Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Analysis of Traditional Chinese Medicine Symptoms in Children with Spastic Cerebral Palsy: A Data Mining Study
Authors Wang X , Pang F, Du XG
Received 25 November 2023
Accepted for publication 26 February 2024
Published 1 March 2024 Volume 2024:17 Pages 913—922
DOI https://doi.org/10.2147/JMDH.S451768
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xing Wang,1,2 Fang Pang,3 Xiao-Gang Du2
1M. Kandiah Faculty of Medicine and Health Sciences, Universiti Tunku Abdul Rahman, Kajang, Selangor, Malaysia; 2Famous TCM Expert Heritage Studio, Xi’an Encephalopathy Hospital Affiliated to Shaanxi University of Chinese Medicine, Xi’an, Shaanxi, People’s Republic of China; 3Institute of Sports Biology, Shaanxi Normal University, Xi’an, Shaanxi, People’s Republic of China
Correspondence: Xiao-Gang Du, Famous TCM Expert Heritage Studio, Xi’an Encephalopathy Hospital Affiliated to Shaanxi University of Chinese Medicine, Xi’an, Shaanxi, People’s Republic of China, Email [email protected]
Background: Cerebral palsy (CP) ranks as a major cause of motor disabilities in children, with spastic CP making up roughly 70– 80% of all CP cases. The primary objective of our study is to identify characteristics of Traditional Chinese Medicine(TCM) symptom of spastic CP, thereby establishing correlations between the TCM symptom and the disease, providing a more scientific theoretical foundation for TCM treatments on spastic CP, enabling a deeper comprehension of clinical interventions, ultimately, improving rehabilitation outcomes in TCM treatment for spastic CP.
Methods: We conducted a data mining study on TCM symptom of spastic CP children aged 4– 14 years old treated at Xi’an Encephalopathy Hospital Affiliated to Shaanxi University of Chinese Medicine, from October 2021 to March 2023. The medical records of all eligible and complete spastic CP patients were extracted, processed for data cleansing, transformed, and subsequently analyzed to discern distinctive TCM symptom. K-Means Clustering Analysis and Association Rule Analysis were used for data mining.
Results: Core symptoms identified for spastic CP encompassed “Motor Dysfunction”, “Impaired Speech”, “Delayed Development”, “Limb Stiffness”, “Rigidity in the limbs”, “Intellectual Impairment”, “Timidity and susceptibility to startle responses”, “Muscle Wasting”, and “Pale or Dull Complexion”. Among the top-ranking associations of symptom, patterns emerge wherein “Motor dysfunction” intertwine with “Impaired speech”, “Motor dysfunction” coexist with “Delayed development”, and “Impaired speech” are accompanied by “Delayed development”.
Conclusion: This study identified the core symptom of spastic CP and tentatively suggests that the clinical manifestations of spastic CP are essentially consistent with the TCM pattern “liver exuberance and spleen weakness”. This finding has facilitated the preliminary establishment of correlations between TCM pattern differentiation and the disease in medicine. It is anticipated that this correlation will bring tangible benefits to a larger number of children with spastic CP.
Keywords: spastic cerebral palsy, TCM symptom, data mining, R language
Cerebral palsy (CP) ranks as a major cause of motor disabilities in children,1 with spastic CP making up roughly 70–80% of all CP cases.2 Its identification often occurs during the early stages of life.3 The majority of cases of spastic cerebral palsy stem from perinatal or early postnatal brain injuries.4 Factors such as hypoxia, birth trauma, preterm birth, and low birth weight may contribute to abnormal brain development, culminating in impairments in motor control and coordination.5 Clinical manifestations of this condition encompass muscular spasms, motor impairments, and neurological dysfunctions.6 Its profound impact significantly disrupts the daily lives and overall functionality of those affected, causing notable distress and limitations to their quality of life. Despite some medical interventions available, such as physical therapy,7 medication treatment,8 surgical interventions,9 nutrition interventions10 and assistive devices,11 a comprehensive and universally effective solution is currently lacking. Consequently, some patients continue to encounter persistent challenges and disruptions in their treatment.
