Back to Journals » Clinical Ophthalmology » Volume 18
Angle Kappa is Not Correlated with Patient-Reported Outcomes After Multifocal Lens Implantation
Authors Liu X, Hannan SJ, Schallhorn SC, Schallhorn JM
Received 28 November 2023
Accepted for publication 16 February 2024
Published 26 February 2024 Volume 2024:18 Pages 605—612
DOI https://doi.org/10.2147/OPTH.S452147
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xi Liu,1,2 Stephen J Hannan,3 Steven C Schallhorn,4,5 Julie M Schallhorn5,6
1Southwest Hospital/Southwest Eye Hospital, Third Military Medical University (Army Military Medical University), Chongqing, People’s Republic of China; 2Key Laboratory of Visual Damage and Regeneration & Restoration in Chongqing, Chongqing, People’s Republic of China; 3Optical Express, Glasgow, UK; 4Carl Zeiss Meditec, Dublin, CA, USA; 5Department of Ophthalmology, University of California, San Francisco, San Francisco, CA, USA; 6Francis I. Proctor Foundation, University of California United States, San Francisco, CA, USA
Correspondence: Julie M Schallhorn, Francis I. Proctor Foundation, University of California, 490 Illinois St, San Francisco, CA, USA, Tel +1 415-514-1922, Email [email protected]
Purpose: To examine the effect of preoperative angle kappa on patient-reported outcomes after multifocal lens placement during cataract surgery and determine if it is an effective measure for preoperative patients screening for multifocal lens placement.
Setting: Private refractive surgery clinics.
Design: Retrospective cohort study.
Methods: All patients undergoing bilateral cataract or refractive lens exchange surgery with a target of emmetropia between 2013 and 2017 at Optical Express (Glasgow, UK) with multifocal lens placement for whom preoperative angle kappa measurement and a postoperative month 1 patient-reported outcomes measures were available were included.
Results: A total of 1368 patients were identified. Median preoperative angle kappa was 0.41mm with an interquartile range of 0.30mm to 0.53mm. Preoperative angle kappa did not have a significant association with patient-reported satisfaction with vision (correlation coefficient 0.15, 95% confidence interval − 0.081 to 0.39, P = 0.20) nor with patient-reported photic phenomena (P > 0.09 for all comparisons). A receiver-operator characteristic analysis did not yield a viable cutoff predictive of patient-reported satisfaction.
Conclusion: Angle kappa was not predictive of patient-reported satisfaction in this study. This study did not find evidence that it should be used as a screening test for patients considering multifocal intraocular lens placement.
Keywords: angle kappa, multifocal intraocular lens, refractive lens exchange
Introduction
Angle kappa is defined as the angle of intersection between the nodal point of the eye and the visual axis and represents the amount of offset between the pupillary center and the visual axis. Larger values of angle kappa have been implicated in patient-reported photic phenomena and dissatisfaction after undergoing cataract surgery,1–3 although this association has not been held up universally.4,5 Previous authors have suggested an angle kappa cutoff of half the width of the central zone of the lens for implantation of a specific IOL.6,7
In this study, we explore the relationship between angle kappa, visual outcomes, and patient-reported outcomes in a population of patients undergoing surgery with presbyopia-correcting multifocal intraocular lenses. This analysis was constructed to determine if a relationship between patient-reported outcomes and angle kappa exists, and to explore the potential for developing a cutoff value for angle kappa that is predictive of patient-reported satisfaction.
Methods
This retrospective study was deemed exempt from full review by the Institutional Research Board at the University of California, San Francisco, because it used only retrospective, de-identified patient data. This study complies with the tenets of the Declaration of Helsinki. Informed consent to undergo refractive lens exchange or cataract surgery was obtained from all patients prior to surgery. As a part of informed consent, all patients agreed to use their de-identified data for research purposes and statistical analysis.
Preoperative refraction data, surgical data, and postoperative data at the 1-month visit of patients that underwent refractive lens exchange or cataract surgery with bilateral implantation of multifocal intraocular lens between January 2013 and December 2017 were extracted from Optical Express electronic database. These study dates were selected because, during this time period, all refractive surgery patients routinely underwent imaging with a wavefront aberrometer. Angle kappa was not calculated preoperatively, nor was it considered for preoperative patient selection.
