Back to Journals » Infection and Drug Resistance » Volume 15
Antibiotic Prescription Pattern, Appropriateness, and Associated Factors in Patients Admitted to Pediatric Wards of Tibebe Ghion Specialized Hospital, Bahir Dar, North West Ethiopia
Authors Alekaw H , Derebe D , Melese WM, Yismaw MB
Received 20 August 2022
Accepted for publication 27 October 2022
Published 15 November 2022 Volume 2022:15 Pages 6659—6669
DOI https://doi.org/10.2147/IDR.S380897
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Habtemariam Alekaw,1 Dagninet Derebe,2 Wondim Melkam Melese,2 Malede Berihun Yismaw2
1Department of Pharmacy, Debre Berhan University, Debre Berhan, Ethiopia; 2Department of pharmacy, Bahir Dar University, Bahir Dar, Ethiopia
Correspondence: Dagninet Derebe, Email [email protected]
Background: Irrational prescribing of antibiotics leads to the emergence of resistant bacteria. Despite this fact, antimicrobial agents are commonly prescribed in the inpatient setting, especially in infants and children.
Objective: The aim of this study was to assess the pattern of antibiotic prescription, appropriateness, and associated factors in pediatric wards of Tibebe Ghion Specialized Hospital (TGSH), Bahir Dar, North West Ethiopia, September 11th, 2021 to October 12th, 2021 GC (Gregorian Calendar).
Methods: An institution-based cross-sectional study was conducted in the pediatric wards of TGSH from September, 2020 to August, 2021 GC. Data were collected using a structured checklist containing each patient’s socio-demographic characteristics, clinical information, list of prescribed drugs, and reason for prescription. A systematic random sampling technique was used to select pediatric patients’ medical records containing prescribed antibiotics. The collected data were entered and analyzed using SPSS version 25 software.
Results: A total of 279 pediatric patients’ medical cards including at least one antibiotic were reviewed. The study revealed that antibiotics were prescribed for most of the patients (88.9%) for empiric treatment purposes. The main medical conditions for which antibiotics were prescribed were pneumonia (16.8%) and early-onset neonatal sepsis (14.0%). Ceftriaxone was the most widely used (84.9%) antibiotic among the monotherapeutic antibiotics, while ceftriaxone plus metronidazole (23.5%) was the most frequently used combination of antibiotics. A high proportion (30.8%) of the pediatric patients was exposed to inappropriate treatment. Residence in rural areas (P=0.046) and being 1 year old or younger (P< 0.05) were found to be independent determinants of inappropriate drug use.
Conclusion: Antibiotics were the most prescribed class of medications for pediatric patients in TGSH. Ceftriaxone and ampicillin were the most frequently prescribed antibiotics in the pediatric wards of TGSH. A high proportion of patients had been exposed to inappropriate antibiotic treatment. Early age and rural residence were found to be the factors that were significantly associated with inappropriate antibiotic utilization.
Keywords: antibiotics, pediatric, appropriateness, prescribing pattern, determinant factor
Introduction
Many of the antibiotics in use today are unnecessarily prescribed for viral infections, such as the common cold. Thus, using antibiotics to treat these viral infections is considered misuse or overuse of antibiotics. The availability of antimicrobial agents without prescription in many developing countries is a big problem, which has been facilitating the development of resistance.1,2
About one-third of the total prescriptions in a hospital are antibiotics; about one-third of these antibiotic prescriptions are usually irrational, and about one-third of the hospital pharmacy budget is spent on antibiotics.3,4 There have been fewer studies on antibiotic use in children than in adult patients. The development of antibiotic resistance is promoted by the use of antibiotics for viral infections and by the use of broad-spectrum antibiotics when a more selective and narrow-spectrum agent would be more appropriate.5,6 Irrational use of antibiotics can result in financial wastage and harm to patients and the pharmaceutical industry.7,8 The continual exposure of microorganisms to antimicrobial agents diminishes the wide ecologic effects, which enables the organisms to develop mechanisms to ensure their survival. Thus, the progeny of the resistant strain is unaffected by the drug and has the capability to produce disease, while the sensitive strains are exterminated by a process known as selective pressure. Intensive treatment with antibiotics such as azithromycin in the community has resulted in resistant Streptococcus pathogens through selective pressure.9,10