Traditional Chinese Medicine (TCM), as a time-honored medical system rich in experiential knowledge, offers unique perspectives and methodologies for treating neurological disorders.12 Particularly, in addressing symptom like muscular spasms13 and neurological impairments,14 TCM employs widely practiced therapies such as acupuncture and herbal medicine. However, the specific selection of TCM treatments often relies on the clinical expertise and individual experience of practitioners, resulting in uncertainties regarding clinical efficacy and safety.15 “TCM Symptoms” as a comprehensive term encompassing a series of symptoms within the framework of TCM. This includes the overall manifestations of the body during the disease process, as perceived through the Four Diagnoses (Observation, Olfaction and Auscultation, Inquiry, and Palpation). Therefore, adhering to the fundamental principles of differentiation and treatment in TCM, there arises a necessity to scientifically understand the characteristic of TCM symptom in spastic CP, thereby consolidating the theoretical foundation of TCM treatment. Enhancing the potential value of TCM treatment on spastic CP becomes profoundly imperative in this context.
In the realm of TCM data mining, R language assumes as an important role due to its capabilities in data analysis and processing.16,17 It brings researchers with effective tools facilitating the profound exploration of latent information within clinical data, thereby furnishing scientific guidance for both TCM clinical practice and research. According to the theory of TCM, we assumed that there must be definite rules between the symptoms of spastic CP. This study use R language to analysis clinical data to identify characteristics of TCM symptom of spastic CP, thereby establishing correlations between the TCM symptom characteristics and the disease in medicine, providing a more scientific theoretical foundation for TCM treatments on spastic CP, enabling a deeper comprehension of clinical interventions, ultimately, improving rehabilitation outcomes in TCM treatment for spastic CP.
Methods and Analysis
Design of the Study
We conducted a data mining study on TCM symptom of spastic CP children aged 4–14 years old treated at Xi’an Encephalopathy Hospital Affiliated to Shaanxi University of Chinese Medicine, from October 2021 to March 2023. In order to ensure the accuracy of the data analysis, a sufficient sample size was sought. Adhering to the principle of comprehensive inclusion, initially, 265 medical records were considered. Among these, 20 cases did not meet the inclusion criteria, and 14 had incomplete information, resulting in the final inclusion of 231 cases for analysis. Ethical approval for this study (Approval No. XN2023-13) was obtained from the hospital’s ethics committee. The study protocol with more information was published on October 25, 2023,18 maintaining the core aspects of the research design while adjusting certain research details, such as utilizing the R language for cluster analysis and association rule analysis. The specific flowchart of the research process is depicted as Figure 1.
 |
Figure 1 The flowchart of the TCM symptom analysis study. |
Review Process
Data Screening
Inclusion criteria for medical records included: (1) The age range of children is between 4 and 14 years old. (2) The diagnosis confirmed spastic CP, with diagnostic criteria determined by the committee members outlined in the “Chinese Guidelines for Rehabilitation and Treatment of Cerebral Palsy ”19 (3) Admission information was completion, encompassing demographic details of the patients and completeness of critical elements within the medical records. Simultaneously, the medical records were required to include essential components such as chief complaints and present symptom in the admission notes. (4) Detailed records of TCM symptom and tongue-pulse symptom. (5) Patients did not have severe organic diseases affecting vital organs such as the heart, liver, or kidneys.
Principle of Data Normalization Processing
The process of standardizing TCM symptom data for spastic CP involves adherence to the following principles:20,21 (1) Rationality: Entities, characteristics, concepts, and relationships within clinical diagnostic data, even after standardization, should still align with their specific contextual meaning. (2) Accuracy: Standardization of clinical data into standardized terminologies should accurately reflect the original meaning of the data. (3) Consistency: Synonyms or different terms for the same concept should be standardized into a unified terminology. (4) Completeness: Refers to ensuring that standardized terminologies (words or phrases) maintain semantic integrity as much as possible without losing their original significant meaning after standardization.
