Back to Journals » Psychology Research and Behavior Management » Volume 16
Analysis of the Mediation Effects of Adverse Mental Health Outcomes in HIV-Infected Women of Childbearing Age from Multiple Perspectives Including Discrimination Perception
Authors Zheng Y , Li X, Xia Y, Li X, Yang G, Shi R, Feng Y
Received 12 May 2023
Accepted for publication 17 August 2023
Published 28 August 2023 Volume 2023:16 Pages 3447—3459
DOI https://doi.org/10.2147/PRBM.S421071
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Mei-Chun Cheung
Yinxia Zheng, Xianfeng Li, Yan Xia, Xiaoqin Li, Genglin Yang, Rui Shi, Ying Feng
Urumqi Maternal and Child Health Hospital, Urumqi, Xinjiang, People’s Republic of China
Correspondence: Ying Feng, Email [email protected]
Objective: To Analysis of the mediation effects of adverse mental health outcomes in HIV-infected women of childbearing age from multiple perspectives including discrimination perception, social capital, and other factors.
Methods: A cross-sectional survey was conducted among 553 people in Xinjiang region of China using Survey scale. AMOS was used to identify factors that influenced the “discrimination perception/mental resilience/social capital-depression-poor mental health outcomes” pathway.
Results: A total of 44.85% and 42.13% of the study participants had anxiety and depression symptoms, as perceived discrimination increased, the higher the level of depression in HIV-infected women of childbearing age. Correlation coefficient among depression with poor mental health outcomes was also significant. Psychological resilience, social capital and depression have mediating effects on perceived discrimination and poor mental health outcomes, discrimination perception had an indirect effect on depression through social capital and an indirect effect on adverse mental health outcomes through depression and psychological resilience. The modified model has a good fitting effect.
Conclusion: Discrimination perception was shown to affect adverse mental health outcomes by impacting mental resilience, depression, and social capital. The findings suggest the need for measures to reduce adverse mental health outcomes by decreasing discrimination perception, increasing social capital, and enhancing psychological resilience.
Keywords: women of childbearing age, HIV-infected, psychological resilience, discrimination perception, mental health
Introduction
HIV infection (Human immunodeficiency virus) has become a manageable chronic disease. Research across several disciplines has sought to inform the development of new HIV prevention and treatment efforts. The Joint United Nations Programme on HIV/Acquired Immunodeficiency Syndrome reports that by 2020, an estimated 37.7 million people worldwide will be living with HIV, of whom more than half (53%) will be women aged 15 years and older.1 The same report also shows that women in sub-Saharan Africa have a high rate of HIV infection, with girls and women living with HIV accounting for 63% of total infections in the region.1,2
However, more recent studies have also focused on understanding the living conditions and improving mental health of people living with HIV.3 According previous studies, 25–40% of people infected with HIV will have mental problems, and some even have suicidal thoughts.4 Previous studies have shown WLHIV in low - and middle-income countries reportedly experience considerable psychological challenges, including depression, stress, anxiety, and fear, due to various issues they face after an HIV diagnosis.5–7 People living with HIV also reportedly face many social challenges, such as stigma and discrimination at the hands of others or those not infected in the family, community, workplace and health care Settings, manifested in discriminatory and stigmatized attitudes and behaviours.8 As a result, people living with AIDS have gradually reduced their social capital, social capital mainly includes their relatives, friends and all kinds of resources that can be used, the amount of social capital shows whether they can get timely and effective help when they have difficulties.
Given that sexual transmission and sharing needles are two of the primary routes of HIV infection, people living with HIV (PLHIV) often are frequently labeled as immoral. This population often experiences societal stigma and discrimination and receives unequal treatment when seeking medical care, education, employment, and legal assistance, which can reduce quality of life.9 In a society where public stigma is widespread, it is easier to identify with societal views and further transform them into self-stigma, which can lead to depression, anxiety, concealment, revenge, and other negative behaviors.10
A recent study found that identifying the factors that influence PLWHA and providing an appropriate intervention can effectively improve treatment compliance,11 personal well-being,12 mental health, and life quality.13 The poor mental health status of PLWHA is a critical public health issue.14 This requires an analysis of current mental health status of PLWHA, factors affecting patient quality of life, and the causal relationship between them, as well as potential risk groups. Findings can help inform intervention measures that effectively improve the quality of life of PLWHA.