Pediatric populations are different from adult populations in their physiology, pharmacokinetics, and pharmacodynamics. The market for children’s medicines tends to be small and the range of doses used for any drug formulation may be wide because many drugs prescribed widely for infants and children are not available in suitable dosage forms, leading to a lack of attention to pediatric medicines.1 A variety of factors have been found to influence (predict) antibiotic prescription. These include patient characteristics, such as low socioeconomic status, the age of the patient, and comorbidity; physician factors, such as educational qualifications, experience of the physician, and source of updating knowledge; and practice setting. Even promotion of a drug by the pharmaceutical industry can increase the chances of irrational prescribing.11–14
Statement of the Problem
A government agency has calculated that there are around 250,000 Clostridium difficile infections in hospitalized patients every year due to incorrect prescribing of antibiotics.15 Knowledge of drug administration in children and infants lags behind that in adults for many reasons, including developmental differences that affect the pharmacodynamics and pharmacokinetic profiles of drugs, ethical and financial reasons, research capabilities, and regulatory guidelines and constraints. Irrational drug use, especially antimicrobials in a pediatric population, has become a commonly noted practice. A study in the USA and Canada showed that 50% and 85% of antibiotics, respectively, were prescribed inappropriately to children.1
World Health Organization (WHO) reports have shown that efforts to promote rational antibiotic use are poor in developing countries, including Ethiopia.16 To promote a more rational use of antibiotics, many countries have implemented antibiotic stewardship programs. However, Ethiopia is a country that has no such program in the health sector. Considering the fact that timely access to healthcare services for infants and children is in the hands of parents or any other third party, which could adversely impact the health status of pediatric patients, healthcare workers are expected to play crucial and lifesaving roles by selecting the most appropriate drugs, including antibiotics, for pediatric patients.6 So far, no studies have been carried out to assess whether physicians are playing their expected crucial role in managing and saving the lives of pediatric patients admitted to Tibebe Ghion Specialized Hospital (TGSH), Bahir Dar, North West Ethiopia. Hence, this study aimed to assess the appropriateness of the antibiotic prescribing pattern and its determinants.
Significance of the Study
Assessment of the proper use of antibiotics at a ward level can generate detailed information about the magnitude and composition of antibiotic consumption, and gives an insight into the rationality of prescribing. Furthermore, this study could also provide information for policy makers on the real situation of antibiotic utilization, which can significantly help them to monitor, evaluate, and suggest corrections to the practitioners’ prescription habits, and implement cost-effective policies to make patient care more reasonable and effective through the promotion of rational antibiotic use. This study could also be used as a basis to undertake studies at the national level on the appropriateness of antibiotic utilization and development of resistance.
Objective
General Objective
To assess the antibiotic prescribing practice, appropriateness, and associated factors among patients in the pediatric wards of TGSH, Bahir Dar, North West Ethiopia, in 2020–2021 GC (Gregorian Calendar).
Specific Objectives
- To determine the patterns of antibiotic prescription in the pediatric wards of TGSH.
- To evaluate the appropriateness of antibiotic prescription in the pediatric wards of TGSH.
- To determine the factors associated with inappropriate antibiotic prescription in the pediatric wards of TGSH.
Methods
Study Design and Period
A retrospective cross-sectional study was conducted from September, 2020 to August, 2021 GC.
Study Area
The study was conducted in TGSH, which is a teaching hospital of Bahir Dar University. The hospital is located in Bahir Dar city, 565 km away from Addis Ababa. The hospital currently provides inpatient and outpatient services for more than 7 million people in Amhara region and the surrounding Benishangul Gumuz region. The hospital provides pharmacy services, clinical laboratory services, surgery, gynecology and obstetrics, maternal and child health, emergency, and other healthcare services.
Population
Source Population
All pediatric patients who have been admitted to pediatric wards of TGSH.
Study Population
All admitted pediatric patients who had received antibiotics as treatment during the study period and fulfilled the inclusion criteria.
Eligibility Criteria
Inclusion Criteria
- Pediatric patients who had been admitted for 24 hours or more.
- Pediatric patients whose medical history cards contained complete information and with at least one prescribed antibiotic. For repeated admissions, antibiotics were taken from the last admission.
