Back to Journals » Patient Preference and Adherence » Volume 17
Antibiotic Self-Medication Patterns and Associated Factors in the Context of COVID-19, Medellín, Colombia: A Survey Based Cross Sectional Study
Authors Arboleda Forero V , Cruzate Hernández JP , Yepes Restrepo M , Higuita-Gutiérrez LF
Received 5 August 2023
Accepted for publication 14 October 2023
Published 23 November 2023 Volume 2023:17 Pages 3057—3066
DOI https://doi.org/10.2147/PPA.S434030
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Valentina Arboleda Forero,1 Jhanelis Patricia Cruzate Hernández,1 Maricela Yepes Restrepo,1 Luis Felipe Higuita-Gutiérrez1,2
1School of Microbiology, Universidad de Antioquia, Medellín, Colombia; 2School of Medicine, Universidad Cooperativa de Colombia, Medellín, Colombia
Correspondence: Luis Felipe Higuita-Gutiérrez, Email [email protected]
Objective: To describe the frequency of self-medication with antibiotics and its associated factors in Medellín, Colombia.
Methods: A descriptive study was conducted on 778 individuals surveyed regarding sociodemographic characteristics, self-medication with antibiotics, reasons for using these drugs, and types of antibiotics used. The analysis was performed in SPSS using absolute and relative frequencies with their corresponding confidence intervals, chi-square test, and logistic regression.
Results: The frequency of self-medication with antibiotics was 46% (95% CI 42.5– 49.5), with 47.4% (95% CI 42.2– 52.5) of the population using antibiotics without medical prescription for flu-like symptoms related to COVID-19. Amoxicillin (33.7%), azithromycin (10.9%), and cephalexin (4.7%) were the most used antibiotics. The main factors associated with self-medication were age group, zone of residence, and lack of information on the appropriate use of these medications.
Conclusion: The city exhibits a high frequency of self-medication with antibiotics, predominantly in conditions where they are ineffective, such as flu-like symptoms related to COVID-19. These findings highlight the contribution of the COVID-19 pandemic to bacterial resistance through self-medication and underscore the need to implement targeted actions to control the use of these medications.
Keywords: self-medication, antibiotics, COVID-19, bacterial resistance
Background
Self-medication (SM) is a common practice that involves the use of medications without a medical prescription to treat self-diagnosed symptoms or disorders.1 According to the World Health Organization (WHO), more than 50% of medications prescribed, dispensed, or sold worldwide are inappropriately administered. At the same time, it has been reported that up to 50% of patients take medications incorrectly.2 The frequency of this behavior varies depending on each country and its level of development, ranging from 11.2% to 93.7%.3
Within the phenomenon of SM, the use of antibiotics constitutes a global public health problem because it has been associated with antimicrobial resistance and the development of adverse effects, which, in addition to the consequences in morbidity and mortality, represent an economic burden for health services.4 There are multiple reasons that lead to SM with antibiotics, including difficult access to the healthcare system, proximity of pharmacies to the place of residence, education level, socioeconomic status, the need to reduce costs for patients, and emergencies.5
One of the recent emergency situations with the greatest impact on global public health was the COVID-19 pandemic, during which SM with antibiotics became a prevalent practice for the prevention and management of symptomatic cases associated with this disease.1 Some studies indicate that during the first year of the pandemic, the use of antibiotics and cases of resistant infections increased, with 50% of patients with severe COVID-19 infection dying in hospitals due to bacterial resistance.6
Previous studies conducted across globe have measured the frequency of SM with various categories of medications, including antibiotics during the pandemic in Iran,7 Pakistan,8 Togo9 and Australia.10 In Latin America, SM is common. In Peru, a frequency of SM for COVID-19 treatment of 54.8% was reported, with 71.5% of them using azithromycin.11 In Ecuador, a frequency of SM of 48.4% was found, with azithromycin being the most used antibiotic (22%), and this practice was associated with male sex and access to unreliable sources of information.12
In Colombia, there is only one study in which it was revealed that the COVID-19 pandemic has prompted people to increase SM behavior as a way to control their health.4 This study was conducted in the city of Pereira and the surrounding areas. The results showed that 136 of the participants had SM practices from the beginning of the quarantine until the time of the survey, representing a frequency of 34.3%, and approximately 15% of people who SM used antibiotics.4 This behavior is due to several reasons, including uncertainty and concern generated by the disease, lack of access or availability of medical care due to healthcare system overload, and the search for quick and accessible solutions to relieve symptoms or prevent the disease.4
In Medellín, the second largest city in Colombia, there is a lack of data regarding the prevalence of SM with antibiotics during the COVID-19 pandemic. Moreover, no previous studies have been conducted to identify the frequency of this practice and its associated factors in the general population of the city. The present study was undertaken to address this gap and provide a description of the frequency of SM with antibiotics and its related factors during the COVID-19 pandemic in Medellín, Colombia.
