Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Analysis of Symptom Spectra and Associated Factors Among 536 Respondents During the COVID-19 Epidemic in China: A Cross-Sectional Study
Authors Wang Y , Li F, Liu J, Liu J, Qin P , Zhang J, Zhang Y, Wu S
Received 31 July 2023
Accepted for publication 17 October 2023
Published 3 November 2023 Volume 2023:16 Pages 3261—3272
DOI https://doi.org/10.2147/JMDH.S426607
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ye Wang,1,* Fenxiang Li,1,* Jian Liu,2 Jing Liu,3 Pei Qin,4 Jiayi Zhang,5 Yingtao Zhang,5 Shuning Wu6
1Department of Epidemiology, School of Medicine, Jinan University, Guangzhou, People’s Republic of China; 2Department of General Surgery, Maternal and Child Health Hospital, Qingyuan, Guangdong, People’s Republic of China; 3Intensive Care Unit 1, The First Affiliated Hospital, Jinan University, Guangdong, Guangzhou, People’s Republic of China; 4Shenzhen Qianhai Shekou Free Trade Zone Hospital, Shenzhen, People’s Republic of China; 5Guangdong Provincial Center for Disease Control and Prevention, Guangzhou, People’s Republic of China; 6Department of Thyroid and Breast Surgery, Shenzhen Qianhai Shekou Free Trade Zone Hospital, Shenzhen, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yingtao Zhang, Guangdong Provincial Center for Disease Control and Prevention, Guangzhou, 510000, People’s Republic of China, Tel +86 15918805867, Email [email protected] Shuning Wu, Thyroid and Breast Surgical Department, Shenzhen Qianhai Shekou Free Trade Zone Hospital, Shenzhen, 518067, People’s Republic of China, Tel +86 13480209989, Email [email protected]
Purpose: This study aims to identify common COVID-19 symptoms and asymptomatic infection rates during the epidemic in China. We also introduce the concepts of “Time-point asymptomatic rate” and “Period asymptomatic rate”.
Object and Methods: A questionnaire survey was conducted online from December 2022 to January 5, 2023, collecting demographic characteristics, laboratory results, clinical symptoms, lifestyle and vaccination history. Statistical methods were used to analyze symptom characteristics, associated factors, and patterns during an 8-day observation period. Numerical variables were described by median M (Q1-Q3) or mean and standard deviation (). Categorical variables are described by frequency (N), ratio (%) or rate (%). The influencing factors were studied by Wilcoxon or Kruskal-Willis H rank sum test or logistic regression analysis, and the trend of symptom incidence by Spearman rank correlation. P value being ≤ 0.05 was statistically significant.
Results: Out of 536 participants, 493 (91.98%) were infected, with 3 asymptomatic cases and 490 symptomatic cases within 8 days. The time-point asymptomatic rate increased from 0.61% on day 1 to 15.42% on day 8. Fever, cough, and fatigue were the main symptoms, with additional symptoms such as vomiting, diarrhea, and hyposmia reported. Symptom durations varied, with cough and expectoration lasting longer and vomiting and diarrhea lasting shorter. Several symptoms showed a downward trend over time.
Conclusion: Our online survey highlighted that most COVID-19 patients experienced symptoms, and the time-point asymptomatic rate showed a dynamic change among the infected population. Onset patterns and demographic factors influence symptom occurrence and duration. These findings have implications for clinical practitioners and decision-makers in public health measures and strategies.