Exclusion Criteria
- Patient who had received topical/non-systemic antibiotics.
- Patients who had taken anti-TB medications only.
Variables of the Study
Dependent Variable
Appropriateness of antibiotics use.
Independent Variables
- Sex, age.
- Residence.
- Diagnosis.
- Comorbid conditions.
- Duration of hospital stay.
- Family preference.
Sample Size Determination and Sampling Procedure
Sample Size Determination
The sample size was determined using a single population proportion formula considering the prevalence of antibiotic prescriptions as 74.7%,4 with a 95% confidence level, a margin of error of 5%, and a 10% non-response rate. A correction for the finite population (the number of admitted pediatric patients in TGSH who received prescribed antibiotics in 2020/2021 was 2015) was also considered. The calculated size was 279 patient cards.
Sampling Technique
A systematic random sampling technique was used to select the admitted pediatric patients’ medical records with prescribed antibiotics. Every seventh medical record of the pediatric patients was selected from a total of 2015 pediatric patients’ medical records for 1 year (September, 2020 to August, 2021 GC). The first card was taken randomly from the first seven cards using a lottery method.
Definitions of Terms and Operational Definitions
Antibiotics: Chemotherapeutic agents with activity against microorganisms.
Antibiotic utilization: Use of antibiotics for the treatment of bacterial infections.
Antimicrobial stewardship (AMS): Coordinated interventions designed to improve and measure the appropriate use of antimicrobials by promoting the selection of the optimal antimicrobial drug regimen, dose, duration of therapy, and route of administration.
Appropriate antibiotics: Antibiotics which are prescribed for the right indication, at the right dose, frequency, and duration.
Empirical treatment: Administration of drugs without identification of the causative agent.
Infants: Individuals aged less than 1 year.
Kinetic treatment: Treatment undertaken after definitive identification of the causative agent.
Pediatrics: Individuals aged up to 14 years.
Resistance: Lack of responsiveness of microorganisms to antimicrobials, as a result of developing their own mechanisms.
Data Collection Tool
Data were collected from the medical records of patients on the pediatric wards using a pretested semistandard questionnaire. The data collection format contains the patients’ socio-demographic characteristics, patterns of antibiotics prescription, clinical information, and suspected factors associated with antibiotic prescribing patterns. Once the data had been collected, the appropriateness of antibiotic therapy was evaluated using various references, including Medscape, UpToDate version 21.6, Micromedex, standard and updated text books, and specific guidelines from the Ministry of Health of Ethiopia and the American Academy of Pediatrics (AAP), based on the updated daily patient and clinical characteristics. Based on the above resources, treatment with antibiotics was considered appropriate if antibiotics were prescribed for the right indication, at the right dose and frequency, and for the correct duration. The questionnaire was developed in English.
Data Quality Assurance
Before starting the actual data collection, the data extraction sheet was pretested on 5% of the actual sample size of the patients’ medical cards. Based on the findings of the pretest, the data extraction sheet was revised. Completeness of the data was checked on a daily basis.
Reassessment of the card was carried out to incorporate missing information.
Data Analysis Technique
The collected data were coded, entered, and analyzed using SPSS version 25 software. Data were described and presented using frequencies, tables, and charts. Crude and adjusted odds ratios with 95% confidence intervals (CIs) were computed using univariable and multivariable logistic regression to identify factors associated with antibiotic prescribing patterns. A P-value ≤0.05 was considered statistically significant.
Ethical Considerations
Prior to commencement of the actual study, the proposal was approved by Bahir Dar University, College of Medicine and Health Sciences, Ethical Review Board. In addition, permission was obtained from the general director of TGSH and the dataset owner to use the information in databases/repositories for the purposes of the research conducted. As this was a retrospective study, the requirement for consent was waived by the ethics board/committees. Confidentiality was achieved by omitting patient identifiers. Our study was conducted in accordance with the Declaration of Helsinki.
