Back to Journals » Clinical Pharmacology: Advances and Applications » Volume 14
Anti-Diarrheal Activities of Hydromethanolic Crude Extract and Solvent Fractions of Acacia seyal (Fabaceae) Roots in Mice
Authors Mengesha AK , Birru EM , Adugna M
Received 2 August 2022
Accepted for publication 4 October 2022
Published 15 November 2022 Volume 2022:14 Pages 99—110
DOI https://doi.org/10.2147/CPAA.S383896
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Arthur E. Frankel
Assefa Kebad Mengesha, Eshetie Melese Birru, Meaza Adugna
Department of Pharmacology, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Assefa Kebad Mengesha, Email [email protected]
Background: Traditionally, the root of Acacia seyal is used for the treatment of diarrhea. However, its efficacy has not been scientifically evaluated. Thus, this study aimed to validate the antidiarrheal activities using hydromethanolic crude extract and solvent fractions of Acacia seyal roots in mice.
Methods: In each model, mice were divided into five groups of six mice at random. Group I mice (negative controls) were given 1mL/100 g distilled water for hydromethanolic crude extract tests as well as n-hexane, ethyl acetate and aqueous fractions, while groups II, III, and IV were given 100 mg/kg, 200 mg/kg, and 400 mg/kg of hydromethanolic crude extract or solvent fractions. Group V mice (positive control) were given 3 mg/kg Loperamide for the castor oil-induced diarrhea and enteropooling test. All of the doses were taken orally. However, Atropine sulfate, 5 mg/kg, was given intraperitoneally for the gastrointestinal motility test. Statistical Package for the Social Sciences (SPSS) version 26 was used to examine the statistical significance of differences in the number and weight of wet and total feces, distance traveled by a charcoal meal, and intestinal fluid accumulation across groups.
Results: When compared to the vehicle-treated group, the crude extract and n-hexane fraction notably delayed the onset of diarrhea, reduced the weight and volume of intestinal contents, and hindered the intestinal transit at all tested doses (P < 0.001). The ethyl acetate fraction also significantly (P < 0.001) decreased the weight of intestinal content at all doses examined. Only at 400 mg/kg did the aqueous fraction statistically (P < 0.01) prolonged the onset of diarrhea and impeded gastrointestinal motility.
Conclusion: According to this study, the hydromethanolic crude extract and solvent fractions of Acacia seyal roots have promising antidiarrheal effects.
Keywords: antidiarrheal, Acacia seyal, castor oil, enteropooling, gastrointestinal motility
A Letter to the Editor has been published for this article.
A Response to Letter by Dr Panjaitan has been published for this article.
Background
Diarrhea is the passage of three or more loose or liquid stools per day.1–3 It continues to be an existential danger to global public health, particularly for children aged five and under in low- and middle-income countries, where access to and the cost of excellent healthcare are both inadequate and unaffordable.1 Diarrhea is the second-greatest cause of death in children under the age of five worldwide, accounting for 15% of all deaths in this age group.4,5 According to the World Health Organization 2017, the mortality rate for children under the age of five in low-income countries was 73.1 fatalities per 1000 live births in 2016, roughly 14 times the rate in high-income nations.4
 |
Figure 1 Anti-diarrheal indices of the crude extract and solvent fractions of Acacia seyal roots in mice. |
Herbal medications play an important role in improving primary healthcare in both developed and developing countries since they are effective in biological and therapeutic qualities.6 Ethnomedicine is always the first choice for treating ailments in Africa since it is inexpensive and may be obtained from locally available plants or other natural sources.7 Traditional medicine is widely used in Ethiopia both in urban and rural regions, as opposed to modern medicine, which could be due to the systems’ accessibility, cultural acceptance, and economic affordability.8
Acacia seyal is a thorny tree that grows 6 to 17 meters tall and has white to greenish-yellow or orange-red bark on the trunk. Acacia seyal has high contents of flavonoids, phenolics and anthocyanins.9–11 Traditionally, Acacia seyal is used for the treatment of malaria, wound, cancer (for crushing and spitting leaves), diarrhea (maceration of water-extract roots), edema, and dandruff.12–18 Pharmacologically, the plant, Acacia seyal has also reported in vitro antioxidant, anti-inflammatory, and antibacterial19–22 as well as in vivo antimalarial and antidepressant effects.23,24 According to Ethnobotanical survey studies, several plants have claimed antidiarrheal activities,8,25 but scientific therapeutic and safety evaluations on some of these plants such as Acacia seyal have not been reported. Thus, this study is aimed to validate the antidiarrheal activity and safety evaluation of Acacia seyal root using animal models and the result of the study may also initiate further investigation.
Methods
Plant Material
Fresh roots of Acacia seyal were collected around Makisegnit town 41km from Gondar city, North West Ethiopia in April 2021. Authentication of the plant was done by a botanist (Mr. Abiyu Enyew, Plant biology, and biodiversity Gondar University) and a voucher specimen (number 001/AKM/2021) was deposited in the Department of Biology, National Herbarium, University of Gondar.