Keywords: Novel coronavirus infection, onset patterns, clinical features, associated factors, time-point asymptomatic, period asymptomatic rate
Introduction
Since December 2019, the novel coronavirus disease (COVID-19) has hit humans and triggered a global pandemic,1,2 and the World Health Organization (WHO) has declared COVID-19 a public health emergency of international concern.3 According to an announcement issued by the National Health Commission of China on December 24, 2022, 397,195 cases of COVID-19 were confirmed in mainland China, with 5241 deaths.4 As of March 16, 2023, there have been more than 760 million confirmed cases and 6.8 million deaths worldwide.5 In response, according to WHO, as of 24 May 2023, 65.53% and 31.40% of individuals have received full vaccination and booster dose of COVID-19 vaccines worldwide, respectively.6 China has vaccinated more than 90% of its population as of April 27, 2023.7 However, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) continues to evolve. The Omicron variant was detected in October 2021 and exhibited high transmissibility and immune evasion, which means current jabs are not very good at providing long-lasting protection against infection.8 As an emerging infectious disease, COVID-19 has obvious symptoms such as fever, cough, fatigue and so on.2,9–11 Pre-symptomatic infection and asymptomatic infection (true asymptomatic or recessive infection) may not have any symptoms,12,13 even if some infected persons are intermittently asymptomatic.14 The investigators anticipated that COVID-19 has its unique symptom spectrum, including its symptom type, onset time, duration, change patterns, and asymptomatic rate at different time points. At present, reports on common symptom types and asymptomatic infection rates of COVID-19 are inconsistent. In terms of the main types of symptoms, Guan et al reported cough, fever and expectoration,15 Shi et al reported fever, cough and fatigue,16 Huang et al considered fever, cough and dyspnea;10,17–19 With regard to the duration of symptoms, Lane et al reported that the mean duration of each symptom was 19 days,2 with a minimum of 0 days and a maximum of 93 days. Regarding the asymptomatic infection rate, Chen et al included 104 studies involving 20,152 cases and considered it to be 33.53%,12 while Gao et al found that it ranged from 1.6% to 80%.20,21
This study was a cross-sectional survey of 536 people in China during the epidemic period from December 2022 to January 2023. The purpose of our research was to study clinical symptom spectra (including generalized spectra of asymptomatic and change patterns) and their associated factors of COVID-19 patients.
Objects and Methods
Subjects and Inclusion and Exclusion Criteria
This survey was conducted in Chinese residents from December 1, 2022, to January 5, 2023. For this study, we followed the STROBE guidelines for observational studies in epidemiology. Subjects were enrolled according to the following criteria: infected or uninfected persons, symptomatic or asymptomatic persons among infected persons were categorized, and relevant indicators were defined.
Infection criteria: Those with positive etiology and serology or clinical manifestations listed in the Diagnosis and Treatment Protocol for New Coronavirus Infection (Trial version of the 10th Edition) proclaimed by National Health Commission of China on January 5, 2023. Inclusion criteria were the following: (1) Adults (≥18 years); (2) Informed consent after being informed of the purpose of this investigation and the information involved; (3) Only participants who were first infected after November 30, 2022 (COVID-19 epidemic period in China); (4) Participants who did not answer the questions repeatedly or without logic. In addition, the following measures were defined: (1) Time-point asymptomatic rate refers to the proportion of infected persons without any clinically relevant symptoms at a particular time in all infected persons; (2) Period asymptomatic rate refers to the proportion of infected persons without any clinically relevant symptoms in all infected persons at a particular period of time; (3) Total asymptomatic rate refers to the proportion of infected persons without any clinically relevant symptoms in all infected persons from the time of virus infection to the time when it is completely eliminated. The “period” of this study finished within 8 days after the occurrence of symptoms after infection in combination with a pre-investigation.
The study was carried out in accordance with the Declaration of Helsinki. Ethical approval was obtained from the Bioethical Committee of School of Medicine of Jinan University. When filling out the online questionnaire, all the surveyors would first read a form of informed consent and choose to agree before they could answer the questionnaire.