Some studies suggest that Women infected with HIV have the significantly increased risk among anxiety and depression compared to those who are not infected. For example, a cohort study conducted in 2018 showed that women infected with HIV during pregnancy have a higher risk of depression than women not infected with HIV.15 A study shows that women infected with HIV, within 18–24 months after delivery, the subjects all expressed concerns about their children’s HIV infection, were reluctant to disclose their HIV infection to others, and felt that HIV infection would bring shame to the family.16 Studies have shown that perinatal patients infected with HIV often lack the motivation to take preventive measures, do not participate in routine HIV monitoring, and are reluctant to consult and participate in testing.17 There may be many reasons for this phenomenon. First of all, women are more likely to experience anxiety, depression and other conditions, and HIV infection can further increase women’s anxiety and depression symptoms. Secondly, women infected with HIV will worry about their own health, whether it will be transmitted to their children, worry that their children will be isolated and unable to take little care of their children, which will increase the psychological burden of women.18
However, there is a lack of research on mental health challenges related to HIV and other factors in women infected HIV globally and in China. This study aims to analyzes sociodemographic characteristics, HIV infections, and the impact of social capital and perceived discrimination on adverse mental health outcomes among PLWHA from multiple perspectives. The findings should provide a scientific basis for improving mental health of HIV-infected women of childbearing age. Understanding and exploring the physiological impact of HIV will provide empirical evidence for the psychosomatic health treatment policies of HIV patients, and provide targeted evidence-based interventions and ideas for further improving the mental health of HIV-infected women of childbearing age.
Materials and Methods
This is a cross-sectional study design, We use STROBE revised study design, description settings, data collection, ethics and so on.
Study Subjects
This study in accordance with the Declaration of Helsinki. The study subjects included 553 women of childbearing age who visited designated antiviral treatment institutions in the Xinjiang Uygur Autonomous Region from September 2021 to September 2022 and were identified by convenient sampling. Recruitment of volunteer research subjects was publicized by the project leader of each medical unit and each subject was fully informed about the study. The research subjects signed informed consent before participating. Subjects fill out their own questionnaires and if they have any questions, they can ask our investigators. Study subjects who were women of childbearing age (20–39 years of age), had an HIV infection confirmed by Centers for Disease Control and Prevention, can read clearly, understand and answer questions correctly, and agreed with cooperating the investigation, were included in the study. Individuals who were critically ill, unable to read and fill out questionnaires due to objective circumstances, had a mental illness or intellectual deficiency that made it impossible to complete the survey were excluded. This study was approved by the Ethics Committee (XJFYLL2021033) at the Urumqi Maternal and Child Health Hospital.
Survey Method and Content
A survey questionnaire was anonymously completed by the study subjects. Questions obtained information about (1) general sociodemographic characteristics, including age, education level, occupation, economic status, and residence, (2) HIV-related knowledge, Including the mode of infection, the route of transmission, prevention, treatment, (3) HIV-related characteristics, including physical health status, route and year of HIV infection, sexual partners, childhood abuse and sexual abuse, (4) discrimination perception, (5) psychological resilience, (6) social capital status, and (7) mental health outcomes. (8) SAS-20 (self-rating anxiety scale),(9) Center for Epidemiologic Studies Depression Scale-10.
Measurement Tools of the Primary Indicators
The questionnaire and scale were revised to focus on the experience of HIV-positive women of childbearing age and were tested for reliability and validity. The following scales were included: (1) an 8-item Personal Social Capital Scale (PSCS-8),19 (2) a 12-item short HIV Stigma Scale used to measure discrimination perception,20 and (3) the psychological resilience Scale (PRS) used to measure psychological resilience.
PSCS-8 used to measure social capital was developed by Wang et al. This is a simplified version of the original 42-item social capital scale compiled by Chen et al. Eight items are included and scored using a Likert scale. The 1–5 scores represent “Little or no (None)”, “A Few (AFP)”, “Some (Some)”, “Many (Most)” and “Very many or all (All)”, respectively. The simplified scale has been applied and is shown to have good reliability among HIV-positive individuals in China, with a Cronbach α coefficient = 0.866, indicating good reliability.