Results
Socio-Demographic Characteristics of the Participant Pediatric Patients
A total of 279 admitted pediatric patients’ medical records containing prescribed antibiotics were reviewed and analyzed for the evaluation of the appropriateness of antibiotic prescription and its associated factors in TGSH pediatric wards. Of these, 176 (69.1%) were male and about two-thirds (67.4%) were from rural areas. The mean age of the study population was 1.96±3.48 years, and the majority of them (n=181, 64.5%) were neonates and infants. The body weight of the majority of the study population (n=134, 48.0%) was <5 kg, which was followed by 81 patients (29.0%) with a body weight of 5–9.99 kg (table 1).
 |
Table 1 Socio-Demographic Characteristics of Pediatric Patients in TGSH Pediatric Wards, from September 1st, 2020 to August 31st, 2021 GC (n=279) |
Types of Diagnosis and Drug Prescription Pattern
Almost all (99.3%) of the pediatric patients included in this study had an empiric diagnosis. Concerning the purpose of therapy, 248 (88.9%) of the patients were prescribed with drugs for empiric treatment purposes. The numbers of antibiotics used for empiric, prophylactic, and definitive treatment were 546, 51, and 14, respectively. Regarding the number of diseases diagnosed per individual patient, 101 (36.2%) had a single diagnosis, 78 (28%) had two diagnoses, and 100 (34.9%) had more than two diagnosed illnesses. The most common diagnosed diseases were pneumonia, early-onset neonatal sepsis (EONS), and meningitis, each accounting for n=47 (16.8%) n=39 (14%), and n=21 (7.5%), respectively (table 2).
 |
Table 2 Common Conditions for Which Antibiotics Were Prescribed for Pediatric Patients in TGSH Pediatric Wards, from September 1st, 2020 to August 31st, 2021 GC |
Prescribing Pattern of Antibiotics
In this study, a total of 964 drugs were prescribed to the patients, of which 611 (63.38%) were antibiotics. Of the 53 (8.7%) antibiotics prescribed as a single agent, ceftriaxone (n=45, 84.9%) was the most frequently prescribed monotherapeutic agent. From the total of 558 (91.3%) antibiotics prescribed in combination, ceftriaxone + metronidazole (n=53, 23.5%) took the largest percentage share, followed by ampicillin + gentamicin (n=49, 21.7%), and ampicillin + ceftriaxone (n=24, 1%) (table 3).
 |
Table 3 Frequency and Percentage of Combination and Single Antibiotics Prescribed to Pediatric Patients in TGSH Pediatric Wards, from September 1st, 2020 to August 31st, 2021 GC |
The average number of drugs per patient was 3.46 and more than 90% of the patients were exposed to at least two drugs. The average number of antibiotics per prescription was 2.19 and most of the patients (83.2%) were treated with a combination of two or more antibiotics. The maximum number of drugs per patient was 10 and the maximum number of antibiotics per patient was seven (0.7%).
The parenteral route accounted for the administration of most (85.3%) of the prescribed drugs, and a shift from the parenteral to the oral route upon discharge was practiced in only 31 (11.1%) of the cases. The most common oral medication prescribed upon discharge was cefixime (48.6%). Nearly all (97.8%) antibiotic drugs were prescribed under their generic name.
Appropriateness of the Prescribed Antibiotics
In this study, only 69.2% of the participants were prescribed with the appropriate drug at the correct dose, duration, and frequency. The highest proportion of the patients (20.8%) was exposed to antibiotics that were not recommended for their condition, followed by inappropriate duration (16.1%), inappropriate dose (14%), and inappropriate frequency (4.7%).
The age, weight, and disease were considered as patient factors in stating that the dosage regimen was appropriate or inappropriate. The WHO Pediatric Handbook 2nd ed.,21 Nelson Textbook of Pediatrics 20th ed.,22 and Ethiopian standard treatment guidelines for general hospitals were used as references.23
Drug interactions were found in 12.9% of the pediatric patients and the commonest drug interaction were antibiotics. In 20.8% of pediatric patients antibiotics were prescribed in the presences of contraindications. Ceftriaxone and azithromycin are prescribed drugs in the presence of contraindication (table 4).
