Back to Journals » Journal of Inflammation Research » Volume 16
Application of Circulating Tumor Cells and Interleukin-6 in Preoperative Prediction of Peritoneal Metastasis of Advanced Gastric Cancer
Received 30 March 2023
Accepted for publication 16 June 2023
Published 20 July 2023 Volume 2023:16 Pages 3033—3047
DOI https://doi.org/10.2147/JIR.S414786
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Zitao Liu,1 Huakai Tian,2 Zhengming Zhu1
1Department of Gastrointestinal Surgery, The Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, People’s Republic of China; 2Department of Gastrointestinal Surgery, The First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, People’s Republic of China
Correspondence: Zhengming Zhu, Department of Gastrointestinal Surgery, The Second Affiliated Hospital of Nanchang University, 1 MinDe Road, Nanchang, Jiangxi, 330006, People’s Republic of China, Tel +8613970880051, Email [email protected]
Background: The purpose of this study was to explore the clinical significance of circulating tumor cells (CTCs) and cytokines in peripheral blood in preoperative prediction of peritoneal metastasis (PM) in advanced gastric cancer (AGC).
Methods: The clinicopathological characteristics of 282 patients with AGC were retrospectively analyzed. The patients were divided into training and validation groups according to the time of receiving treatment. We used univariate analysis and multivariate logistic regression analysis to screen out the independent risk factors of PM in AGC. Then, we incorporated independent risk factors into the nomogram, and evaluated the discriminative ability.
Results: The levels of CTCs and interleukin-6 (IL-6) of AGC patients with PM were higher than those without PM (P< 0.05). Moreover, the levels of CTCs and IL-6 in the occult peritoneal metastasis (OPM) group and the CT-positive PM group were higher than those in the negative PM (P< 0.05). Multivariate logistic regression analysis showed that IL-6 > 12.22 pg/mL, CTCs > 4/5mL, CA724 > 6 IU/mL, CA125 > 35 U/mL and tumor size > 5 cm were independent risk factors for PM of AGC. The area under the ROC curve of the nomogram were 0.898 and 0.926 in the training and validation sets, respectively. The clinical decision curve showed that the nomogram had good clinical utility.
Conclusion: CTCs and IL-6 in peripheral blood are promising biomarkers for predicting the risk of PM in AGC. The nomogram constructed from five risk factors can effectively assess the risk of PM in AGC patients individually.
Keywords: circulating tumor cell counts, interleukin-6, advanced gastric cancer, peritoneal metastasis, occult peritoneal metastasis
Introduction
Gastric cancer is the fifth most common malignancy and the third leading cause of cancer death worldwide.1 Peritoneal metastasis is the common way of distant metastasis of gastric cancer and the main cause of poor prognosis. Previous studies have shown that the median survival time of peritoneal metastases is only 3–6 months.2–4 Once a patient is diagnosed with peritoneal metastases, traditional gastrectomy and regional lymph node dissection will no longer be the optimal treatment options.5 Recent studies have shown that hyperthermic intraperitoneal chemotherapy (HIPEC) + cytoreductive surgery (CRS), conversion therapy and targeted therapy can improve the prognosis of gastric cancer patients with peritoneal metastasis, and even some patients with early peritoneal metastasis have the opportunity of surgical resection after comprehensive treatment. Therefore, early and accurate diagnosis of peritoneal metastases is essential to formulate the optimal treatment plan and avoid unnecessary surgery.6–9
CT scans are routine examinations for the clinical diagnosis of peritoneal metastases.10 CT scans mainly diagnosed peritoneal metastasis by imaging features such as omental cake, massive ascites, peritoneal thickening, and nodular signal enhancement. However, these manifestations are usually seen in the late stage of peritoneal metastases, which makes tiny metastases easily missed.11 Previous studies have shown that the sensitivity of CT for diagnosing peritoneal metastases is only 25%–50%.12,13 Therefore, about 10% ~ 30% of advanced gastric cancer patients have no signs of peritoneal metastasis on preoperative CT examination, but they are diagnosed with positive peritoneal metastasis during surgery, which is clinically called occult peritoneal metastasis (OPM).14,15 Positron emission tomography/computed tomography (PET/CT) has been favored by clinicians because of its sensitivity in detecting distant metastases of organs. However, there are significant differences in FDG uptake among different histological types of gastric cancer, such as signet ring cell carcinoma and mucinous adenocarcinoma have very low uptake of FDG.16 Therefore, these deficiencies, such as inaccurate localization of lesions, high false-negative rate due to inconsistent tumor uptake of FDG and high cost, limit the clinical application of PET-CT. Laparoscopy plus pathological biopsy is the gold standard for diagnosing peritoneal metastases.10 Clinicians are controversial about the widespread use of laparoscopy in the detection of peritoneal metastases due to its associated surgical complications, mental and physical trauma, and high cost.17,18 Therefore, a non-invasive and accurate method for preoperative prediction of peritoneal metastasis is urgently needed.