The 12-item Short HIV Stigma scale was used to measure discrimination perception. The scale is divided into four dimensions: personalized stigma (actual discrimination), disclosure concerns (fear of disclosure), concerns with public attitudes (public attitude), and negative self-image (negative self-impression), with a total of 12 items. A Likert quadruple scale is used with 1–4 points representing “strongly disagree”, “disagree”, “agree”, and “strongly agree”, respectively. The scores of each dimension were added with higher total scores representing more severe discrimination perception. The construct validity of the scale and the Cronbach α of each dimension were >0.7, with good construct validity and reliability.
The psychological Resilience Scale (PRS) was used to measure physiological resilience status. This scale contains 15 items that are scored using a Likert 5 scale, with 1–5 points representing “completely inconsistent”, “not quite consistent”, “unclear”, “more consistent”, and “fully consistent”, respectively. A higher total score indicates higher psychological resilience and an increased chance that individuals will recover from stressful events. The PRS was shown to have good reliability and validity in China.
PSCS-8, Stigma scale, PRS are shown in the appendix.
Statistical Analysis
This study was the first to use discrimination perception and social capital as the independent variable, X, poor mental health outcomes as the dependent variable, Y, and depression as the mediating variable. Using SPSS (Statistical Product and Service Solutions) to the data for Statistical analysis. This established the mediation effect model, M. To more clearly assess the relationship between particular variables, use AMOS (Analysis of Moment Structure) build a structural equation model, to analyze the effects of discrimination perception, social capital, depression, and life quality and to establish a pathway analysis of the “discrimination perception/social capital-depression-adverse outcomes of mental health.”
Results
Basic Information About the Respondents
We investigated 553 HIV patients, more than half of whom were >35 years of age, and 32.4% of whom were 25–35 years of age. Slightly more respondents lived in an urban area rather than a rural area, and most had a high school education or below (91.5%), with only 2.5% having a bachelor’s degree or above. More than 50% respondents were married, while 24.4% were divorced, 11.6% were widowed and 7.4% were unmarried. Most (65.6%) of the participants were unemployed. The average monthly income was relatively low, with 44.7% and 43.6% having an income of <1000 yuan (about 138.4 dollar) or 1000–3000 yuan ((about 138.4–415.2 dollar). Most (71.8%) people had new rural cooperative medical scheme (NRCMS) insurance or resident medical insurance, while 19.5% had employee medical insurance and 4.9% had no insurance. Most (65.5%) of patients contracted the disease through heterosexual sex and most became infected after >1 year. Most married couples (63.8%) used condoms every time they had sex, while 10.92% never used condoms (Table 1).
 |
Table 1 Basic Characteristics of the Survey Respondents |
Discrimination Perception, Depression, Social Capital, and Poor Mental Health Outcomes
The perceived discrimination, anxiety, depression, and poor mental health outcomes of PLWHA are described in Table 2. HIV-related stigma scores were averaged into four dimensions, actual discrimination mean and SD = 6.57 ± 2.56), public fear (mean and SD = 7.31 ± 2.34), public attitude (mean and SD= 6.56 ± 2.52), and negative self-image (mean and SD = 6.74 ± 2.55). The total social capital mean and SD of 20.24 was divided into three dimensions, family support (mean and SD = 1.24 ± 0.42), social support (mean and SD = 1.20 ± 0.40), and life attitude (mean and SD = 1.29 ± 0.45). The mean anxiety (SAS-20) and depression (CESD-10) mean and SD were 81.25 ± 50.11 and 9.02 ± 5.55, respectively. A total of 44.85% and 42.13% of the study participants had anxiety and depression symptoms, respectively. Worrying about the public was the biggest concern relating to discrimination perception. Over 10% of participants stated having poor mental health outcomes (Table 2).