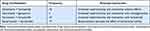 |
Table 4 Potential Drug–Drug Interactions Between Some Concomitantly Prescribed Drugs at TGSH, Bahir Dar, Ethiopia, from September 1st, 2020 to August 31st, 2021 GC |
Factors Associated with Antibiotic Prescription Appropriateness
The appropriateness of antibiotic prescription among pediatric patients was associated with various factors. There was more inappropriate drug therapy in pediatric patients from rural areas than urban ones (AOR=0.574, 95% CI=0.333–0.989, P=0.046). Significant associations were observed between the appropriateness of antibiotic prescription and both the age of the patients and parental negligence. Patients aged <1 month (AOR=4.933, 95% CI=1.577–15.428, P=0.06) and 1 month to 1 year (AOR=3.18, 95% CI= 1.166–11.225, P=0.026) had higher levels of inappropriate drug therapy. Regarding parental negligence, patients whose parents were negligent during their child’s treatment were more likely to have inappropriate drug therapy compared to those without parental negligence (AOR=6.978, 95% CI 1.872–20.017, P=0.04) (table 5).
Discussion
In this study, the majority of pediatric patients were male (n=176, 63.1%), were infants (n=181, 64.5%), and came from rural areas (n=187, 67%). The finding that the highest numbers of admission were in neonates and infants suggests that patients in these age groups are highly susceptible to infections. The weight was measured in all patients. However, there was a problem in failing to measure the body weight in a study conducted in Nekemte Referral Hospital, in which no weight was recorded for 29.03% of pediatric patients.6 This improvement regarding weight measurement in the pediatric wards of TGSH could be due to health professionals’ intention in measuring weight for the calculation and administration of the correct doses of drugs. This activity is very important to provide the right dose to pediatric patients, who have a high risk of malnourishment.
Most of the pediatric patients (88.9%) were prescribed with drugs for empiric treatment purposes. This is similar to the results from studies conducted in two hospitals in Ethiopia, where 83.58% and 75.9% of the antibiotics were prescribed for empiric treatment in Nekemte Referral Hospital and Shenan Gibe Hospital, respectively.1,6 The high level of empiric treatment in higher level hospitals in the country could be related to the seriousness of diseases that need prompt management, the absence of diagnostic stewardship, late presentation to healthcare service delivery points, rural residence, and the associated low levels of healthcare-seeking behavior.
In this study, pneumonia was the most common reason for hospitalization, accounting for 47 (16.8%) of the cases, followed by early-onset sepsis (n=39, 14%) and meningitis (n=21, 7.5%). These results are in line with study a conducted in Shenan Gibe Hospital, where the major medical conditions for prescribed antibiotics were pneumonia (n=125, 38.5%), sepsis (n=49, 15.2%), and acute gastroenteritis (n=41, 12.7%).1 These results are also in concordance with a study conducted in Jimma University specialized hospital, where the major medical conditions for prescribed antibiotics were severe pneumonia (31.23%) and late-onset neonatal sepsis with meningitis (20.60%).17 The similarities in the reasons for hospitalization in pediatric patients in different hospitals in Ethiopia could provide a hint for identifying the most common pediatric infectious problems in the country.
In total, 611 antibiotics were prescribed for 279 patients; this indicated an average of 2.19 antibiotics per prescription. This value is similar to that in a study conducted in Jimma University specialized hospital, where the average number of antibiotics per patient was 2.17;17 however, it is a little lower than in a study conducted in Shenan Gibe Hospital, where it was 2.37.1 Most of the patients (n=232, 83.2%) were treated with a combination of two or more antibiotics, while 47 (16.8%) were treated with a single antibiotic. The maximum number of antibiotics per prescription was seven, which was higher than in the study conducted in Hawassa University Referral Hospital pediatric ward, where it was found to be three,4 and Jimma University specialized hospital, where it was found to be four.17 The high level of antibiotics may be associated with the high level of antibiotic utilization for empiric treatment.
This study showed that ceftriaxone was the most frequently prescribed antibiotic, followed by ampicillin. This utilization is in line with the reasons for admission of pediatric patients. Most of the patients (n=238, 85.3%) were treated with injections. This could be due to the fact that the study was conducted in admitted patients, in which the parenteral route of administration is common practice, and that most of the disease conditions need immediate onset of action of the drugs.