Circulating tumor cells (CTCs) are defined as tumor cells that shed from primary or metastatic foci into the blood circulation during tumor formation and progression, and have the potential to develop into metastatic lesions.19 The detection of CTCs in peripheral blood is one of the methods of liquid biopsy, which has important value in the early detection of cancer, evaluation of therapeutic efficacy and prognosis.20–22 Currently, CTCs have been approved by the FDA as biomarkers for monitoring the prognosis of patients with breast, prostate, and colorectal cancer.23 However, it remains unclear whether CTCs in peripheral blood are associated with peritoneal metastasis of gastric cancer. In addition, cytokines, as signaling and effector molecules, play an important role in the tumor microenvironment (TME).24 Cytokines are of great value in regulating complex systems of pro-tumor and anti-tumor.25 At present, some studies have confirmed that cytokines are closely related to the occurrence, invasion, metastasis and prognosis of gastric cancer.26,27 However, there are few studies on the relationship between cytokines in peripheral blood and peritoneal metastasis in patients with gastric cancer. Therefore, the purpose of our study was to explore the correlation between CTCs and cytokines in peripheral blood and peritoneal metastasis of gastric cancer, and to construct a nomogram that preoperatively predicts peritoneal metastasis of gastric cancer, which can help to formulate the best treatment plan in clinic.
Materials and Methods
Patients
A total of 282 patients with AGC who were treated in the Second Affiliated Hospital of Nanchang University from May 2020 to June 2022 were selected for this retrospective study. Patients treated between May 2020 and December 2021 served as the training set (n=215), and those treated between January 2022 and June 2022 served as the validation set (n=67). Inclusion criteria: 1. Patients with postoperative pathological diagnosis of advanced gastric cancer or peritoneal metastasis, or patients with peritoneal metastasis diagnosed by a multidisciplinary team; 2. Peripheral blood tests, CTCs, and cytokine detection were performed before receiving any treatment. Exclusion criteria: 1. The postoperative pathological diagnosis is early gastric cancer, because the possibility of peritoneal metastasis in early gastric cancer is very low; 2. Gastric stump cancer, combined with other tumors, or distant metastasis found in other organs (except peritoneal metastasis); 3. Receive neoadjuvant chemoradiotherapy or targeted therapy; 4. Patients with infection at admission; 5. Patients with blood system diseases, or combined with liver, kidney and heart dysfunction; 6. Incomplete clinical data and examination.
Diagnosis of Peritoneal Metastasis
All the patients in this study received enhanced CT scans or PET-CT scans. When a patient’s examination report suspected peritoneal metastases, our multidisciplinary team (MDT) conducted a case discussion. If the multidisciplinary team believed that there was sufficient evidence of peritoneal metastasis, the diagnosis was made directly; conversely, if the evidence was insufficient, laparoscopy and pathological biopsy were performed. When the patient’s CT showed no signs of peritoneal metastasis, the surgeon performed laparoscopy, peritoneal lavage and exfoliative cytology. If there were no macroscopic metastases during the operation, gastrectomy and regional lymph node dissection would be performed.
Clinicopathologic Characteristics
Clinicopathological characteristics of patients were obtained from the hospital’s electronic health record system. Clinical data mainly include: gender, age, history of hypertension, history of diabetes, and body mass index (BMI). In addition, blood test indexes such as tumor markers, albumin, fibrinogen and inflammatory markers were collected when patients did not receive any treatment at admission. The levels of inflammatory markers were divided into high and low groups according to the best cut-off value of the ROC curve. The levels of CEA, CA125, CA199 and CA724 in this research center were considered abnormal when they were above 5.0 ng/mL, 37.0 U/mL, 35.0 U/mL and 6 IU/mL, respectively. The location, maximum diameter and Borrmann type of the tumor were determined according to the results of the gastroscopy. The tumor location was divided into upper 1/3, middle 1/3 and lower 1/3 of stomach. The tumors were divided into two groups based on the maximum diameter of 5 cm. According to the pathological results, the histological types were divided into: high and moderately differentiated adenocarcinoma group, poorly differentiated adenocarcinoma group, signet ring cell carcinoma and undifferentiated carcinoma group.
The Detection of CTCs
5mL peripheral blood sample was taken before the patient received any treatment, and blood samples were tested within 8 hours to minimize cell damage. In this study, we used the detection technology of the Cyttel platform, which uses immunomagnetic bead negative enrichment combined with immunofluorescence in situ hybridization (im-FISH) to detect CTCs count. The experimental methods for CTCs detection are as follows: 1. Negative enrichment operation. We performed plasma separation, lysis of red blood cells, and specific removal of leukocytes by immunomagnetic beads on peripheral blood samples, so as to preserve the rarest cells in the peripheral blood samples. 2. Immunofluorescence in situ hybridization (im-FISH) operation. CTCs were identified by the characteristics of high-frequency chromosomal aneuploidy and CD45-negative in tumor cells. The enriched rare cells were hybridized with fluorescent probes of chromosomes 8 and 17, stained with CD45, and counterstained with DAPI. Finally, the circulating tumor cells were observed and counted under fluorescence microscopy. If the observed cells have characteristics such as CD45-, DAPI+ and chromosome 8 or 17 fluorescent probe signal point ≧3, they are identified as CTCs (Figure 1). Compared with antigen-dependent methods, this detection technique can avoid false positives caused by epithelial-mesenchymal transition (EMT) in some normal cells, and effectively improve the detection rate of CTCs.
