Back to Journals » Nature and Science of Sleep » Volume 15
APAP Treatment Acceptance Rate and Cost-Effectiveness of Telemedicine in Patients with Obstructive Sleep Apnea: A Randomized Controlled Trial
Authors Pei G , Ou Q, Lao M, Wang L, Xu Y, Tan J, Zheng G
Received 7 April 2023
Accepted for publication 27 July 2023
Published 4 August 2023 Volume 2023:15 Pages 607—622
DOI https://doi.org/10.2147/NSS.S416221
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Valentina Alfonsi
Guo Pei,1,2,* Qiong Ou,1,2,* Miaochan Lao,1 Longlong Wang,1 Yanxia Xu,1 Jiaoying Tan,1 Gaihong Zheng1
1Department of Sleep Center, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, 510080, People’s Republic of China; 2School of Medicine, South China University of Technology, Guangzhou, 510006, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qiong Ou, Department of Sleep Center, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, 510080, People’s Republic of China, Tel +86-13609717251, Email [email protected]
Purpose: This study evaluated the treatment acceptance rate and cost-effectiveness of the telemedicine model in clinical practice for adult patients with obstructive sleep apnea (OSA).
Patients and Methods: Patients admitted to the sleep center for snoring were randomly divided into telemedicine and control groups. Patients diagnosed with moderate-to-severe OSA using the Home Sleep Apnea Test (HSAT) were voluntarily treated with auto-adjusted positive airway pressure (APAP) therapy. The acceptance rate of the APAP treatment, cost of patient visits, time cost, and labor cost of doctors in the two groups were observed.
Results: A total of 57 subjects were included, with an average age of 40.12± 11.73 years, including 47 males (82.5%); 26 patients were in the telemedicine group, and 31 were in the control group. Follow-up results showed that the acceptance rate of APAP treatment was 57.7% and 54.8% in the telemedicine and control groups, respectively, with no significant difference between the two groups (p=0.829). The cost-benefit analysis showed that the telemedicine group reduced the cost of patients’ medical treatment [− 457.84(− 551.19,1466.87)] but increased the extra intervention frequency and time outside the doctor’s office. Further analysis showed that male subjects of older age, higher education level, distant residence, no fatty liver, poor sleep quality, severe insomnia, and higher OSA severity were more likely to receive telemedicine diagnosis and treatment.
Conclusion: The APAP treatment acceptance rate and compliance of OSA patients in the telemedicine group were similar to those in the control group, and the cost of patients’ medical treatment was reduced. However, telemedicine increases the frequency and duration of additional out-of-hospital interventions.
Keywords: home sleep apnea, auto-adjusted positive airway pressure, cost-benefit analysis, telemedicine, clinical diagnosis, adults
Introduction
Obstructive Sleep Apnea (OSA) is the most common sleep-disordered breathing characterized by repetitive airway collapses that could lead to multiple organ dysfunction, increased morbidity and mortality, and increased use of medical resources.1–3 At present, the continuous improvement in diagnosis rates does not meet the higher demand for healthcare, and the medical resources related to sleep, such as doctors, technicians, and health resources allocated to OSA, are insufficient.4 OSA management has not improved, and there is an urgent need to explore a new clinical diagnosis and treatment model to solve these problems.
In recent years, with the continuous development of information technology, telemedicine has rapidly developed in long-term postoperative and chronic disease management, and related measures are also improving. Current studies on OSA telemedicine have primarily focused on continuous positive airway pressure (CPAP) treatment compliance. Existing studies have shown that compared with conventional care,5 remote monitoring did not significantly improve adherence to CPAP therapy, but it increased outpatient attendance for OSA assessment, saved nursing time, and improved cost-effectiveness during follow-up.6–9 There are also reports that adherence to positive airway pressure (PAP) therapy is significantly improved by providing patients with information on the Internet regarding their use of the treatment10 CPAP remote monitoring and telemedicine may provide innovative and practical solutions for high-risk patients with OSA who are reluctant to receive treatment, allowing home care providers and physician resources to be allocated primarily to those most in need. The rate of CPAP treatment use is low due to different medical insurance payment systems in different countries, and it remains to be determined whether telemedicine can effectively improve the use rate for clinical diagnosis and treatment among patients with OSA.
