Back to Journals » International Journal of General Medicine » Volume 16
Analysis of Inter-Eye Vault Differences After Implantable Collamer Lens (V4c) Implantation
Authors Tan X, Liu W, Chang Y, Wu W, Yang L, Liu J
Received 3 April 2023
Accepted for publication 12 June 2023
Published 16 June 2023 Volume 2023:16 Pages 2451—2459
DOI https://doi.org/10.2147/IJGM.S384858
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xin Tan, Wenjie Liu, Ying Chang, Wanmin Wu, Lichun Yang, Jiewei Liu
Cataract Department, Shanxi Eye Hospital, Taiyuan, Shanxi Province, People’s Republic of China
Correspondence: Jiewei Liu, Cataract Department, Shanxi Eye Hospital, Taiyuan, Shanxi Province, People’s Republic of China, Tel +86-13834648535, Email [email protected]
Purpose: The safety and stability of implantable collamer lens (ICL) implantation are closely related to the vault. We aimed to assess clinical data from patients with similar anterior segment anatomy who received ICL of the same model placed in the same position and analyze common range and factors affecting the vault inter-eye difference.
Patients and Methods: A prospective study was performed, including 162 eyes of 81 patients with a bilateral ICL (V4c) implantation. Subjects were evaluated before the surgery and 1 day, 1 week, and 1 month postoperatively, and they were divided into 4 groups based on the ICL size. Bivariate correlation and multiple linear regression (stepwise) analyzed associations between vault inter-eye differences and horizontal sulcus-to-sulcus diameter, anterior chamber depth, lens thickness, ICL size, spherical equivalent, and vault.
Results: One month after surgery, mean vault inter-eye differences were 74.59 ± 55.59 μm. Nearly 70% of patients presented with vault inter-eye differences lower than 100 μm. The second eye vault variance of 69% was attributed to the first eye vault. Vault inter-eye differences were positively correlated with ICL spherical equivalent (regression equation: vault inter-eye differences (μm) = 139.415 + 6.295 × ICL spherical equivalent). Vaults after ICL implantation were similar in fellow eyes, with some considerable differences. The 95% confidence interval of the vault inter-eye difference was − 34.4 ~ 183.6 μm.
Conclusion: In eyes with similar anterior segment anatomy, there is a 95% probability that the vault will vary from − 34.4 μm to − 183.6 μm when a similar ICL is implanted. These results can help surgeons to select an appropriate ICL size to achieve an ideal vault. The smaller the spherical equivalent, the larger the difference between the two vaults, which provides a reference for size in moderate myopia. ICL spherical equivalent affects and predicts vault inter-eye differences after ICL implantation.
Keywords: implantable collamer lens, vault, inter-eye differences
Introduction
With extensive developments in refractive surgery in China, implantable collamer lenses (ICLs) have gradually become popular. High myopia and astigmatism can be effectively treated with the implantation of an ICL.1,2 The ICL is implanted between the posterior iris and the anterior surface and anterior suspensions of the lens capsule and is fixed to the ciliary sulcus by loops.3
The vault is the vertical distance between the posterior surface of the ICL and the anterior surface of the lens. Studies show that when the vault is <250 μm it increases the risk of postoperative cataract formation,4,5 while >750 μm increases the risk of angle closure, pupillary block, and pigment-dispersed glaucoma.6,7 Therefore, Montés-Micó et al8 suggest that the optimal vault is between 250 μm and 750 μm. To reduce the occurrence of complications after ICL implantation, many experts and scholars have proposed formulas to predict the vault.9,10 Kojima et al11 added the ACD and the distance between the sulcus-to-sulcus plane and the anterior surface of the lens as variables and obtained the K-formula, which was significantly better than the traditional STAAR formula for predicting postoperative vault. Igarashi et al12 concluded that the angle-to-angle measurements had higher reproducibility than the white-to-white measurements on AS-OCT, making it a more important predictor of postoperative vault. Nakamura et al obtained the NK formula by incorporating anterior chamber width and crystalline lens rise into the calculation of ICL size, which greatly improved the proportion of the ideal postoperative vault.13,14
Kamiya et al,15 Martinez et al,16 and Cerpa et al17 concluded that the vault obtained in both eyes was highly correlated. We aimed to measure the clinical data of patients with similar anterior segment anatomy who were implanted with ICLs of the same model placed in the same position and analyze the common range and factors affecting the vault inter-eye difference.