Cytokine Assays
2mL peripheral blood sample was taken before the patient received any treatment. In this study, the levels of 12 cytokines (IL-5, IFN-a, IL-2, IL-6, IL-1 β, IL-10, IFN-γ, IL-8, IL-17, IL-4, IL-12P70, TNF-a) in peripheral blood were measured by flow cytometry. The twelve cytokine assay kits used in the study were purchased from Qingdao Raisecare Biotechnology Company. We strictly followed the instructions of the kits during the experiment. The experimental methods were as follows: 1. Prepared matrix B, experimental buffer and different final concentrations of standard products; 2. Added the diluted sample, capture microsphere antibody, detection antibody and SA-PE to the standard product in turn, and incubated in the dark; 3. Resuspended the microspheres by vortexing; 4. We used a flow cytometer for detection, and calculated the level of cytokines according to the standard curve.
Statistical Analysis
For continuous variables, we first used single sample K–S test for normality test. If the data conformed to a normal distribution, it was described by the mean and standard deviation, and the data were analyzed by the t-test. Otherwise, they were described by the median and interquartile range, and the data were analyzed by the Mann–Whitney U-test. The categorical variables were described with rates, the Chi square test (or Fisher’s exact test in specific conditions) was used for data analysis. The random forest algorithm was used to rank the importance of meaningful variables in univariate analysis. Random forest algorithm is one of the ways of machine learning, which is a supervised learning method and can be regarded as an extension of decision tree. In the random forest algorithm, the greater the Mean Decrease Accuracy of the variable, the greater the importance. These variables that were significant in the univariate analysis were included in multivariate logistic analysis. We used the stepwise backward regression method to analyze the risk factors of peritoneal metastasis of advanced gastric cancer. A nomogram was constructed according to the results of the multivariate logistic regression analysis. The C-index, ROC curve and PR curve were used to evaluate the predictive ability of the nomogram. The calibration curve and Brier score were used as indicators to evaluate the internal calibration, and the Hosmer-Lemeshow test was used to evaluate the goodness of fit of the nomogram. In addition, in order to measure the clinical utility of the nomogram, the net benefit was measured by the clinical decision curve. Finally, 100 times 10-fold cross-validation was used for internal validation, and the performance of the model was evaluated by area under the ROC curve (AUC), goodness of fit (R-Squared), discrimination index (D) and Brier score. Data analysis was performed in the R language (version 4.1.1). In all statistical analyses, P values (two-sided) < 0.05 were considered statistically significant.
Results
Patient Characteristics
The clinicopathological characteristics of the patients are shown in Table 1. Among the 282 patients with AGC, 87 (30.9%) were diagnosed as PM positive. In the training set (n=215), 72 (33.5%) cases were complicated with peritoneal metastasis. All 72 patients with peritoneal metastases received whole-abdominal enhanced CT scans before surgery. 37 patients with peritoneal metastases were diagnosed by CT scans, and the detection rate of CT scans was only 51.4%. Another 35 patients showed no signs of peritoneal metastases on preoperative CT scans, they were finally diagnosed with peritoneal metastases by laparoscopy and pathological biopsy. Of which 1 (1/35) patients had no macroscopic lesions under laparoscopy, but abdominal exfoliation cytology was positive. The incidence of occult peritoneal metastases was 16.3%. In the validation set (n=67), 15 (22.4%) cases were PM positive, of which 6 (9.0%) cases were OPM positive.
 |
Table 1 Univariate Analysis of Preoperative Clinicopathological Factors |
In the training set, the median age of the patients was 66.0 years, and the interquartile range was 58.0–72.0 years. The maximum diameter of tumor under endoscope was less than 5 cm in 54.9% of patients. The tumors usually occurred in the lower third of the stomach, the most common type was Borrmann type III (invasive ulcer type). The histological type was poorly differentiated adenocarcinoma in 51.6% of patients. The pathological TNM stages of 215 patients with advanced gastric cancer were as follows: 10 cases of stage I, 45 cases of stage II, and 88 cases of stage III, including 39 cases of stage IIIA, 30 cases of stage IIIB, 19 cases of stage IIIC, and stage IV with peritoneal metastasis 72 cases.
Association of CTCs and Cytokines with Peritoneal Metastasis
CTCs were detected in peripheral blood in 245 of 282 patients with AGC, and the detection rate of CTCs was 86.9%. In the training set (n=215), 184 (85.6%) patients detected CTCs in peripheral blood. The other 31 patients were negative for CTCs in peripheral blood, including 22 patients with negative peritoneal metastasis, 6 patients with occult peritoneal metastasis (OPM), and the remaining 3 patients with positive peritoneal metastasis diagnosed by preoperative CT. In the validation set (n=67), 61 cases (91.0%) were positive for CTCs and 6 cases were negative for CTCs, all of which were negative for peritoneal metastasis. The counts of CTCs in gastric cancer with peritoneal metastasis were higher than those without peritoneal metastasis in the training set (P=0.008) (Table 1, Figure 2A). According to the cutoff value of the ROC curve, CTCs were divided into two groups with 4/5 mL as the boundary. 60% of patients with peritoneal metastasis had a count of more than 4 CTCs in the peripheral blood (Figure 2B). In addition, the counts of CTCs in the occult peritoneal metastasis group and the CT-positive peritoneal metastasis group were higher than those in the negative peritoneal metastasis group (P<0.05), but there was no significant difference between the two groups (Figure 2C). The CTCs count of stage IV combined with peritoneal metastasis was higher than that of stage I/II and stage IIIA (P<0.05), but it was not significantly different from that of stage IIIB/IIIC, and the CTCs count of both stage IIIA and stage IIIB/IIIC was also higher than that of stage I/II (P<0.05) (Figure 2D).