Currently, telemedicine is not fully mature and is not widely used in clinical practice. The clinical and economic feasibilities of OSA management using telemedicine are unclear. The key to applying telemedicine in clinical practice is to explore the treatment acceptance rate and cost-benefit analysis of telemedicine in real-world OSA diagnosis and treatment and to establish a telemedicine model that ensures medical quality, a good cost-benefit ratio, and improved ventilator treatment compliance among patients with OSA. Therefore, our study compared the acceptance rate of APAP treatment and cost-effectiveness in clinical practice between telemedicine and control groups and observed patients’ compliance during follow-up in order to form a new model of integrated and remote monitoring, diagnosis, treatment, follow-up, and management of sleep disorders.
Materials and Methods
Study Design
This study was a prospective, single-center, randomized controlled trial. Participants who met the inclusion criteria were required to provide informed consent. The participants were registered, and their basic information and medical history were collected from the medical records. The subjects were randomly divided into telemedicine and control groups and followed up for six months (Figure 1). The experimental procedures conformed to the Declaration of Helsinki and were approved by the Ethics Review Committee of Guangdong Provincial People’s Hospital (KY-Q-2021-162-02), and the study was registered at the Chinese Clinical Trial Registry (Registration number: ChiCTR2300069870).
 |
Figure 1 Study flowchart. Abbreviations: HST, Home Sleep Apnea Test; OSA, Obstructive sleep apnea; APAP, Auto-adjusted positive airway pressure. |
Population
From November 2021 to November 2022, 326 patients visited the sleep clinic for snoring. After communicating with the researchers, 57 patients met the inclusion criteria and participated in the study. In the telemedicine group, the diagnostic equipment was sent back to the hospital by mail, and treatments and follow-ups were carried out via a remote APP (Application) on video/phone. In the control group, the subjects went to the sleep clinic in person for face-to-face treatment. Only the researchers knew about the groups; the patients were only told about the group’s treatment and follow-up plans. Patients who did not meet the requirements or refused to participate were scheduled for routine clinical management. The inclusion criteria were 1) age 18–65 years; 2) visitation to a sleep center, snoring complaints, suspicion of sleep apnea, and requirement for portable sleep monitoring; 3) ability to complete scale assessment and interview on time; and 4) familiarity with the Internet and ability to communicate online without obstacles. The exclusion criteria were: 1) absence of questionnaire and follow-up data; 2) previous diagnosis of OSA, central sleep apnea, tidal breathing, obesity hypoventilation syndrome, or narcolepsy; 3) history of PAP therapy, surgery, and other OSA treatments, or current requirement for oxygen therapy; 4) frequent business trips, irregular working hours, and night shifts within six months; 5) organic diseases such as tumors and coronary artery disease, or mental diseases such as anxiety and depression; and 6) age > 65 years or unfamiliarity with the Internet.
Randomization
Participants who completed the baseline interview were randomly assigned (1:1) to either the control or telemedicine groups. Randomization was carried out using the random number table method. First, patient labels were randomly numbered. Then, starting from any row or column in the random number table, three digits were read as a random number and input under the number. Thereafter, all the random numbers selected were numbered from small to large (those with the same random numbers were numbered in the order of first hand) and recorded in the third line. We defined numbers 1–27 as the control group and 28–57 as the intervention group, thus completing the grouping. This procedure was performed by non-research-related personnel. The randomization numbers were sequenced and sealed in envelopes not opened until the subjects provided informed consent. The subjects could withdraw at any time during the study.
Home Sleep Apnea Monitoring
After their first visit, subjects in the two groups were monitored overnight with the Home Sleep Apnea Test (HSAT) device (Alice Nightone, PHILIPS, USA). The subjects in the telemedicine group watched the teaching video and learned on the remote APP we developed and completed the HSAT. The subjects in the control group received face-to-face guidance from the research doctor in the outpatient department. The next day, the telemedicine group mailed the HSAT back to the sleep center, and the control group sent it back in person. A study doctor downloaded the data and interpreted the results. Any unqualified records were rescheduled for monitoring. Sleep monitoring data were manually analyzed and interpreted by trained physicians following the American Academy of Sleep Medicine’s Manual of Interpretation of Sleep and Related Events standards.11 The Apnea-Hypopnea Index (AHI) is the number of apneas and hypopneas per hour of sleep. According to the International Classification of Sleep Disorders, third edition (ICSD-3), PAP therapy is recommended for those with AHI≥15 times/hour or 5≤AHI<15 times/hour, with accompanying lethargy, wakefulness at night, hypertension or type 2 diabetes, and other diseases. In the telemedicine group, doctors communicated via video or telephone via the remote APP, interpreted the monitoring and diagnosis report in detail, and informed patients of the follow-up diagnosis and treatment process. In the control group, a doctor interpreted the report face-to-face at a sleep center and informed them about the follow-up procedures.