 |
Table 2 Discrimination Perception, Depression, Social Capital, and Adverse Mental Health Outcomes Among the Participants |
Correlation Analysis of Perceived Discrimination, Depression, Social Capital, Psychological Resilience, and Poor Mental Health Outcomes
The correlation between discrimination perception, depression, social capital, mental resilience, and poor mental health outcomes was assessed. The correlation coefficient for visual perception was 0.859 (p<0.001), while the coefficients for actual discrimination, public concern, public attitude, and negative self-impression were 0.886, 0.926, and 0.893, respectively (p<0.001), indicating that total discrimination perception and actual discrimination, public concern, negative self-impression have high positive correlations, total discrimination perception and public attitude has very high positive correlation. Depression was also significantly correlated (p<0.001), with correlation coefficients of 0.116 (p=0.006), and 0.157 (p<0.001), 0.145 (p=0.001), 0.211 (p<0.001), and 0.176 (p<0.001), Depression and actual discrimination, worry about the public, public attitude, negative impression total discrimination perception have negligible correlations. The correlation coefficient between depression and poor mental health outcomes was also significant (0.243; p<0.001), while they have negligible correlations. The total psychological resilience score and the correlation coefficients for the four dimensions of hardship, continuous work, strength, and hope were 0.802, 0.7090, 0.889, and 0.885, respectively (p<0.001), indicating they have high positive correlations. The total score for social capital and the three dimensions of family support, social support, and life attitude correlation coefficients were 0.621 (p<0.001), 0.667 (p<0.001), and 0.142 (p=0.001), respectively. They have moderate positive correlations except life attitude.
In summary, the visual perception score and the four dimensions (actual discrimination, worry about the public, public attitude, and negative impression) were strongly correlated. Psychological resilience was also strongly correlated with its four dimensions and social capital was well correlated with its three dimensions (Table 3).
 |
Table 3 Correlation Analysis of Perceived Discrimination, Depression, Social Capital, Psychological Resilience, and Adverse Outcomes of Mental Health |
Model Parameter Estimation and Fit Evaluation
After developing the path diagram, importing the data, running the program, and making repeated corrections through the comprehensive observation correction index, standardization coefficient, and regression coefficient of the P value, the path model 8 coefficient was obtained. Discrimination perception was found to have the indirect effect on depression, mental health outcomes as a result of psychological resilience. The four dimensions of discrimination perception, actual discrimination, worry about the public, public attitude, and negative self-impression had an effect value of >0.7. Two dimensions of social capital, family and society, had a high effect value, while life attitude had a low effect value (Figure 1).
 |
Figure 1 Path analysis graph of discrimination, social capital, psychological resilience. |
Table 4 shows the values of each path coefficient in the path analysis, where a P value < 0.05 indicates that this path has an effect. For example, the first row, discrimination perception - mental resilience, has a standardized effect value of 0.14, indicating that discrimination perception will increase mental resilience; the third row, social capital - depression, has a standardized effect value of −0.23. Suggesting that having sufficient social capital reduces the incidence of depression. The effect value of the four dimensions of psychological resilience, hard-working, continuous work, strength, and hope, had an effect value of >0.7 (Table 4).
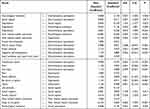 |
Table 4 Pathway Coefficients for the Pathway Model |
Table 5 provides the standard range and actual fitting index of the structural equation model, where in CFI (Comparative Fit Index), which compares a hypothetical model to an independent model, The value ranges from 0 to 1. The closer to 0, the worse the fitting effect, the closer to 1, the better the fitting effect. It is widely believed that the model fits well if CFI is ≥0.9. TL (Tuck-Lewis index) is a kind of relatively fitting index. The value ranges from 0 to 1. The closer the model is to 0, the worse the model matching effect, and the closer the model is to 1, the better the model matching effect. If TLI>0.9, the model is considered to have a good fit. RMSEA (root-mean-square error of approximation), that is, approximate root-mean-square error, RMSEA is an index to evaluate the model does not fit. If the value tends to 0, the fitting effect is better; If the value tends to 1, the worse the model fits. Researchers generally believe that when RMSEA=0, the model fitting is very perfect. RMSEA≥0.10 indicates poor model fitting effect. The specific indicators are shown in Table 5. According to the model fitting coefficient, Chi-square = 3.25, GFI = 0.921, RMSEA = 0.084, IFI = 0.927, TLI = 0.910, CFI = 0.926, and NFI = 0.909, The path analysis graph shows that discrimination perception can reduce poor mental health outcomes by increasing mental resilience, can lead to psychological problems by increasing depression, and discrimination can increase depression by reducing social capital. In addition, discrimination is highly correlated with dimensions such as actual discrimination, public concern, public attitude, negative self-image, and psychological resilience shows the same results, highly correlated with dimensions (Table 5).