We analyzed 12 cytokines in peripheral blood, and the results showed that only 3 cytokines (IL-6, IL-1β and IL-8) were different between the peritoneal metastasis group and the without peritoneal metastasis group (P<0.05) (Table 1) (Figure 2). However, only the levels of IL-6 differed between PM-positive and PM-negative groups in the validation set. IL-6, IL-1β and IL-8 were classified into high and low groups according to the optimal cut-off values of the ROC curve, which were 12.220 pg/mL, 4.365 pg/mL and 4.795 pg/mL, respectively. In addition, the levels of IL-6 in the occult peritoneal metastasis group and CT-positive peritoneal metastasis group were higher than those in the negative peritoneal metastasis group (P < 0.05), but there was no statistical difference between the two groups (Figure 2G). The level of IL-6 in stage IV with peritoneal metastasis was higher than that in stage I/II and stage III (P<0.05), and the level of IL-6 in stage III was also higher than that in stage I/II, but there was no statistical significance (Figure 2H).
Univariate and Multivariate Analyses
The correlations between the variables are shown in Figure 3A. Univariate analysis showed that 12 variables, including the degree of differentiation, tumor size, BMI, fibrinogen, neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), fibrinogen-to-albumin ratio (FAR), CA125, CA724, CTCs, IL-6 and IL-1β, were associated with peritoneal metastasis of advanced gastric cancer (Table 1). The random forest algorithm was used to rank the importance of the above 12 variables, and the results showed that the top four variables were CA125, CA724, CTCs and tumor size in order (Figure 3B). Multivariate analysis showed that IL-6 > 12.220 pg/mL (OR=2.435, P=0.042), CTCs > 4/5 mL (OR=7.981, P<0.001), CA724 > 6.000 IU/mL (OR=2.837, P =0.015), CA125 > 35.000 U/mL (OR=28.988, P<0.001) and tumor size > 5.000 cm (OR=9.279, P<0.001) were independent risk factors for peritoneal metastasis of advanced gastric cancer (Table 2).
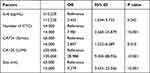 |
Table 2 Multivariate Analysis of the Correlation Between Preoperative Clinicopathological Factors and Peritoneal Metastasis of Gastric Cancer |
Development and Validation of the Nomogram
Based on the results of multivariate analysis, we constructed a nomogram for preoperatively predicting the risk of peritoneal metastasis in advanced gastric cancer (Figure 4). Each variable in the nomogram was assigned a weighted score, and the scores for each variable were summed to get the patient’s individualized total score. The higher the total score, the higher the risk of peritoneal metastasis. The C-index of the nomogram was 0.898, the C-index after 1000 Bootstrap corrections was 0.888. The areas under the ROC curve in the training and validation sets were 0.898 and 0.926, respectively (Figure 5A). The area under the PR curve was 0.840 (Figure 5B). These values indicated that the nomogram had good discrimination ability. The P value of the Hosmer-Lemeshow test was 0.411, showing a good fit of the nomogram. The calibration curve showed that the nomogram predicted the risk of peritoneal metastasis in good agreement with the actual probability (Figure 6A). The Brier score was 0.112, suggesting that the model’s predictions were well calibrated. The accuracy, sensitivity, specificity, positive predictive value and negative predictive value of the nomogram were 82.33%, 85.31%, 76.39%, 87.77% and 72.37%, respectively. Additionally, we constructed Model2 based on variables (CA125, CA724, and tumor size) that previous studies had demonstrated to be associated with peritoneal metastasis. ROC curve and clinical decision curve (DCA) showed that the prediction model had good clinical practicability, and patients could obtain greater net benefit (Figure 6B and C).
 |
Figure 5 (A) The receiver operating characteristic curve (ROC) of the nomogram. (B) The PR curve of the nomogram. |
We used 100 times 10-fold cross-validation for internal validation. The mean area under the ROC curve (AUC), goodness of fit (R-Squared), discrimination index (D) and Brier score after validation were 0.887, 0.463, 0.396 and 0.122, respectively (Table 3). The discrimination index is above 0.40 points, which means that the discrimination ability of the model is very excellent; Between 0.30–0.39, the discrimination ability is good. If it is less than 0.30, it means that the model needs to be modified. The Brier score is a parameter that measures probabilistic calibration. The smaller the value, the better the predictive calibration. After cross-verification, these metrics change little, which proves that the model performs well enough and has good generalization ability.
 |
Table 3 The Multi-Indicator Combined with 100 Times ten-Fold Cross-Validations Evaluates the Nomogram |
Discussion
Peritoneal metastasis is the most common way of distant metastasis of gastric cancer and the main cause of poor prognosis. In this study, we constructed a nomogram model for predicting peritoneal metastasis based on CTCs and IL-6 in preoperative peripheral blood. The nomogram provides an easy-to-use, individualized and sensitive tool for clinical diagnosis of peritoneal metastasis, which is helpful for early identification of peritoneal metastasis and making the best individualized treatment plan.