Experimental Animals
Swiss albino mice of either sex (age 8–12 weeks, weight 20–30) were utilized, which were raised at the University of Gondar’s Department of Pharmacology. In the department’s animal house, they were kept in regular conditions with a 12 h light/12 h dark cycle, pellets, and water ad- libitum. Before beginning the experiment, all mice were acclimatized to the experimental environment for one week. They were kept and cared for by OECD guidelines.26
Preparation of Plant Material
Acacia seyal roots were cleaned with tap water before being sliced into small pieces and dried in the shade at room temperature. The dried roots were then roughly pulverized with an electrical mill, and the coarsely powdered roots were macerated in a 1: 6 (W/V) ratio with hydro methanol.27 The mixtures were separated after 72 hours, first with gauze and then with Whatman filter paper number 1. The residue was macerated twice for 72 hours using the same volume of hydro methanol. The filtrates were mixed and evaporated to dryness under reduced pressure at 40°C.Finally, 100 grams of dried extract was obtained and kept at 4°C in the refrigerator.
Fractionation
In a separatory funnel, 65g of the dried hydromethanolic crude extract of Acacia seyal roots was dissolved in 390 mL distilled water and then diluted with 390 mL n-hexane. The n-hexane filtrate was collected, and the procedure was carried out three times more. The residue was separated three times using 390 mL of ethyl acetate, and the top layer was collected after each time. The n-hexane and ethyl acetate fractions were dried in evaporator at 40° C with reduced pressure, and the aqueous fraction was lyophilized for additional drying. Finally, 33.48 g of n-hexane, 2.9 g of ethyl acetate, and 28.67 g of aqueous dry fractions were obtained and kept at 4°C in separate vials.27
Grouping and Dosing of Animals
In each model, mice were randomly divided into five groups (n = 6) with the group I receiving the vehicle and groups II to IV receiving of the extract respectively at 100, 200, and 400 mg/kg.26 Group V mice (positive control) were given 3 mg/kg Loperamide for the castor oil-induced diarrhea and enteropooling test. All of the doses were taken orally. However, Atropine sulfate, 5 mg/kg, was given intraperitoneally for the gastrointestinal motility test.28 The extract test doses were chosen based on the findings of the acute toxicity research. Mice were sacrificed by cervical dislocation during enteropooling and gastrointestinal motility testing.29
Acute Oral Toxicity Testing
On healthy female mice, the acute oral toxicity of a hydromethanolic crude extract of Acacia seyal roots was assessed using limit test procedures based on the OECD-425 Guidelines for Chemical Testing.26 Five female Swiss albino mice, weighing 20–30 g and aged 8–12 weeks, were starved for three hours prior to receiving the extract and one hour afterward. A single female mouse was given 2000 mg/kg of the extract as a single dosage by oral gavage for this study, and no death was seen within 24 hours. A total of four mice were employed and given the same dose of the extract. The animals were housed individually in cages and watched for general signs and symptoms of toxicity (such as termer, and hair erection), food and water intake, and mortality for 4 h at 30-minute intervals and then for 14 days at a 24-h interval.
Phytochemical Screening Tests
To investigate the existence of secondary metabolites, phytochemical screening of hydromethanolic crude extract and solvent fractions of Acacia seyal roots was carried out using methodologies previously published in peer-reviewed journals.30,31
Determination of Antidiarrheal Activity
Castor Oil-Induced Diarrhea
According to the directions in the grouping and dosing sections, the mice were fasted for 18 h before being dosed with the test and standard medications. One hour following dosing with the test drugs, each mouse was given 0.5 mL castor oil orally. The mice were then maintained in glass metabolic cages with a clear paper-coated floor so that the number and consistency of feces could be observed. The papers were changed every hour to make the feces visible for counting and checking its consistency. The mice were monitored for four hours, and the timing of the beginning of diarrhea, as well as the quantity and weight of dry and wet feces, were noted. The onset was determined by the time interval in minutes between the introduction of castor oil and the appearance of the first diarrheal stool. The total quantity of diarrheal stools in the negative control group was set at 100%, and the percentages of diarrheal inhibitions for the wet and total content of feces were determined.32
Castor Oil-Induced Enteropooling
The effect of extract and solvent fractions of Acacia seyal root on intraluminal fluid buildup was assessed by measuring the collected fluid in the gut. Mice were fasted for 18 h before receiving the test drugs, as described in the grouping and dosing section, and then given 0.5 mL of castor oil via oral gavage one hour after receiving the test substances. One hour after receiving castor oil, the mice were slaughtered, and their small intestines were removed and weighed. The volume of the contents of the intestine was estimated after they were evacuated into a test tube. The intestine was then reweighed after milking to determine the percentage of inhibition.33
Gastrointestinal Motility Test
As stated in the grouping and dosing sections, the mice were grouped and fasted for 18 h before the experiment. Each mouse received 0.5 mL castor oil one hour after receiving the test chemicals. A normal charcoal meal of 1mL, prepared as a 10% suspension of activated charcoal in 5% gum acacia, was administered by oral gavage after one hour. After thirty minutes, the mice were slaughtered, with the abdomen opened and the small intestine removed, and the length measured with a ruler. The distance traveled by charcoal from the pylorus to the cecum was measured and expressed as a percentage of the length of the small intestine.25
In vivo Antidiarrheal Index
The combined influence of defecation delay, gut meal transit distance, and purging frequency on the number of wet stools are known as the antidiarrheal index (Figure 1).