Questionnaire Design, Data Processing Methods
The questionnaire added up and adjusted based on the pre-survey results after soliciting expert opinions. The main contents included demographic information, past medical history (including previous infections and underlying diseases), vaccination history, results of antigen or nucleic acid test of novel coronavirus, and 16 infection symptoms mainly mentioned in China’s Diagnosis and Treatment Protocol for Novel Coronavirus Infection (Trial version of the 10th Edition) for 8 consecutive days. In addition, menstrual changes in women after infection were recorded and participants were allowed to report additional symptoms or comorbidities. Because the pre-survey results showed that participants could not accurately recall their drug use during the illness, we only asked whether they used drugs based on symptoms and received special treatment. At the beginning of 2023, the questionnaire was uploaded to the Internet through the “Questionnaire Star” software (https://www.wjx.cn), and then issued to people through online promotion and sharing. During the survey, the participants answered the questions by themselves, and after completing all the required items, the answers were transferred to the researchers via the Internet. To avoid different symptoms caused by different infection time and incubation period, the researchers synchronized onset time of symptoms of each infected person in this study when sorting out the data. For example, if an infected person with a positive nucleic acid test result had no symptoms in the first 2 days and had relevant symptoms on the third day, the third day was taken as the first day of symptom occurrence, and so on. People aged ≤17 years old were not included in the analysis because they may not be able to accurately reflect their symptoms during the infection and only occupied 0.87% of the total participants. To rule out the effect of non-pharmacological interventions, we also excluded people whose time of infection is not consistent. Finally, 536 subjects were included in the study according to the inclusion criteria, including 43 uninfected persons, 3 asymptomatic infected persons and 490 symptomatic infected persons (Figure 1).
 |
Figure 1 Inclusion process of respondents. |
Statistical Analysis Method
Since this is a cross-sectional descriptive study, no formal sample size calculation was required or performed. Numerical variables were described by median M (Q1-Q3) or mean and standard deviation ( ). Categorical variables were described by frequency (N), ratio (%) or rate (%). The influencing factors were studied by Wilcoxon or Kruskal–Wallis H rank sum test or logistic regression analysis, and the trend of symptom incidence by Spearman rank correlation. P value being ≤0.05 was statistically significant.
). Categorical variables were described by frequency (N), ratio (%) or rate (%). The influencing factors were studied by Wilcoxon or Kruskal–Wallis H rank sum test or logistic regression analysis, and the trend of symptom incidence by Spearman rank correlation. P value being ≤0.05 was statistically significant.
Approach to missing data: When the missing value is in the main variable of the analysis, it is supplemented by mean replacement, median replacement, or multiple interpolation according to the data type and actual situation. When missing values are concentrated on a few variables, and these variables are not the main variables in the analysis, these variables with missing values are deleted and do not participate in the corresponding analysis.
Results
Baseline Characteristics and Infection Status
The 536 respondents came from 29 provinces and cities in China except Inner Mongolia, Tibet, Qinghai, Taiwan, and Macao. There were 204 males (38.06%) and 332 females (61.94%). The median age was 33 years old. Among 536 participants, 43 (8.0%) was uninfected and 493 (91.98%) were infected. Middle-aged and non-student populations experienced a higher infection incidence than other populations. Among the infected 493 persons, 490 participants (99.39%) were symptomatic, and 3 individuals (0.61%) were asymptomatic for 8 days. The asymptomatic rate was 8.58%, and the symptomatic rate was 91.42%. 91.8% of those respondents were infected after 10 December 2022. None of the participants received special treatment. The baseline characteristics of the respondents are illustrated in Table 1.
 |
Table 1 Baseline Characteristics of 536 Respondents According to SARS-CoV-2 Infection or Not |
Time-Point Asymptomatic Rate, Incidence, and Duration of Symptoms
Among 493 infected persons, 490 (99.39%) had different types of symptoms, 8 of them had intermittent symptoms (symptoms were discontinuous), with the longest interruption of 2 days (see Table S1); The total number of symptoms per person ranged from 4 (2–6) on Day 1 to 3 (2–5) on Day 6, 2 (1–4) on Day 7, and 2 (1–3) on Day 8, with a median of 3 (2–5) symptoms during the 8-day period; the common symptoms were fever (88.16%), cough (86.53%), and fatigue (76.94%), the longer lasting symptoms were cough for 6 (4–7) days, followed by expectoration for 5 (3–6) days, and the shortest symptom was vomiting for 1 (1–2) days (Table 2).
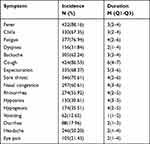 |
Table 2 Incidence and Duration (Days) of Different Symptoms in Symptomatic Infected Persons (n=490) |
Among 493 infected persons, there were 3,10,10,17,24,32,49 and 76 asymptomatic persons from day 1 to day 8, respectively. The Time-point asymptomatic rate gradually increased from 0.61% on day 1 to 15.42% on day 8, showing a dynamic trend (see Figure 2 for details). The first symptoms were fever (71.84%), fatigue (56.73%) and chills (55.10%). The overall incidence changes during the 8-day period are presented in Figure 3. In addition, 30.4% of women infected with regular menstruation in the past had irregular menstruation, with decreased menstrual volume and prolonged menstruation.