Home Pressure Titration
Patients diagnosed with OSA and voluntarily receiving auto-adjusted positive airway pressure (APAP) underwent a five-day home pressure titration (S10 AutoSetTM PlusC, ResMed, Australia; PHILIPS Auto-CPAP, USA). The subjects in the control group went to the sleep center to receive the APAP device. The sleep doctor introduced the working principle of APAP treatment, its benefits, and how to avoid and deal with the possible side effects, and demonstrated how to operate and maintain the APAP equipment. Subjects in the telemedicine group were sent the APAP device by the sleep doctor and watched the teaching and operation videos through the remote APP. The APAP setting for all the subjects was 4–20 cmH2O.
Auto-Adjusted Positive Airway Pressure Treatment and Follow-Up
At the end of the home pressure titration, the telemedicine and control subjects sent the APAP device back to the sleep center by mail and in person, respectively, and the study physician downloaded the data and generated a report. In the telemedicine group, the sleep doctor made a video or telephone communication through the telemedicine APP, interpreted the pressure titration report in detail, informed the patients to purchase the APAP device at their own expense, and conducted a 6-month follow-up. In the control group, a sleep doctor interpreted the report face-to-face at a sleep center and informed them about the course of treatment.
Patients willing to receive APAP were followed up for six months after purchase. The patients were followed up by experienced sleep doctors in the first week and after 1, 3, and 6 months of treatment. Follow-up included patients’ APAP compliance data (duration of use, pressure, air leakage, residual AHI, etc.), subjective feelings, snoring, and other symptom improvements. The APAP compliance data of the telemedicine group were uploaded to the ResMed Airview and PHILIPS Encore Anywhere platforms. Physicians downloaded patient data on the platform and followed up with the patients via a remote APP video/phone. Follow-up questionnaires were completed at the corresponding follow-up time points. Participants in the control group visited the sleep center in person for face-to-face follow-ups with a sleep doctor. The time and cost of visits were recorded at each follow-up, and visits and follow-ups outside the nodes were considered additional interventions.
Time/Economic Cost and Its Transformation
We considered both direct and indirect costs in our cost-benefit analysis. Direct costs included the salaries of the study physicians and all costs associated with follow-up visits, including masks, humidifiers, and medications used by the patients, as well as additional costs for visits to other specialized doctors, nurses, and emergency services. Non-directly related expenses refer to travel expenses incurred by patients during the study period. Indirect costs are the opportunity costs of lost productivity and work due to follow-up, and we also considered the time lost due to hospital visits and video conferencing.
All time and financial costs incurred from the first visit till the end of follow-up in both groups were recorded through questioning and timing. Direct time spent related to OSA treatment included the first face-to-face visit with the sleep doctor (ask patient), the sleep doctor setting HSAT information for a patient and initializing the HSAT (record), informing the patient on how to use HSAT face-to-face/informing patient on how to watch the HSAT wearing and using video on the remote APP (record), downloading data and interpreting the HSAT (record), and arranging patient’s visit with the sleep doctor. Other aspects comprised outpatient face-to-face/video phone assessment after HSAT treatment (record), outpatient face-to-face/video phone interpretation of the HSAT report (record), preparation and setting of the APAP device (record), and face-to-face instruction of patients on how to use APAP/telling patients how to watch APAP wearing and using video on remote APP and matters needing attention (record). Outpatient face-to-face/remote follow-up (records), and outpatient/remote follow-up (records) at 1 week, 1 month, 3 months, and 6 months after the ventilator data were downloaded from the program platform and home pressure titration was performed also comprised the direct time related to OSA treatment. Non-directly related expenses included transportation and accommodation costs for the first visit (inquiry), leave time for the first visit (inquiry), transportation and accommodation costs for returning HSAT (inquiry), leave time for returning HSAT (inquiry), transportation and accommodation costs for the outpatient service after HSAT (inquiry), and outpatient service leave time after HSAT (inquiry). Other non-directly related expenses were transportation and accommodation costs for receiving APAP equipment (inquiry), leave time for receiving APAP equipment (inquiry), transportation and accommodation expenses for the first week and 1, 3, and 6-month follow-up (inquiry), and leave time for the first week and 1, 3, and 6-month follow-up (inquiry).
