Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Anxiety and Depression Among US Nursing Home Residents with Chronic Obstructive Pulmonary Disease
Authors Osundolire S , Goldberg RJ , Lapane KL
Received 13 May 2023
Accepted for publication 11 August 2023
Published 28 August 2023 Volume 2023:18 Pages 1867—1882
DOI https://doi.org/10.2147/COPD.S417449
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jill Ohar
Seun Osundolire, Robert J Goldberg, Kate L Lapane
Department of Population and Quantitative Health Sciences, University of Massachusetts Chan Medical School, Worcester, MA, 01605, USA
Correspondence: Kate L Lapane, Department of Population and Quantitative Health Sciences, University of Massachusetts Chan Medical School, Worcester, MA, 01605, USA, Tel +1 508-688-7618, Email [email protected]
Background: Chronic obstructive pulmonary disease (COPD) is highly prevalent among nursing home residents; however, few studies have focused on the psychological impact of this clinically significant condition on nursing home residents.
Objective: We examine the prevalence of, and factors associated with, anxiety and depression in nursing home residents with COPD.
Methods: Using the US 2018 Minimum Dataset (MDS), we conducted a cross-sectional study among 239,615 residents aged ≥ 50 years old in US Medicare/Medicaid certified nursing homes with COPD. Anxiety and depression were diagnosed based on clinical diagnoses, physical examination findings, and treatment orders. Multivariable adjusted Poisson models with a generalized estimating equations approach account for the clustering among residents within nursing homes.
Results: The average age of the study population was 79 years (SD: 10.6), 62.0% were women, and 43.7% had five or more comorbid conditions. In this population, 37.2% had anxiety, 57.6% had depression, and 27.5% had both mental health conditions. Women, current tobacco users, persons 50– 64 years old, those who reported having moderate or severe pain, and nursing home residents with multimorbidity were more likely to have anxiety or depression than respective comparison groups.
Conclusion: Anxiety and depression are common among US nursing home residents with COPD. Women, medically complex patients, and those who report having moderate-to-severe pain appear to be more likely to have anxiety and depression. Clinical teams should be aware of these findings when managing nursing home residents with COPD and use various nonpharmacological and medical interventions for the effective management of anxiety and depression. Longitudinal studies evaluating how anxiety and depression affect the management of COPD and related outcomes, and how best to improve the quality of life of nursing home residents with COPD, are warranted.
Keywords: chronic obstructive pulmonary disease, anxiety, depression, aging, nursing homes
Introduction
Chronic obstructive pulmonary disease encompasses multiple pulmonary conditions, which limit airflow to the lungs and cannot be fully reversed.1 Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide2 and is the fourth leading cause of death in Americans.3 An estimated 6.2% of adults in the United States currently have COPD.4 Estimates of the magnitude of COPD, and trends over time therein, vary by country1 and increases in the prevalence of, and mortality associated with, COPD are expected in the future due to the aging of various populations and epidemiological transitions ongoing in many countries throughout the world.5,6
Despite the importance of COPD as a leading cause of death and the adverse impact of this chronic condition on an individual’s physical functioning and quality of life, which disproportionately affects older adults, little is known about the epidemiology of COPD for those living in nursing homes. In the United States, there are ~15,000 nursing homes currently providing care for 1.5 million adults. Among American men and women who reach age 65 years old, 40% will enter a nursing home at least once during their lifetime.7 In the nursing home setting, between one in every 10 and one in every five residents have COPD.8,9
Although Guidelines from the National Institutes of Health and Care Excellence,10 and the Global Initiative for Chronic Obstructive Lung Disease,11 emphasize the importance of effective screening and management of anxiety and depression for persons with COPD, relatively little is known about the psychological impact of this pulmonary condition. Based on the characteristics of nursing home residents with COPD, there is most likely an accompanying depression or anxiety. The objectives of this large cross-sectional study were to estimate the prevalence of depression and anxiety among middle-aged and older long-term stay nursing home residents with COPD and evaluate sociodemographic and clinical factors associated with depression and anxiety in this population.
Methods
Data Source and Study Design
This is a retrospective cross-sectional study that uses information from the 2018 Minimum Dataset, version 3.0 (MDS), which contains detailed information about all nursing home residents in Medicare and Medicaid certified facilities in the United States. MDS is a mandated process for the clinical assessment of all nursing home residents, which was developed in response to the landmark Institute of Medicine Report on Nursing Home Quality.12 Nursing home staff conduct MDS assessments on residents at the time of admission, discharge, and other pre-specified time intervals including quarterly, semi-annually, annually, or when there is a significant change in the resident’s health status.13 The MDS assessment includes residents' demographic information, clinical conditions, symptoms (eg, pain and shortness of breath), as well as measures of cognitive and physical functioning (eg, activities of daily living and cognitive impairment).13 For Medicare beneficiaries, claims for hospitalizations were also used to identify nursing home residents with COPD. The University of Massachusetts Chan Medical School Institutional Review Board approved this observational study.
