therefore, CNV-seq can be used to detect more rare and severe microdeletion/microduplication syndromes. What makes it even more appealing is that CNV-seq does not require cell culture to significantly shorten the detection cycle. At present, CNV-seq is included in the first-line prenatal diagnosis in China7,8 and has become one of the important technical means in the secondary prevention and control system of birth defects in China. In this study, CNV-seq analysis was performed on high-risk pregnant women with abnormal ultrasound soft markers admitted to Luoyang Maternal and Child Health Hospital from January 2020 to December 2021, with a view to systematically evaluating the clinical application potential of CNV-seq in the diagnosis of foetuses with abnormal ultrasound.
Subjects and Methods
Subjects and Inclusion Criteria
A total of 422 pregnant women who underwent amniocentesis in Luoyang Maternal and Child Health Hospital from January 2020 to December 2021 were selected as subjects by convenience sampling. There were three inclusion criteria: (1) pregnant women aged 18–44; (2) pregnant women who had not had non-invasive prenatal screening (NIPS) or had negative NIPS results; and (3) pregnant women with at least one abnormal ultrasound soft marker. Ultrasound soft markers and their criteria for abnormal judgment were as follows (See Figure 1 for an example): (1) NT thickness ≥2.5 mm; (2) NF thickness ≥6 mm; (3) choroid plexus cyst: choroid plexus cysts of any size or number in the ventricle; (4) echogenic intracardiac focus: a spot-like echogenic intracardiac focus in any single ventricle, with echo intensity comparable to bone; (5) intestinal echo enhancement: intestinal echo intensity ≥ bone echo intensity; (6) pyelic separation: anteroposterior diameter of renal pelvis >4 mm; (7) nasal bone dysplasia; (8) ventricle enlargement; (9) short long bones: ratio of observed value to expected value <0.9; (10) single umbilical artery; and (11) tricuspid regurgitation. Exclusion criteria were as follows: (1) pregnant women with aneuploidy risk soft markers and mild hydronephrosis; (2) pregnant women with multiple pregnancies; (3) pregnant women with signs of threatened abortion in the previous 3 months; and (4) pregnant women who did not consent to participate in this study.
 |
Figure 1 The fetal nuchal translucency was thickened. |
Pregnant women were divided into the following five groups according to the characteristics of ultrasound soft markers: (1) isolated NT group: only NT thickening was detected; (2) combined NT group: NT thickening combined with other soft markers or clinical abnormalities; (3) isolated soft marker group: only soft marker anomalies with non-NT thickening were detected; (4) combined soft marker group: two or more soft marker anomalies with non-NT thickening were detected simultaneously; and (5) combined non-NT group: soft marker anomalies with non-NT thickening were detected combined with other clinical abnormalities. All subjects signed informed consent and received full genetic counselling before and after the test.
CNV Sequencing Analysis
Genomic deoxyribonucleic acid (DNA) of amniotic fluid cells was extracted with the kit from Annaroad Gene Technology (Beijing) Co., Ltd. After passing quality inspection, short tandem repeats (STR) detection technology was used to eliminate maternal contamination in uncultured amniotic fluid cells. The CNV-seq was continued on the samples without maternal contamination; DNA samples of about 10 ng were taken for sequencing library preparation, including digestion, ligation, amplification, purification, quantification and quality control. Downstream experiments were carried out when the library concentration was >1 ng/L. Sequencing was performed on the Illumina NextSeq 550AR platform using a single-end 40 bp sequencing mode, with a sequencing data volume of 7.5 Mb. Subsequently, the sequencing data were compared with the hg19 genome sequence, and the identified CNVs were queried via public databases, including the Database of Genomic Variants, Genome Aggregation Database, Database of Chromosomal Imbalance and Phenotype in Humans using Ensembl Resources, Online Mendelian Inheritance in Man and Clinical Genome Resource. In terms of pathogenicity, CNVs were classified into five categories according to the guidelines of the American College of Medical Genetics and Genomics:9 benign, likely benign, pathogenic, likely pathogenic and uncertain significance. In this study, only pathogenic and likely pathogenic CNVs (pCNVs) were statistically analysed.