Ethical Clearance
The experimental protocols were requested to and approved by the Institutional Review Board of the College of Medicine and Health Sciences, University of Gondar, and ethical clearance was obtained (SOP4/98/2013) from the research and publication office of the University.All the experimental animals were handled and used according to the animal care and welfare guidelines34 and OECD guidelines.26
Sponsorship
I got a sponsorship (Grant number: ምር/ህብ/ገ/ም/ፕ/05/26/2013) from University of Gondar, College of medicine and Health Sciences to perform my thesis entitled with Anti-Diarrheal Activities of Hydromethanolic Crude Extract and Solvent Fractions of Acacia seyal (Fabaceae) Roots in Mice.
Statistical Analysis
SPSS version 26.0 was used to analyze the data. All grouped data were statistically examined, with one-way analysis of variance (ANOVA) and Tukey’s HSD post hoc test used to determine the significance of various treatments. The study’s findings were expressed as a mean plus or minus standard error of the mean (SEM) in text, tables, and graphs. At a p-value of 0.05, the results were likewise declared statistically significant.
Results
Acute Oral Toxicity Testing
Acute oral toxicity in mice at a limit dose of 2000 mg/kg body weight did not result in mortality or visible signs of toxicity such as convulsions, anxiety, polyuria, coma, or diarrhea. As a result, the extract’s LD50value is greater than 2000 mg/kg, based on the lack of mortality and toxicity.
Phytochemical Screening Test
Preliminary phytochemical analysis of the hydromethanolic crude extract and solvent fractions of Acacia seyal roots revealed the presence of secondary metabolites like tannins, saponins, phenols, flavonoids, and steroids (Table 1).
 |
Table 1 Types of Secondary Metabolites Present in the Hydromethanolic Crude Extract and Solvent Fractions of Acacia seyal Roots |
Effects on Castor Oil-Induced Diarrheal Model
In this model, the hydromethanolic extract of Acacia seyal roots significantly (P<0.001) delayed the onset of diarrhea, as well as reduced the number and weight of wet and total stools at all tested doses as compared to the negative control. When compared to the negative control, the n-hexane fraction significantly (P<0.001) prolonged the time of diarrheal induction at all tested doses, as well as significantly reduced both the number and weight of wet and total fecal outputs at 100 mg/kg (P<0.01), 200 mg/kg (P<0.001), and 400 mg/kg (P<0.001).Similarly, at 200 mg/kg (P<0.01) and 400 mg/kg (P<0.001), the ethyl acetate fraction, except the 100 mg/kg tested dose, significantly delayed the beginning of diarrhea and decreased the frequency of wet and total feces compared to the vehicle-treated control. In comparison to the vehicle-treated group, this fraction reduced both the weight of wet and total feces at the intermediate (P<0.05) and highest (P<0.001) doses. When compared to the negative control, the aqueous fraction significantly delayed the onset of diarrhea and reduced the number and weight of wet stools at 400 mg/kg (P<0.01). This fraction also statistically (P<0.01 and P<0.05) reduced the number and average weight of total feces when compared to the vehicle-treated group at the tested dose (400 mg/kg).The lowest and medium dosages of this fraction, however, did not show significant reductions in the number and average weight of wet and total fecal outputs when compared to the vehicle-treated group. The highest percentage inhibition of defecation was obtained by the highest dose of the hydromethanolic crude extract (75.55%), which is nearly equivalent to the percentage inhibition of fresh stool defecation of the standard antidiarrheal drug, Loperamide hydrochloride 3 mg/kg (78.04%) as shown in Table 2.