Methods
Design and Population
This study is a cross-sectional descriptive study that included 778 individuals over 18 years old from the general population of Medellín city, distributed across seven geographical zones. In the sample, we maintained the proportion of individuals contributed by each zone to the total population as follows: North-western (% of the population 19.8 - % of the sample 20.3 (95% CI 17.6–23.2)), North-eastern (% of the population 22.7 - % of the sample 19.3 (95% CI 16.6–22.2)), Central-western (% of the population 13.9 - % of the sample 14.4 (95% CI 12.1–17.0)), Central-eastern (% of the population 16.0 - % of the sample 17.1 (95% CI 14.6–19.9)), South-western (% of the population 10.8 - % of the sample 10.9 (95% CI 8.9–13.3)), South-eastern (% of the population 4.3 - % of the sample 5.0 (95% CI 3.6–6.7)), Rural districts (% of the population 12.5 - % of the sample 13.0 (95% CI 10.8–15.5)). The sample size was calculated following the approach used by Sampedro et al.13 Participants who demanded financial compensation for their participation, those who did not sign the informed consent form, and those who could not respond to the entire survey were excluded. Additionally, a control variable was considered to exclude participants who reported taking antibiotics but used other types of drugs such as analgesics, antihypertensives, anti-inflammatories, among others. Therefore, 136 individuals were excluded from the initial 914 required in the sample size calculation.
Survey
For this study, a primary source of information was used, which consisted of a survey with 11 items that inquired about sociodemographic characteristics and SM with antibiotics during 2021–2022 (Supplementary Survey). The socioeconomic level was defined according to the socioeconomic stratification conducted by the National Administrative Department of Statistics (DANE, acronym in Spanish). The inclusion of this timeframe is justified by the declaration of a state of health emergency due to COVID-19 in Colombia on March 12, 2020,14 followed by Decree 457 of March 22, 2020, which ordered mandatory preventive isolation nationwide starting on March 25, 2020. This included measures such as restricted movement and curfews that limited the free circulation of both individuals and vehicles.15 The mandatory isolation period was extended several times, with different measures applied for the reactivation of municipalities according to their level of virus impact.16–21 From September 1, 2020, a selective isolation measure was implemented, which included continued individual responsibility for distancing, selective isolation in highly affected municipalities, compliance with biosecurity protocols for activities, teleworking or working from home, and border closures.22 The following stage was referred to as the “new normality”, which involved the continuation of some regulations on free circulation but allowed for the gradual resumption of activities subject to compliance with biosecurity protocols established by the Ministry of Health and Social Protection. Finally, the Health Emergency due to COVID-19 was lifted on July 1, 2022, leading to relaxed isolation measures that enabled the execution of this study.23
The survey instrument design was based on similar studies conducted in other countries such as Peru,24 Nigeria,25 Iran,7 and Togo.9 Additionally, a validation process was carried out by microbiologists with experience in bacterial resistance research for its appearance, and a pilot test was conducted on 30 people to ensure its applicability and acceptability among the study subjects. The survey was self-administered and took approximately 5 to 10 min.