Study Sample
The study sample consisted of all long-term stay nursing home residents (90+ days) 50 years and older in Medicare and Medicaid certified United States nursing homes in 2018 who satisfied the following inclusion criteria: (1) had at least one quarterly or annual MDS assessment in 2018 and (2) had a diagnosis of COPD identified on the MDS or on Medicare hospital claims using ICD-10 codes (J41, J43, and J44). Nursing home staff used information retrieved from transfer notes, physical examination findings, medication and treatment orders, and hospital discharge documentation to identify persons with COPD. We excluded those who were in a comatose state and persons with missing data on key study variables. The final study sample consisted of 239,615 nursing home residents (Supplemental Figure 1).
Primary Outcome Variable (Anxiety and Depression)
We examined two mental health conditions, namely anxiety and depression, as our principal study outcomes. Nursing home staff used patient’s transfer notes at admission, and through tests, symptoms, and medications and other treatment orders documented in the resident’s progress notes to determine whether the resident had been diagnosed with anxiety and/or depression. The MDS codes I5700 and I5800 were used to define anxiety and depression diagnoses, respectively. Although not considered as a primary outcome variable, we also included descriptive information on depressive symptoms included in the Patient Health Questionnaire-9 (PHQ-9). In the MDS, two versions of the PHQ-9 exist, each having a 14-day look back period.14 The standard PHQ-9 was used in residents capable of being interviewed for their depressive symptoms (range: 0–27). If residents were unable to self-report, the PHQ-9 OV (based on staff observation) was used (range 0–30).15 The PHQ-9 OV has an additional question regarding whether the resident was “short tempered, easily annoyed.” We categorized residents as having either minimal depression (PHQ-9 or PHQ-9-OV scores between 0 and 4), mild depression (PHQ-9 or PHQ-9-OV scores between 5 and 9), moderate depression (PHQ-9 or PHQ-9-OV scores between 10 and 14), or severe depression (PHQ-9 or PHQ-9-OV score ≥15).
Covariates
The covariates considered were sociodemographic, clinical characteristics, and comorbid conditions thought to be associated with anxiety and depression in persons with COPD. Age was categorized as 50–64 years, 65–74, 75–84, and ≥85 years. Race/ethnicity was collapsed into four categories: non-Hispanic White, non-Hispanic Black, Hispanic, and others (eg, American Indian/Native Alaskan/Native Hawaiian/Asian and Other Pacific Islander), because of the small number of nursing home residents in these latter groups13. Pain intensity and dyspnea (during a 7-day look back period) were based on self-reports of these symptoms on either exertion, sitting at rest, or when lying flat. Current tobacco use and use of oxygen (during a 14-day look back period) were included, while the level of social connectedness was measured using the social connectedness index (high connectedness: Yes/No).16
Physical functioning was measured using the Activities of Daily Living (ADL) Self-Performance Hierarchy Scale categorized as either independent/supervision in one ADL, moderate, or dependent.17 We evaluated residents' level of cognitive impairment using the Cognitive Function Scale,18 which combines the Brief Interview for Mental Status (BIMS) and Cognitive Performance Scale (CPS).19 Residents were classified as either cognitively intact (if they were able to complete the BIMS and score between 13 and 15) or having mild (BIMS score of 8–12 or a CPS score of 0–2), moderate (BIMS score of 0–7 or a CPS score of 3 or 4), or severe cognitive impairment (when residents cannot complete BIMS and have a CPS score of 5 or 6).18
The comorbid conditions examined included neurological conditions (eg, dementia and stroke), cardiovascular conditions (ie, hypertension, heart failure, peripheral vascular disease, atrial fibrillation, and coronary artery disease), nephropathy, gastroesophageal reflux, osteoporosis, arthritis, hyperlipidemia, anemia, obesity, cancer, cirrhosis, peripheral vascular disease, pneumonia, and diabetes mellitus. The modified Charlson Comorbidity Index (CCI) was used to classify the extent of chronic disease burden in the study population and categorized as 1–4, 5, 6–7, and ≥8.20 Body mass index (BMI) was categorized as ≤18.5 kg/m2, between ≥18.5 kg/m2 and ≤25 kg/m2, and >25 kg/m2. Additional facets of a nursing home resident’s condition included their history of falls and whether they had urinary or bowel incontinence.