All the time spent was converted into economic cost, and the specific conversion standard was the time spent by sleep doctors on diagnosis and treatment calculated according to a monthly salary of 10,000 yuan and a working period of 21.75 days. The patient’s leave time due to medical treatment was calculated according to a monthly salary of 10,000 yuan and a working period of 21.75 days.
Statistical Analysis
The planned sample size was based on the assumption that 85% of the patients randomly assigned to the treatment group met the per-protocol sample definition for the non-inferiority test described above. This study was based on the assumption that the mean adherence without intervention was 4 hours/day (SD=1.8). Based on a unilateral type I error of 0.025 and 80% efficacy, APAP compliance in the telemedicine group was verified to be no less than 1 h/day (SD=2), with an assumed dropout rate of 10% and a sample size of 60 cases per group.
The statistical software used was SPSS version 26.0. We conducted a descriptive statistical analysis of all observations. Continuous variables with a normal distribution are represented as mean ± standard deviation, and the utilization rate and percentage of subtype variables are presented. Longitudinal data were analyzed using a mixed-effect model, linear correlation analysis, and single-factor repeated measurement analysis of variance. A paired t-test was used before and after the same measurement, and non-parametric tests were used to compare rates and percentages. Statistical significance was set at p < 0.05.
Results
A total of 326 subjects were screened. Fifty-seven subjects met the inclusion criteria and signed informed consent, including 47 males (82.5%). The mean age of the patients was 40.12±11.73 years. By random grouping, 26 and 31 patients were assigned to the telemedicine and control groups, respectively. There was no significant difference in the completion of each stage between the two groups. The basic information is shown in Table 1. There were no significant differences between the telemedicine and control groups in terms of age, sex, education level, working status, per capita monthly family income, smoking, or alcohol consumption ratios. There was no significant difference in the proportion of patients with hypertension between the two groups. However, the body mass index (BMI) of the telemedicine group was higher than that of the control group (28.69±4.64 vs 26.29±3.85 kg/m2, p=0.037), and the proportion of patients with diabetes was higher than that of the control group (15.4% vs 0, p=0.024).
 |
Table 1 Baseline Characteristics |
APAP Treatment Acceptance Rate
Overall, 15 (57.7%) and 19 (61.3%) patients in the telemedicine and control groups, respectively, received home pressure titration. There was no difference in the rate of home pressure titration between the two groups (p=0.783). After home pressure titration, 15 (57.7%) and 17 (54.8%) subjects in the telemedicine and control groups, respectively, were willing to purchase the APAP device by themselves. There was no difference in the acceptance rate of APAP treatment between the two groups (p=0.829) (Table 2).
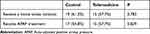 |
Table 2 Acceptance Rate of APAP Treatment and Home Stress Titration |
Improvement in Symptoms and Sleep Scale Scores After Treatment
As shown in Table 3 and Table 4, there was no statistically significant difference in symptom improvement and scale scores between the two groups before and six months after treatment, except for the difference in the degree of improvement of daytime sleepiness symptoms. After APAP treatment, there was no significant difference between the two groups in the improvement of the Pittsburgh Sleep Quality Index (PSQI), Insomnia Severity Index (ISI), Epworth Sleepiness Scale (ESS), Fatigue Severity Scale (FSS), short Sleep Apnea Quality of Life Index (SAQLI), and other scales. However, the scores on the sleep-related scales improved in the two groups. The proportion of improved daytime sleepiness symptoms was significantly higher in the telemedicine group than in the control group, although daytime sleepiness symptoms improved in both groups. There was no significant difference between the two groups in the improvement of OSA-related symptoms, such as snoring, frequent nighttime awakenings, observed apnea, nocturia, dry mouth in the morning, and sleep disturbance. However, symptoms improved after APAP treatment in both groups.
 |
Table 3 Comparison of Change from Baseline in Questionnaire Scores Between the Telemedicine and Control Groups |
 |
Table 4 Comparison of Typical OSA Symptoms Between the Telemedicine and Control Groups |
Adherence to APAP Treatment
In the first week, first month, and third month of follow-up, the mean time of APAP use in the telemedicine vs control groups was 5.99±1.34 vs 6.42±0.97, 5.74±1.35 vs 6.31±1.00, and 5.60±1.29 vs 5.93±1.27 hours, respectively. There was no difference in the mean time of APAP use between the two groups in the first week (p=0.306), first month (p=0.178), and third month (p=0.486). There was also no significant difference between the two groups in the number of days of average APAP use of ≥4 hours in the first week (p=0.118), first month (p=0.316), and third month (p=0.359). The parameters of APAP use and compliance data (duration, pressure, air leakage, AHI participation, etc.) in the first week, first month, and third month were compared between the two groups, and there were no significant differences.