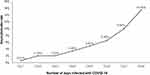 |
Figure 2 The Time-point asymptomatic rate during 8 days of infection (n=493). |
 |
Figure 3 Symptom spectra for 8 days (n=490). |
Factor analysis of symptoms showed that all 16 symptom variables are well expressed by common factors. Based on the eigenvalue greater than 1, two factors are extracted, which together explained 98.18% of the total variance of symptoms. Fever, chills, fatigue, backache, dyspnea, headache, eye pain and vomiting have a high load in the first factor, and the trend of symptom incidence of the first factor begins to peak, and then decreases monotonically, which is interpreted as “monotone decline.” And according to the component score coefficient matrix, it is more reasonable to classify nasal congestion, rhinorrhea, sore throat, diarrhea, cough, expectoration, hyposmia and hypogeusia classify into the second factor. The change trend of symptom incidence of the second factor starts with a certain height, then decreases and then increases. The peak time is about 4 days after the onset of disease, which is presented as “fluctuant decline” (see Tables S2–S4 and Figures S1–S3).
Associated Factors of Different Symptoms Incidence and Duration
The results showed that cough, sore throat, nasal congestion, and eye pain were affected by many factors (≥5). Age, education, occupation, the number of vaccine dosages, gender, smoking habit, and medication use influenced many symptoms (≥4). The number of vaccines doses, age, gender and medication use were positively correlated with symptoms (Table 3 and Table 4). It should be noted that for the missing value of “Interval between last Vaccination” because there were only two persons, accounting for 0.40% of all infected persons, we directly eliminated them and did not participate in the analysis.
 |
Table 3 Logistic Regression Analysis of the Associated Factors of Different Symptoms Incidence |
 |
Table 4 Analysis on the Associated Factors of Different Symptoms Duration |
Discussion
The novel coronavirus, SARS-CoV-2, belongs to the same family as other respiratory viruses such as SARS-CoV and MERS-CoV, and it causes COVID-19.19,20 The symptoms of COVID-19 can vary due to different variants of SARS-CoV-2, including their onset time, duration, change patterns, and even the rate of asymptomatic cases at different time points. At the end of 2022, the China government made major adjustments to the COVID-19 prevention and control policy, and an epidemic dominated by Omicron variants BA.5.2 and BF.7 branches occurred in China.21 In our study, we aimed to investigate the clinical symptom spectrum and influencing factors of individuals infected with the novel coronavirus variants BA.5.2 and BF.7 in China during a specific period at the end of 2022.
The survey included 536 individuals, and it revealed that more than 90% of the investigated population were infected with SARS-CoV-2 (91.98%), and a similar percentage experienced symptomatic manifestation (91.42%). Conversely, the non-infection rate and asymptomatic rate were less than 10% (8.02% and 8.58% respectively). These findings provide a scientific basis for public health decision-makers to allocate health-care resources and design effective public health measures.
Among the infected individuals, the most prevalent symptoms, ranked in descending order of incidence, were fever, cough, fatigue, sore throat, chills, backache, nasal congestion, rhinorrhea, headache, hypogeusia, dyspnea, hyposmia, eye pain, diarrhea, vomiting, and expectoration. These symptoms align with the 16 main infection symptoms outlined in China’s “Diagnosis and Treatment Protocol for Novel Coronavirus Infection (Trial version of the 10th Edition).” Additionally, a significant proportion of individuals (99.39%) reported having at least one symptom, while the asymptomatic rate was less than 1% (0.61%) within an 8-day period. It is worth noting that previous reports have shown varying asymptomatic rates (ranging from 1.6% to 80%) due to differences in the understanding and judgment of the definition of “asymptomatic.”20,21 This variance can be attributed to differences in the incubation period, the timing of symptom appearance and the proportion of asymptomatic cases among individuals infected with SARS-CoV-2.