Psychiatric Medication Use
We evaluated the use of antidepressants, anxiolytics, hypnotics, antipsychotics, and opioids with a 7-day look back period before the MDS assessment. Any medication or therapy received from any licensed mental health professional by residents (after admission into the nursing home) is documented in the medications section and special treatments, procedures, and program section of the MDS.14
Statistical Analysis
We first describe the prevalence of selected demographic, clinical characteristics, and comorbid conditions among residents with COPD. We then estimated the prevalence of each mental health outcome (ie, anxiety and depression) by each demographic, clinical characteristic, and comorbid condition. Finally, we construct crude and multivariable adjusted Poisson regression models with a generalized estimating equations approach to account for the clustering among residents within nursing homes. Crude and multivariable adjusted prevalence ratios (aPR) and corresponding 95% confidence intervals (CI) were derived from these models. Before conducting our regression models, we evaluated correlations and variance inflation factors for the covariates. To avoid multicollinearity, any variable whose variance inflation factor exceeded 2.5 was not included in the fully adjusted model. We removed the individual clinical conditions in favor of keeping the Charlson Comorbidity Index to avoid the potential for collinearity.
Results
Characteristics of the Study Population
The final study sample consisted of 239,615 long-stay residents 50 years and older who were diagnosed with COPD. The average age of the study population was 79 years (SD: 10.6). Approximately one-third of the study sample was 85 years and older, 62% were women, and four-fifths were non-Hispanic whites (Table 1). Overall, 55% had moderate dependence in activities of daily living, 42% were cognitively intact, 82% had a diagnosis of hypertension, 48% had dementia, 42% had diabetes mellitus, 35% had a BMI ≥ 30 kg/m2, and 26% had a Charlson Comorbidity Score ≥6. One-quarter reported having moderate pain, 23% had dyspnea, and 27% used oxygen (Table 1).
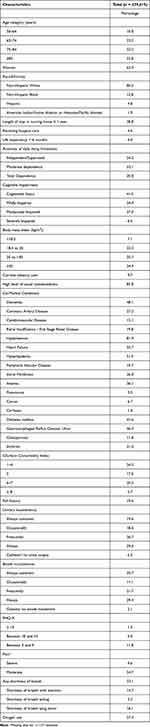 |
Table 1 Characteristics of Long Stay Residents with Chronic Obstructive Pulmonary Disease Living in US Nursing Homes in 2018 |
Prevalence of Anxiety According to Nursing Home Resident Characteristics
Among nursing home residents diagnosed with COPD, the prevalence of anxiety was 37.2% and 54.8% of residents with anxiety were treated with anxiolytics (Supplemental Table 2). The prevalence of anxiety decreased with advancing age and the prevalence of anxiety was higher among women than men (Table 2). Two in every five non-Hispanic white residents had anxiety, nearly one-quarter of non-Hispanic black residents had anxiety, three in every 10 Hispanic residents had anxiety, and one in every five American Indians/Native Alaskan or Native Hawaiian, or Other Pacific Islanders residents had anxiety. The frequency of anxiety was markedly elevated among those with independence in activities of daily living, those who were cognitively intact, and among persons with a BMI ≥30 kg/m2. Residents with pneumonia, gastroesophageal reflux disease, osteoporosis, arthritis, and a history of falls had the highest prevalence of anxiety among nursing home residents with COPD (Supplemental Table 1). The prevalence of anxiety ranged from 36.0% in those with a Charlson Comorbidity Index of 1–4 to 42.3% in those with a Charlson Comorbidity Index ≥8. The proportion of residents with anxiety increased with higher PHQ-9 scores, as well as with increased pain severity; 74.1% of nursing home residents with COPD and anxiety also had accompanying depression.
Prevalence of Depression According to Nursing Home Resident Characteristics
The prevalence of depression in this study population was 57.6%. Based on the PHQ-9 assessment, 11.8% had mild depression and 6.3% had severe depression. Suicidal ideation was most frequently self-reported or staff observed depressive symptom, followed by worthlessness and psychomotor retardation (Figures 1 and 2). The frequency of individual depressive symptoms was low in those who self-reported the PHQ-9 (Figure 1) or among those with staff-observed symptoms (Figure 2); most residents (86.8%) with depression were treated with antidepressants (Supplemental Table 2).
 |
Figure 1 Frequency of self-reported depressive symptoms. |
 |
Figure 2 Frequency of staff observed depressive symptoms. |
There was a decrease in the prevalence of depression with advancing age (Table 3). Three in five women had depression, while slightly more than one-half of men had depression. While 60.6% of non-Hispanic white residents had depression documented, 44.1% of non-Hispanic black residents, 36.7% of American Indians/Native Alaskan or Native Hawaiian, or Other Pacific Islanders residents, and 51.3% of Hispanic had depression. The prevalence of depression was highest among those with dementia, coronary artery disease, hypertension, heart failure, cerebrovascular disease, peripheral vascular disease, hyperlipidemia, diabetes mellitus, gastroesophageal reflux disease, osteoporosis, arthritis, cirrhosis, and anemia (Supplemental Table 1). There was an increased prevalence of depression among those who were current tobacco users, in those who had a BMI ≥30 kg/m2, no or a low level of social connectedness, a Charlson Comorbidity Index ≥8, greater pain severity, dyspnea, and among those who required oxygen (Table 3). Among nursing home residents with COPD and depression, 47.8% also had anxiety.