A total of 31 patients completed the 6-month follow-up; 15 patients in the telemedicine group completed the remote APP video follow-up, and 16 patients in the control group completed the face-to-face outpatient follow-up. The average duration of APAP use in the two groups was 5.34±1.30 and 5.92±1.30 hours, respectively, and there was no difference between the two groups (p=0.228). There was also no difference between the two groups in the number of days of average APAP use of ≥4 hours (p=0.235). The parameters of APAP use and compliance data (duration, pressure, air leakage, AHI participation, etc.) were compared between the two groups in the sixth month, and there were no significant differences (Table 5).
 |
Table 5 Follow-Up of APAP Treatment |
Linear regression analysis showed that different treatment modalities did not affect APAP treatment compliance, nor did baseline sex, age, BMI, AHI, PSQI, ISI, FSS, or short SAQLI scale score. However, the baseline ESS score affected compliance with APAP treatment. For every 1-point increase in the ESS score, APAP treatment compliance increased by 4.46% (Table 6).
 |
Table 6 Factors Influencing Adherence to APAP Therapy |
Cost-Benefit Analysis
Table 7 summarizes the time and financial costs for both groups at different stages of the diagnostic treatment and follow-up processes. Subjects in the two groups were randomized after the first interview, so the two groups were consistent in registration fees, scale evaluation fees, HSAT, and pressure titration costs. The telemedicine group had significantly less transportation, room and board costs, leave time, loss of work caused by leave, time spent by doctors, and hours spent by doctors than the control group.
 |
Table 7 Cost Analysis |
The European five-dimensional health scale (EQ-5D), a measure of health-related quality of life, has been widely used worldwide. In this study, the index scores of the first five dimensions of EQ-5D were used to calculate quality-adjusted life years (QALYs).12 Since there is no EQ-5D conversion scale in China, the point conversion scale of Japan, which is also an East Asian country closest to Chinese ethnic characteristics and preference for health, was used for conversion. The cost-benefit comparison between the two groups is shown in Table 8. The total and OSA-related costs of the telemedicine and the control groups were 2100.25 and 2558.09 yuan and 1781.42 and 1841.85 yuan, respectively. The difference in QALYs between the two groups was small (telemedicine vs control: 0.0872 vs 0.0893), but the QALYs of the telemedicine group were slightly lower than those of the control group. The difference in QALYs between the two groups and the 95% confidence intervals (−0.0024, 0.0025) were obtained using the same random sampling method. Total and OSA-related costs were lower in the telemedicine group than in the control group, and the average efficacy index (QALYs) was lower in the telemedicine group. However, the difference in overall QALYs was smaller, indicating that the telemedicine group was more cost-effective.
 |
Table 8 Cost-Effectiveness Analysis |
Additional Intervention Times
In the process of diagnosis, treatment, and follow-up in this study, the telemedicine group had more additional intervention times outside the diagnosis and follow-up nodes than the control group (p=0.03), and the extra intervention time was longer than that in the control group (p=0.048) (Table 9).
 |
Table 9 Additional Interventions of Two Groups |
Characteristics of OSA Patients Receiving Telemedicine
The telemedicine group was divided into the treated and untreated groups according to whether they received APAP treatment (Table 10). The age of the treated group was higher than that of the untreated group (p=0.021), the proportion of males was higher in the treated group (p=0.032), the proportion of those living in the province outside the city was higher in the treated group (p=0.031), the education level of the subjects was higher in the treated group (p=0.035), and the proportion of fatty liver was lower in the treated group (p=0.014). The PSQI score of the treated group was higher than that of the untreated group (p=0.047), and the ISI score was higher in the treated group (p=0.021). In terms of sleep monitoring, the AHI of the treated group was higher than that of the untreated group (p=0.006), the mean and minimum oxygen saturation levels were lower in the treated group (p=0.028, p=0.049), and the time of oxygen saturation < 90% was higher in the treated group (p=0.019). Male subjects of older age, higher education level, farther living distance, no fatty liver, higher PSQI and ISI scores, higher AHI, and lower oxygen saturation were more likely to accept telemedicine diagnosis and treatment.