Database Establishment
We extracted diagnostic and therapeutic information of spastic CP children pertinent to our study from the hospital’s medical records system through the medical information department. Subsequently, this data was transformed into an Excel file using a binary data conversion method. In this transformation, patients exhibiting a specific symptom were denoted as “1”, while those not exhibiting the symptom were marked as “0” in the file. This transform rule aimed to facilitate subsequent statistical analyses. Following the completion of all conversions, a senior-level physician verified and cross-checked the information for accuracy.
Data Entry Requirements
Ensuring accuracy and maintaining a record of corrections are very important when inputting information of children in Excel. Prior to data entry, meticulous scrutiny of the file’s structure is essential to confirm accurate field correspondence, absence of omissions, and avoidance of duplications. During data entry, if corrections are necessary, it is advised not to modify the original data directly. Instead, create a new column or worksheet specifically designated for recording corrected data. In this new column, it’s recommended to annotate the reason for correction, date, and the operator’s details to guarantee transparency and traceability of the data corrections. Additionally, before making any alterations, ensure the creation of a backup by duplicating the original dataset. Regular review and validation of the data are imperative.
Statistical Methods
Descriptive analysis was conducted using SPSS 22.0. K-Means Clustering analysis is employed to partition the observations in TCM symptoms into a predetermined number (k) of clusters, grouping together similar observations. Association Rule Analysis is employed to discover association relationships or patterns among Traditional Chinese Medicine symptoms. They were performed utilizing the R language tool. The “clusGap” function was employed to estimate the optimal number of clusters. Packages such as “pheatmap”, “arules”, “arulesViz”, and “RColorBrewer” in R were selected for data processing. The apriori algorithm was applied for association rule operations, initially setting the support at 0.05 and confidence at 0.8, with adjustments made based on research requirements. Visualization of the data was executed using plotting tools within the R language.
Results
Demographic Information
Among the 231 cases of spastic CP included in this study, there were 128 males (55.41%) and 103 females (44.59%). Urban patients accounted for 122 cases (52.84%), while rural patients accounted for 109 cases (47.16%). The most concentrated age distribution was observed at 4 years old with 42 cases (41.35%), followed by 5 years old (40.35%), and 26 cases at 8 years old (11.26%). The age groups with the smallest proportions were 13 and 14 years old, each with only 9 cases (3.90%). Concerning the disease course, the incidence was most concentrated between 12 to 24 months, totaling 70 cases (30.30%), while the least occurred within a 3-month span, comprising 25 cases (11.65%). Detailed data are presented in Table 1
 |
Table 1 Demographic Information of Included Patients |
Top TCM Symptom in Spastic CP Patients
Upon conducting analysis of TCM symptom within the patient included in the study, particularly focusing on the top 30 symptom. The majority of these children presented with similar symptom of “Motor dysfunction”, “Impaired speech”, “Delayed development”, and ‘Limb stiffness’. Furthermore, exceeding 120 children exhibited a wide spectrum of TCM symptom and tongue-pulse characteristics. These encompassed features such as “Thin and white tongue coating”, ‘Rigidity in the limbs’, a tongue named “Pale red tongue”, a pulse named “Rapid and thready”, “Intellectual impairment”, ‘Stiff neck, and “Light fingerprint patterns”. Additionally, over 90 children displayed clinical features including “Timid and easily startled”, “Muscle wasting”, “Stunted growth”, “Dull expression”, “Delayed response”, “Fatigue and weakness”, “Phlegm rales in the throat”, “Susceptibility to colds”, “Cyanosis of the fingertips”, “Spontaneous perspiration”, “Frequent and clear urination”, “Poor appetite”, “Diarrhea”, “Restlessness and insomnia”, “Slow movement of limbs”, “Dry and brittle hair”. Notably, clinical symptom of “Irritability and easy anger”, “Pale or dull complexion” were also relatively common, each being observed in over 80 children. For an even more detailed data of these findings can be seen in Table 2.