Materials and Methods
Patients
Patients who underwent bilateral ICL/TICL (EVO-V4c, STAAR Surgical AG, Nidau, Switzerland) at Shanxi Eye Hospital between March and September 2022 were included as per the following criteria: (1) aged 18 to 51 years; (2) myopia higher than −3.0 D, astigmatism lower than −5.0 D, and annual diopter change ≤0.50 D for two consecutive years; (3) anterior chamber depth (ACD) ≥2.8 mm; (4) corneal endothelial cell count ≥2000/mm2 and stable cell morphology; (5) ACD difference ≤0.2 mm in both eyes, white-to-white distance (WTW) difference ≤0.4 mm, spherical equivalent (SE) of ICL <10 D, horizontal sulcus-to-sulcus (hSTS) of both eyes <1 mm, lens thickness (LT) of both eyes <1 mm; (6) same type and size of ICL implanted in both eyes and the implantation axis for spherical lenses within 10° of horizontal deviation. We excluded patients as per the following criteria: (1) glaucoma, uveitis, diabetic retinopathy, pigment dissemination, and pseudo-exfoliation syndrome; (2) other ocular surgery; (3) autoimmune diseases (such as systemic lupus erythematosus) or mental diseases; (4) lactating or pregnant patients; and (5) patients who lacked data or did not cooperate with the examination. The Medical Ethics Committee at Shanxi Eye Hospital approved this study, which was conducted according to the Declaration of Helsinki principles.
Preoperative Examination
All patients underwent a series of ocular examinations before surgery, including uncorrected distance visual acuity (UDVA), best-corrected distance visual acuity (BDVA), subjective and objective refraction, slit-lamp assessment of the anterior segment anatomy, intraocular pressure, mydriasis, ocular ultrasound, corneal endothelial cell count, and optical coherence tomography (OCT). A Pentacam (HR, OCULUS Optikgeräte GmbH, Wetzlar, Germany) was used to measure WTW, corneal curvature, ACD, and anterior chamber volume. An IOL Master 700 (Carl Zeiss Meditec, Jena, Germany) was used to measure the axial length, LT, and WTW. Horizontal and vertical sulcus-to-sulcus ratios were measured using ultrasound bio-microscopy (Suowei Electronic Technology Co, Tianjin, China).
Size Selection of ICL
The ICL/TICL is a single flat, concave lens made of a collamer, which is highly biocompatible, absorbs ultraviolet light, and is foldable. The V4C lenses used at the institute have a central aperture. The optical area has a central aperture of 0.36 mm, allowing aqueous humor to enter the anterior chamber directly through the central aperture, thus avoiding a preoperative iridotomy, and can maintain the normal physiological environment of the eye. ICL/TICL comes in four sizes: 12.1 mm; 12.6 mm; 13.2 mm; and 13.7 mm. The sphere diopter of ICL was −0.5 ~ −18.0 D, and the cylinder diopter of TICL was −0.5 ~ −6.0 D. Preoperative refraction, corneal curvature K 1 and K 2, ACD, and WTW from Pentacam were entered into the Online Calculator and Ordering System (OCOS) (https://evo-ocos.staarag.ch/live/). The diopter, astigmatism, axial, and size of ICL/TICL were calculated. Horizontal and vertical sulcus-to-sulcus and the size, location, and number of iris cysts were considered to select the ICL/TICL size.
Surgical Technique
The same surgeon performed all the surgeries on two different days, with the right eye as the first operated eye. The ICL/TICL implantation was performed using a standard procedure. TICL implantation patients also underwent axial labeling under a slit-lamp microscope before mydriasis. The limbal incision was made at the position of 120° after routine disinfection and topical anesthesia. After the ICL/TICL was pushed into the anterior chamber, an appropriate amount of viscoelastic agent was injected into the upper ICL/TICL, and a positioning hook was used to adjust the ICL/TICL in the posterior chamber. If an ICL was implanted, we adjusted to the center position; if TICL, we adjusted to the planned axis position according to the localization chart and corneal marker. A washing needle was used to wash the viscoelastic agent in the anterior chamber, and the incision was closed using water.
Antibiotic and corticosteroid drugs were dropped into the conjunctival sac. The intraocular pressure (IOP), the position of the ICL/TICL, and the reaction of the anterior chamber were measured 2 h after surgery. No intra-operative complications were observed.
Postoperative Examination
The same physician performed all examinations at one day, week, and month after surgery. We examined visual acuity (UDVA and BDVA), intraocular pressure, and slit-lamp microscopy. Anterior segment OCT (AS-OCT) (RTVue100, Zeiss Meditec AG, Jena, Germany) was performed to measure the vault under dark ambient illumination (0.5 lux). The patient’s gaze and scan status were monitored using a screen to ensure that the scanning site was at the center of the cornea. The vault was measured vertically from the posterior surface of the ICL to the anterior surface of the lens. Inter-eye vault difference was recorded between the vaults of the first and second eyes. The 95% confidence interval (CI) was mean ± 1.96 standard deviation (SD). The two ophthalmologists analyzed the measurements’ accuracy, which was performed using the instrument’s own measurement software (Figure 1).
 |
Figure 1 AS-OCT measurements of the bilateral vault. The vault is the vertical distance from the posterior surface of the ICL to the anterior surface of the lens. |
Statistical Analysis
SPSS v26.0 (IBM Corp., Armonk, NY, USA) was utilized for all statistical analyses. All results are provided as mean ± SD. The Kolmogorov–Smirnov test was used to determine the normality of the data. The paired sample t-test and the Kruskal–Wallis rank test were used when the data samples were not normally distributed. Pearson’s test was used to test the correlation with normal distribution, and Spearman’s test was used to test the correlation with non-normal distribution. Multivariate linear regression (stepwise method) was applied to determine the influence of the parameter’s magnitude (RE and LE average: horizontal sulcus-to-sulcus diameter, anterior chamber depth, lens thickness, ICL size, spherical equivalent, and vault) on the absolute vault ΔE, to understand whether parameters’ magnitude influenced the vault ΔE. The intraclass correlation coefficient (ICC) was used to test the consistency of the parameters between the left and right eyes. P < 0.05 was deemed statistically significant.