As a liquid biopsy method for solid tumors, circulating tumor cell detection has attracted more and more attention due to its advantages of high repeatability, non-invasiveness, and true reflection of tumor burden.20 In recent years, circulating tumor cells in peripheral blood have been considered as promising biomarkers for early diagnosis, postoperative recurrence and metastasis monitoring, efficacy evaluation, drug resistance monitoring, prognosis evaluation, and immunosuppressive target detection of gastric cancer.20–22,28 Joon et al confirmed that high levels of CTCs and TWIST (+) CTCs in peripheral blood of gastric cancer patients were associated with poorer prognosis.21 In patients with unresectable gastric cancer, high levels of CTCs before and during chemotherapy indicated poor OS, PFS and DC rates.29 Mishima et al found that patients with advanced gastric cancer whose primary tumor was HER2- but CTCs HER2+ could benefit from trastuzumab treatment.30 Yue et al’s study found that the level of CTCs with high PD-L1 expression could be used as a predictive indicator for screening patients with PD-1/PD-L1 blockade therapy, and detecting the dynamic changes of CTCs was helpful for early observation of treatment response.31 In this study, we found that the count of CTCs in gastric cancer with peritoneal metastasis was higher than that in the group without peritoneal metastasis, and the count of CTCs in the group with occult peritoneal metastasis was also higher than that in the group without peritoneal metastasis, which is helpful for preoperative diagnosis of OPM. In addition, we also found that the later the TNM stage of the tumor, the higher the count of CTCs in peripheral blood. The count of CTCs in patients with stage IV gastric cancer was significantly higher than that in stage I/II and IIIA, and the count of CTCs in patients with stage IIIA and IIIB/IIIC was also higher than that in stage I/II (P<0.05), but there was no significant difference between stage IV and IIIB/IIIC, which may be related to the small sample size. Peritoneal metastasis is closely related to tumor infiltration beyond the gastric serosa or later TNM stage. Therefore, we can reflect tumor burden and TNM stage by detecting CTCs counts in peripheral blood of gastric cancer patients, which indirectly help us assess the risk of peritoneal metastasis. Finally, the results showed that CTCs > 4/5 mL was an independent risk factor for peritoneal metastasis of advanced gastric cancer.
The enrichment and identification of CTCs is a key step in the detection of CTCs. At present, these detection methods can be roughly divided into antigen-dependent and antigen-independent methods. Antigen-dependent methods are mainly based on the highly expressed antigens on the surface of CTC. According to the surface markers, they can be divided into epithelial type (such as EpCAM, CK), interstitial type (vimentin, CD44 or TWIST) and mixed type. The main characteristic of the antigen-independent method is that it does not depend on the expression of tumor cell-specific markers and the physical properties of tumor cells. The representative technique is the negative enrichment technique. Compared with antigen-dependent methods, this method can avoid false positives caused by high expression of these markers in normal epithelial cells, and missed detection caused by loss of surface markers in CTCs undergoing EMT or MET processes.20–22 In this study, we used negative enrichment combined with immuno-fluorescence in situ hybridization (im-FISH) to detect CTCs in peripheral blood. The detection rate of CTCs was 86.9%. The detection rate of CTCs in this study was significantly higher than that of previous studies using the CellSearch platform,32,33 which may be related to the improvement of detection technology and the inclusion of only advanced gastric cancer patients in the study. Although this study has a high detection rate, there are still 37 patients with negative CTCs in peripheral blood, including 9 patients with peritoneal metastasis. The negative CTCs in peripheral blood of advanced gastric cancer may be related to the high heterogeneity of gastric cancer, but the specific reason is still unclear and needs further study.
As signal and effector molecules, cytokines play an important role in determining T helper cell differentiation, activating and regulating other immune cells. It can also regulate transcription factors and other intracellular signal pathways to play a role in tumor growth and metastasis.26 Therefore, different cytokine expression patterns may be associated with specific pathways of gastric cancer progression and different prognosis.25,26 Gunjigake et al found that IL-17A could inhibit the expression of E-cadherin and increase the expression of α-SMA in peritoneal mesothelial cells through the STATS pathway, thereby promoting peritoneal fibrosis and leading to peritoneal metastasis.27 Epithelial-mesenchymal transition (EMT) is a key step in the occurrence of peritoneal metastasis, and cytokines (IL-17A, IL-8, TGF-β) and chemokines are important factors in the induction of EMT.26 In addition, cytokines produced locally by the tumor may be released into the blood and can be detected in peripheral plasma. Norma et al found that the levels of IL-6, IFN-γ, and IL-10 in peripheral blood of gastric cancer patients were higher than those of healthy controls.34 In the study of Kim et al, it was found that preoperative high IL-6 levels were associated with lymph node metastasis, late TNM staging, postoperative recurrence and poor prognosis of gastric cancer.35 Li et al found that IL-6, IL-8 and TNF-α were superior to traditional tumor markers in early detection of gastric cancer.36 In this study, we found that the median levels of IL-6, IL-1β and IL-8 in the peritoneal metastasis group were higher than those in the non-peritoneal metastasis group, and the IL-6 level in the occult peritoneal metastasis group was also higher than that in the advanced gastric cancer group. IL-6 > 12.220 pg/mL is an independent risk factor for peritoneal metastasis of gastric cancer. In addition, our study also confirmed that the preoperative high level of IL-6 was closely associated with the later TNM stage of gastric cancer. The level of IL-6 in stage IV gastric cancer patients with peritoneal metastasis was significantly higher than that in stage I/II and III (P<0.05). Therefore, preoperative detection of IL-6 levels in peripheral blood is helpful to accurately predict the risk of peritoneal metastasis of gastric cancer.