Factors Associated with Anxiety in Nursing Home Residents with COPD
Anxiety was more commonly diagnosed among residents aged 50–64 years old and women, whereas racial/ethnic minorities were less likely to be diagnosed with anxiety compared with non-Hispanic whites after adjusting for several sociodemographic and clinical characteristics and comorbidities (Table 2). Compared to residents who were independent in activities of daily living, those who had moderate or total dependence in performing activities of daily living were less likely to have anxiety, while, compared with cognitively intact nursing home residents, those with moderate or severe cognitive impairment were more likely to be diagnosed with anxiety. Anxiety was more common as the PHQ-9 score increased, among those with severe pain, and in persons with a higher Charlson Comorbidity Index. After adjusting for several sociodemographic, clinical characteristics, and comorbidities, nursing home residents with COPD and anxiety were 1.84 times (95% CI 1.81–1.86) more likely to have accompanying depression compared to those without COPD and anxiety (Table 2).
Factors Associated with Depression in Nursing Home Residents with COPD
After adjusting for various sociodemographic, clinical characteristics, and comorbidities, residents aged 50–64 years old were more likely to be diagnosed with depression compared with those aged 65–74 years, whereas those aged 75 years and older were less likely to have depression (Table 3). Women were more likely to be diagnosed with depression compared with men, while racial/ethnic minorities were, in general, less likely to be diagnosed with depression as compared with non-Hispanic white residents. Those with a high social connectedness index were less likely to be diagnosed with depression compared with residents with no or low social connectedness, while long-stay nursing home residents with a higher Charlson Comorbidity Index and those with moderate or total dependence on ADLs were more likely to be diagnosed with depression. Persons with greater cognitive impairment were less likely to be diagnosed with depression, while residents with higher pain severity were more likely to be diagnosed with depression compared to those without documented pain. After adjusting for several sociodemographic, clinical characteristics, and comorbidities, nursing home residents with COPD and depression were 1.44 times more likely (95% CI 1.43–1.45) to be diagnosed with anxiety than residents without COPD and depression (Table 3).
Discussion
In this national study of long-term stay nursing home residents with COPD, we found that more than one-third had anxiety and more than one-half of these individuals were being treated with anxiolytics. Depression was common (58%), most of these individuals’ received antidepressants, severe depression was uncommon, and the frequency of specific depressive symptoms was low. There was a higher prevalence of anxiety and depression among women than men and a lower prevalence among racial/ethnic minorities relative to non-Hispanic whites. Among nursing home residents with COPD, those with depression were more likely to also have accompanying anxiety than those without depression and residents with anxiety were more likely to have co-morbid depression in comparison to those who did not have a diagnosis of anxiety.
Prevalence of Anxiety Among Nursing Home Residents with COPD
Our observational study of long-stay nursing home residents with COPD showed a higher prevalence of anxiety in this nationally representative study population than previous research studies conducted in nursing homes. In prior studies, the frequency of anxiety among all nursing home residents has ranged widely, varying from none to upward of one-quarter of persons being diagnosed with anxiety.21–24 Results from a study of 126,121 residents living in US nursing homes in 2009 and 2010 showed that the overall prevalence of anxiety was 23%.9 Our study, which was conducted in a national sample of 239,616 residents living in US nursing homes in 2018, revealed a prevalence rate of 37% among nursing home residents diagnosed with COPD. In a review of 81 studies published between 1968 and 2004, the prevalence of anxiety was higher in those who had COPD than in the general population.25
We found a lower prevalence of anxiety with advancing age and a higher prevalence of anxiety among women than men. Several prior studies conducted in the United States and Europe have shown a similar pattern of higher prevalence rates of anxiety among women than men,26–30 and a lower prevalence of anxiety for older than younger adults living in nursing homes and the broader community.26,31 One explanation for the lower prevalence of anxiety in older than younger nursing home residents could be due to older residents having fewer obligations and typically being restricted in their daily living activities, such that older individuals avoid activities or situations that may predispose them to anxiety.32 In addition, the lower frequency of anxiety with advancing age and higher prevalence of anxiety that we observed in women with COPD is likely attributed to selective survival (ie, men die sooner than women with increasing age).
Nursing home residents with a higher PHQ-9 score, Charlson Comorbidity Index, cognitive impairment, and increased pain severity were more likely to report anxiety than their respective comparison groups. In a study of 994 adults 61 years and older living in long-term care facilities, anxiety was strongly associated with depression and with physical health, functional disability, and cognitive status.24 Our results showing increased pain severity among those with anxiety were similar to the results of a study of more than 270,000 newly admitted nursing home residents aged 65 years or older between 2011 and 2012, which showed that more than three-quarters of these individuals reported having moderate or severe pain intensity during the prior 5 days.33
Our findings suggest a strong association between anxiety among nursing home residents with COPD and associated comorbidities. We showed an increased prevalence of anxiety among those with increasing Charlson comorbidity index score, PHQ-9 score, cognitive impairment, and pain severity.