 |
Table 2 High-Frequency Distribution of TCM Symptom in Spastic CP Patients |
Cluster Analysis results of the High-Frequency TCM Symptom on Spastic CP Patients
We conducted a cluster analysis focusing on the top 30 symptom. To determine the optimal number of clusters, we employed the “clusGap()” function, resulting in a peak at four clusters, indicating the most suitable clustering solution, as represented in Figure 2. Subsequently, we performed a cluster analysis encompassing TCM symptom in the children with spastic CP. Employing the “pheatmap()” function. The clusters included: (1) “Motor Dysfunction”, “Impaired speech”, “Delayed development”, “Limb stiffness”, “Rigidity in the limbs”, “Intellectual impairment”, “Timid and easily startled”, “Muscle wasting”, and “Pale or dull complexion”, was identified as the core set of symptom associated with this spastic CP patients. Additionally, these individuals typically exhibited a tongue with “Thin and white tongue coating”, “Pale red tongue”, and a “Rapid and thready pulse”. (2) “Irritability and easy anger”, “Dull expression”, “Restlessness and insomnia”, “Drooling”, “Delayed response”, “Spontaneous sweating”, and “Cyanosis of the fingertips”. (3)“Poor appetite”, “Dry and brittle hair” “Slow Movement of limbs”, “Light fingerprints”, “Phlegm rales in the throat”, “Frequent clear urination”, and “Diarrhea”. (4)“Stunted growth”, “Stiff neck”, “Susceptibility to colds”, and a persistent state of “Fatigue and weakness”. Notably, as demonstrated in Figure 3. Within these clusters, the first group stands out as the core TCM symptom commonly associated with spastic CP children, while other clusters encompass non-core TCM symptom.
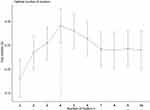 |
Figure 2 The result of optimal cluster number. |
 |
Figure 3 The cluster analysis result of TCM symptom in spastic CP patients. |
Association Rule Analysis Results of the High-Frequency TCM Symptom on Spastic CP Patients
We conducted an association rule analysis, focusing on the 30 top TCM symptom among the children with spastic CP. Our approach involved setting a minimum support threshold at 0.1 and a minimum confidence threshold at 0.8, which effectively guided the entire association rule analysis process. “Motor dysfunction” had a strong association with the TCM symptom of “Impaired speech” and “Delayed development”. Similarly, “Delayed development” had a strong link with “Impaired speech” and “Limb stiffness”, reaffirming the symbiotic nature of these symptom. Notably, “Impaired speech” and “Delayed development” “Limb stiffness” and “Impaired speech”, as well as “Delayed development” and “Limb stiffness”, collectively shaped the fundamental symptom that individuals with spastic CP. Our findings shed light on “Thin and white tongue coating” as the most prevalent tongue and pulse symptom among individuals with spastic CP. Simultaneously, “Pale or dull complexion” is the most common facial feature among spastic CP patients. This is similar as the diagnosis of the syndrome pattern characterized by liver exuberant and spleen weakness adds further credence to these findings. We ranked and analyzed the top 20 contributing association rules within our research, which is presented in Table 3.