 |
Table 2 Anti-Diarrheal Effects of Crude Extract and Solvent Fractions of the Roots of Acacia seyal on Castor Oil-Induced Diarrhea in Mice |
Effects on Castor Oil-Induced Enteropooling
When compared to the negative control the crude extract demonstrated a substantial (P<0.001) reduction in both the weight and volume of intestinal contents at all doses examined. This extract also produced the highest percentage reduction of the average weight of intestinal contents (75%) at the tested dose of 400 mg/kg, which is nearly equivalent to the percentage reduction of the average weight of intestinal contents produced by the standard anti-diarrheal drug, loperamide 3 mg/kg (76.20%). The n-hexane fraction also reduced both the volume and weight of intestinal contents significantly (P<0.001) at all tested doses as compared to the vehicle-treated group. At the middle and the highest tested doses, this fraction also significantly (P<0.001) reduced the volume of intestinal contents as compared to the 100 mg/kg dose of ethyl acetate fraction. While the ethyl acetate fraction significantly (P<0.001) reduced the average weight of intestinal contents at all tested doses as compared to the vehicle-treated group. However, the aqueous fraction reduced the average weight of intestinal contents only at the middle (P<0.05) and highest (P<0.01) doses as compared to the vehicle control group as shown in Table 3.
 |
Table 3 Effects of the Hydromethanolic Crude Extract and Solvent Fractions of the Roots of Acacia seyal on Castor Oil-Induced Enteropooling in Mice |
Effects on Castor Oil-Induced Gastrointestinal Motility
At all doses, the hydromethanolic crude extract significantly (P<0.001) slowed the transit of the intestine when compared to the negative control. The extract’s tested dose of 400 mg/kg (80.33%) likewise induced the greatest percentage inhibition of intestinal transit, which is comparable to the percentage inhibitions produced by the standard anti-diarrheal medicine, Atropine sulfate 5 mg/kg (83.63%). At all doses examined, the n-hexane fraction significantly (P<0.001) decreased the intestinal motility of charcoal marker when compared to the vehicle-treated mice. Furthermore, this fraction (at 200 mg/kg) significantly slowed the transit of the intestine when compared to the lowest doses of the ethyl acetate fraction (P<0.001).Similarly, as compared to the negative control, the ethyl acetate fraction statistically impeded the transit of the intestine at 200 mg/kg (P<0.01) and 400 mg/kg (P<0.001).However, as compared to the negative control, this fraction did not have a significant effect on intestinal transit inhibition at the tested dose of 100 mg/kg.When compared to the lowest dose of its portion, the extr asact (at 400 mg/kg) significantly slowed intestinal motility. As compared to the vehicle-treated group, the aqueous fraction statistically (P<0.01) inhibited gastrointestinal transit only at the highest tested dose as shown in Table 4.
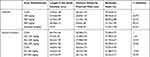 |
Table 4 Effects of Hydromethanolic Crude Extract and Solvent Fractions of the Roots of Acacia seyal on Castor Oil-Induced Gastrointestinal Motility in Mice |
In vivo Anti-Diarrheal Index
Three parameters were used to calculate the in vivo anti-diarrheal indices (ADI) of the crude extract and solvent fractions. Delay in defecation, gut meal travel distance, and purging frequency in the number of wet stools are all factors to consider. The crude extract had the highest anti-diarrheal index (107.17%) at the tested dose of 400 mg/kg, according to this study. The aqueous fraction likewise produced the lowest antidiarrheal index value at the tested dose of 400 mg/kg (59.63%). The anti-diarrheal index values of both the crude extract and solvent fractions increased in a dose-dependent manner as shown in Figure 1: hydromethanolic extract (R2= 0.989), aqueous fraction (R2= 0.997), ethyl acetate fraction (R2= 1), and n-hexane fraction (R2=0.995).
Discussion
Individuals utilize plants or plant-derived preparations customarily, that’s considered to be compelling against diarrheal diseases without any logical premise to clarify the activity of such plants.35 Some previous studies have affirmed the utility of anti-diarrheal medicinal plants by investigating the biological activities of the extracts which have antispasmodic impacts, delay intestinal travel, smother intestine motility, stimulate water retention, or decrease intraluminal liquid aggregation.36
In traditional medicine, the root of Acacia seyal is typically extracted with water to treat diarrhea, but in this study, we used hydromethanolic solvent instead because, due to their expanded polarity range, hydromethanolic solvents (especially 80% methanol) are typically better and more effective at extracting the most significant bioconstituents of the plant material.37,38
Using castor oil-induced diarrhea models, this investigation confirmed the roots of Acacia seyal’s traditional use and safety profile (castor oil-induced diarrhea, enteropooling, and gastrointestinal motility). The study was also carried out to facilitate the discovery of its putative mechanisms of action, which are thought to give diarrhea protection. The oral acute toxicity test, which used the mouse’s maximum dose of 2000 mg/kg body weight, was found to be safe. There was no mortality or visible behavioral or physical abnormalities, indicating that the extract’s median lethal dose (LD50) is larger than 2000 mg/kg.26
Castor oil is transformed into ricinoleic acid in the gut, which subsequently irritates, inflames, and releases inflammatory mediators including prostaglandins and histamine into the intestinal mucosa.39,40 The ensuing prostaglandin production promotes vasodilation, mucus secretion, and smooth muscle contraction in the small intestines.28 In the castor oil-induced diarrhea model, the hydromethanolic crude extract significantly (P< 0.001) delayed the onset of diarrhea and decreased the quantity and weight of wet and total feces. When compared to the negative control, the n-hexane fraction significantly reduced the quantity and weight of wet and total feces at 100 mg/kg (P<0.01), 200 mg/kg (P<0.001), and 400 mg/kg (P<0.001), and the ethyl acetate fraction also significantly delayed the onset of diarrhea and reduced the frequency of wet and total feces at 200 mg/kg (P<0.01) and 400 mg/kg (P<0.001), whereas the aqueous fraction significantly delayed the onset of diarrhea and reduced the number and weight of wet stools (P<0.01) at the highest dose.