Prevalence of Depression Among Nursing Home Residents with COPD
In our study, the prevalence of depression among long-stay nursing home residents with COPD was 58%. This was higher than the prevalence of depression (50%) found among US nursing home residents with COPD between 2009 and 2010.9 In another study conducted in 783,826 residents in Medicare and Medicaid certified nursing homes in the US in 2011/2012, the prevalence of depression was 36% among newly admitted individuals.33 Similar to our observations with regard to anxiety, we found a higher prevalence of depression in women than men, and a decreased frequency of depression with advancing age. We observed that the prevalence of depression was highest among residents who had been previously diagnosed with a variety of chronic conditions including dementia, coronary artery disease, hypertension, cerebrovascular disease, peripheral vascular disease, diabetes mellitus, gastroesophageal reflux disease, arthritis, cirrhosis, and anemia.
Based on PHQ-9 and PHQ-9-OV assessments, our study results showed that symptoms such as suicidal ideation, worthlessness, and psychomotor retardation were relatively frequent among residents with COPD. Although few recent studies have examined the association between suicidal ideation and COPD, results from prior studies show a significant association between COPD and an increased likelihood of suicidal ideation.34–36 In a study using data from the National Comorbidity Study-Replication sample of persons 18 years and older in the US (n=9882), COPD was associated with significantly increased odds of suicidal ideation and suicide attempts, compared with those without COPD in both crude and multivariable adjusted analyses.35 These findings suggest that depression might be strongly linked to impaired quality of life among those with COPD due to a high prevalence of comorbidities and cognitive impairment.
Prevalence of Anxiety/Depression Among Nursing Home Residents with COPD
The prevalence of both anxiety and depression was high among residents with COPD as 27.5% of our study samples were diagnosed with these two mental health conditions. Women and current tobacco users, as well as those with an increased Charlson comorbidity index score and increased pain intensity, were more likely to be diagnosed with COPD and comorbid anxiety or depression than their respective comparison groups. Several prior studies reported a high prevalence of both anxiety and/or depression among those with COPD than those with other chronic diseases such as cancer, heart disease, renal disease, and the acquired immunodeficiency syndrome.37–40
In our study, it is noteworthy that nursing home residents with COPD who had moderate to total dependence on activities of daily living were less likely to have anxiety but were more likely to have depression. The increased prevalence of depression among older adults with COPD, because of their requirement for more daily care due to worsening physical health, may lower their self-esteem and self-efficacy, predisposing them to depression.40
Among the present long-term stay nursing home residents with COPD, greater cognitive impairment was associated with an increased prevalence of both anxiety and depression, except in residents with severe cognitive impairment, who were less likely to be diagnosed with depression. A case series of four patients with depressive pseudo dementia and two recent literature reviews on cognitive impairment in depression suggested that in those with severe cognitive impairment, depression may be a form of pseudo-dementia such that depression can impair cognition and give the appearance of a neurodegenerative disease such as dementia;41–43 these findings suggest that these individuals may be experiencing dementia rather than depression. This could explain, in part, why the prevalence of dementia was so relatively high among those with comorbid depression.
In this population of nursing home residents with COPD, the prevalence of depression was considerably higher than the prevalence of anxiety. A higher prevalence of depression than anxiety in our study population can be due to the considerably increasing prevalence of comorbidities and high prevalence of pain,33 as well as the insufficient recognition of depression and lack of adequate guideline-based treatment by physicians.44
Clinical Implications
Greater understanding of the epidemiology of the co-occurrence of COPD and anxiety or depression for adults living in nursing homes is a necessary first step to inform intervention development and improve disease management protocols. A systematic review and meta-analysis of approximately 29,000 individuals with COPD with a mean age of 63 years followed for 1 to 8 years, and six studies on COPD as a predictor of depression in nearly 7.5 million participants followed for 1 to 35 years, demonstrated that COPD increased the risk of developing anxiety or depression, and vice versa.45 Furthermore, patients with COPD and comorbid depression or anxiety had a markedly increased risk of dying during the periods under study, a finding consistent with prior literature that has shown that both conditions are associated with an increased risk of dying among persons with COPD.38,46 Less than one-third of persons followed in these studies with these comorbidities received the necessary interventions. This is because pharmacological management, including the use of antidepressants and anxiolytics, has questionable efficacy when used as the sole treatment option in those with COPD and comorbid anxiety or depression. Rather, it is more efficacious to combine treatment with nonpharmacological approaches such as pulmonary rehabilitation (eg, exercise-based), psychological therapy (cognitive-behavioral therapy), and a collaborative care model involving the core components of exercise training, education, and psychological support.47,48 Therefore, it is crucial for clinicians to utilize a multidisciplinary team approach to screen for these comorbidities, when a diagnosis of COPD is made, and develop effective treatment plans to improve patients' psychological and physical health outcomes.