 |
Table 3 Association Rules for High-Frequency TCM Symptom in Spastic CP Patients |
Discussion
CP is generally considered to fall within the scope of TCM ‘s “Five Chi, Five Ruan, and Five Ying”, often related to congenital insufficiency or improper postnatal nurturing.22 The disorder is thought to involve disharmony in organs such as the liver, spleen, and kidneys.23 However, the diagnosis and treatment of TCM are often a dynamic and personalized process.24 TCM practitioners approach treatment through a holistic lens, aiming to restore balance of qi blood, and yin yang in the body. But different academic system and professional orientations can lead to varying syndrome differentiation conclusions, such as organ-based differentiation(Zang Fu), defense-qi nutrient, and blood differentiation(Wei Qi Ying Xue), six meridian differentiation(Liu Jing), and three-Jiao differentiation.25,26 This rich tapestry of theories enriches the scope of clinical diagnosis and treatment in TCM but also poses challenges in organizing, summarizing, communicating, and learning knowledge of diagnosis and treatment in TCM. Therefore, this study does not use TCM syndrome types as the classification basis for children with CP. Instead, it chooses spastic CP diagnosed in Western medicine as the inclusion criteria for the study. Through the integration of data mining techniques, evidence-based medicine theory, computer technology, and TCM theory, it explores the characteristics of TCM symptom in the included children diagnosed with spastic CP. It aims to summarizes the clinical symptom of the corresponding population, understands their clinical differentiation patterns, and ultimately provides guidance and standardization for clinical TCM intervention for this disease.
Syndrome differentiation and treatment(SDT)27,28 is one of the fundamental therapeutic principles in TCM. It entails TCM practitioners continuously collecting experiences from effective medical cases of predecessors and their own practice. By aggregating these experiences, TCM practitioners identify common symptom, contemplate shared pathogenic mechanisms, and summarize effective treatment methods and prescriptions. Building upon this knowledge, practitioners then apply these identified patterns to clinical practice and continually validate the reliability of the derived principles through ongoing clinical verification and validation. The significance of SDT transcends theoretical understanding—it is deeply rooted in pragmatic clinical application. TCM practitioners implement these principles in the tailoring treatments to individual patients. Through continuous application and validation in clinical scenarios, practitioners not only reaffirm the efficacy of identified patterns but also contribute to the evolution and expansion of the vast tapestry of TCM knowledge.29,30
This study focused on exploring TCM symptom distribution in children with spastic CP. A comprehensive analysis was carried out on 231 medical records, involving data extraction, cleansing, mining, and summarization. The study revealed prevalent TCM symptom shared among the majority of patients with spastic CP, typified by “Motor dysfunction”, “Impaired speech”, “Delayed development”, and “Limb stiffness”. Furthermore, over half of the patients exhibited similar symptom such as “Thin and white tongue coating”, “Rigidity in the limbs”, “Intellectual impairment”, “Stiff neck”, and “Light fingerprints” with “Pale red tongue” and “Rapid and thready pulse”, which shed light on specific TCM patterns observed in both tongue and pulse manifestations, contributing valuable insights into the diagnostic and therapeutic approaches for spastic CP within the realm of TCM. The study provides a foundational understanding to aid further research and to refine tailored treatments for affected individuals, potentially improving their overall quality of life.
Among the top-ranking associations of symptom, patterns emerge wherein “Motor dysfunction” intertwine with “Impaired speech”, “Motor dysfunction” coexist with “Delayed development”, and “Impaired speech” are accompanied by “Delayed development”. These association rules provide critical insights into the intricate interplay of symptom,31 allowing for a more nuanced understanding of the spastic CP. Upon analysis of clustering and high-frequency TCM symptom, a central framework of core symptom for children diagnosed with spastic CP materializes. This foundational framework comprises important symptom like “Motor Dysfunction”, “Impaired speech”, “Delayed development”, “Limb stiffness”, “Rigidity in the limbs”, “Intellectual impairment”, “Timid and easily startled”, “Muscle wasting”, and “Pale or dull complexion”. These core symptoms encapsulate the key clinical manifestations that define spastic CP in the context of TCM. In addition to the core symptom, there exist non-core symptom that, while noteworthy, do not hold the same level of important in characterizing spastic CP. These include manifestations such as “Irritability and easy anger”, “Dull expression”, “Restlessness and insomnia”, “Drooling”, “Delayed response”, “Spontaneous sweating”, “Cyanosis of the fingertips”, “Poor appetite”, “Dry and brittle hair” “Slow Movement of limbs”, “Light fingerprints”, “Phlegm rales in the throat”, “Frequent clear urination”, “Diarrhea”, “Stunted growth”, “Stiff neck”, “Susceptibility to colds”, and a persistent state of “Fatigue and weakness”. Although these non-core symptoms provide valuable clinical insights into the overall health and state of the individual with CP, they are not as pivotal as the core symptom in characterizing the condition. By addressing the core symptom that play a central role in spastic CP, TCM practitioners can give treatment method that encompass a holistic approach striving for enhanced therapeutic outcomes and improved quality of life for affected individuals. This statement aligns with both the TCM knowledge and adheres to the scientific achievements of data mining technology.