Patients were included if they met the following criteria: received bilateral surgery during the study time frame with implantation of the same class of lens in each eye, had no history of preoperative corneal refractive surgery, absence of any ocular pathology other than refractive error and cataract, had preoperative aberrometer measurements that could be used to derive angle kappa, attended a postoperative month 1 follow-up exam, and completed a patient-reported outcomes questionnaire.8
Preoperative examination included detailed ophthalmic examination with manifest and cycloplegic refraction, uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), uncorrected near visual acuity (UNVA), slitlamp evaluation, dilated fundoscopy, autorefraction and tonometry (Tonoref II, Nidek Co. Ltd.), corneal topography (Pentacam, Oculus, Inc.), and wavefront aberration measurement (iDesign Advanced WaveScan System, Johnson & Johnson Vision Care, Inc, Santa Ana, CA). Distance visual acuity was measured at 3 m with a logarithmic acuity chart, and near reading acuity was measured at 40cm with a logarithmic reading card and recorded in Snellen distance equivalent.
Intraocular surgeries were performed either manually or with the assistance of a femtosecond laser (Catalys Precision Laser System, Johnson & Johnson Vision Care, Inc., Santa Ana, CA). Patients with greater than 1.5D of corneal astigmatism underwent placement of a toric lens. Patients with corneal astigmatism between 0.8 and <1.5D generally underwent placement of femtosecond limbal relaxing incisions. For all other patients, the main incision was made on the steep axis if possible. Postoperatively, patients were instructed to instill one drop of levofloxacin 0.5%, 4 times daily for 2 weeks, 1 drop of dexamethasone 0.1%, 4 times daily for 2 weeks, and one drop of ketorolac 0.5%, 4 times daily for one month.
Lens choice was driven by the desired range of postoperative near vision as well as preoperative corneal astigmatism. During the study time period, the Tecnis Multifocal platform was not available in toric models, so patients with corneal astigmatism >1.5D received either a Tecnis Symfony Toric (ZXTx, Johnson & Johnson Vision, Santa Ana, CA) or a Lentis MPlus Toric (Oculentis B.V., Arnhem, the Netherlands). The other lenses utilized were the Tecnis Multifocal 3.25 (Johnson&Johnson Vision), the ReSTor 2.5 ActiveFocus (Alcon, Ft. Worth, TX), and the Lentis MPlus (Oculentis B.V.).
As part of their routine clinical care, patients were asked to complete a patient-reported outcomes questionnaire at their preoperative, 1 month and 3 months postoperative follow-up visits.8 This questionnaire utilizes a 5-point scale to quantify patient-reported satisfaction with vision as well as difficulties with visual photic phenomena such as glare, halos, starbursts, and ghosting. Its use and content have been previously described.8 It was self-administered by the patient using a password protected and secure computer terminal in a private area of the clinic. The questionnaire responses were stored in the secured central database, which is compliant with ISO 27001 for information security management systems and the answers were not available to clinic personnel or the treating surgeon.
Patients received preoperative imaging with a Hartmann Shack wavefront aberrometer, either the WaveScan or the iDesign (both devices from Johnson & Johnson Vision, Santa Ana, CA). Both devices provide the x and y coordinates of the offset between the pupillary axis and the corneal apex. The chord length of this offset was calculated using the Pythagorean theorem. As angle kappa and chord length are used interchangeably in the refractive literature,9 the chord length is referred to as angle kappa in this manuscript.
Visual and patient demographics such as age are reported as the median with interquartile range as they did not follow a normal distribution. Patient-reported outcomes measures were analyzed on a per-patient basis. For angle kappa which might have different values for each eye, the data from the eye with the higher value were used in an attempt to magnify any potential significant association of angle kappa. A sensitivity analysis was conducted looking at the lower angle kappa value, which yielded near-identical effect levels. Binocular visual acuity was used in all patient-reported outcomes models. A linear regression model treating patient-reported photic phenomena and patient-reported satisfaction as continuous outcomes was constructed. In both models, a Bonferroni-Holm correction was applied for multiple comparisons, and thus a p value of less than 0.01 was considered significant.