Secondary metabolites are found in variable amounts in the crude extract and each solvent phase. So, these metabolites may be used to measure the level of anti-diarrheal impact of both the crude extract and each fraction by inhibiting the active secretion of ricinoleic acid and the release of prostaglandins, altering the activity of sodium-potassium ATPase or inhibiting chloride channel activation.25,32,33 The aqueous fraction exhibits the lowest anti-diarrheal activity. This could be explained by the aqueous solvent’s polyphenol oxidase enzyme breaking down the anti-diarrheal properties of polyphenols like tannins and flavonoids.41 The dose-dependent percentage inhibition of stool defecation by the hydromethanolic crude extract and each fraction could be attributed to biological elements responsible for this effect, which were shown to be more concentrated at higher tested doses.
In the enteropooling test the hydromethanolic crude extract considerably (P<0.001) reduced the average weight of intestinal fluid buildup when compared to the negative control at all doses tested. At all doses studied, the n-hexane and ethyl acetate fractions significantly (P<0.001) reduced the average weight of intestinal fluid buildup when compared to the vehicle control. The n-hexane fraction significantly (P<0.001) reduced the volume of intestinal contents at the middle and highest tested values when compared to the 100 mg/kg ethyl acetate fraction. At the medium and maximum doses, the aqueous fraction considerably (P<0.05) reduced the volume of intestinal fluid aggregation when compared to the vehicle-treated group.
The types and amounts of biological elements present in both the crude extract and each fraction could be the cause of these effects. These compounds inhibited fluid secretion by acting on various secretory pathways, resulting in either individual or synergistic antisecretory actions. For example, tannins, flavonoids, terpenoids, and alkaloids found in both the crude extract and the n-hexane fraction; saponins, flavonoids, and tannins found in the crude extract and ethyl acetate fraction; and terpenoids found in the crude extract and aqueous fraction could inhibit nitric oxide synthesis (since nitric oxide plays a role in the laxative effect of castor oil-induced diarrhea) and thus reduce fluid accumulation in the intestine.8,28,40,42–44 While tannins in the crude extract, n-hexane, and ethyl acetate fractions may reduce fluid secretion by inhibiting cystic fibrosis transmembrane conductance regulator or calcium-activated channels, aquaporins 2 and 3 expressions, and causing protein-precipitating reactions to the gastrointestinal mucosa.45–47 Flavonoids, unlike the aqueous fraction, may limit fluid secretion by blocking acetylcholine release48 and activating 2-adrenergic receptors in intestinal absorptive cells.49
In the gastrointestinal motility test, the crude extract significantly reduced (P<0.001) the propulsion of charcoal marker at all doses tested when compared to the negative control. Insolvent fractions, the n-hexane fraction significantly (P<0.001) decreased intestinal transit when compared to the vehicle-treated group. When compared to the 100 mg/kg dose of its fraction, the lowest and middle doses of the ethyl acetate fraction, and the negative control, this fraction statistically inhibited intestinal transit (P<0.001) at the highest dose, whereas the ethyl acetate fraction statistically inhibited intestinal transit at the middle (P<0.01) and highest (P<0.001) tested doses. It also decreased intestinal motility statistically (P<0.001) at 400 mg/kg when compared to the 100 mg/kg dose of its portion, whereas the aqueous fraction exhibited a significant (P<0.01) antispasmodic effect at the maximum dose when compared to the vehicle-treated control.
These effects could be owing to the presence of biological elements in both the hydromethanolic crude extract and each solvent fraction, as mentioned in the castor oil-induced diarrhea and enteropooling models. Flavonoids present in the crude extract, n-hexane, and ethyl acetate fractions could inhibit contractions induced by spasmogens,50 as well as the release of autacoids and prostaglandins,51 while tannins present in these extracts could have a similar effect by activating the calcium pumping system or by reducing the intracellular calcium concentration.35 Terpenoids found in the crude extract, as well as the aqueous and n-hexane fractions may help to mitigate castor oil’s altered propulsive movement. Additionally, tannins and flavonoids found in the hydromethanolic extract, ethyl acetate, and n-hexane fractions, as well as phenols found in all extracts, may prevent oxidation by transferring electrons to free radicals, blocking oxidases, or activating antioxidant enzymes.52,53 This effect supports the previous in vitro anti-oxidant21 study of the plant. Both the crude extract and each solvent fraction caused dose-dependent percentage inhibition of intestinal transit (Table 4). This could be because the crude extract and each solvent fraction had larger concentrations of biological components in the higher doses tested doses.