Results of our study are consistent with previous studies conducted worldwide. Among symptomatic individuals infected with SARS-CoV-2, the average number of symptoms per person within 8 days was three. The most common symptoms observed were fever, cough, and fatigue, which align with the findings of previous studies.2,9–11 However, the incidence of fever in our study (88.16%) differed from the fever rates reported for SARS-CoV (100%), MERS-CoV (98%), and the original case report published in Wuhan (98%).2,10,22,23 Further investigation is required to determine whether this difference is attributed to changes in the symptom spectrum of COVID-19, virus mutation, or the impact of vaccination.
Some symptoms, such as cough and expectoration, lasted longer, with median durations of 6 days and 5 days, respectively, while vomiting and diarrhea occurred for shorter periods, with median durations of 1 day and 2 days, respectively. Other studies have reported that gastrointestinal symptoms are present in 11.4–61.1% of infected patients, but they are typically mild and self-limited.22 Additionally, our findings revealed that symptoms gradually alleviated within 8 days. Symptoms such as fever, chills, fatigue, backache, dyspnea, headache, eye pain, and vomiting demonstrated a monotonous downward trend, while symptoms such as nasal congestion, rhinorrhea, sore throat, diarrhea, cough, expectoration, hyposmia, and hypogeusia exhibited a declining trend with intermittent periods of remission. Klimek L reported that more than 12 months after the onset of 7% of infected people still have hyposmia and hypogeusia.23 In addition, the incidence of hyposmia (30.61%) was lower than that reported by Borsetto et al (47–95% CI: 36–59%).24 Whether it is a different effect of race,25 a unique symptom of COVID-19 and may be the only symptom,26,27 or an important clue to distinguish it from general influenza and allergic rhinitis28 remains to be discussed. According to the survey, more than 30% (30.4%) of women have irregular menstruation, such as reduced menstrual volume and prolonged menstruation, which can confirm that COVID-19 is not only a respiratory disease but also a multiple-system disease.29 The survey also found that among 493 infected persons during the 8-day period, 8 persons (1.62%) had intermittent symptoms (the symptoms were discontinuous) and could be interrupted for 2 days. Specific reasons need to be further studied. In addition, cough, expectoration, fatigue, rhinorrhea and nasal congestion remained more than 19% on day 8, which was similar to the results of Song et al's study that “cough can last for several weeks or months after SARS-CoV-2 infection,30 and the incidence of cough is still 2.5% after 1 year”.31
Our current study contributes some scientific value to the estimation of time-point prevalence in epidemiological study. From day 1 to day 8, there were 3,10,10,17,24,32,49 and 76 asymptomatic persons in 493 infected people, respectively. The time-point asymptomatic rate gradually increased from 0.61% to 15.42% on the eighth day, showing a dynamic trend. In order to solve the problem of different asymptomatic rates, some scholars suggest replacing “asymptomatic” with “latent period”,32 but such a description is still not accurate enough, because in addition to the latent period of infection also includes the real asymptomatic infection, if people do not observe the whole infection process and only understand the asymptomatic situation at a certain time point, they will not be able to effectively distinguish the real asymptomatic infection and incubation period infection. Therefore, to correctly apply the “asymptomatic rate”, it is necessary to distinguish between the “Time-point asymptomatic rate” at a certain time point and the “period asymptomatic rate” within a certain time period. For example, the time-point asymptomatic rate during nucleic acid detection is the asymptomatic rate at the time point of nucleic acid detection. It is understandable that the time-point asymptomatic rate can vary. The asymptomatic rate within a specific period (period) is period asymptomatic rate, such as the 8-day asymptomatic rate and the whole asymptomatic rate, which reflects the degree of harm of the disease and is the inherent characteristic of the disease. Distinguishing the differences between the two can reduce the possible misreading and misunderstanding in and out of the public and even avoid the misjudgment and mistake of the prevention and control policies of the decision-making departments. In order to more accurately and comprehensively describe the change rule of disease symptoms, it is recommended that time-point asymptomatic rate and “period asymptomatic rate” including “total asymptomatic rate” be combined in the study of disease symptoms.