A receiver-operator characteristic (ROC) curve was constructed to analyze the characteristics of the cutoff value of angle kappa in predicting patient-reported satisfaction. For the purposes of this analysis, patient-reported satisfaction was treated as a binary outcome, with patients reporting they were “Very Satisfied” or “Satisfied” treated as satisfied, and patients reporting “Neither Satisfied or Dissatisfied”, “Dissatisfied”, and “Very Dissatisfied” being treated as not satisfied.
Results
A total of 1368 patients were identified. Demographics and implanted lenses are available in Table 1. The median angle kappa value was 0.41mm, with an interquartile range (IQR) of 0.30mm to 0.53mm and a range of 0.02mm to 2.02mm (Figure 1A). There was, expectedly, a temporal displacement of the visual axis relative to the pupil center in left and right eyes (Figure 1B). Right eyes had, on average, a slightly higher angle kappa value than left eyes (median 0.44mm [IQR 0.32mm to 0.56mm] versus 0.37mm [IQR 0.29mm to 0.49mm], P < 0.001 by Mann–Whitney U-test).
 |
Table 1 Demographics and Lenses Implanted for the Study Population. Data is Presented as Median with Interquartile Range (IQR) Due to the Non-Gaussian Distribution |
 |
Figure 1 Histogram of angle kappa values in this population (A) and scatterplot (B) of the location of the offset of the corneal vertex from the pupil center for left and right eyes. |
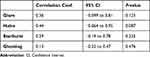
A linear regression model was constructed to analyze factors contributing to patient-reported satisfaction (Table 2). This did not demonstrate a relationship between angle kappa and patient-reported satisfaction. Binocular uncorrected distance visual acuity (correlation coefficient 0.069, 95% CI 0.019 to 0.12, P = 0.007) was the strongest association. A sensitivity analysis was conducted with separate models for patients receiving just one type of lens, but yielded similar effect estimates in each model (Table S1). This indicates that the influence of angle kappa does not depend on lens design.
As angle kappa has been suggested as a screening tool for patients receiving multifocal intraocular lenses, a receiver operator curve was constructed to examine the utility for defining a cutoff value for angle kappa to screen out patients with a higher likelihood of being dissatisfied after surgery (Figure 2). This curve plots the true-positive rate versus the false-positive rate of an ascending order of cutoff values. An ideal curve would yield a value with a high true positive rate and a low false-positive rate, whereas a test with no predictive value would trend close to the unity line where the true positive rate is the inverse of the false-positive rate. The curve for angle kappa trends close to the unity line, indicating that angle kappa has low utility for use as a screening test.
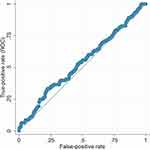 |
Figure 2 Receiver operator characteristic curve of angle kappa predictive of patient-reported satisfaction. |
A larger angle kappa has been suggested to be responsible for increased patient-reported photic phenomena, such as glare, halos, starbursts, and ghosting. An analysis was conducted to examine if there was a relationship between patient-reported photic phenomena and angle kappa (Table 3). No association was found between angle kappa and patient-reported photic phenomena.
To analyze for potential effects of loss to follow up, we studied the distribution of angle kappa and preoperative refractive error in this population versus the population of patients that underwent surgery during the same time period but did not complete a 1 month follow-up, did not undergo surgery in both eyes during the time period, who underwent surgery with a monofocal lens, or who did not fill out a patient-reported outcomes questionnaire. During this time period, a total of 6982 patients underwent surgery and had a preoperative angle kappa measurement available. The median angle kappa for the entire cohort was 0.41 (IQR 0.29 to 0.53), which did not differ from the study cohort (P = 0.9, Mann Whitney test). The manifest spherical equivalent (MSE) for the study population was slightly more hyperopic than for the overall population (mean +1.30±2.31D for the study population vs +1.18±2.39D for the overall population, P < 0.001).
Discussion
In this study of angle kappa in a large patient population undergoing bilateral surgery with multifocal lenses, we did not find an association between angle kappa and patient-reported satisfaction with vision or patient-reported photic phenomenon. Sensitivity analyses within patients receiving the same type of lens likewise did not demonstrate an association. A receiver-operator characteristic analysis did not reveal any utility in angle kappa as a screening characteristic to select patients that would be satisfied after surgery.