 |
Table 10 Characteristics of Subjects Receiving APAP Treatment in the Telemedicine Group |
Discussion
The demand for OSA treatment has increased with its rising incidence, and the consequences of its social and multiorgan damage have increased the economic burden on society.13,14 It has been reported that the cost of OSA diagnosis and treatment can reach up to US $12.4 billion.13 Traditional diagnosis and treatment models find it difficult to meet the huge needs regarding the diagnosis, treatment, and chronic disease management of OSA. Therefore, remote management has emerged. Although professional societies such as the American Medical Association of Sleep Medicine have issued guidelines for the standardized diagnosis, treatment, and management of adult OSA, emphasizing the importance of early diagnosis, standardized treatment, and long-term management of OSA,13 the practice of remote management is still limited and has not been widely promoted, especially in Asian countries. Some studies have evaluated CPAP compliance with remote management,15 and the compliance and effectiveness of patients with OSA with CPAP under telemedicine guidance and monitoring are not inferior to traditional outpatient medical treatment. However, it is unclear if telemedicine is accepted by patients, which is an important factor hindering the practice of telemedicine in China. Further evidence is needed for the clinical evaluation of the remote management model to guide practice.
Our results showed that the APAP treatment acceptance rate of the telemedicine group was not inferior to that of the control group, indicating that telemedicine is effective and feasible for OSA diagnosis and treatment. Verbraecken points out that telemedicine may be cost-effective, but better evidence is needed. Although barriers to implementation remain, telemedicine is feasible, but its use is at the discretion of doctors and patients.16 Most foreign studies have evaluated CPAP compliance, but in China, CPAP treatment is not supported by medical insurance, and patients pay for it themselves. Our study showed that telemedicine did not affect the rate of APAP treatment for patients with OSA and was not inferior to traditional medical treatment in terms of patient self-payment, demonstrating its meaningfulness and feasibility in clinical practice.
Our study found that the telemedicine and control groups had similar APAP use adherence. The analysis of factors influencing compliance found that the ESS score was correlated with APAP compliance, with treatment compliance increasing with an increase in ESS score. Bruyneel et al15 found that CPAP adherence was related to AHI and ESS scores. This is consistent with our findings. However, existing studies have failed to reach a consensus regarding whether telemedicine can improve treatment compliance in patients with OSA. Recently, Murphie et al17 systematically reviewed the role of telemonitoring-related teleconsultation in the follow-up of patients with OSA. The results of studies on CPAP compliance were mixed. Two studies showed that the compliance regarding CPAP was similar in the remote and traditional monitoring groups,18,19 which was also consistent with the results of our study. Three other smaller studies reported slight improvements in CPAP adherence with remote monitoring.20–22 Sparrow et al23 randomly assigned 250 patients who started CPAP therapy to the telephone follow-up and routine outpatient groups for 12 months of treatment. Although the remote follow-up group showed a small degree of improvement in compliance, the overall compliance was generally low. However, in an RCT involving 60 subjects, Chumpangern et al24 provided remote telephone intervention guidance to subjects with poor CPAP use for two consecutive nights. The results showed that the average time of CPAP use per night in the remote intervention subjects significantly increased, and treatment compliance significantly improved. Overall, most studies differ on the effects of telemedicine on CPAP compliance, possibly owing to differences in study sample sizes and design methods.
Despite the decline in the cost of information and communication technologies, cost-effectiveness issues associated with telemedicine remain critical. Our study showed that the telemedicine group was more cost-effective. Two recent research teams evaluated the cost-effectiveness of the remote follow-up of patients treated with CPAP. In the first study, 139 CPAP patients were randomly assigned to tele-follow-up (telemonitoring and teleconsultation) or usual care for six months of therapeutic follow-up. The results showed that remote follow-up was more cost-effective, with lower cost despite more visits, and no significant difference in compliance.15 In the second study,6 100 CPAP patients were randomly assigned to receive remote monitoring or regular care for three months, and researchers found that remote monitoring was more cost-effective. Both studies support the cost-effectiveness of telemedicine for CPAP patients, and the same conclusions were confirmed in our study. However, the research subjects of our study were all from the same province. This telemedicine model may be even more cost-effective if applied to remote areas or people with busy or fixed working hours. The cost reduction brought about by the telemedicine model is not only reflected in transportation, accommodation, and leave time. It is also greatly reduced by transforming the diagnosis method from expensive polysomnography to portable home sleep monitoring devices. The follow-up in the treatment process has changed from the original outpatient registration face-to-face follow-up to remote APP video follow-up. This reduces the cost of medical treatment for patients in all stages. However, our study found that additional intervention times were needed in the telemedicine group, while the visits and follow-up nodes were fixed for the traditional group. Due to the convenience of the network, patients would take the initiative to seek doctors’ help without limit, which increased doctors’ additional consultation time for telemedicine subjects. These extra interventions and follow-ups were not included in the clinical treatment. If this part is free, it increases the work burden of doctors outside the hospital, and the current medical service does not meet such needs.