Results of our study showed that a large proportion of nursing home residents with depression and anxiety were being treated with antidepressants and anxiolytics. A study in Ontario, Canada, among 28,360 persons with COPD aged 66 years and older who were being treated with antidepressants, and a similar number of older adults who were not being treated with these medications, found that antidepressant use was associated with a 15% increased risk of hospitalization and emergency room visits.49 Moreover, several studies have shown that those diagnosed with COPD exhibit lower rates of medication adherence in general than those without this pulmonary condition.50,51 Clinical teams should consider nonpharmacological interventions for COPD-related anxiety and depression. For example, pulmonary rehabilitation, education, and psychosocial support have been shown to significantly reduce anxiety and depression more than standard care in patients with COPD.52–55 The extent to which these strategies would be effective in nursing home residents with COPD warrants further study.
Study Strengths and Limitations
We used information collected from MDS, a large nationally representative database of nursing home residents used extensively for nursing home research. MDS consists of typically understudied, but vulnerable and medically complex, nursing home residents. We used the modified Charlson Comorbidity Index, a validated algorithm to determine the extent of disease burden in this population,20 and we used the PHQ-9 assessment or the PHQ-9 OV score based on staff observation to determine the severity of depression.15,56–58 Our cross-sectional study design allowed us to estimate the prevalence of important mental health outcomes, but we could not determine the bidirectionality of anxiety or depression with the sociodemographic and clinical factors under study. Our study did not differentiate between early-onset and the more commonly occurring late-onset depression, which is more frequently associated with selected comorbidities.59 We also lacked data on forced expiratory volume, which would have been helpful in determining the form and severity of COPD (using the Global Initiative for Chronic Obstructive Lung Disease (GOLD) grades) in our study population.
Conclusion
The prevalence of anxiety and depression is high among nursing home residents with COPD. Pharmacologic management of anxiety and depression was common. It is important for clinicians to closely monitor residents with COPD for anxiety and depression and engage a multidisciplinary team approach to manage these conditions. Further investigation is also needed for appropriate and effective screening, diagnosis, and management of anxiety and depression among nursing home residents with COPD since these conditions have been shown to lead to an increased risk of disease exacerbation and death.
Funding
Dr Osundolire was funded by a training grant from the National Institutes of Health grants to (T32HL120823). This research was supported in part by a research grant to Dr Lapane (R01AG071692).
Disclosure
Drs Osundolire, Goldberg, and Lapane have no conflicts to report for this work.
References
1. Celli BR, Wedzicha JA. Update on clinical aspects of chronic obstructive pulmonary disease. N Engl J Med. 2019;381(13):1257–1266.
2. World Health Organization. The top 10 causes of death; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
3. Xu J, Murphy SL, Kockanek KD, Arias E. Mortality in the United States, 2018. NCHS Data Brief. 2020;355:1–8.
4. Wheaton AG, Liu Y, Croft JB, et al. Chronic obstructive pulmonary disease and smoking status - United States, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(24):533–538. doi:10.15585/mmwr.mm6824a1
5. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi:10.1371/journal.pmed.0030442
6. Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet. 2017;389(10082):1931–1940. doi:10.1016/S0140-6736(17)31222-9
7. Spillman BC, Lubitz J. New estimates of lifetime nursing home use: have patterns of use changed? Med Care. 2002;40(10):965–975. doi:10.1097/00005650-200210000-00013
8. Pleasants R. Chronic obstructive pulmonary disease in long-term care. Ann Longterm Care. 2009;17:24–30.
9. Zarowitz BJ, O’Shea T. Chronic obstructive pulmonary disease: prevalence, characteristics, and pharmacologic treatment in nursing home residents with cognitive impairment. J Manag Care Pharm. 2012;18(8):598–606. doi:10.18553/jmcp.2012.18.8.598
10. Excellence NIoHaC. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. NG115; 2019. Available from: https://www.nice.org.uk/guidance/ng115.
11. Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(4):347–365. doi:10.1164/rccm.201204-0596PP
12. Care IoMUCoIQiL-T. Improving the Quality of Long-Term Care. Washington (DC): National Academies Press (US); 2001.
13. Centers for Medicare & Medicaid Services. Long-Term Care Facility Resident Assessment Instrument 3.0 User’s Manual. Department of Health & Human Services, ed; 2016.
14. Medicare Cf, Services M. Long-term care facility resident assessment instrument 3.0 user’s manual. Accessed May. 2015;9:2016.