There have been a number of studies exploring the relationship between patient-reported outcomes measures and preoperative angle kappa in the clinical setting. Prakash, et al, reported in 2011 that increased angle kappa had a negative association with patient-reported photic phenomena and satisfaction in a cohort of 37 patients undergoing placement of a zonular refractive IOL (ReZoom IOL, no longer in manufacture).1 Fu, et al, demonstrated that a larger angle kappa was associated with decreased modulation transfer function and Strehl ratio in a cohort of patients receiving an extended depth of focus lens (Tecnis Symfony), but did not analyze its effects on patient satisfaction.3
Conversely, other authors have not reported an association between angle kappa and patient-reported satisfaction. Garzon, et al, did not find an association between angle kappa and patient-reported halos in a cohort receiving implantation of a trifocal IOL (PodF, PhysIOL, Liége, Belgium)4 A study of a rotationally asymmetric refractive multifocal lens (SBL-3, Lenstec, St. Petersburg, FL) by Liu, et al, found no influence of angle kappa on patient-reported outcomes, modulation transfer function, or the Strehl ratio.5
Decentration of a multifocal lens with respect to the visual axis has the potential to induce aberrations due to zones of diffractive or refractive change overlapping fixation.2 This has been demonstrated both theoretically in diffractive multifocal lenses and with an optical bench system with one type rotationally asymmetric segmented multifocal lenses.2,10 It is curious as to why we did not see an effect when there is the optical and theoretical potentials for there to be one.
A theoretical study by Karhanova, et al, proposed the concept of a critical angle kappa value for each type of diffractive multifocal lens.2 This critical value is theoretically dependent upon the effective lens position, diameter of the central optic, and keratometry in a non-linear relationship. The average critical angle kappa values that they described were quite high – between 10° and 15° depending on lens type, which corresponds to a chord length of 1 to 1.5mm in an average eye. A potential reason that we did not see an effect of angle kappa is that we might not have had a large enough number of patients with a substantially high angle kappa to show a difference. The distribution of angle kappa that we encountered in eyes in this study compares similarly to previously reported studies, so it is unlikely that we are studying a population that differs substantially from a population of normal patients seeking to undergo cataract surgery. We did not have many eyes in this study with very large angle kappa values (>1mm), so it is theoretically possible that such eyes may experience a decrease in visual quality. We did not find evidence of a step-off in patient-reported satisfaction or photic phenomena at any level of angle kappa in this cohort.
Karhanova et al recommended taking care when implanting multifocal lenses in hyperopic eyes due to a potentially shallow effective lens position, which reduces the critical angle kappa.2 We unfortunately do not have postoperative effective lens position data to study this effect, but the cohort of patients in this study was overwhelmingly hyperopic (86% of patients had a hyperopic preoperative manifest spherical equivalent). Our failure to find an association between angle kappa and patient-reported satisfaction indicates that angle kappa is unlikely to be a substantial factor in the hyperopic population.
Angle kappa has been shown to diminish after cataract surgery.11 In this study, we only had preoperative angle kappa measurements, and it is possible that the decrease is such that it renders any potential effects from a larger angle kappa preoperatively insignificant. However, we think this is unlikely given the reported magnitude of change (0.04mm in chord length), which is small compared to the median preoperative chord length 0f 0.41mm in this population.
This study has several limitations. First, it is retrospective and as such is subject to loss to follow-up bias. A sensitivity analysis revealed that the patients included in this study had similar baseline angle kappa and preoperative refraction to patients who did not complete a patient-reported outcomes questionnaire. This indicates that our variable of interest, angle kappa, did not influence patient follow-up. The study population was slightly more hyperopic than the entire population, but this would theoretically have the effect of increasing any effect of angle kappa per the model in Karhanova et al.2 Additionally, we recently analyzed risk factors and potential for bias in follow-up and completion of patient-reported outcomes questionnaires in patients undergoing laser vision correction and found that patients with worse visual outcomes were more likely to both follow-up and complete a questionnaire.12 If this were to have happened in our population, the effect would have been to bias our population toward greater degrees of dissatisfaction and thus amplify the effects of any factors contributing to this. Thus, we believe it is unlikely that loss to follow-up would have obscured an effect of angle kappa in this population.