Data Collection
Three researchers distributed across each city’s zone administered the survey. They stationed themselves in high-traffic areas, such as those near mass transit systems, shopping centers, parks, and sports venues. This procedure occurred between August and December 2022.
Data Analysis
In the data analysis, surveys with more than 20% of unanswered questions were excluded. The data were analyzed by calculating absolute and relative frequencies of sociodemographic variables with their 95% confidence intervals. A comparison was made between the frequency of SM and sociodemographic variables such as age group, sex, economic level, zone, education level, healthcare profession, familiarity with the term “resistance”, receiving information about resistance, and receiving information about the use of antibiotics using Pearson’s Chi-square test. The strength of the association was quantified using odds ratios with 95% confidence intervals. A binary logistic regression model was used to identify confounders and explanatory variables. In constructing the model, variables with a p-value < 0.25 in bivariate analysis were considered.26 This procedure allowed the estimation of the adjusted odds ratios (ORa). For polytomous variables, indicator variables were created using the lowest frequency group as the reference group. Analyses were considered significant with p-values < 0.05 and were executed using SPSS 29 software.
Ethics
This study was conducted following the ethical principles outlined in the Declaration of Helsinki and was approved by the Institutional Ethics Committee of the Universidad Cooperativa de Colombia with the code BIO233. Additionally, according to Resolution 8430 of the Ministry of Health of Colombia, this study is classified as a research with no risk.27
Results
This study included 778 participants, of whom 52.1% (95% CI 48.5–55.6) were female. Most of the participants were located in the urban part of the city 87.9% (95% CI 84.5–89.2). Regarding educational level, 31.7% (95% CI 28.5–35.1) had a basic level of education, while 12.1% (95% CI 10.0–14.6) had an education in the healthcare field or related areas. Regarding the population’s awareness of the study topic, 55.1% (95% CI 51.6–58.6) had not heard of the term “bacterial resistance”, 58.8% (95% CI 55.3–62.3) had not received information on this topic, and 51.2% (95% CI 47.6–54.7) had not received information on the use of antibiotics (Table 1).
 |
Table 1 Description of the Sociodemographic Characteristics of the General Population of Medellín, 2022 |
The frequency of SM with antibiotics was 46% (95% CI 42.5–49.5). The most used antibiotic was amoxicillin 33.7% (95% CI 29.0–38.7), followed by azithromycin with 10.9% (95% CI 8.0–14.4), and cephalexin with 4.7% (95% CI 2.9–7.3) (Figure 1). The main reasons for use were flu-like symptoms associated with COVID-19 47.4% (95% CI 42.2–52.5), urinary tract infection 8.1% (95% CI 5.6–11.2), and tonsillitis 8.1% (95% CI 5.6–11.2) (Figure 2).
 |
Figure 1 Most commonly used antibiotics in self-medication among the general population of Medellín, 2022. Note: 36.9% do not recall the antibiotic they consumed. |
 |
Figure 2 Reasons for self-medication with antibiotics in the population of Medellín, 2022. |
When comparing the sociodemographic characteristics of the population with the frequency of SM with antibiotics, it was found to be more common in adults 50.6% (95% CI 45.9–55.2), in women with 48.5% (95% CI 43.7–53.4), individuals from higher socioeconomic level with 63.6% (95% CI 42.9–81.1), and those residing in the southwest region with 62.4% (95% CI 51.8–72.1) (Figure 3). Additionally, it was more prevalent in individuals with higher education levels 57.1% (95% CI 48.2–65.8), and those with a background in the healthcare field with 49.5% (95% CI 39.4–59.5). A statistically significant association was observed for age group, region, and education level (p < 0.05) (Table 2).