Serum tumor markers are widely used in clinical diagnosis, prognosis evaluation and disease monitoring of gastrointestinal tumors. Huang et al found that preoperative high levels of CA125, CA199 and CA724 in gastric cancer patients were closely related to peritoneal metastasis.37 Yang et al found that elevated serum CA125 levels were significantly associated with occult peritoneal metastases.38 However, Chen et al showed that preoperative CA199 and CEA levels were completely unrelated to peritoneal metastasis.39 The results of Qin et al also showed that serum tumor markers could not effectively predict peritoneal metastasis.40 In this study, the results showed that the levels of CA125 and CA724 in the peritoneal metastasis group were significantly higher than those in the non-peritoneal metastasis group. CA125 was considered to be the most important variable in the importance ranking of the random forest algorithm. In addition, the weight score assigned by CA125 in the nomogram was also the largest. Therefore, preoperative CA125 and CA724 levels are effective indicators for predicting peritoneal metastasis of advanced gastric cancer.
In recent years, some studies have confirmed that tumor-related inflammation is closely related to the proliferation, invasion, metastasis and prognosis of gastric cancer.41,42 Zhao et al showed that decreased lymphocyte count in peripheral blood was closely related to peritoneal metastasis.43 Chen et al showed that the preoperative platelet/lymphocyte ratio (PLR) was an effective indicator for predicting peritoneal metastasis.39 Nakamura et al showed that preoperative neutrophil/lymphocyte ratio (NLR) was an independent predictor of peritoneal metastasis.44 In this study, fibrinogen, NLR, and PLR were associated with peritoneal metastasis in univariate analysis, but they were not independent risk factors for peritoneal metastasis in multivariate analysis. This result is somewhat different from previous studies, which may be related to the inclusion of only advanced gastric cancer patients in this study. Therefore, the role of inflammatory markers in predicting peritoneal metastasis of gastric cancer needs to be further investigated.
Some previous studies have shown that some clinicopathological features of patients with gastric cancer were also associated with peritoneal metastasis, such as Borrmann IV, tumor size (> 5 cm), signet ring cell carcinoma, undifferentiated cancer, female and Lauren diffuse gastric cancer were independent risk factors for peritoneal metastasis.15,45,46 In this study, univariate analysis showed that the degree of differentiation and tumor size (>5 cm) were associated with peritoneal metastasis, while multivariate analysis showed that only tumor size (>5 cm) was an independent predictor of peritoneal metastasis. We suggest that the increased degree of tumor invasion may increase the probability of tumor cell shedding from the primary tumor, thereby increasing the risk of peritoneal metastasis.
There are some limitations in this study. First of all, this study is a retrospective study with a small sample size, which may have some selectivity bias. The prediction model is only validated internally, not externally, so it needs to be further verified by multicenter big data research. Second, due to the small number of patients with occult peritoneal metastases in this study, we did not construct a nomogram for predicting occult peritoneal metastases. Then, some clinical factors were not included in this study, such as Lauren typing, tumor growth factor (TGF-β), circulating tumor microthrombi (CTM), and molecular phenotype on the surface of CTCs. Finally, radiomics is a hot research area, it is hoped that the accuracy of the model can be improved by combining radiomics in the future.
Conclusion
CTCs and IL-6 in peripheral blood are promising biomarkers for predicting the risk of peritoneal metastasis in gastric cancer. The predictive model constructed from five risk factors has good predictive ability and clinical utility, which can help clinicians diagnose peritoneal metastasis early and tailor the best individualized treatment.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of our institutional research committee and were performed in accordance with the Declaration of Helsinki. This study was approved by the Ethics Committee of the Second Affiliated Hospital of Nanchang University, and all patients signed informed consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Key Research and Development Program of Jiangxi Province (Grant Number: 20202BABL206091).