Statistical Analysis
All data were analysed by R (version 3.5.3) software for statistical analysis. Numerical data were described by the number of cases or the percentage, the chi-squared (χ2) test or Fisher’s exact test were employed for the comparison between groups, and post hoc pairwise comparisons were performed with Bonferroni correction. Unless otherwise specified, P < 0.05 indicates a statistically significant difference.
Results
Numbers of Ultrasound Soft Markers
Among the 422 pregnant women, the abnormal ultrasound soft markers detected and the number of cases of each (from highest to lowest) were as follows: NT thickening (144 cases), choroid plexus cyst (80 cases), echogenic intracardiac focus (65 cases), pyelic separation (53 cases), nasal bone dysplasia (33 cases), ventricle enlargement (32 cases), tricuspid regurgitation (32 cases), single umbilical artery (20 cases), short long bones (15 cases), echogenic bowel (10 cases) and NF thickening (five cases). In general, the detection rate of the non-isolated type of abnormal soft markers was higher than that of the isolated type. Within the isolated soft markers, the top three detection rates were for NT thickening, pyelic separation and short long bones, while the top detection rates within the non-isolated soft markers were for NT thickening, single umbilical artery, nasal bone dysplasia and short long bones (Table 1).
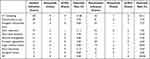 |
Table 1 Statistics of Chromosome Aneuploidy and pCNVs Detected by Ultrasound Soft Markers |
Comparisons of Abnormality Detection Rates
As shown in Table 2, the detection rate of abnormal foetal NT thickening was 12.38% when it was detected alone and increased to 36.11% when it was combined with other indications. However, the detection rates of other ultrasonic soft marker abnormalities, whether isolated or combined, were low (3.74% and 3.08%, respectively). Only when ultrasound soft marker abnormalities were combined with other clinical abnormalities did the detection rate (10.09%) come close to that of the isolated NT group.
 |
Table 2 Grouping of 422 Pregnant Women and Statistics of Abnormal Detection Rate |
The χ2 test showed a statistically significant difference in the detection rates of abnormalities among the five groups (χ2 = 35.44, P < 0.001). Further pairwise comparison (using correction with the Bonferroni method) found that the detection rate of the combined NT group was significantly higher than that of the other four groups, with a statistically significant difference (P < 0.01), while there was no statistically significant difference among the other four groups.
Detection of Chromosomal Abnormalities
According to CNV-seq analysis, a total of 43 cases of chromosomal aneuploidy and pCNVs were confirmed in the 422 pregnant women with abnormal ultrasound soft markers, of which 18 cases were common trisomy abnormalities, four were sex chromosome abnormalities, two were aneuploidy chimerism and 19 were pCNVs (Table 3). Of these cases, 33 women had an induced labour, five were lost to follow-up and five continued the pregnancy to delivery; of the five cases that continued to delivery, four of them had no abnormalities at follow-up to date and one of them had pulmonary artery stenosis detected at about 1 year of age, with a good postoperative condition (Table 3).
 |
Table 3 Summary of Information from 43 Fetuses Diagnosed with Aneuploidy and pCNVs by CNV-Seq |
Discussion
Since the introduction of China’s two-child policy, the birth rate in China has shown an obvious upward trend, triggering a broad market demand for accurate prenatal diagnosis. In this study, to further the improvement in the resolution and accuracy of prenatal diagnosis, the genome copy number variation sequencing technology, described as “accurate and efficient, was applied to prenatal diagnosis, with a view to providing theoretical guidance for accurate screening for clinical prenatal diagnosis”.