 |
Table 5 Model-Fitting Exponents |
Discussion
We find that A total of 44.85% and 42.13% of the study participants had anxiety and depression symptoms, as perceived discrimination increased, the higher the level of depression women of childbearing age infected with HIV. The correlation coefficient between depression and poor mental health outcomes was also significant. Psychological resilience, social capital and depression have mediating effects on perceived discrimination and poor mental health outcomes, Discrimination perception had an indirect effect on depression through social capital and an indirect effect on adverse mental health outcomes through depression and psychological resilience. The modified model has a good fitting effect. While antiviral treatment measures can prolong the life span of HIV-positive individuals, the disease remains incurable and still poses a serious health threat.21 In China, there is widespread fear and discrimination relating to HIV and AIDS. As a result, HIV patients have low adaptability to the disease, experience external pressure, and have low coping ability, psychological resilience, and social capital.
This study found that the higher an individual’s literacy level, the better their psychological resilience. More education may make it easier for PLWHA to understand and accept their current situation, including the severity of the disease, its high infectivity, the risk of fatality, and the lack of a cure.22 Patients also had higher psychological resilience if they were participants of the NRCMS possibly because of the relatively low reimbursement ratio of residents/NRCMS, low patient willingness to seek treatment, reduced attention to their own health status, lower concern about the disease, and higher psychological resilience.
Our research found that perceived discrimination was significantly associated with depression. The correlation coefficient for visual perception was 0.859, while the coefficients for actual discrimination, public concern, public attitude, and negative self-impression were 0.886, 0.926, and 0.893, respectively, indicating that total discrimination perception and actual discrimination, public concern, negative self-impression have high positive correlations, total discrimination perception and public attitude has very high positive correlation. Similar findings have been found in other studies.22 Such as, in developed countries, a recent research of HIV-infected women found that women identified as having anxiety disorders were 1.30 times more likely to report HIV-related discrimination (95% CI: 1.16,1.43), However, women identified as depressed were 1.61 times more likely to report HIV-related discrimination (95% CI: 1.38,1.83).23 In a report from a cohort study in New Orleans, Felker-Kantor et al apparently higher levels of HIV-related discrimination were significantly associated with anxiety (relative risk (RR) =1.91, 95% CI: 1.17,3.12) and depression (RR=1.67, 1.25, 2.23).24 The possible reason is that HIV-induced discrimination leads to social isolation/exclusion and lack of social support, which then further exacerbates symptoms of anxiety and depression.25,26 AIDS-related discrimination and quality of life are also highly correlated, and some studies have found that feelings of discrimination may directly impact an individual’s quality of life. n developing countries, such as China, A recent analysis found that the quality of life of HIV patients reporting no discrimination was 1.83 times greater than those experiencing discrimination (95% CI: 1.24,2.41).27 The results of our study were not significant, One possible explanation is the bias of insufficient sample size or participant heterogeneity, including differences in their regional and cultural backgrounds.