The combined effects of intestinal motility, delay in onset of diarrheal defecations, and purging frequency in the number of wet stools were the in vivo anti-diarrheal indices (ADI) of the crude extract as well as solvent fractions. The anti-diarrheal indices were dose-dependent manner in both the crude extract and solvent fractions(as shown in Figure 1). The root of Acacia seyal extract contains antisecretory and antimotility properties, according to this study. Furthermore, prior in vitro studies have shown that the root extract exhibits antibacterial activity against Klebsiella pneumonia, Bacillus subtilis,19 and Shigella sonnei.20 Therefore, Acacia seyal root extract can be a good choice for treating diarrhea brought on by a range of causes.
Conclusion
The findings of the present study demonstrated that the hydromethanolic crude extract as well as solvent fractions of Acacia seyal roots were found to have promising antidiarrheal properties in dose dependent manner. These antidiarrheal activities might be attributed to the presence of phytoconstituents in the Acacia seyal roots. Thus the findings of this study provide scientific proof for the folkloric use of Acacia seyal roots as a diarrhea management.
Data Sharing Statement
The dataset can be obtained/requested by sending an email or other kind of media to the relevant author.
Ethical Approval
The experimental protocols using laboratory animals were requested and approved by the Institutional Review Board, University of Gondar.
Acknowledgments
The study participants, as well as the University of Gondar, are acknowledged by the authors of this work.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The funding was requested and acquired from the University of Gondar after the proposal was prepared. The writers then completed all of the study’s tasks.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. World Health Organization. Diarrhoeal disease fact sheet. World Heal Organ Media Cent; 2017:1–4.
2. Ugboko HU, Nwinyi OC, Oranusi SU. Childhood diarrhoeal diseases in developing countries. Heliyon. 2020;6(4):1–10.
3. Guerrant RL, Van Gilder T, Steiner TS, et al. Practice guidelines for the management of infectious diarrhea. Clin Infect Dis. 2001;32(3):331–351. doi:10.1086/318514
4. Arasaradnam RPBS, Forbes A, Forbes A, et al. Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology. Gut. 2018;67:1380–1389. doi:10.1136/gutjnl-2017-315909
5. Walker CLF, Sack D, Black RE. Etiology of diarrhea in older children, adolescents and adults: a systematic review. PLoS Negl Trop Dis. 2010;4(8):1–8.
6. Li Y, Tian J. Evaluation of local anesthetic and antipyretic activities of Cinchona alkaloids in some animal models. Trop J Pharm Res. 2016;15(8):1663–1666. doi:10.4314/tjpr.v15i8.10
7. Shimelis D, Benti D, Challi D. Effect of zinc supplementation in treatment of acute diarrhea among 2–59 months children treated in Black Lion Hospital, Addis Ababa, Ethiopia. Ethiop J Health Dev. 2008;22(2):187–190.
8. Messaoudene D, Belguendouz H, Ahmedi ML, et al. Ex vivo effects of flavonoids extracted from Artemisia herba alba on cytokines and nitric oxide production in Algerian patients with Adamantiades-Behçet’s disease. J Inflamm. 2011;8(1):1–9. doi:10.1186/1476-9255-8-35
9. Abdel-Farid I, Sheded M, Mohamed E. Metabolomic profiling and antioxidant activity of some Acacia species. Saudi J Biol Sci. 2014;21(5):400–408. doi:10.1016/j.sjbs.2014.03.005
10. Bussmann RW, Paniagua-Zambrana NY, Njoroge GN. Acacia drepanolobium Harmes ex Sjostedt Acacia nilotica (L.) Willd. ex Delile Acacia senegal (L.) Willd. Acacia seyal Delille Acacia tortilis (Forssk.) Hayne F abaceae. Ethnobotany Mount Region Afr. 2021;2021:81–93.
11. Awad S, Rabah A, Ali H, Mahmoud T. Acacia Seyal Gums in Sudan: Ecology and Economic Contribution. Gum Arabic: Elsevier; 2018:3–11.
12. Mesfin F, Seta T, Assefa A. An ethnobotanical study of medicinal plants in Amaro Woreda, Ethiopia. Ethnobot Res Appl. 2014;12:341–354. doi:10.17348/era.12.0.341-354
13. Tefera BN, Kim Y-D. Ethnobotanical study of medicinal plants in the Hawassa Zuria District, Sidama zone, Southern Ethiopia. J Ethnobiol Ethnomed. 2019;15(1):1–21. doi:10.1186/s13002-019-0302-7
14. Esubalew ST, Belete A, Lulekal E, Gabriel T, Engidawork E, Asres K. Review of ethnobotanical and ethnopharmacological evidences of some Ethiopian medicinal plants traditionally used for the treatment of cancer. Ethiop J Health Dev. 2017;31(3):161–187.