In addition to serious congenital structural abnormalities, prenatal ultrasound can detect some minor anatomical changes; most of these small changes are transient, but some may be related to an abnormal chromosome number in the foetus, pCNVs or even monogenic diseases, which are called “ultrasound soft markers”.10 In the study by Zhao et al,3 513 foetuses with abnormal ultrasound soft markers but without definite structural abnormalities were analysed, and the detection rates of abnormal chromosome number and pCNVs were 10.14% and 6.43%, respectively. Zhu et al11 also analysed 580 foetuses with abnormal ultrasound soft markers but without definite structural abnormalities, and the detection rates of abnormal chromosome number and pCNVs were 8.62% and 4.14%, respectively. Another study by Yao et al12 analysed 542 foetuses with abnormal ultrasound soft markers in the second trimester, and the detection rates of abnormal chromosome number and pCNVs were 2.40% and 3.14%, respectively. In this study, the detection rates of abnormal chromosome number and pCNVs in 422 foetuses with abnormal ultrasound soft markers were 5.68% and 4.50%, respectively, which differ from previous studies; this may be due to factors such as the study population, soft marker type and diagnostic technology.
Several previous studies have revealed a significant increase in the probability of detecting chromosomal abnormalities or pCNVs when non-isolated ultrasound soft markers are present.4,13 Despite the higher detection rate of combined ultrasonic soft markers than that of isolated ones in this study, the χ2 test only supported a statistically significant difference in the detection rate between the “combined NT group” and the other four groups, while the difference in detection rates between the “combined soft marker group” and the “isolated soft marker group” was not statistically significant. It was further found that the majority of cases in the “combined soft marker group” contained two ultrasound soft markers, and the cases with three or more soft markers accounted for a small proportion. It was thus concluded that non-NT thickened ultrasound soft markers may have minimal influence on the risk of genetic diseases, at least for the population in Luoyang area; therefore, prenatal diagnosis should be made carefully. For three or more non-NT thickening ultrasonic soft markers, more population data are needed to support the clinical application value.
Some studies have proved the reliability of using certain isolated ultrasound soft markers as indications for prenatal diagnosis, for example, NT thickening, which is currently one of the most clinically significant ultrasound soft markers. Other studies have revealed a clear correlation between NT thickening and chromosomal aneuploidy, which can significantly increase the risk of congenital heart disease, intellectual disability, developmental retardation and other related genetic syndromes.14,15 Nuchal fold thickening is considered to be the most important ultrasound soft marker indicating chromosomal abnormalities in the second trimester, and its detection cannot be replaced by NT examination.16,17 Of the 26 positive samples with NT thickening in this study, aneuploidy accounted for 61.54% (16/26), indicating a close relationship between NT thickening and aneuploidy, while pCNVs accounted for 38.46% (10/26), so they should also be regarded seriously. It was also found that NT thickening was detected in all 22q11.2 (proximal) microdeletion or microreplication syndromes, which supported the conclusion of Cao et al18 that NT thickening was the early clinical manifestation of these syndromes. The correlation of choroid plexus cysts, the second most common ultrasound soft marker in this study behind NT thickening, with chromosomal abnormalities is uncertain.19,20 In this study, it was shown that in foetuses with choroid plexus cysts, the detection rate of abnormalities was low in both isolated and non-isolated indications, which may imply that there is no correlation between choroid plexus cysts and chromosomal abnormalities.19 Despite isolated nasal dysplasia11,21 and NF thickening16 being reported in some studies as possible indications for prenatal diagnosis, such conclusions cannot be supported as valid by this study due to the small number of samples included. The detection rates of two other indications, pyelic separation and short long bone, were close that of NT thickening in this study; the isolated occurrence of these markers may have prenatal diagnostic significance for the population in Luoyang area, although previous studies consider that these two may not be related to chromosomal abnormalities.16 Therefore, further verification is needed in the future.
In this study, pCNVs were confirmed by CNV-seq in 19 foetuses, 15 of which involved severe syndromes. There were 16 cases of pCNVs with a fragment size <5 Mb, indicating that 78.95% of pCNVs were likely to be missed under the current detection capability of NIPS.22,23 Further exploration found that 86.67% of cases (13/15) were in the “isolated NT group”, “combined NT group” and “combined non-NT group”, suggesting that prenatal diagnosis should still be a concern in most foetuses with pCNVs <3 Mb. It can be seen that the soft markers found on prenatal ultrasound, which can minimise the risk of missed detection of pCNVs when combined with NIPS, are still critical markers. Besides routine karyotype analysis, CNV-seq is also recommended for prenatal diagnosis to detect chromosome deletion or duplication larger than 0.1 Mb and to screen pathogenic chromosome copy number variation, which cannot be resolved by karyotype analysis.