The path analysis graph shows that discrimination perception leads to poor mental health outcomes by aggravating depression. In China, there is an “immoral” label and discriminatory attitude towards PLWHA, a stigmatization that is often further internalized into a negative evaluation of self.28 Social discrimination and negative self-evaluation together increase the negative emotions of HIV-infected people and leads to adverse mental health outcomes.10 On the other hand, Studies in some developed countries show that PLWHA experiencing a low level of discrimination may be less sensitive to unfriendly discrimination settings, reducing their psychological burden and increasing their quality of life.29
Discrimination perception was also found to have an indirect effect on mental health by increasing psychological resilience. Individual feelings of stress were shown to be mediated by discrimination and the relationship of mental health, a finding consistent with those of Paine E et al in developing country. In other words, while the psychological resilience of People with HIV have higher levels discrimination perception gradually improved, the increase in resilience contributed to poorer mental health outcomes.30 Discrimination perception can also indirectly affect mental health through social capital, which mediates discrimination perception and poor mental health outcomes. The disclosure of HIV infection is a prerequisite for PLWHA to receive social support for their medical care; however, this population often conceals their infection status, affecting their social support, and further affect mental health.31
While our study did not find a significant direct effect of social capital on adverse mental health outcomes, structural equation models found that perceived discrimination had an important indirect effect on adverse mental health outcomes by reducing social capital. Very little research has also shown that HIV-related discrimination is a significant risk factor for poor mental health among people living with HIV.32 The likely reason is that HIV-related stigma can lead to feelings of social isolation/social exclusion, which further leads to a rapid decline in life quality,33 which in turn causes adverse psychological outcomes. It is also possible that feelings of discrimination decrease self-esteem and social support for PLWHA, ultimately reducing their quality of life. Serious effects on mental health can result in adverse outcomes.34 In developed countries, previous research has shown that lack of social capital, experiences of social exclusion and isolation, avoidance by relatives, internalization or perceptions of discrimination, and poor economic conditions are also important factors contributing to depression, anxiety, fear and worry among HIV-infected people.35
Overall, the current findings suggest that HIV-related perceptions of discrimination play a very important role in the quality of life and mental health of people living with HIV, and that social capital partially mediates the association between perceptions of discrimination and poor mental health outcomes.
In summary, women of childbearing age infected with HIV often have low social capital and experience significant discrimination, especially those patients with higher levels of education, those who are divorced or widowed, or those of low income. Special attention should be given to this population to increase their medical care, assure that they have an appropriate understanding of the disease, stay healthy, avoid serious disease complications, and are not financially burdened. In addition, measures should be taken to reduce perceived discrimination, increase social capital, and enhance psychological resilience along with other psychological interventions that can improve the mental health and quality of life of women of childbearing age infected with HIV and reduce the risk of adverse mental health outcomes.
Theoretical Contributions
All authors have made important contributions to this study, whether in the research ideas, design, field investigation, data collation, statistical analysis and explanation of causes, etc. Participate in the drafting, revision or critical review of articles; Finalizing the manuscript for publication; All authors agree to contribute to the journal and are responsible for the content of their articles.
Practical Implications
Our study aims to develop a structural equation model to explore the complex relationship between discrimination perception, depression and adverse mental health outcomes, and based on the findings, provide a new perspective and thinking for interventions to improve mental health and quality of life in women of Childbearing age living with HIV. To explore the relationship between HIV discrimination cognition, social capital, depression and mental health status of women living with HIV in childbearing age, and provide evidence-based medical basis and support for the development of corresponding intervention measures and treatment programs. The results of this study will have certain help and benefits for women of childbearing age infected with HIV.
Study Limitations and Strengths
There are some limitations to the number of sites surveyed in this study, mainly because all the data came from two antiviral treatment sites in Xinjiang, China, and the study sites were not extensive enough, and the results of this study may have certain limitations in extending to other regions. In addition, the data in our study was mainly collected by the subjects who filled in the questionnaire themselves, and the influence of social expectation effect on the subjects could not be excluded, which may lead to certain reporting bias. Nevertheless, there are many advantages and necessity to our study, which is the first to examine the mental health, quality of life and poor mental health outcomes of HIV infection in the childbearing age in Xinjiang, China, and the study design includes multiple perspectives such as perception of discrimination, mental resilience and social capital.
Future Research
We currently have fewer sites to study, and more HIV-infected people will be investigated in the future. However, we still do not know whether psychological counseling and counseling will improve the psychological status of HIV-infected people, so the future study will be carried out: psychological intervention for people with poor mental health outcomes, to assess whether this intervention is enough to really change the psychological status of HIV-infected people.
Conclusion
Discrimination perception was shown to affect adverse mental health outcomes by impacting mental resilience, depression, and social capital. It is suggested that psychological counseling and intervention should be carried out on HIV-infected people to improve their mental health. The content of psychological counseling should include reducing discrimination, increasing social capital, and enhancing psychological resilience. In addition, the families of women of childbearing age with HIV should also invited to participate, encouraging HIV-infected people to build self-confidence, make more friends, and tell their true thoughts to their families. These methods are helpful to improve the effect of psychotherapy.