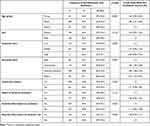 |
Table 2 Comparison Between Sociodemographic Characteristics and the Frequency of Self-Medication with Antibiotics |
In the multivariate analysis, age group, geographical zone, and lack of information about antibiotic use showed a statistically significant association with SM with antibiotics. The frequency of SM with antibiotics was 2.037 (95% CI 1.416–2.930) times higher in adults than in older adults. Those residing in Zone 6 (Southwest) practiced SM with antibiotics 2.524 (95% CI 1.386–4.598) times more than those residing in other areas of the city. Additionally, individuals who did not receive information about antibiotic use engaged in SM 1.405 (95% CI 1.048–1.883) times more than those who received information about antibiotic use. Furthermore, it was identified that educational level was a confounding variable (Table 3).
 |
Table 3 Multivariate Analysis of Factors Associated with Self-Medication with Antibiotics |
Discussion
In this study, the frequency of SM with antibiotics in Medellin was 46%. In addition, the main reason for using antibiotics without a medical prescription was to treat symptoms associated with COVID-19, accounting for 47.4%. This finding was significantly higher than that of a similar study conducted in Australia, where the frequency was 19.5% (n=2217),10 and another in Kenya, where the frequency was 23.6% (n=280).28 It was also higher than a research conducted in Pereira’s city, Colombia (n=397), where the frequency was 15%.4 The differences among the studies could be attributed to factors such as stricter regulations regarding the over-The-counter sales of these drugs in each country or city.10 One study in Medellín found that pharmacists exhibit inadequate knowledge, attitudes, and practices regarding the use and sale of antibiotics without a medical prescription, with 41.3% admitting to selling antibiotics without a prescription for upper respiratory tract infections.29 Initiatives to regulate the sale of antibiotics without a medical prescription have been implemented in Latin American countries suggest that implementing regulatory measures to control the over-The-counter sale of antibiotics has an immediate impact on reducing their consumption.30 Another reason for these differences is the knowledge and beliefs of the SM population. A study in Medellín in this regard show that up to one in four people believe that antibiotics have analgesic or antipyretic properties.13 In response to this issue, the World Health Organization (WHO) has proposed initiatives such as World Antibiotic Awareness Week.31 However, these initiatives alone are insufficient, and it is necessary to design interventions that involve the participation of different sectors that go beyond the unidisciplinary approach of the health sector and extend to the socio-structural determinants of SM.32
On the other hand, amoxicillin (33.7%) was the most used antibiotic, followed by azithromycin (10.9%). These results are consistent with those of a study conducted in Nigeria, which found that amoxicillin was the most used antibiotic, accounting for 24.9% of all antibiotics.25 Similarly, studies in Pakistan and Nepal reported that azithromycin was the most commonly used antibiotic, with percentages of 14.9% and 8%, respectively.8,33 One reason for this finding is that these antibiotics are frequently prescribed for the outpatient treatment of respiratory infections. Therefore, the common use of these drugs may be related to previous prescriptions.34 The high frequency of using these two medications is alarming. On one hand, it contributes, as mentioned earlier, to antibiotic resistance, and on the other hand, it can be associated with adverse effects. Amoxicillin, for example, can cause gastrointestinal problems such as diarrhea, abdominal pain, and even severe allergic reactions, including anaphylaxis, angioedema, or bronchospasm.35 In addition, azithromycin can lead to adverse effects such as diarrhea, abdominal pain, nausea, vomiting, headache, dizziness, taste disturbances, and ototoxicity with the administration of high doses over a prolonged period.36
Furthermore, the most common reasons for SM with antibiotics were flu-like symptoms associated with COVID-19, urinary tract infection symptoms, and tonsillitis. Similarly, in Kenya, Bangladesh, and Peru, it has been reported that treating COVID-19-related symptoms was one of the main reasons for SM with antibiotics.24,28,37 This trend in the results can be attributed to the widespread belief that antibiotics can treat symptoms related to viral infections.10,38 However, antibiotics such as amoxicillin work by inhibiting the synthesis of peptidoglycans in the bacterial cell wall, whereas azithromycin inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit.36 Therefore, as emphasized by the World Health Organization (WHO), antibiotics are not effective against viral infections. It is crucial to debunk the misconception that antibiotics can treat symptoms related to viral infections because these medications are designed exclusively for the treatment of bacterial infections.39