Disclosure
All authors declare no conflict of interest.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Thomassen I, van Gestel YR, van Ramshorst B, et al. Peritoneal carcinomatosis of gastric origin: a population-based study on incidence, survival and risk factors. Int J Cancer. 2014;134(3):622–628. doi:10.1002/ijc.28373
3. Fujitani K, Yang HK, Mizusawa J, et al. Gastrectomy plus chemotherapy versus chemotherapy alone for advanced gastric cancer with a single non-curable factor (REGATTA): a Phase 3, randomised controlled trial. Lancet Oncol. 2016;17(3):309–318. doi:10.1016/S1470-2045(15)00553-7
4. Coccolini F, Gheza F, Lotti M, et al. Peritoneal carcinomatosis. World J Gastroenterol. 2013;19(41):6979–6994. doi:10.3748/wjg.v19.i41.6979
5. Yonemura Y, Prabhu A, Sako S, et al. Long term survival after cytoreductive surgery combined with perioperative chemotherapy in gastric cancer patients with peritoneal metastasis. Cancers. 2020;12(1):116. doi:10.3390/cancers12010116
6. Gamboa AC, Winer JH. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for gastric cancer. Cancers. 2019;11(11):1662. doi:10.3390/cancers11111662
7. Bonnot PE, Piessen G, Kepenekian V, et al. Cytoreductive surgery with or without hyperthermic intraperitoneal chemotherapy for gastric cancer with peritoneal metastases (CYTO-CHIP study): a propensity score analysis. J Clin Oncol. 2019;37(23):2028–2040. doi:10.1200/JCO.18.01688
8. Van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet. 2016;388(10060):2654–2664. doi:10.1016/S0140-6736(16)30354-3
9. Sato Y, Ohnuma H, Nobuoka T, et al. Conversion therapy for inoperable advanced gastric cancer patients by docetaxel, cisplatin, and S-1 (DCS) chemotherapy: a multi-institutional retrospective study. Gastric Cancer. 2017;20(3):517–526. doi:10.1007/s10120-016-0633-1
10. Smyth EC, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v38–v49. doi:10.1093/annonc/mdw350
11. Diop AD, Fontarensky M, Montoriol PF, Da Ines D. CT imaging of peritoneal carcinomatosis and its mimics. Diagn Interv Imaging. 2014;95(9):861–872. doi:10.1016/j.diii.2014.02.009
12. Kim SJ, Kim HH, Kim YH, et al. Peritoneal metastasis: detection with 16- or 64-detector row CT in patients undergoing surgery for gastric cancer. Radiology. 2009;253(2):407–415. doi:10.1148/radiol.2532082272
13. Kwee RM, Kwee TC. Modern imaging techniques for preoperative detection of distant metastases in gastric cancer. World J Gastroenterol. 2015;21(37):10502–10509. doi:10.3748/wjg.v21.i37.10502
14. Burbidge S, Mahady K, Naik K. The role of CT and staging laparoscopy in the staging of gastric cancer. Clin Radiol. 2013;68(3):251–255. doi:10.1016/j.crad.2012.07.015
15. Dong D, Tang L, Li ZY, et al. Development and validation of an individualized nomogram to identify occult peritoneal metastasis in patients with advanced gastric cancer. Ann Oncol. 2019;30(3):431–438. doi:10.1093/annonc/mdz001
16. Shimada H, Okazumi S, Koyama M, Murakami K. Japanese Gastric Cancer Association Task Force for Research Promotion: clinical utility of 18F-fluoro-2-deoxyglucose positron emission tomography in gastric cancer. A systematic review of the literature. Gastric Cancer. 2011;14(1):13–21. doi:10.1007/s10120-011-0017-5
17. Fukagawa T. Role of staging laparoscopy for gastric cancer patients. Ann Gastroenterol Surg. 2019;3(5):496–505. doi:10.1002/ags3.12283
18. Li K, Cannon JGD, Jiang SY, et al. Diagnostic staging laparoscopy in gastric cancer treatment: a cost-effectiveness analysis. J Surg Oncol. 2018;117(6):1288–1296. doi:10.1002/jso.24942
19. Yap TA, Lorente D, Omlin A, Olmos D, de Bono JS. Circulating tumor cells: a multifunctional biomarker. Clin Cancer Res. 2014;20(10):2553–2568. doi:10.1158/1078-0432.CCR-13-2664
20. Lee MW, Kim GH, Jeon HK, Park SJ. Clinical application of circulating tumor cells in gastric cancer. Gut Liver. 2019;13(4):394–401. doi:10.5009/gnl18484
21. Jhi JH, Kim GH, Park SJ, et al. Circulating tumor cells and TWIST expression in patients with metastatic gastric cancer: a preliminary study. J Clin Med. 2021;10(19):4481. doi:10.3390/jcm10194481
22. Thanh Huong P, Gurshaney S, Thanh Binh N, et al. Emerging role of circulating tumor cells in gastric cancer. Cancers. 2020;12(3):695. doi:10.3390/cancers12030695
23. Pantel K, Alix-Panabières C. Circulating tumour cells in cancer patients: challenges and perspectives. Trends Mol Med. 2010;16(9):398–406. doi:10.1016/j.molmed.2010.07.001
24. Oya Y, Hayakawa Y, Koike K. Tumor microenvironment in gastric cancers. Cancer Sci. 2020;111(8):2696–2707. doi:10.1111/cas.14521
25. Bockerstett KA, DiPaolo RJ. Regulation of gastric carcinogenesis by inflammatory cytokines. Cell Mol Gastroenterol Hepatol. 2017;4(1):47–53. doi:10.1016/j.jcmgh.2017.03.005