Currently, optimizing OSA treatment strategies requires assigning patients to specific phenotypes and proposing personalized treatment strategies for these subtypes.25,26 Remote monitoring of CPAP and telemedicine may provide innovative and practical solutions to identify patients with OSA at the highest risk for non-adherence in the future, thereby allocating physician resources to those most in need. A multicenter RCT of 206 patients with symptomatic OSA but without serious comorbidities and at low cardiovascular risk found that telemonitoring did not achieve better ventilator compliance than conventional monitoring and that the follow-up workload of physicians and home care providers was significantly increased in the telemonitoring group. The above mentioned study suggests that remote monitoring has less of an impact on symptomatic people with low cardiovascular risk. Our results showed that male subjects of older age, higher education level, farther distance, no fatty liver, poor sleep quality, a higher degree of insomnia, and heavier OSA were more likely to receive remote diagnosis and treatment, which also provides a reference for the accurate selection of the OSA population in future clinical applications of telemedicine.
This study has some limitations. Firstly, the sample size of the patients included in this study was small because of the coronavirus pandemic, and the expected sample size was not obtained. Secondly, the study was only verified in a single center, leading to the possibility that some results could not be verified in different centers. In addition, the source of outpatients was limited, the subjects were randomized in Guangdong Province, and their working and family locations were limited. Therefore, the applicability of the research results in remote areas or non-first-tier cities needs to be further studied.
Conclusion
Our study found that APAP treatment acceptance rates in telemedicine were similar to those in traditional treatment, and there was no difference in treatment compliance. Telemedicine is more cost-effective but adds extra intervention time and time for doctors, which limits the application of telemedicine in clinical practice.
Abbreviations
AHI, Apnea-hypopnea index; APAP, Auto-adjusted positive airway pressure; BMI, Body mass index; CPAP, Continuous positive airway pressure; EQ-5D, European Five-Dimensional Health Scale; ESS, Epworth Sleepiness Scale; FSS, Fatigue Severity Scale; HSAT, Home Sleep Apnea Test; ICSD-3, International Classification of Sleep Disorders, third edition; ISI, Insomnia Severity Index; OSA, Obstructive sleep apnea; PAP, Positive airway pressure; PSQI, Pittsburgh Sleep Quality Index; QALYs, Quality-adjusted life years; SAQLI, Sleep Apnea Quality of Life Index.
Data Sharing Statement
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The experimental procedures were approved by the Ethics Review Committee of Guangdong Provincial People’s Hospital (KY-Q-2021-162-02). All participants provided written informed consent.
Acknowledgments
We thank the Sleep Center, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences) for their assistance in this work.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work has been supported by the National Natural Science Foundation of China (82170098).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi:10.1093/aje/kws342
2. Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010;90(1):47–112. doi:10.1152/physrev.00043.2008
3. Tondo P, Fanfulla F, Sabato R, Scioscia G, Foschino Barbaro MP, Lacedonia D. Obstructive sleep apnoea-hypopnoea syndrome: state of the art. Minerva Med. 2023;114(1):74–89. doi:10.23736/S0026-4806.22.08190-3
4. Rotenberg B, George C, Sullivan K, Wong E. Wait times for sleep apnea care in Ontario: a multidisciplinary assessment. Can Respir J. 2010;17(4):170–174. doi:10.1155/2010/420275
5. Hwang D, Chang JW, Benjafield AV, et al. Effect of telemedicine education and telemonitoring on continuous positive airway pressure adherence. The tele-OSA randomized trial. Am J Respir Crit Care Med. 2018;197(1):117–126. doi:10.1164/rccm.201703-0582OC