According to the WHO recommendation, the percentage of drug prescription by generic name should be 100%.18 In this study, antibiotics have been found to be prescribed by their generic name in 97.8% of cases, which is very close to the WHO recommendation. Similarly, studies conducted in the pediatric wards of Bishoftu Hospital in East Ethiopia and in Jimma University specialized hospital found 97.5% and 99% generic prescriptions, respectively.17,19
In this study, 30.8% of patients were exposed to an inappropriate drug, dose, frequency, or duration, alone or in combination, and the highest proportion of the patients (20.8%) was exposed to antibiotics that were not recommended for their condition. This result is in line with a study conducted in India, where the majority of patients (44%) were exposed to the wrong antibiotic indication,3 but it is not concordance with a study conducted in Adigrat General Hospital, where the majority of patients encountered inappropriate use of antibiotics due to high or low doses and the overall level of inappropriateness of antibiotic use was slightly lower (28.3%) than in our study.20 Ceftriaxone has been prescribed to pediatric patients below 2 months of age even though the drug is contraindicated owing to its kernicterus adverse effect, and azithromycin has been prescribed to pediatric patients below 6 weeks of age even though it is contraindicated owing to its infantile hypertrophic pyloric stenosis (IHPS) adverse effects. However, these drugs may have been used because of the unavailability of safer alternative agents.
The multivariable logistic regression analysis showed that inappropriate antibiotic prescription was significantly associated with residence and age group. There was higher inappropriate drug therapy in pediatric patients from rural areas in those from than urban ones (AOR=0.574, 95% CI=0.333–0.989, P=0.046), which could be related to the poor health awareness of the patients’ parents. There was also a significantly high level of inappropriate treatment in infants. This may be due to the complexity of infant case treatments, contraindications, and a scarcity of different dosage forms. This finding was not in line with the study conducted in Adigrat General Hospital, where children aged 6–10 years and 11–18 years had the highest odds of inappropriate drug therapy. This disparity could be due to differences in prescribers’ attention in considering differences in dosing of school-age, adolescent, and adult patients.20 In another study, conducted in Vietnam, comorbidities and duration of antibiotic treatment were significantly associated with inappropriate antibiotic usage.14
Conclusion
Antibiotics were the most utilized (64.4%) pharmacologic class of medications for the treatment of pediatric patients. Ceftriaxone and ampicillin were the most frequently prescribed antibiotics in the pediatric ward of TGSH. A high proportion of patients had been exposed to inappropriate antibiotic treatment. Early age, parental negligence, and rural residence were the factors that were found to be significantly associated with inappropriate antibiotic utilization.
Recommendations
Since most of the antibiotics are utilized for empiric treatment, periodic evaluation of the sensitivity of microorganisms to antibiotics with routine testing, and the implementation of an antimicrobial and diagnostic stewardship approach will produce better outcomes in the future. Prescribers should also consider the cost of long-term use of parenteral medications, and hence the shift to equivalent oral medications based on the patient’s prognosis has to be encouraged.
Acknowledgment
First, we would like to thank Bahir Dar University for providing us with the chance to conduct this study. Our gratitude extends to the general director of Tibebe Ghion Specialized Hospital for providing us with the available information. We are grateful to the data collectors, supervisors, and all study participants for giving their precious time during data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Barghouthi Achalu T. Mensa M retrospective drug use pattern of antibiotics in pediatric ward of shenan gibe hospital, Oromia Region, Ethiopia. J Antibio Res. 2017;1(1):106. doi:10.15744/2574-5980.1.106
2. Alakhali K, Shaik Mohammad A. Prescribing pattern of antibiotics in pediatric patients in the Jazan Region, Kingdom of Saudi Arabia. RGUHS J Pharm Sci. 2014;4(3). doi:10.5530/rjps.2014.3.6
3. Anulakshmi S, Yadavalli A. a prospective study on antibiotic prescribing pattern among in-patients of medicine department of a tertiary care hospital. Int J Basic Clin Pharmacol. 2020;9:902–905. doi:10.18203/2319-2003.ijbcp20202179
4. Woldu MA, Suleman S, Workneh N, Berhane H. Retrospective study of the pattern of antibiotic use in Hawassa University referral hospital pediatric ward Southern Ethiopia. J Appl Pharm Sci. 2013;3(2):093–098.