Additionally, this study found that the main factors associated with SM were being an adult (27–59 years old), residing in the southwestern zone, and lacking information about the proper use of antibiotics. These findings are consistent with those of the existing literature, which also indicates that the frequency of SM is more common in this age group.8,40 One possible explanation for this finding is that the adult population is economically active and often faces higher work demands, which may hinder their access or availability of time to seek proper medical attention. Regarding the zone of residence, our results indicate that those residing in urban areas showed a higher frequency of SM than those living in rural areas, similar to findings in other countries such as Iran7 and Nepal.41 While not explored in depth, there may be several reasons that could explain this finding and could be the subject of future research. For example, urban areas tend to have greater availability and accessibility of pharmacies and establishments where medications can be obtained. In addition, people living in urban areas may have a faster-paced lifestyle, which could lead to reduced willingness to seek medical attention. In this study, it was also found that a lack of information about the proper use of antibiotics is associated with a higher frequency of SM. Other studies have also supported this finding.10,25 However, a research in Medellín found that having good knowledge does not always translate into appropriate practices.13 This highlights the need to redesign intervention strategies with a greater emphasis on actual practices, as knowledge alone does not guarantee appropriate behavior regarding SM.
The findings of this study should be interpreted with caution because it was conducted in the city of Medellín, and they may not be generalizable to the entire population of Colombia. Additionally, it is essential to consider that the information collected only pertains to the period of economic reactivation between 2021 and 2022, excluding the more critical period of the pandemic, which was marked by mandatory preventive isolation in 2020 with stricter quarantine periods. This omission was due to operational limitations that prevented the study from being conducted during the study period. This study did not include a question about the source of information for self-medication. Subsequent studies should consider this aspect. In addition, the results may be subject to memory bias because the participants were asked about their past antibiotic use. Despite these limitations, being the first study of its kind in Colombia, this research could serve as a basis for replication in other cities in the country, allowing for data that reflects the situation at a national level and contributing to informed decision-making in the healthcare sector. In this regard, reducing SM could have a positive impact by lowering expenses related to medical care and treatments associated with antibiotic resistance and adverse effects.
Conclusion
In the city of Medellín, there is a high frequency of SM with antibiotics, and their use is prevalent in illnesses where they are ineffective, such as flu-like symptoms related to COVID-19. These findings highlight the contribution of the COVID-19 pandemic to antibiotic resistance through SM and underscore the need for implementing targeted actions to control the use of these drugs. This study can serve as a reference point for future research in other cities and even in other countries, enabling more specific design of educational strategies and the implementation of actions to regulate the use of antibiotics.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted following the ethical principles outlined in the Declaration of Helsinki and was approved by the Institutional Ethics Committee of Universidad Cooperativa de Colombia with the code BIO233.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was carried out with resources from the Universidad Cooperativa de Colombia grant INV3169.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Faqihi AHMA, Sayed SF. Self-medication practice with analgesics (NSAIDs and Acetaminophen), and antibiotics among nursing undergraduates in University College Farasan Campus, Jazan University, KSA. Ann Pharm Fr. 2021;79(3):275–285. doi:10.1016/j.pharma.2020.10.012
2. Organización Mundial de la Salud (OMS). Promoción del uso racional de medicamentos: componentes centrales [Promoting rational use of medicines : core components]; 2002. Available on https://apps.who.int/iris/bitstream/handle/10665/67532/WHO_EDM_2002.3_spa.pdf;jsessionid=EAD6CC412CE4B3DCCBD5CF425EC84DE9?sequence=1.