26. Yang E, Chua W, Ng W, Roberts TL. Peripheral cytokine levels as a prognostic indicator in gastric cancer: a review of existing literature. Biomedicines. 2021;9(12):1916. doi:10.3390/biomedicines9121916
27. Gunjigake K, Kinoshita J, Yamaguchi T, et al. Interleukin-17A derived from mast cells contributes to fibrosis in gastric cancer with peritoneal dissemination. Gastric Cancer. 2021;24(1):31–44. doi:10.1007/s10120-020-01092-2
28. Zheng Z, Bu Z, Liu X, et al. Level of circulating PD-L1 expression in patients with advanced gastric cancer and its clinical implications. Chin J Cancer Res. 2014;26(1):104–111. doi:10.3978/j.issn.1000-9604.2014.02.08
29. Zou K, Yang S, Zheng L, Wang S, Xiong B. Prognostic role of the circulating tumor cells detected by cytological methods in gastric cancer: a meta-analysis. Biomed Res Int. 2016;2016:2765464. doi:10.1155/2016/2765464
30. Mishima Y, Matsusaka S, Chin K, et al. Detection of HER2 amplification in circulating tumor cells of HER2-negative gastric cancer patients. Target Oncol. 2017;12(3):341–351. doi:10.1007/s11523-017-0493-6
31. Yue C, Jiang Y, Li P, et al. Dynamic change of PD-L1 expression on circulating tumor cells in advanced solid tumor patients undergoing PD-1 blockade therapy. Oncoimmunology. 2018;7(7):e1438111. doi:10.1080/2162402X.2018.1438111
32. Okabe H, Tsunoda S, Hosogi H, et al. Circulating tumor cells as an independent predictor of survival in advanced gastric cancer. Ann Surg Oncol. 2015;22(12):3954–3961. doi:10.1245/s10434-015-4483-6
33. Uenosono Y, Arigami T, Kozono T, et al. Clinical significance of circulating tumor cells in peripheral blood from patients with gastric cancer. Cancer. 2013;119(22):3984–3991. doi:10.1002/cncr.28309
34. Sánchez-Zauco N, Torres J, Gómez A, et al. Circulating blood levels of IL-6, IFN-γ, and IL-10 as potential diagnostic biomarkers in gastric cancer: a controlled study. BMC Cancer. 2017;17(1):384. doi:10.1186/s12885-017-3310-9
35. Kim DK, Oh SY, Kwon HC, et al. Clinical significances of preoperative serum interleukin-6 and C-reactive protein level in operable gastric cancer. BMC Cancer. 2009;9:155. doi:10.1186/1471-2407-9-155
36. Li J, Xu L, Run ZC, et al. Multiple cytokine profiling in serum for early detection of gastric cancer. World J Gastroenterol. 2018;24(21):2269–2278. doi:10.3748/wjg.v24.i21.2269
37. Huang C, Liu Z, Xiao L, et al. Clinical significance of serum CA125, CA19-9, CA72-4, and fibrinogen-to-lymphocyte ratio in gastric cancer with peritoneal dissemination. Front Oncol. 2019;9:1159. doi:10.3389/fonc.2019.01159
38. Yang C, Yang Y, Huang X, et al. A nomogram based on clinicopathologic features and preoperative hematology parameters to predict occult peritoneal metastasis of gastric cancer: a single-center retrospective study. Dis Markers. 2020;2020:1418978. doi:10.1155/2020/1418978
39. Chen XD, Mao CC, Wu RS, et al. Use of the combination of the preoperative platelet-to-lymphocyte ratio and tumor characteristics to predict peritoneal metastasis in patients with gastric cancer. PLoS One. 2017;12(4):e0175074. doi:10.1371/journal.pone.0175074
40. Qin R, Yang Y, Qin W, et al. The value of serum immunoglobulin G glycome in the preoperative discrimination of peritoneal metastasis from advanced gastric cancer. J Cancer. 2019;10(12):2811–2821. doi:10.7150/jca.31380
41. Liu Z, Ge H, Miao Z, Shao S, Shi H, Dong C. Dynamic changes in the systemic inflammation response index predict the outcome of resectable gastric cancer patients. Front Oncol. 2021;11:577043. doi:10.3389/fonc.2021.577043
42. Zhang LX, Wei ZJ, Xu AM, Zang JH. Can the neutrophil-lymphocyte ratio and platelet-lymphocyte ratio be beneficial in predicting lymph node metastasis and promising prognostic markers of gastric cancer patients? Tumor maker retrospective study. Int J Surg. 2018;56:320–327. doi:10.1016/j.ijsu.2018.06.037
43. Zhao J, Qin R, Chen H, et al. A nomogram based on glycomic biomarkers in serum and clinicopathological characteristics for evaluating the risk of peritoneal metastasis in gastric cancer. Clin Proteomics. 2020;17:34. doi:10.1186/s12014-020-09297-4
44. Nakamura N, Kinami S, Fujii Y, et al. The neutrophil/lymphocyte ratio as a predictor of peritoneal metastasis during staging laparoscopy for advanced gastric cancer: a retrospective cohort analysis. World J Surg Oncol. 2019;17(1):108. doi:10.1186/s12957-019-1651-3
45. Chen Y, Zhou Q, Wang H, et al. Predicting peritoneal dissemination of gastric cancer in the era of precision medicine: molecular characterization and biomarkers. Cancers. 2020;12(8):2236. doi:10.3390/cancers12082236
46. Chen X, Chen S, Wang X, et al. Analysis and external validation of a nomogram to predict peritoneal dissemination in gastric cancer. Chin J Cancer Res. 2020;32(2):197–207. doi:10.21147/j.issn.1000-9604.2020.02.07
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