6. Anttalainen U, Melkko S, Hakko S, Laitinen T, Saaresranta T. Telemonitoring of CPAP therapy may save nursing time. Sleep Breath. 2016;20(4):1209–1215. doi:10.1007/s11325-016-1337-9
7. Kuna ST, Shuttleworth D, Chi L, et al. Web-based access to positive airway pressure usage with or without an initial financial incentive improves treatment use in patients with obstructive sleep apnea. Sleep. 2015;38(8):1229–1236. doi:10.5665/sleep.4898
8. Turino C, de Batlle J, Woehrle H, et al. Management of continuous positive airway pressure treatment compliance using telemonitoring in obstructive sleep apnoea. Eur Respir J. 2017;49(2). doi:10.1183/13993003.01128-2016
9. Guralnick AS, Balachandran JS, Szutenbach S, et al. Educational video to improve CPAP use in patients with obstructive sleep apnoea at risk for poor adherence: a randomised controlled trial. Thorax. 2017;72(12):1132–1139. doi:10.1136/thoraxjnl-2017-210106
10. Munafo D, Hevener W, Crocker M, Willes L, Sridasome S, Muhsin M. A telehealth program for CPAP adherence reduces labor and yields similar adherence and efficacy when compared to standard of care. Sleep Breath. 2016;20(2):777–785. doi:10.1007/s11325-015-1298-4
11. Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. doi:10.5664/jcsm.6506
12. Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ. 2004;13(12):1203–1210. doi:10.1002/hec.901
13. Epstein LJ, Kristo D, Strollo PJ, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–276. doi:10.5664/jcsm.27497
14. Tondo P, Fanfulla F, Scioscia G, et al. The Burden of Respiratory Alterations during Sleep on Comorbidities in Obstructive Sleep Apnoea (OSA). Brain Sci. 2022;12(10):1359. doi:10.3390/brainsci12101359
15. Isetta V, Negrín MA, Monasterio C, et al. A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax. 2015;70(11):1054–1061. doi:10.1136/thoraxjnl-2015-207032
16. Verbraecken J. Telemedicine in Sleep-Disordered Breathing: expanding the Horizons. Sleep Med Clin. 2021;16(3):417–445. doi:10.1016/j.jsmc.2021.05.009
17. Murphie P, Little S, McKinstry B, Pinnock H. Remote consulting with telemonitoring of continuous positive airway pressure usage data for the routine review of people with obstructive sleep apnoea hypopnoea syndrome: a systematic review. J Telemed Telecare. 2019;25(1):17–25. doi:10.1177/1357633X17735618
18. Coma-Del-Corral MJ, Alonso-álvarez ML, Allende M, et al. Reliability of telemedicine in the diagnosis and treatment of sleep apnea syndrome. Telemed J E Health. 2013;19(1):7–12. doi:10.1089/tmj.2012.0007
19. Taylor Y, Eliasson A, Andrada T, Kristo D, Howard R. The role of telemedicine in CPAP compliance for patients with obstructive sleep apnea syndrome. Sleep Breath. 2006;10(3):132–138. doi:10.1007/s11325-006-0059-9
20. Fox N, Hirsch-Allen AJ, Goodfellow E, et al. The impact of a telemedicine monitoring system on positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. Sleep. 2012;35(4):477–481. doi:10.5665/sleep.1728
21. Stepnowsky CJ, Palau JJ, Marler MR, Gifford AL. Pilot randomized trial of the effect of wireless telemonitoring on compliance and treatment efficacy in obstructive sleep apnea. J Med Internet Res. 2007;9(2):e14. doi:10.2196/jmir.9.2.e14
22. Smith CE, Dauz ER, Clements F, et al. Telehealth services to improve nonadherence: a placebo-controlled study. Telemed J E Health. 2006;12(3):289–296. doi:10.1089/tmj.2006.12.289
23. Sparrow D, Aloia M, Demolles DA, Gottlieb DJ. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax. 2010;65(12):1061–1066. doi:10.1136/thx.2009.133215
24. Chumpangern W, Muntham D, Chirakalwasan N. Efficacy of a telemonitoring system in continuous positive airway pressure therapy in Asian obstructive sleep apnea. J Clin Sleep Med. 2021;17(1):23–29. doi:10.5664/jcsm.8772
25. Martinez-Garcia MA, Campos-Rodriguez F, Barbé F, Gozal D, Agustí A. Precision medicine in obstructive sleep apnoea. Lancet Respir Med. 2019;7(5):456–464. doi:10.1016/S2213-2600(19)30044-X
26. Bonsignore MR, Suarez Giron MC, Marrone O, Castrogiovanni A, Montserrat JM. Personalised medicine in sleep respiratory disorders: focus on obstructive sleep apnoea diagnosis and treatment. Eur Respir Rev. 2017;26(146):170069. doi:10.1183/16000617.0069-2017
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