Based on the core and non-core symptom observed in the study, the TCM perspective attributes the pathogenesis of these symptom to an exuberant of liver Qi, weakness in spleen Qi, and the dominant and overpowering nature of liver Qi over the weaker spleen. This categorization aligns with TCM syndrome differentiation as the “liver exuberant and spleen weakness” pattern.32 In TCM theory, the liver is believed to govern the body’s tendons and fascia,33 playing a vital role in storing and regulating blood.34 On the other hand, the spleen is responsible for managing the body’s muscles, controlling the processes of digestion and absorption, and serving as the fundamental source for Qi and blood generation.35 When the liver exerts dominance and overpowers the spleen, especially when the spleen is weak, its functionality diminishes.36 This weakening leads to compromised digestion and absorption processes, resulting in a deficiency of Qi and blood generation. Consequently, insufficient blood storage in the liver and its impaired ability to regulate blood volume lead to the muscles losing their nourishment from Qi and blood. This deficiency manifests as stiffness in the limbs, neck rigidity, and difficulty in swallowing, often referred to as the “internal wind” phenomenon or the “five Ying” concept in TCM, characterized by involuntary muscle spasms and rigidity. When the child’s limbs are stimulated, the muscle spasms intensify. Hence, by addressing the imbalance and strengthening the spleen while regulating liver Qi, practitioners possibility could restore balance in the body, ultimately ameliorating the symptom and enhancing the overall well-being of children with spastic CP.
Conclusion
This research employed an interdisciplinary methodologies, integrating data mining techniques, evidence-based medicine, computer technology, big data mining, and TCM. The comprehensive approach was aimed at conducting an in-depth investigation of medical records to explore and understand the TCM symptom prevalent in patients with spastic CP. This study identified the core symptom of spastic CP and tentatively suggests that the clinical manifestations of spastic CP are essentially consistent with the TCM pattern “liver exuberance and spleen weakness”. This finding has facilitated the preliminary establishment of correlations between TCM pattern differentiation and the disease in medicine. It is anticipated that this correlation will bring tangible benefits to a larger number of children with spastic CP. However, it’s important to acknowledge the limitations of this study, which primarily stem from the constraints of individual resources. Only 231 cases of spastic CP were included for analysis. Considering that spastic CP is not a common condition, we still believe that the study results hold valuable insights and merit consideration. Looking ahead, more data mining study and clinical interventional research in the subsequent phase, built upon the insights derived from this study, is expected to bring tangible benefits to a larger number of children grappling with spastic CP.
Consent to Participate
As a data mining study, it did not include any individual patient details. So, the ethics committee allowed it without needing parental consent. Still, the study strictly followed all principles of the Declaration of Helsinki.
Patient and Public Involvement
This study did not involve patients and/or the public in its design, implementation, reporting, or dissemination strategies.