Nevertheless, there were still some shortcomings in this study. First, the small sample led to insufficient statistical power of some ultrasound soft markers. Second, the inclusion of chromosome number abnormalities and pCNVs alone makes it impossible to exclude the correlation between some ultrasound soft markers and monogenic diseases. In future research, a more in-depth exploration will be conducted.
Conclusion
This study has shown NT thickening to be of great clinical significance in indicating chromosome aneuploidy and pCNVs in foetuses with abnormal ultrasound soft markers. The use of CNV-seq diagnosis, whether in isolated NT thickening or in combination with other abnormalities, is recommended to identify chromosomal number abnormalities and the risk of pCNVs. In summary, the CNV-seq diagnosis, once applied, boasts numerous benefits, such as providing more references for the evaluation of prenatal diagnostic technology in China, screening and diagnosing foetal abnormalities as early as possible, and reducing the psychological and economic burden on pregnant women and their families.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Luoyang Maternal and Child Health Hospital. Written informed consent was obtained from all participants.
Funding
This study did not receive any funding in any form.
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately.
References
1. Hu T, Tian T, Zhang Z, et al. Prenatal chromosomal microarray analysis in 2466 fetuses with ultrasonographic soft markers: a prospective cohort study. Am J Obstet Gynecol. 2021;224(5):516.e1–516.e16. doi:10.1016/j.ajog.2020.10.039
2. Jiang W, Deng X, Sun L, et al.Application of ultrasound markers in fetal small genome abnormality. Chin J Med Imag Technol. 2018;34(S1):62–66. doi:10.13929/j.1003-3289.2018091134
3. Zhao P, Song Y, Cui L, et al. Application value of the ultrasonic soft markers in the diagnosis of fetal chromosomal abnormalities. J Clin Ultrasound Med. 2021;23(01):18–22. doi:10.16245/j.cnki.issn1008-6978.2021.01.005
4. Cai M, Lin N, Chen X, et al. Evaluation of chromosomal abnormalities and copy number variations in fetuses with ultrasonic soft markers. BMC Med Genomics. 2021;14(1):19. doi:10.1186/s12920-021-00870-w
5. Lan L, She L, Zhang B, He Y, Zheng Z. Prenatal diagnosis of 913 fetuses samples using copy number variation sequencing. J Gene Med. 2021;23(5):e3324. doi:10.1002/jgm.3324
6. Li F, Yao X, Zhang Y. Research progress of copy number variation sequencing in prenatal diagnosis. J Int Obstetr Gynecol. 2021;48(01):75–78. doi:10.12280/gjfckx.20200527
7. Clinical Genetics Group of Medical Genetics Branch of Chinese Medical Association, Professional Committee of Prenatal Diagnosis of Genetic Diseases of Medical Geneticists Branch of Chinese Medical Association, and Genetic Disease Prevention and Control Group of Professional Committee of Birth Defects Prevention and Control of Chinese Preventive Medical Association. Expert consensus on application of low-depth whole genome sequencing technology in prenatal diagnosis. Chin J Med Genet. 2019;36(4):293–296. doi:10.3760/cma.j.issn.1003-9406.2019.04.001
8. Ting H, Shanling L, Liu S. Guidelines for the application of copy number variation testing in prenatal diagnosis. Chin J Med Genet. 2020;37(9):909–917. doi:10.3760/cma.j.cn511374-20200522-00373
9. Riggs ER, Andersen EF, Cherry AM, et al. Technical standards for the interpretation and reporting of constitutional copy-number variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen) [published correction appears in Genet Med. 2021 Nov; 23(11):2230]. Genet Med. 2020;22(2):245–257. doi:10.1038/s41436-019-0686-8