15. Chekole G. Ethnobotanical study of medicinal plants used against human ailments in Gubalafto District, Northern Ethiopia. J Ethnobiol Ethnomed. 2017;13(1):1–29. doi:10.1186/s13002-017-0182-7
16. Bitew H, Gebregergs H, Tuem KB, Yeshak MY. Ethiopian medicinal plants traditionally used for wound treatment: a systematic review. Ethiop J Health Dev. 2019;33(2):1.
17. Gradé JT, Tabuti JR, Van Damme P. Ethnoveterinary knowledge in pastoral Karamoja, Uganda. J Ethnopharmacol. 2009;122(2):273–293. doi:10.1016/j.jep.2009.01.005
18. Magnini R, Hilou A, Compaore HM-K, Pagès J-M, Davin-Regli A. A Review on ethnobotanical uses, biological activities and phytochemical aspects of Acacia Senegal (L.) Willd. and Acacia seyal Delile. (Fabaceae). Int J Plant Sci Hortic. 2020;32–55. doi:10.36811/ijpsh.2020.110023
19. Eldeen I, Van Staden J. In vitro pharmacological investigation of extracts from some trees used in Sudanese traditional medicine. S Afr J Bot. 2007;73(3):435–440. doi:10.1016/j.sajb.2007.03.009
20. Mekbib SB. In vitro antimicrobial assay of selected medicinal plants against medically important plant and food-borne pathogens; 2016:163–169.
21. Elmi A, Spina R, Risler A, et al. Evaluation of antioxidant and antibacterial activities, cytotoxicity of acacia seyal del bark extracts and isolated compounds. Molecules. 2020;25(10):1–15. doi:10.3390/molecules25102392
22. Eldeen I, Van Staden J. Cyclooxygenase inhibition and antimycobacterial effects of extracts from Sudanese medicinal plants. S Afr J Bot. 2008;74(2):225–229. doi:10.1016/j.sajb.2007.11.009
23. Mwangi GG, Wagacha JM, Nguta JM, Mbaria JM. Brine shrimp cytotoxicity and antimalarial activity of plants traditionally used in treatment of malaria in Msambweni district. Pharm Biol. 2015;53(4):588–593. doi:10.3109/13880209.2014.935861
24. Shehu A, Anyip B, Magaji MG. Antidepressant effect of methanol root bark extract of Acacia seyal Del. (Fabaceae): possible involvement of the inflammatory pathway. Trop J Pharm Res. 2020;19(7):1459–1464. doi:10.4314/tjpr.v19i7.18
25. Umer S, Tekewe A, Kebede N. Antidiarrhoeal and antimicrobial activity of Calpurnia aurea leaf extract. BMC Complement Altern Med. 2013;13(1):1–5. doi:10.1186/1472-6882-13-21
26. Acute Oral Toxicity – Up-and-Down-Procedure (UDP). OECD 425 Guidelines for the Testing of Chemicals; 2008.
27. Ayal GBA, Kahaliw W. Evaluation of wound healing and anti-inflammatory activity of the leaves of Calpurnia aurea (Ait.) Benth (Fabaceae) in mice. Wound Med. 2019;25:1–9. doi:10.1016/j.wndm.2019.100151
28. Sarin RV, Narwal S, Bafna PA. Anti-diarrhoeal activity of aqueous extract of Ocimum kilimandscharicum. J Ethnopharmacol. 2013;148(1):223–228. doi:10.1016/j.jep.2013.03.083
29. Underwood W, Anthony R. AVMA guidelines for the euthanasia of animals: 2020 edition; 2020:2020–2021.
30. Yadav R, Agarwala M. Phytochemical analysis of some medicinal plants. J Phytol. 2011;3(12):10–14.
31. Dahiru D, Onubiyi J, Umaru HA. Phytochemical screening and antiulcerogenic effect of Moringa oleifera aqueous leaf extract. Afr J Tradit Complement Altern Med. 2006;3(3):70–75. doi:10.4314/ajtcam.v3i3.31167
32. Kota BP, Teoh AW, Roufogalis BD. Pharmacology of traditional herbal medicines and their active principles used in the treatment of peptic ulcer, diarrhoea and inflammatory bowel disease. New Adv Basic Clin Gastroenterol. 2012;14:297–310.
33. Kubacey TM, Haggag EG, El-Toumy SA, Ahmed AA, El-Ashmawy IM, Youns MM. Biological activity and flavonoids from Centaurea alexanderina leaf extract. J Pharm Res. 2012;5(6):3352–3361.
34. Council NR. Guide for the care and use of laboratory animals; 2010.
35. Bun -S-S, Ollivier E. Ethnobotanical study of medicinal plants used by K’Ho-Cil people for treatment of diarrhea in Lam Dong Province, Vietnam. J Herb Med. 2020;19:1–43.