Funding
The construction project of the National Famous Senior TCM Experts Heritage Studio of Hujie Song and Construction Project of “Sanqin” Scholar TCM Encephalopathy Innovation Team, Shaanxi Province.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sadowska M, Sarecka-Hujar B, Kopyta I. Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. 2020;16:1505. doi:10.2147/NDT.S235165
2. Ali A, Yalçın R, Ünlüer-Gümüştaş A. Cranial MR characteristics of Cerebral Palsy cases and correlation of findings with clinical results. Turk J Pediatr. 2019;61(4):525–537. doi:10.24953/turkjped.2019.04.009
3. Patel DR, Neelakantan M, Pandher K, Merrick J. Cerebral palsy in children: a clinical overview. Transl Pediatr. 2020;9(l 1):S125. doi:10.21037/tp.2020.01.01
4. Paul S, Nahar A, Bhagawati M, Kunwar AJ. A review on recent advances of cerebral palsy. Oxid Med Cell Long. 2022. doi:10.1155/2022/2622310
5. Abd Elmagid DS, Magdy H. Evaluation of risk factors for cerebral palsy. Egypt J Neurol Psychiatry Neurosurg. 2021;57:1–9. doi:10.1186/s41983-020-00265-1
6. Vitrikas K, Dalton H, Breish D. Cerebral palsy: an overview. Am Family Phys. 2020;101(4):213–220.
7. Apolo-Arenas MD, Jerônimo A, Caña-Pino A, Fernandes O, Alegrete J, Parraca JA. Standardized outcomes measures in physical therapy practice for treatment and rehabilitation of cerebral palsy: a systematic Review. J Pers Med. 2021;11(7):604. doi:10.3390/jpm11070604
8. Lumsden DE, Crowe B, Basu A, et al. Pharmacological management of abnormal tone and movement in cerebral palsy. Arch Dischildhood. 2019;104(8):775–780. doi:10.1136/archdischild-2018-316309
9. Tranchida GV, Van Heest A. Preferred options and evidence for upper limb surgery for spasticity in cerebral palsy, stroke, and brain injury. J Hand Surg. 2020;45(1):34–42. doi:10.1177/1753193419878973
10. Jahan I, Sultana R, Muhit M, et al. Nutrition interventions for children with cerebral palsy in low-and middle-income countries: a scoping review. Nutrients. 2022;14(6):1211. doi:10.3390/nu14061211
11. Bolton M, Donohoe M. Ambulatory assistive devices for children and youth with cerebral palsy. Cerebral Palsy. 2020;2963–2975.
12. Deng Z, Kan Y, Li M, Song J, Lu J-H. assessing the pharmacological effects and therapeutic potential of traditional Chinese medicine in neurological disease models: an update. Front Pharmacol. 2022;13:909153. doi:10.3389/fphar.2022.909153
13. Zhu Y, Yang Y, Li J. Does acupuncture help patients with spasticity? A narrative review. Annals of Physical Rehabilitation Medicine. 2019;62(4):297–301. doi:10.1016/j.rehab.2018.09.010
14. Zhou D, Xie L, Wang Y, et al. Clinical efficacy of tonic traditional Chinese medicine injection on acute cerebral infarction: a Bayesian network meta-analysis. Evid Based Complement Alternat Med. 2020;2020:1–12. doi:10.1155/2020/8318792
15. Kwan YH, Chooi S, Yoon S, et al. Professionalism in traditional Chinese medicine (TCM) practitioners: a qualitative study. BMC Complement Med Ther. 2020;20(1):1–10. doi:10.1186/s12906-020-03127-8
16. Qi X, Guo Z, Chen Q, et al. A data mining-based analysis of core herbs on different patterns (Zheng) of non-small cell lung cancer. Evidence-Based Complementary Alternative Medicine. 2021;2021:1–13. doi:10.1155/2021/3621677
17. Wenxiang D, Jidong Z, Wenan Z, Qinghu H. Traditional Chinese medicine Master XIONG Jibo’s medication experience in treating arthralgia syndrome through data mining. Digital Chinese Medicine. 2022;5(2):154–168. doi:10.1016/j.dcmed.2022.06.005
18. Wang X, Pang F, Du X-G. Analysis of Traditional Chinese Medicine Symptoms in Children with Spastic Cerebral Palsy, a Protocol for Data Mining. J Multidiscip Healthc. 2023;Volume 16:3143–3149. doi:10.2147/JMDH.S426969