Acknowledgments
We would like to thank all women of childbearing age living with HIV and the researchers who contributed to this study, as well as Science and Technology Department of Xinjiang Uygur Autonomous Region and the Key Laboratory of HIV Prevention and Control Research of Xinjiang Uygur Autonomous Region.
Funding
Our research project was funded by the Natural Science Foundation of Xinjiang Uygur Autonomous Region (ID: 2022D01A30) and the Key Laboratory of HIV Prevention and Control Research of Xinjiang Uygur Autonomous Region (ID: XJYS1706-2021002).
Disclosure
All authors declare no conflicts of interest in this work.
References
1. UNAIDS. Global HIV & AIDS Statistics-Fact Sheet; The Joint United Nations Programme on HIV/AIDS. Geneva, Switzerland; 2021. Available from: https://www.unaids.org/en/resources/fact-sheet.
2. UNAIDS. UNAIDS Data; Joint United Nations Programme on HIV/AIDS. Geneva, Switzerland; 2021. Available from: https://www.unaids.org/sites/default/files/media_asset/2020_aids-data-book_en.pdf.
3. Gedefie A, Adamu A, Alemayehu E, et al. Hepatitis C virus infection among HIV-infected patients attending Dessie Referral Hospital, Northeastern Ethiopia. Int J Microbiol. 2021;1:1–7. doi:10.1155/2021/675851
4. Zeng D, Jin Y, Tian B, et al. Incidence and influencing factors of anxiety, depression and sleep disorder in AIDS patients with antiviral therapy. J Daliani Univer. 2019;8(04):86–91.
5. UNAIDS. UNAIDS data Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2020. Available from: https://www.unaids.org/sites/default/files/media_asset/2020_aids-databook_en.pdf.
6. Qin S, Tan Y, Lu B, Cheng Y, Nong Y. Survey and analysis for impact factors of psychological distress in HIV-infected pregnant women who continue pregnancy. J Matern Fetal Neonatal Med. 2018;32:1–8.
7. Ruffell S. Stigma kills! The psychological effects of emotional abuse and discrimination towards a patient with HIV in Uganda. BMJ Case Rep. 2017;1(1):1–8.
8. Halli SS, Khan CGH, Moses S, et al. Family and community level stigma and discrimination among women living with HIV/AIDS in a high HIV prevalence district of India. J HIV AIDS Soc Serv. 2017;16(1):4–19.
9. UNAIDS. Biannual report of the China-UN AIDS Joint Project (2020–2021); 2022.
10. Scofield D, Moseholm E. HIV-related stigma and health-related quality of life in women living with HIV in developed countries: a systematic review. AIDS Care. 2021;13:1–9.
11. Reif S, Wilsonm E, Mcallaster C, et al. The relationship between social support and experienced and internalized HIV-related stigma among people living with HIV in the deep south. Stig Health. 2021;3:6.
12. Heydari M, Mehraeen M, Keshani P, et al. The association between mental health of HIV patients and antiretroviral medication adherence. Int J High Risk Behav Addict. 2021;10(2):. doi:10.5812/ijhrba.102149
13. Delaney E, Brien W, Advisor P, et al. The Association Between Acceptance And Health For Individuals Who Are HIV-Positive [dissertation]. Bowling Green (OH): Graduate College of Bowling Green State University; 2010.
14. Peng L. Study on the Medical Discrimination of HIV/Patients in Guangdong Province. Jinan University; 2016.
15. Ickovics JR, Hamburger ME, Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV epidemiology research study. JAMA. 2011;285(11):1466–1474. doi:10.1001/jama.285.11.1466
16. Orza L, Bewley S, Logie CH, et al. How does living with HIV impact on women’s mental health? Voices from a global survey. J Int AIDS Soc. 2017;18(Suppl 5):20289. doi:10.7448/IAS.18.6.20289
17. Kapetanovic S, Dass-Brailsford P, Nora D, et al. Mental health of HIV-seropositive women during pregnancy and postpartum period: a comprehensive literature review. AIDS Behav. 2018;18(6):1152–1173. doi:10.1007/s10461-014-0728-9
18. Ceccon RF, Meneghel SN, Hirakata VN. Women with HIV: gender violence and suicidal ideation. Rev Saude Publica. 2018;48(5):758–765. doi:10.1590/S0034-8910.2014048005228
19. Wang W, Chen X, Yan H, et al. Association between social capital and suicide ideation, plan and attempt among men living with HIV in China. J Affect Dis. 2021;280:173–179. doi:10.1016/j.jad.2020.11.088
20. Luz P, Torres T, Almeida-Brasil C, et al. Translation and validation of the short HIV stigma scale in Brazilian Portuguese. Health Qual Life Out. 2020;18(1):1–12. doi:10.1186/s12955-020-01571-1
21. Elly A, Musa S, Kafunjo B. Prevalence and factors associated with HIV infection among Teenage Mothers Delivered at Mulago Hospital - a Cross-Sectional Study. Int J Gyneco Obstet. 2022;12:661–670.