15. Saliba D, DiFilippo S, Edelen MO, Kroenke K, Buchanan J, Streim J. Testing the PHQ-9 interview and observational versions (PHQ-9 OV) for MDS 3.0. J Am Med Dir Assoc. 2012;13(7):618–625. doi:10.1016/j.jamda.2012.06.003
16. Bova CA, Jesdale BM, Mbrah A, Botelho L, Lapane KL. Development and psychometric evaluation of the social connectedness index in nursing home residents with Alzheimer’s disease and dementia using the minimum data set 3.0. Int J Geriatr Psychiatry. 2021;36(7):1110–1119. doi:10.1002/gps.5516
17. Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol a Biol Sci Med Sci. 1999;54(11):M546–M553. doi:10.1093/gerona/54.11.M546
18. Thomas KS, Dosa D, Wysocki A, Mor V. The minimum data set 3.0 cognitive function scale. Med Care. 2017;55(9):e68–e72. doi:10.1097/MLR.0000000000000334
19. Chodosh J, Edelen MO, Buchanan JL, et al. Nursing home assessment of cognitive impairment: development and testing of a brief instrument of mental status. J Am Geriatr Soc. 2008;56(11):2069–2075. doi:10.1111/j.1532-5415.2008.01944.x
20. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
21. Cheok A, Snowdon J, Miller R, Vaughan R. The prevalence of anxiety disorders in nursing homes. Int J Geriatr Psychiatry. 1996;11:405–410. doi:10.1002/(SICI)1099-1166(199605)11:5<405::AID-GPS302>3.0.CO;2-O
22. Rovner BW, Kafonek S, Filipp L, Lucas MJ, Folstein MF. Prevalence of mental illness in a community nursing home. Am J Psychiatry. 1986;143(11):1446–1449.
23. Junginger J, Phelan E, Cherry K, Levy J. Prevalence of psychopathology in elderly persons in nursing homes and in the community. Psychiatr Serv. 1993;44(4):381–383. doi:10.1176/ps.44.4.381
24. Parmelee PA, Katz IR, Lawton MP. Anxiety and its association with depression among institutionalized elderly. Am J Geriatr Psychiatry. 1993;1(1):46–58. doi:10.1097/00019442-199300110-00007
25. Hynninen KM, Breitve MH, Wiborg AB, Pallesen S, Nordhus IH. Psychological characteristics of patients with chronic obstructive pulmonary disease: a review. J Psychosom Res. 2005;59(6):429–443. doi:10.1016/j.jpsychores.2005.04.007
26. Flint AJ. Epidemiology and comorbidity of anxiety disorders in the elderly. Am J Psychiatry. 1994;151(5):640–649.
27. Beekman AT, Bremmer MA, Deeg DJ, et al. Anxiety disorders in later life: a report from the Longitudinal Aging Study Amsterdam. Int J Geriatr Psychiatry. 1998;13(10):717–726. doi:10.1002/(SICI)1099-1166(1998100)13:10<717::AID-GPS857>3.0.CO;2-M
28. Forsell Y, Winblad B. Feelings of anxiety and associated variables in a very elderly population. Int J Geriatr Psychiatry. 1998;13(7):454–458. doi:10.1002/(SICI)1099-1166(199807)13:7<454::AID-GPS795>3.0.CO;2-D
29. Lenze EJ, Rogers JC, Martire LM, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9(2):113–135. doi:10.1097/00019442-200105000-00004
30. McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45(8):1027–1035. doi:10.1016/j.jpsychires.2011.03.006
31. Regier DA, Farmer ME, Rae DS, et al. One-month prevalence of mental disorders in the United States and sociodemographic characteristics: the Epidemiologic Catchment Area study. Acta Psychiatr Scand. 1993;88(1):35–47. doi:10.1111/j.1600-0447.1993.tb03411.x
32. De Bellis A. Opinion piece: Australian residential aged care and the quality of nursing care provision. Contemp Nurse. 2010;35(1):100–113. doi:10.5172/conu.2010.35.1.100
33. Ulbricht CM, Hunnicutt JN, Hume AL, Lapane KL. Depression, anxiety, and pain among newly admitted nursing home residents. J Nurs Home Res Sci. 2019;5:40–48. doi:10.14283/jnhrs.2019.8
34. Crump C, Sundquist K, Sundquist J, Winkleby MA. Sociodemographic, psychiatric and somatic risk factors for suicide: a Swedish national cohort study. Psychol Med. 2014;44(2):279–289. doi:10.1017/S0033291713000810
35. Goodwin RD. Is COPD associated with suicide behavior? J Psychiatr Res. 2011;45(9):1269–1271. doi:10.1016/j.jpsychires.2011.01.014
36. Webb RT, Kontopantelis E, Doran T, Qin P, Creed F, Kapur N. Suicide risk in primary care patients with major physical diseases: a case-control study. Arch Gen Psychiatry. 2012;69(3):256–264. doi:10.1001/archgenpsychiatry.2011.1561
37. Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58–69. doi:10.1016/j.jpainsymman.2005.06.007
38. Divo M, Cote C, de Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–161. doi:10.1164/rccm.201201-0034OC
39. Jose AK, Chelangara DP, Shaji K. Factors associated with anxiety and depression in chronic obstructive pulmonary disease. Int J Res Med Sci. 2016;4(4):1074–1079. doi:10.18203/2320-6012.ijrms20160786
40. Tsai T-Y, Livneh H, M-c L, Tsai P-Y, Chen P-C, Sung F-C. Increased risk and related factors of depression among patients with COPD: a population-based cohort study. BMC Public Health. 2013;13(1):976. doi:10.1186/1471-2458-13-976
41. Perini G, Cotta Ramusino M, Sinforiani E, Bernini S, Petrachi R, Costa A. Cognitive impairment in depression: recent advances and novel treatments. Neuropsychiatr Dis Treat. 2019;15:1249–1258. doi:10.2147/NDT.S199746
42. McAllister TW, Price TR. Severe depressive pseudodementia with and without dementia. Am J Psychiatry. 1982;139(5):626–629.