3. Baracaldo D, Trujillo M, Pérez A, Feliciano J, Calderón C, Soler F. Definition of self-medication: a scoping review. Ther Adv Drug Saf. 2022;13. doi:10.1177/20420986221127501
4. Gaviria A, Mejía D, Duarte C, et al. Self-medication and the ‘infodemic’ during mandatory preventive isolation due to the COVID-19 pandemic. Ther Adv Drug Saf. 2022;13. doi:10.1177/20420986221072376
5. Horumpende P, Said S, Mazuguni F, et al. Prevalence, determinants and knowledge of antibacterial self-medication: a cross sectional study in North-eastern Tanzania. PLoS One. 2018;13(10):e0206623. doi:10.1371/journal.pone.0206623
6. CDC. COVID-19 reverses progress in fight against antimicrobial resistance in U.S. Centers for Disease Control and Prevention; 2022. Available from: https://www.cdc.gov/media/releases/2022/s0712-Antimicrobial-Resistance.html.
7. Mahmoudi H. Assessment of knowledge, attitudes, and practice regarding antibiotic self-treatment use among COVID-19 patients. GMS Hyg Infect Control. 2022;17:12. doi:10.3205/dgkh000415
8. Chaudhry B, Azhar S, Jamshed S, et al. Factors associated with self-medication during the COVID-19 pandemic: a Cross-Sectional Study in Pakistan. Trop Med Infect Dis. 2022;7(11):330. doi:10.3390/tropicalmed7110330
9. Sadio A, Gbeasor F, Konu R, et al. Assessment of self-medication practices in the context of the COVID-19 outbreak in Togo. BMC Public Health. 2021;21(1):58. doi:10.1186/s12889-020-10145-1
10. Zhang A, Hobman E, De Barro P, Young A, Carter D, Byrne M. Self-medication with antibiotics for protection against COVID-19: the role of psychological distress, knowledge of, and experiences with antibiotics. Antibiotics. 2021;10(3):232. doi:10.3390/antibiotics10030232
11. Vasquez E, Failoc V, Martinez R, Morocho N, Temoche M, Valladares M. Self-medication in hospitalized patients with COVID-19: a cross-sectional study in northern Peru. Germs. 2022;12(1):46–53. doi:10.18683/germs.2022.1305
12. Arias F, Izquierdo J, Naranjo P, et al. A cross-sectional analysis of self-medication patterns during the COVID-19 pandemic in Ecuador. Medicina. 2022;58(11):1678. doi:10.3390/medicina58111678
13. Sampedro M, González M, Arango S, Higuita-Gutiérrez LF. Knowledge, attitude and practice regarding antibacterial and their resistance in Medellín-Colombia: a Cross-Sectional Study. Antibiotics. 2023;12(7):1101. doi:10.3390/antibiotics12071101
14. Función Pública. Decreto 417 de 2020 [Decree 417 of 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=110334.
15. Función Pública. Decreto 457 de 2020 [Decree 457 fo 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=110674.
16. Función Pública. Decreto 531 de 2020 [Decree 531 of 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=111854.
17. Función Pública. Decreto 593 de 2020 [Decree 593 of 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=116478.
18. Función Pública. Decreto 636 de 2020 [Decree 636 of 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=119997.
19. Función Pública. Decreto 749 de 2020 [Decree 749 of 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=126400.
20. Función Pública. Decreto 990 de 2020 [Decree 990 of 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=134763.
21. Función Pública. Decreto 1076 de 2020 [Decree 1076 of 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=137170.
22. Función Pública. Decreto 1168 de 2020 [Decree 1168 of 2020]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=140210.
23. Función Pública. Decreto 655 de 2022 [Decree 655 of 2022]. Available on: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=186066#11.
24. Quispe J, Fidel E, Manrique D, et al. Self-medication practices during the COVID-19 pandemic among the adult population in Peru: a cross-sectional survey. Saudi Pharm J. 2021;29(1):1–11. doi:10.1016/j.jsps.2020.12.001
25. Wegbom A, Edet C, Raimi O, Fagbamigbe A, Kiri V. Self-medication practices and associated factors in the prevention and/or treatment of COVID-19 virus: a population-based survey in Nigeria. Front Public Health. 2021;4(9):606801. doi:10.3389/fpubh.2021.606801
26. Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. doi:10.1186/1751-0473-3-17
27. Ministerio de Salud. Resolución 8430 de 1993. Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. [Resolution 8430 of 1993. By which the scientific, technical, and administrative standards for health research are established.]; 1993. Available on: https://www.minsalud.gov.co/salud/Lists/Normatividad%20%20Salud/DispForm.aspx?ID=2110&ContentTypeId=0x0100A08A4A1DF8E9D448BEF600BFAC0E7622.