19. Li X Revision of guidelines, definitions, classification and diagnostic criteria for cerebral palsy.
20. Cai L, Zhu Y. The challenges of data quality and data quality assessment in the big data era. Data Sci. J. 2015;14:2. doi:10.5334/dsj-2015-002
21. Juddoo S, George C, Duquenoy P, Windridge D. Data governance in the health industry: investigating data quality dimensions within a big data context. Appl Syst Innov. 2018;1(4):43. doi:10.3390/asi1040043
22. Li D, Qu J, Tian Z, Mou Z, Zhang L, Zhang X. Knowledge-Based Recurrent Neural Network for TCM Cerebral Palsy Diagnosis. Evidence-Based Complementary Alternative Medicine. 2022.
23. Yang J, Wang H. Exploring the Mechanism of Umbilical Moxibustion on Improving Spastic Cerebral Palsy of Liver Strong Spleen Weak Type Based on the Theory of. Clin Med. 2023;4(2):113–118.
24. Jiao W, Wang H. Research progress of traditional Chinese medicine in children with cerebral palsy. Clin Med. 2022;3(2):74–80.
25. Matos LC, Machado JP, Monteiro FJ, Greten HJ Can traditional Chinese medicine diagnosis be parameterized and standardized? A narrative review.
26. Liu S, Zhu JJ, Li JC. The interpretation of human body in traditional Chinese medicine and its influence on the characteristics of TCM theory. Anat Record. 2021;304(11):2559–2565. doi:10.1002/ar.24643
27. Dou Z, Xia Y, Zhang J, et al. Syndrome differentiation and treatment regularity in traditional Chinese medicine for type 2 diabetes: a text mining analysis. Front Endocrinol. 2021;12:728032. doi:10.3389/fendo.2021.728032
28. Ma Y, Chen M, Guo Y, et al. Prevention and treatment of infectious diseases by traditional Chinese medicine: a commentary. Apmis. 2019;127(5):372–384. doi:10.1111/apm.12928
29. Zhang SQ, Li JC. An introduction to traditional Chinese medicine, including acupuncture. Anat Record. 2021;304(11):2359–2364. doi:10.1002/ar.24782
30. Deng W-X, Zhu J-P, Liu Y-J, Zhang Y-G, Huang H-Y, Zhang W-A. Design of a WeChat learning platform for syndrome differentiation. Digital Chinese Medicine. 2018;1(2):143–154. doi:10.1016/S2589-3777(19)30019-9
31. He Y, Zheng X, Sit C, et al. Using association rules mining to explore pattern of Chinese medicinal formulae (prescription) in treating and preventing breast cancer recurrence and metastasis. J Translational Med; 2012.
32. Xia X. Introduction to Chinese Internal Medicine. World Scientific; 2013.
33. Liu Z-W, Shu J, Tu J-Y, Zhang C-H, Hong J. Liver in the Chinese and Western medicine. Integr Med Int. 2017;4(1–2):39–45. doi:10.1159/000466694
34. Zhang Y, Fang X-M. Hepatocardiac or cardiohepatic interaction: from traditional Chinese medicine to Western medicine. Evidence-Based Complementary Alternative Med. 2021.
35. Chung YK, Chen J, Ko KM. Spleen function and anxiety in Chinese medicine: a western medicine perspective. ChinMed. 2016;7(3):110–123. doi:10.4236/cm.2016.73012
36. Ots T. The angry liver, the anxious heart and the melancholy spleen. In: Medical Anthropology. Routledge; 2023:237–274.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