43. Brodaty H, Connors MH. Pseudodementia, pseudo-pseudodementia, and pseudodepression. Alzheimers Dement. 2020;12(1):e12027. doi:10.1002/dad2.12027
44. Kramer D, Allgaier A-K, Fejtkova S, Mergl R, Hegerl U. Depression in nursing homes: prevalence, recognition, and treatment. Int J Psychiatr Med. 2009;39(4):345–358. doi:10.2190/PM.39.4.a
45. Atlantis E, Fahey P, Cochrane B, Smith S. Bidirectional associations between clinically relevant depression or anxiety and COPD: a systematic review and meta-analysis. Chest. 2013;144(3):766–777. doi:10.1378/chest.12-1911
46. Laforest L, Roche N, Devouassoux G, et al. Frequency of comorbidities in chronic obstructive pulmonary disease, and impact on all-cause mortality: a population-based cohort study. Respir Med. 2016;117:33–39. doi:10.1016/j.rmed.2016.05.019
47. Yohannes AM, Alexopoulos GS. Depression and anxiety in patients with COPD. Eur Respir Rev. 2014;23(133):345–349. doi:10.1183/09059180.00007813
48. Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134(4 Suppl):43s–56s. doi:10.1378/chest.08-0342
49. Vozoris NT, Wang X, Austin PC, et al. Serotonergic antidepressant use and morbidity and mortality among older adults with COPD. Eur Respir J. 2018;52(1). doi:10.1183/13993003.00475-2018
50. George J, Kong DC, Thoman R, Stewart K. Factors associated with medication nonadherence in patients with COPD. Chest. 2005;128(5):3198–3204. doi:10.1378/chest.128.5.3198
51. Morrison D, Agur K, Mercer S, Eiras A, González-Montalvo JI, Gruffydd-Jones K. Managing multimorbidity in primary care in patients with chronic respiratory conditions. NPJ Prim Care Respir Med. 2016;26:16043. doi:10.1038/npjpcrm.2016.43
52. Coventry PA, Hind D. Comprehensive pulmonary rehabilitation for anxiety and depression in adults with chronic obstructive pulmonary disease: systematic review and meta-analysis. J Psychosom Res. 2007;63(5):551–565. doi:10.1016/j.jpsychores.2007.08.002
53. Gordon CS, Waller JW, Cook RM, Cavalera SL, Lim WT, Osadnik CR. Effect of pulmonary rehabilitation on symptoms of anxiety and depression in COPD: a systematic review and meta-analysis. Chest. 2019;156(1):80–91. doi:10.1016/j.chest.2019.04.009
54. Coventry PA, Gellatly JL. Improving outcomes for COPD patients with mild-to-moderate anxiety and depression: a systematic review of cognitive behavioural therapy. Br J Health Psychol. 2008;13(Pt 3):381–400. doi:10.1348/135910707X203723
55. Usmani ZA, Carson KV, Heslop K, Esterman AJ, De Soyza A, Smith BJ. Psychological therapies for the treatment of anxiety disorders in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017;3. doi:10.1002/14651858.CD010673.pub2
56. Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the patient health questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21(6):547–552. doi:10.1111/j.1525-1497.2006.00409.x
57. Merz EL, Malcarne VL, Roesch SC, Riley N, Sadler GR. A multigroup confirmatory factor analysis of the patient health questionnaire-9 among English- and Spanish-speaking latinas. Cultur Divers Ethnic Minor Psychol. 2011;17(3):309–316. doi:10.1037/a0023883
58. Bélanger E, Thomas KS, Jones RN, Epstein-Lubow G, Mor V. Measurement validity of the patient-health questionnaire-9 in US nursing home residents. Int J Geriatr Psychiatry. 2019;34(5):700–708. doi:10.1002/gps.5074
59. Potter GG, Steffens DC. Contribution of depression to cognitive impairment and dementia in older adults. Neurologist. 2007;13(3):105–117. doi:10.1097/01.nrl.0000252947.15389.a9
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.