28. Kimathi G, Kiarie J, Njarambah L, Onditi J, Ojakaa D. A cross-sectional study of antimicrobial use among self-medicating COVID-19 cases in Nyeri County, Kenya. Antimicrob Resist Infect Control. 2022;11(1):111. doi:10.1186/s13756-022-01150-7
29. Colonia DRM, Ramírez Patiño D, Higuita-Gutiérrez LF. Knowledge, attitudes, and practices regarding antibiotic sales in pharmacies in Medellín, Colombia 2023. Antibiotics. 2023;12(9):1456. doi:10.3390/antibiotics12091456
30. Bavestrello F, Cabello M, Casanova Z. Impacto de medidas regulatorias en la tendencia de consumo comunitario de antibióticos en Chile. [Impact of regulatory measures on antibiotic sales in Chile]. Rev Med Chil. 2002;130(11):1265–1272. doi:10.4067/S0034-98872002001100009
31. World Health Organization (WHO). Antibiotic resistance; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance.
32. Lescure D, Paget J, Schellevis F, van Dijk L. Determinants of self-medication with antibiotics in European and Anglo-Saxon countries: a systematic review of the literature. Front Public Health. 2018;6:370. doi:10.3389/fpubh.2018.00370
33. Acharya A, Shrestha M, Karki D. Self-medication among medical students and staffs of a tertiary care centre during COVID-19 pandemic: a Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2022;60(245):59. doi:10.31729/jnma.7247
34. Llanos F, Mayca J, Contreras C. Características de la prescripción antibiótica en los consultorios de medicina del Hospital Cayetano Heredia de Lima, Perú. [Characteristics of Antibiotic Prescription in the Ambulatory Consultation of the Department of Medicine at the Cayetano Heredia Hospital, Lima, Perú]. Rev Esp Salud Pública. 2002;76(3):207–214. doi:10.1590/S1135-57272002000300005
35. Rodríguez Carranza R. Amoxicilina: Antimicrobianos. [Amoxicillin: antimicrobials.]. En: Vademécum Académico de Medicamentos [Internet]. New York, NY: McGraw-Hill Education; 2015. Available on: accessmedicina.mhmedical.com/content.aspx?aid=1113052055.
36. Heidary M, Ebrahimi A, Kargari A, et al. Mechanism of action, resistance, synergism, and clinical implications of azithromycin. J Clin Lab Anal. 2022;36(6):e24427. doi:10.1002/jcla.24427
37. Nasir M, Chowdhury A, Zahan T. Self-medication during COVID-19 outbreak: a cross sectional online survey in Dhaka city. Int J Basic Clin Pharmacol. 2020;9:1325–1330. doi:10.18203/2319-2003.ijbcp20203522
38. World Health Organization (WHO). WHO multi-country survey reveals widespread public misunderstanding about antibiotic resistance; 2015. Available from: https://www.who.int/news/item/16-11-2015-who-multi-country-survey-reveals-widespread-public-misunderstanding-about-antibiotic-resistance.
39. World Health Organization (WHO). Coronavirus disease (COVID-19) advice for the public: mythbusters; 2022. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters.
40. Elayeh E, Akour A, Haddadin R. Prevalence and predictors of self‐medication drugs to prevent or treat COVID‐19: experience from a Middle Eastern country. Int J Clin Pract. 2021;75(11):e14860. doi:10.1111/ijcp.14860
41. Nepal A, Hendrie D, Robinson S, Selvey L. Knowledge, attitudes and practices relating to antibiotic use among community members of the Rupandehi District in Nepal. BMC Public Health. 2019;19:1558. doi:10.1186/s12889-019-7924-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