22. Algarin A, Sheehan DM, Varas-Diaz N, et al. Enacted HIV-related Stigma’s Association with Anxiety & Depression Among People Living with HIV (PLWH) in Florida. AIDS Behav. 2021;25(1):93–103. doi:10.1007/s10461-020-02948-5
23. Beer L, Tie Y, Padilla M, et al. Generalized anxiety disorder symptoms among persons with diagnosed HIV in the United States. AIDS. 2019;33(11):1781–1787. doi:10.1097/QAD.0000000000002286
24. Felker-Kantor E, Wallace ME, Madkour AS, et al. HIV stigma, mental health, and alcohol use disorders among people living with HIV/AIDS in New Orleans. J Urban Health. 2019;96(6):878–888. doi:10.1007/s11524-019-00390-0
25. Hojilla J, Santiago-Rodriguez E, Sterling S, et al. HIV stigma and its associations with longitudinal health outcomes among persons living with HIV with a history of unhealthy alcohol use. AIDS Behav. 2021;25(1):215–224. doi:10.1007/s10461-020-02963-6
26. Nyblade L, Stockton M, Saalim K, et al. Using a mixed‐methods approach to adapt an HIV stigma reduction intervention to address intersectional stigma faced by men who have sex with men in Ghana. J Int AIDS Soc. 2022;25(S1):e25908. doi:10.1002/jia2.25908
27. Wang W, Wang Y, Xiao C, et al. Psychological pathway to suicidal ideation among people living with HIV/AIDS in China: a structural equation model. Psych Res. 2018;260:255–261. doi:10.1016/j.psychres.2017.11.077
28. Onu D. Treatment adherence mediates the relationship between HIV-related stigma and health-related quality of life. AIDS Care. 2021;3:1–5.
29. Szkody E, Mckinney C. Appraisal and social support as moderators between stress and physical and psychological quality of life. Stress Health. 2020;36(5):586–595. doi:10.1002/smi.2957
30. Paine E, Lee Y, Mergenova G, et al. Compounding vulnerabilities: victimization and discrimination is associated with COVID-19 disruptions to HIV-related care among gay, bisexual, and other men and transgender and nonbinary people who have sex with men in Kazakhstan. AIDS Care. 2023;35:1–7.
31. Crawford T, Silverstein S, Spaulding T, et al. Exploring the impact of experiences with everyday and major discrimination and HIV-related stigma on engagement in HIV care among older African Americans living with HIV. J Racial Ethnic Health Disp. 2022;2022:1–8.
32. Akena D, Musisi S, Joska J, et al. The association between aids related stigma and major depressive disorder among HIV-positive individuals in Uganda. PLoS One. 2012;7(11):e48671. doi:10.1371/journal.pone.0048671
33. Vancampfort D, Byansi P, Kinyanda E, et al. Internalised HIV-related stigma associated with physical inactivity in people with HIV and AIDS: a cross-sectional study from Uganda. Afr J AIDS Res. 2021;20(3):238–243. doi:10.2989/16085906.2021.1979607
34. Akatukwasa C, Getahun M, El Ayadi A, et al. Dimensions of HIV-related stigma in rural communities in Kenya and Uganda at the start of a large HIV ‘test and treat’ trial. PLoS One. 2021;16(5):e0249462. doi:10.1371/journal.pone.0249462
35. Azhar SV. HIV Stigma and Gender: A Mixed Methods Study of People Living with HIV in Hyderabad, India. Livingston, NJ, USA: ProQuest LLC; 2018.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