10. Study on the standardized system of prenatal screening and diagnosis of structural malformation based on imaging. Research group of ultrasound diagnosis department of the First Medical Center of General Hospital of Chinese People’s Liberation Army. Ultrasonographic diagnosis and suggestions for further diagnosis of common ultrasonographic soft markers and subtle abnormalities. Chin J Perinat Med. 2022;25(2):122–128. doi:10.3760/cma.j.cn113903-20210518-00463
11. Zhu X, Yuan F, Gu L, et al. Correlation between fetal ultrasound soft marker and chromosome copy number variation. Acta Acad Med Xuzhou. 2022;42(06):419–423. doi:10.3969/j.issn.2096-3882.2022.06.006
12. Yao Y, Zhang C, Song J. Correlation analysis between ultrasound soft marker and chromosome abnormality in the second trimester. Prog Obstetr Gynecol. 2021;30(12):933–936. doi:10.13283/j.cnki.xdfckjz.2021.12.005
13. Li Y, Wen X, Sun M, et al. Analysis on the detection of fetal chromosomal abnormalities with low-risk ultrasound soft markers by non-invasive DNA examination. Shandong Med J. 2022;62(08):67–70. doi:10.3969/j.issn.1002-266X.2022.08.017
14. Yuan B, Li N, Long Y, et al. Study on the value of copy number variation sequencing technology in prenatal diagnosis of high-risk fetus with normal ultrasound performance in non-invasive prenatal screening. Chin J Pract Gynecol Obstetr. 2022;38(04):447–450. doi:10.19538/j.fk2022040114
15. Abele H, Wagner P, Sonek J, et al. First trimester ultrasound screening for Down syndrome based on maternal age, fetal nuchal translucency and different combinations of the additional markers nasal bone, tricuspid and ductus venosus flow. Prenat Diagn. 2015;35(12):1182–1186. doi:10.1002/pd.4664
16. Sun L, Deng X, Jiang W, et al. Value of the second trimester ultrasound markers in fetal chromosomal abnormality screening. Chin J Med Imag Technol. 2016;32(05):765–768. doi:10.13929/j.1003-3289.2016.05.034
17. Bromley B, Shipp TD, Lyons J, Groszmann Y, Navathe RS, Benacerraf BR. What is the importance of second-trimester “soft markers” for trisomy 21 after an 11- to 14-week aneuploidy screening scan? J Ultrasound Med. 2014;33(10):1747–1752. doi:10.7863/ultra.33.10.1747
18. Cao P, Zhu X, Gu L, Liu W, Li J. Analysis of related phenotype of prenatal cases with copy number variations in various region of 22q11.2. Chin J Med Genet. 2021;38(11):1055–1059. doi:10.3760/cma.j.cn511374-20200818-00606
19. Ruan A, Ge Y, Cai M, et al. Correlation analysis between fetal choroid plexus cyst and fetal chromosome abnormality. Chin J Ultrasound Med. 2022;38(04):406–409. doi:10.3969/j.issn.1002-0101.2022.04.013
20. Xu M. Meta-analysis of common ultrasonic soft markers in prenatal diagnosis. J Qinghai Univ. 2020. doi:10.27740/d.cnki.gqhdx.2020.000263
21. Xu H, Song T, Zheng J, et al. Analysis of prenatal diagnosis results of 212 fetuses with abnormal nasal bone development. Hainan Med J. 2020;31(21):2778–2781. doi:10.3969/j.issn.1003-6350.2020.21.017
22. Hu Y, Liu W, He G, Xu J, Peng Y, Wang J. Clinical utility of expanded NIPT for chromosomal abnormalities and etiology analysis of cytogenetic discrepancies cases. J Assist Reprod Genet. 2022;39(1):267–279. doi:10.1007/s10815-021-02351-6
23. Zhai X, Lu Q, Lai C, et al. Clinical significance of non-invasive prenatal testing technology for fetal chromosome copy number variation detection. Lab Med Clin. 2022;19(08):1070–1074. doi:10.3969/j.issn.1672-9455.2022.08.015
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