An additional drawback is that we did not use a validated questionnaire in our study. Unfortunately, there are no currently available validated questionnaires for studying patient-reported outcomes in patients receiving multifocal intraocular lenses. Our questionnaire is based on one validated for use in laser vision correction, but not multifocal lens surgery.
Overall, our analysis of angle kappa in this large patient cohort with multiple designs of multifocal lenses indicates broadly that angle kappa is not related to patient-reported visual or photic outcomes in this population. Although there might be theoretical effects of lens decentration on visual quality, we are not able to detect this in a systematic way such that angle kappa should be used as a screening tool for patients’ candidacy for multifocal lens placement.
Funding
The Department of Ophthalmology at the University of California, San Francisco, is supported by an unrestricted educational grant from Research to Prevent Blindness, as well as a departmental Core Grant for Vision Research, NIH-NEI EY002162.
Disclosure
Hannan, SJ: Employee of Optical Express. Schallhorn, SC: Chief Medical Officer of Carl Zeiss, Meditec. He is also on the Medical Advisor Board of Optical Express. Schallhorn, JM: Consultant for Carl Zeiss, Meditec, Allergan, Neurotrigger, Forsight V6. Equity in Longbridge Medical, Novus Vision, Journey 1. The authors report no other conflicts of interest in this work.
References
1. Prakash G, Prakash DR, Agarwal A, Kumar DA, Agarwal A, Jacob S. Predictive factor and kappa angle analysis for visual satisfactions in patients with multifocal IOL implantation. Eye. 2011;25(9):1187–1193. doi:10.1038/eye.2011.150
2. Karhanová M, Pluháček F, Mlčák P, Vláčil O, Šín M, Marešová K. The importance of angle kappa evaluation for implantation of diffractive multifocal intra-ocular lenses using pseudophakic eye model. Acta Ophthalmol. 2015;93(2):e123–8. doi:10.1111/aos.12521
3. Fu Y, Kou J, Chen D, et al. Influence of angle kappa and angle alpha on visual quality after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2019;45(9):1258–1264. doi:10.1016/j.jcrs.2019.04.003
4. Garzón N, García-Montero M, López-Artero E, et al. Influence of angle κ on visual and refractive outcomes after implantation of a diffractive trifocal intraocular lens. J Cataract Refract Surg. 2020;46(5):721–727. doi:10.1097/j.jcrs.0000000000000156
5. Liu Y, Gao Y, Liu R, et al. Influence of angle kappa-customized implantation of rotationally asymmetric multifocal intraocular lens on visual quality and patient satisfaction. Acta Ophthalmol. 2020;98(6):e734–e742. doi:10.1111/aos.14356
6. Moshirfar M, Hoggan RN, Muthappan V. Angle Kappa and its importance in refractive surgery. Oman J Ophthalmol. 2013;6(3):151–158. doi:10.4103/0974-620x.122268
7. Berdahl J, Waring GOI. Match right lens to patient needs: 10 objective measurements can improve multifocal IOL implantation outcomes [monograph on the internet]. Ophthalmol Times. 2012;2012:28–29.
8. Schallhorn SC, Hettinger KA, Teenan D, Venter JA, Hannan SJ, Schallhorn JM. Predictors of patient satisfaction after refractive lens exchange with an extended depth of focus IOL. J Refract Surg. 2020;36(3):175–184. doi:10.3928/1081597x-20200211-01
9. Chang DH, Waring GO. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol. 2014;158(5):863–874. doi:10.1016/j.ajo.2014.06.028
10. Bonaque-González S, Jaskulski MT, Carmona-Ballester D, Pareja-Ríos A, Trujillo-Sevilla JM. Influence of angle Kappa on the optimal intraocular orientation of asymmetric multifocal intraocular lenses. J Optom. 2021;14(1):78–85. doi:10.1016/j.optom.2020.07.004
11. Wang R, Long T, Gu X, Ma T. Changes in angle kappa and angle alpha before and after cataract surgery. J Cataract Refract Surg. 2020;46(3):365–371. doi:10.1097/j.jcrs.0000000000000063
12. Schallhorn JM, Schallhorn SC, Hannan SJ. Impact of refractive outcomes on bias in follow up and completion of patient-reported outcomes measures after laser vision correction. Ophthalmology. 2021;128:1284–1291. doi:10.1016/j.ophtha.2021.01.030
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.