5. Shivaleela J, Revankar S, Vedavathi H, Prasad N, Chidanand KN, Jean LM. A study of prescription pattern of antibiotics in pediatric in-patients of McGann teaching hospital shivamogga institute of medical sciences (SIMS), Shivamogga, Karnataka. IOSR J Dental Med Sci. 2014;13(12):67–71. doi:10.9790/0853-131246771
6. Asefa L, Bayissa G, Abera Z. Antibiotics use evaluation for pediatrics at nekemte referral hospital, East Wollega Zone, Oromia Region, West Ethiopia. World J Medical Sci. 2016;13(1):17–26.
7. Dodoo CC, Orman E, Alalbila T, et al. Antimicrobial prescription pattern in ho teaching hospital, Ghana: seasonal determination using a point prevalence survey. Antibiotics. 2021;10:199. doi:10.3390/antibiotics10020199
8. Ambindei ML, Lobe MG, Acha AE. Indications and patterns of antibiotic prescription in the Buea Regional Hospital of Cameroon. Health Sci Dis. 2015;16(1):1.
9. Choudhury DK, Bezbaruah BK. Antibiotic prescriptions pattern in pediatrics inpatient department Gauhati medical college and hospital, Guwahati. J Appl Pharm Sci. 2013;3(8):144–148.
10. Olayinka AT, Jimoh O, Ejembi J, et al. Antimicrobial prescription pattern in a tertiary hospital. Sahel Med J. 2020;23:103–108. doi:10.4103/smj.smj_17_18
11. Marlot CK, Jan M. A systematic review of quality indicators for appropriate antibiotic use in hospitalized adult patients. Infect Dis Rep. 2017;9:6821. doi:10.4081/idr.2017.6821
12. Chem ED, Anong DN, Akoachere J-FKT. Prescribing patterns and associated factors of antibiotic prescription in primary health care facilities of Kumbo East and Kumbo West Health Districts, North West Cameroon. PLoS One. 2018;13(3):e0193353. doi:10.1371/journal.pone.0193353
13. Bist A, Kulkarni GP, Gumma KM. Study of patterns of prescribing antibiotics in geriatric patients admitted to the medical wards in a tertiary care hospital. Int J Basic Clin Pharmacol. 2016;5:155–158. doi:10.18203/2319-2003.ijbcp20160119
14. Nguyen LV, Pham LTT, Bui AL, et al. Appropriate antibiotic use and associated factors in Vietnamese outpatients. Healthcare. 2021;9:693. doi:10.3390/healthcare9060693
15. Kumari S, Bagati KD, Krishnan SB. Study of antibiotic utilization pattern in tertiary care teaching hospital. Natl J Physiol Pharm Pharmacol. 2021;11(6):622–627. doi:10.5455/njppp.2021.11.01034202127012021
16. Gube AA, Gonfa R. Evaluation of antibiotic use in medical ward of fitche District Hospital, North Showa Zone, Oromia Region, Ethiopia. Adv Pharmacoepidemiol Drug Saf. 2017;6:217.
17. Achalu TS, Yimam B, Kebede TM. Antibiotics utilization pattern in pediatric ward: the case from tertiary teaching Hospital, South West Ethiopia. Int J Adv Multidiscip Res. 2015;2(9):54.
18. World Health Organization. How to investigate drug use in health facilities: selected drug use indicators. World Health Organization; 1993.
19. Feleke M, Yenet W. Jimma Likisa Lenjisa Prescribing pattern of antibiotics in pediatric wards of Bishoftu Hospital, East Ethiopia. Int J Basic Clin Pharmacol. 2013;2(6):718–722. doi:10.5455/2319-2003.ijbcp20131209
20. Yehualaw A, Taferre C, Bantie AT, Demsie DG. Appropriateness and pattern of antibiotic prescription in pediatric patients at adigart general hospital, Tigray, Ethiopia. Biomed Res Int. 2021;2021:6640892. doi:10.1155/2021/6640892
21. World Health Organization. Pocket book of hospital care for children: guidelines for the management of common childhood illnesses. World Health Organization; 2013.
22. Abbott MB, Vlasses CH. Nelson textbook of pediatrics. Jama. 2011;306(21):23878.;306(21):23878.
23. Standard treatment guidelines for general hospital 4th edition, ministry of health Ethiopia; 2021.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