Demographic factors also impacted the occurrences of COVID-related symptoms. Our results showed that cough, sore throat, nasal congestion, and eye pain were affected by many factors (≥5). Age, education, occupation, the number of vaccines dosages, gender, smoking, and medication use influenced many symptoms (≥4). Among the influencing factors, medication use was positively correlated with the onset of fever, chills, fatigue, backache, cough, nasal congestion, hypogeusia and headache, and was positively correlated with the duration of fever, sore throat, rhinorrhea, and eye pain. It may be that patients with more symptoms and longer duration are more likely to use drugs during the COVID-19 epidemic. Gender and the number of vaccines dosages can increase the incidence of at least five symptoms; Older infected people are less likely to have fever, sore throat, nasal congestion, and rhinorrhea, but are more likely to have fatigue and backache. These factors may be real, some results have been confirmed by studies showing that, for example, in patients with mild symptoms of SARS-CoV-2 infection, hyposmia or hypogeusia appears to be more common in women.33 Another systematic review has shown that among people infected with COVID-19, the incidence of hyposmia or hypogeusia declines with age and is less common in men.28 Even so, we found a lower incidence of symptoms in men and older infected people, which does not mean the disease will be milder. Two systematic reviews34,35 and cohort studies from Wuhan36 have shown that infected men or older people are more likely to develop severe or critical illness and even die.
However, there are three main limitations to this study: First, we could not fully determine which virus variant the patients carried. However, from December 1, 2022, to January 30, 2023, the Chinese Center for Disease Control and Prevention reported the effective genome sequence of 11,311 local COVID-19 cases, all of which were Omicron mutant strains, with a total of 26 evolutionary branches, and the main prevalent variants were BA.5.2.48 (62.8%) and BF.7.14 (26.95%).24 Da Huo et al indicated that there are no substantial differences in clinical manifestations, duration of illness, healthcare-seeking behaviors, or treatment between these two subvariants.37 Second, although online surveys (also known as web surveys or Internet surveys) can provide a quick, easy, and inexpensive way to obtain information, allowing researchers to collect a large amount of data in a short period of time, it will generate certain biases in the survey population included in the study. For example, people who know the Internet and are concerned about COVID-19 are more likely to participate, while other groups are less likely to respond or even have no response, such as the elderly, or even people who are seriously ill or died. There were fewer older participants in the study (age range 20 to 72 years, median age 33 years). This results in a lack of information about severity and comorbidities, as the characteristic of Omicron is attenuated pathogenicity38 and vaccination is widespread in China today.7 However, the constituent ratio of infected people aged 19–60 years and ≥61 years in China were 39.49% and 34.91%, respectively,24 which were relatively close, so the bias in this study was estimated to be less than 5%. Finally, since nucleic acid screening tests will no longer be carried out in mainland China after December 8, 2022, some infected persons in this study were diagnosed only based on symptoms, which may lead to certain misclassification bias. However, comparing the data from five sources (number of positive nucleic acid tests, resident antigen detection information collection APP (APP), number of patients in fever clinics (consulting rooms) in China, weekly influenza-like cases (body temperature ≥38°C, accompanied by cough or sore throat) in sentinel hospitals, and simultaneous detection of COVID-19 and influenza virus in influenza-like case specimens in online laboratories),39 the infections of the participants in this study in December 2022 were consistent with those in the real world, that is, they were concentrated in the middle and late December, so the bias of diagnostic misclassification could be basically ignored (see Table S5). In summary, although there may be some unavoidable information bias, the results of this study, as an immediate and specific cross-sectional survey during the COVID-19 epidemic in China, are still accurate and reliable, and we also have effectively controlled recall bias (collecting symptom information for 8 days within 1 month after the adjustment of prevention and control policy). Most importantly, in the context of the relative lack of research on the dynamic changes of COVID-19 clinical symptoms,40 the concepts of “Time-point asymptomatic rate” and “Period-asymptomatic rate” timely proposed in this study fill in some gaps in the study of clinical characteristics of COVID-19 (infectious disease) infected people in the real world, which is conducive to the government to grasp a more real epidemic situation.