36. Wansi L, Deumeni R, Kamani P, Sama F, Tchoumi T, Kuiate R. Antidiarrhoeal activity of aqueous and methanolic Alchornea laxiflora (Euphorbiaceae) leaves extracts in rats. J Med Plants Stud. 2017;5(1):205–211.
37. Parekh J, Chanda S. In-vitro antimicrobial activities of extracts of Launaea procumbens Roxb. (Labiateae), Vitis vinifera l. (Vitaceae) and Cyperus rotundus l. (Cyperaceae). Afr J Biomed Res. 2006;9(2):89–93.
38. Sarker SD, Latif Z, Gray AI. Natural Product Isolation. Springer; 2006:1–25.
39. Ammon H, Thomas P, Phillips S. Effects of oleic and ricinoleic acids on net jejunal water and electrolyte movement. Perfusion studies in man. J Clin Invest. 1974;53(2):374–379. doi:10.1172/JCI107569
40. Nwidu LL, Essien GE, Nwafor PA, Vilegas W. Antidiarrheal mechanism of Carpolobia lutea leaf fractions in rats. Pharm Biol. 2011;49(12):1249–1256. doi:10.3109/13880209.2011.589854
41. Tiwari P, Kumar B, Kaur M, Gurpreet-Kaur G, Kaur H. Phytochemical screening and extraction: a review. Int Pharm Sci. 2011;1(1):98–106.
42. Ishii R, Saito K, Horie M, Shibano T, Kitanako S, Amano F. Inhibitory effects of hydrolyzable tannins form Melastoma dodecandrum Lour. on nitric oxide production by a murine macrophage-like cell line, Raw264. 7, activated with lipopolysaccharide and interferon-γ. Biol Pharm Bull. 1999;22(6):647–653. doi:10.1248/bpb.22.647
43. Jang DS, Min H-Y, Jeong Y-H, Lee SK, Seo E-K. Di-and sesqui-terpenoids isolated from the pods of Sindora sumatrana and their potential to inhibit lipopolysaccharide-induced nitric oxide production. Arch Pharm Res. 2004;27(3):291–294. doi:10.1007/BF02980062
44. Kondo Y, Takano F, Hojo H. Inhibitory effect of bisbenzylisoquinoline alkaloids on nitric oxide production in activated macrophages. Biochem Pharmacol. 1993;46(11):1887–1892. doi:10.1016/0006-2952(93)90628-A
45. Högenauer C, Hammer HF, Krejs GJ, Reisinger C. Mechanisms and management of antibiotic-associated diarrhea. Clin Infect Dis. 1998;27(4):702–710. doi:10.1086/514958
46. Liu C, Zheng Y, Xu W, Wang H, Lin N. Rhubarb tannins extract inhibits the expression of aquaporins 2 and 3 in magnesium sulphate-induced diarrhoea model. Biomed Res Int. 2014;2014:1–14.
47. Hughes S, Higgs N, Turnberg L. Loperamide has antisecretory activity in the human jejunum in vivo. Gut. 1984;25(9):931–935. doi:10.1136/gut.25.9.931
48. Jahan S, Kar A, Das A, Chowdhury MAU, Islam MS, Hasanuzzaman M. Antidiarrheal and antimotility activities of stem bark extracts of annona reticulata Linn. in mice model. J Appl Life Sci Int. 2019;20(3):1–9. doi:10.9734/jalsi/2019/v20i330082
49. Di Carlo G, Autore G, Izzo A, et al. Inhibition of intestinal motility and secretion by flavonoids in mice and rats: structure-activity relationships. J Pharm Pharmacol. 1993;45(12):1054–1059. doi:10.1111/j.2042-7158.1993.tb07180.x
50. Akuodor G, Muazzam I, Usman-Idris M, et al. Evaluation of the antidiarrheal activity of methanol leaf extract of Bombax buonopozense in rats. Ibnosina J Med BS. 2011;3(1):15–20. doi:10.4103/1947-489X.210845
51. Pérez GS, Pérez GC, Zavala S. MA. A study of the antidiarrheal properties of Loeselia mexicana on mice and rats. Phytomedicine. 2005;12(9):670–674. doi:10.1016/j.phymed.2004.01.010
52. Ramde-Tiendrebeogo A, Moumouni AN. A comparative study of phytochemical profile and antioxidant activity of Sahelian plants used in the treatment of infectious diseases in northern part of Burkina Faso: acacia seyal Delile and Acacia tortilis (Forssk.) Hayne subsp. raddiana (Savi). J Pharmacogn Phytotherapy. 2019;11(3):74–79. doi:10.5897/JPP2019.0555
53. Prasad SK, Laloo D, Kumar R, Sahu AN, Hemalatha S. Antidiarrhoeal evaluation of rhizomes of Cryptocoryne spiralis Fisch. ex Wydler: antimotility and antisecretory effects. Indian J Exp Biol. 2014;52(2):139–146.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