Conclusion
In our quick and inexpensive online study, most current COVID patients (90%) developed clinical symptoms during current survey period, and time-point asymptomatic rate showed a dynamic change among the infected population. Clinical practitioners can benefit from onset patterns of symptom occurrences orders and magnitudes. Decision-makers could develop sound public health measures and strategies.
Data Sharing Statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The present study was conducted after the approval of the institutional review board of the Medicine School of Jinan University and adhered to the guidelines outlined in the Declaration of Helsinki. All patient data were anonymized.
Acknowledgments
The authors would like to thank Dr Zhiyong Hong at Public Health Agency of Canada, Professor Qingshan Chen and Associate Professor Dalin Lu at Department of Epidemiology of Medicine School of Jinan University for their technical support and guidance. In particular, the concepts of “Time-point asymptomatic rate” and “Period asymptomatic rate” first proposed by Professor Qingshan Chen are the innovation and motivation of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Key-Area Research and Development Program of Guangdong Province (No. 2019B111103001) and the National Natural Science Foundation of China (grant number: 82003522).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81(2):e16–e25. doi:10.1016/j.jinf.2020.04.021
2. Lane A, Hunter K, Lee EL, et al. Clinical characteristics and symptom duration among outpatients with COVID-19. Am J Infect Control. 2022;50(4):383–389. doi:10.1016/j.ajic.2021.10.039
3. World Health Organizatio. IHR emergency committee on novel coronavirus; 2019.
4. National Health Commission of the People’s Republic of China. As of 24:00 on February 23, 2022, the latest situation of the novel coronavirus pneumonia epidemic; 2022.
5. World Health Organization. Weekly epidemiological update on COVID-19 - 20 April 2023; 2023.
6. World Health Organization. WHO Coronavirus (COVID-19) Dashboard; 2023.
7. Chinese Center for Disease Control and Prevention. Situation of Novel coronavirus infection in China; 2020.
8. Sarkar A, Omar S, Alshareef A, et al. The relative prevalence of the Omicron variant within SARS-CoV-2 infected cohorts in different countries: a systematic review. Hum Vaccin Immunother. 2023;19(1):2212568. doi:10.1080/21645515.2023.2212568
9. Ling MS, Wang CP, Hsieh YL, et al. Emotional disturbance and risk factors among COVID-19 confirmed cases in isolation hotels. Int J Ment Health Nurs. 2023;32(2):469–478. doi:10.1111/inm.13063
10. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
11. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. doi:10.1016/j.tmaid.2020.101623
12. Chen C, Zhu C, Yan D, et al. The epidemiological and radiographical characteristics of asymptomatic infections with the novel coronavirus (COVID-19): a systematic review and meta-analysis. Int J Infect Dis. 2021;104:458–464. doi:10.1016/j.ijid.2021.01.017
13. World Health Organization. Coronavirus disease (COVID-19): how is it transmitted?; 2021.
14. Ma Q, Liu J, Liu Q, et al. Global percentage of asymptomatic SARS-CoV-2 infections among the tested population and individuals with confirmed COVID-19 diagnosis: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(12):e2137257. doi:10.1001/jamanetworkopen.2021.37257
15. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi:10.1056/NEJMoa2002032
16. Shi Y, Wang G, Cai XP, et al. An overview of COVID-19. J Zhejiang Univ Sci B. 2020;21(5):343–360. doi:10.1631/jzus.B2000083
17. Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi:10.1016/S1473-3099(20)30086-4
18. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi:10.1016/S0140-6736(20)30211-7
19. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi:10.1016/S2213-2600(20)30079-5
20. Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ. 2020;369:m1375. doi:10.1136/bmj.m1375
21. Gao Z, Xu Y, Sun C, et al. A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect. 2021;54(1):12–16. doi:10.1016/j.jmii.2020.05.001
22. Lee N, Hui D, Wu A, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348(20):1986–1994. doi:10.1056/NEJMoa030685
23. Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13(9):752–761. doi:10.1016/S1473-3099(13)70204-4
24. Wang S, Niu P, Su Q, et al. Genomic Surveillance for SARS-CoV-2 - China, September 26, 2022 to January 29, 2023. China CDC Wkly. 2023;5(7):143–151. doi:10.46234/ccdcw2023.026
25. Kariyawasam JC, Jayarajah U, Riza R, Abeysuriya V, Seneviratne SL. Gastrointestinal manifestations in COVID-19. Trans R Soc Trop Med Hyg. 2021;115(12):1362–1388. doi:10.1093/trstmh/trab042
26. Klimek L, Hagemann J, Döge J, et al. Olfactory and gustatory disorders in COVID-19. Allergo J Int. 2022;31(7):243–250. doi:10.1007/s40629-022-00216-7
27. Borsetto D, Hopkins C, Philips V, et al. Self-reported alteration of sense of smell or taste in patients with COVID-19: a systematic review and meta-analysis on 3563 patients. Rhinology. 2020;58(5):430–436. doi:10.4193/Rhin20.185
28. von Bartheld CS, Hagen MM, Butowt R. Prevalence of chemosensory dysfunction in COVID-19 patients: a systematic review and meta-analysis reveals significant ethnic differences. ACS Chem Neurosci. 2020;11(19):2944–2961. doi:10.1021/acschemneuro.0c00460
29. Aziz M, Goyal H, Haghbin H, Lee-Smith WM, Gajendran M, Perisetti A. The Association of “Loss of Smell” to COVID-19: a systematic review and meta-analysis. Am J Med Sci. 2021;361(2):216–225. doi:10.1016/j.amjms.2020.09.017
30. Song WJ, Hui CKM, Hull JH, et al. Confronting COVID-19-associated cough and the post-COVID syndrome: role of viral neurotropism, neuroinflammation, and neuroimmune responses. Lancet Respir Med. 2021;9(5):533–544. doi:10.1016/S2213-2600(21)00125-9
31. Fernández-de-Las-Peñas C, Guijarro C, Plaza-Canteli S, Hernández-Barrera V, Torres-Macho J. Prevalence of post-COVID-19 cough one year after SARS-CoV-2 infection: a multicenter study. Lung. 2021;199(3):249–253. doi:10.1007/s00408-021-00450-w
32. Oran DP, Topol EJ. The proportion of SARS-CoV-2 infections that are asymptomatic: a systematic review. Ann Intern Med. 2021;174(5):655–662. doi:10.7326/M20-6976
33. Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA. 2020;323(20):2089–2090. doi:10.1001/jama.2020.6771
34. Barek MA, Aziz MA, Islam MS. Impact of age, sex, comorbidities and clinical symptoms on the severity of COVID-19 cases: a meta-analysis with 55 studies and 10014 cases. Heliyon. 2020;6(12):e05684. doi:10.1016/j.heliyon.2020.e05684
35. Jain V, Yuan JM. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int J Public Health. 2020;65(5):533–546. doi:10.1007/s00038-020-01390-7
36. Pan A, Liu L, Wang C, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1915–1923. doi:10.1001/jama.2020.6130
37. Huo D, Yu T, Shen Y, et al. A Comparison of clinical characteristics of infections with SARS-CoV-2 Omicron Subvariants BF.7.14 and BA.5.2.48 - China, October-December 2022. China CDC Wkly. 2023;5(23):511–515. doi:10.46234/ccdcw2023.096
38. Suzuki R, Yamasoba D, Kimura I, et al. Attenuated fusogenicity and pathogenicity of SARS-CoV-2 Omicron variant. Nature. 2022;603(7902):700–705. doi:10.1038/s41586-022-04462-1
39. Chinese Center for Disease Control and Prevention. COVID- 19 clinical and surveillance data--Dec 9, 2022 to Jan 23, 2023, China; 2023.
40. Liao CX, Wang B, Lyu J, Li LM. 新型冠状病毒Omicron变异株病原学及流行病学研究进展 [Progress in research of etiology and epidemiology of 2019-nCoV Omicron variant]. Zhonghua Liu Xing Bing Xue Za Zhi. 2022;43(11):1691–1698. Chinese. doi:10.3760/cma.j.cn112338-20220929-00829
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