Results
Eighty-one patients (162 eyes) with a mean age of 27.3 ± 6.7 years (range, 19–51 years) were included in the analysis, comprising 22 men and 59 women (Table 1). In either the right or left eye, there was no significant difference in the ICL SE, ACD, hSTS, or LT (P > 0.05). There was high agreement between the measurements of the right eyes and the left eyes (ICC range: 0.79 ~ 0.97) (Table 2). According to Spearman correlation analysis, ICL SE, and vault ΔE had a positive correlation one month after surgery (r = 0.301, P = 0.006), but ACD, hSTS, and LT did not correlate with vault ΔE one month after surgery (P > 0.05).
 |
Table 1 Demographic Summary of the Sample After Similarity Control Between Fellow Eyes |
 |
Table 2 Pre- and Postoperative Anatomical and Lens Parameters After Control Between Fellow Eyes |
According to the ICL/TICL size, the patients were divided into four groups: 12.1 mm group (N = 15); 12.6 mm group (N = 47); 13.2 mm group (N = 18); and 13.7 mm group (N = 1). The mean values of vault ΔE in the 12.1 mm group, 12.6 mm group, and 13.2 mm group were 89.2 ± 70.0 μm, 63.8 ± 46.8 μm, and 85.58.8 μm, respectively. The 95% CI of vault ΔE of the three groups was −48 to 226.4 μm, −27.9 to 155.5 μm, and −29.8 to 200.8 μm, respectively; however, the vault ΔE of the three groups did not differ significantly (Kruskal–Wallis χ2 = 4.393, P = 0.222). Only one patient was in the 13.7 mm group, with a vault ΔE of 166 μm.
Right and left eyes had similar vaults at one day, week, or month after surgery (P > 0.05) (Table 2). As a result of Pearson correlation analysis, there was a positive correlation between the left and right eye vaults at one month after surgery (R = 0.83, P < 0.05); the right eye vault could be predicted by the left eye vault in 69% of patients.
Bland–Altman plots showed no correlation between vault ΔE and bilateral vault at one month after surgery (r = 0.005, P = 0.961) (Figure 2). The mean ΔE of the vault was 74.59 ± 55.59 μm, and the 95% CI was −34.4 ~ 183.6 μm one month after surgery (Figure 3).
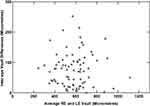 |
Figure 2 Correlation between the average right eye and left eye vault and inter-eye vault differences. |
 |
Figure 3 Histogram of the inter-eye absolute vault differences 1 month after ICL/TICL implantation. |
According to the vault of the first eye, the patients were divided into three groups: low vault group (<250 μm), optimal vault group (250 ~ 750 μm), and high vault group (>750 μm).10 According to the vault of the first eye one month after surgery, the patients were divided into the low vault (N = 1), optimal vault (N = 72), and high vault (N = 8) groups. The mean of vault ΔE of the right eye was 74.59 ± 55.59 μm. There was only one patient in the low vault group, with a vault ΔE of 81 μm. The mean of vault ΔE in the optimal vault group and high vault group was 74.21 ± 55.37 μm and 77.25 ± 64.84 μm, respectively, with 95% CIs of −34.3 ~ 182.7 μm and −49.8 ~ 204.3 μm, respectively. There were no significant differences between the two groups in vault ΔE (Kruskal–Wallis χ2 = 0.107, P = 0.948) (Figure 4).
 |
Figure 4 Inter-eye vault differences for all cases, divided into three vault ranges. Box edges represent the limits of the 25% and 75% quartiles, and lines inside the boxes represent the median. |
In all patients, the difference of vault was <50 μm in 42% and <100 μm in 70.4%. The difference in the vault in the low vault group was <100 μm. In the optimal vault group, the vault difference below 50 μm accounted for 41.7%, and the vault difference below 100 μm accounted for 72.2%. In the high vault group, the vault difference below 50 μm accounted for 50%, and the vault difference below 100 μm accounted for 50% (Table 3).
 |
Table 3 Cumulative Percentage of Inter-Eye Vault Differences |
Multiple regression analyses of the relative factors of vault ΔE one month after surgery were used as independent variables, and the mean of ICL SE, ACD, hSTS, LT, size, and bilateral vault were used as dependent variables. The results showed that ICL SE influenced vault ΔE (partial regression coefficient B = 6.295, standard regression coefficient β = 0.279, P = 0.012, 95% CI: 1.446~11.144), and the other factors had no statistical significance (all P > 0.05). The regression equation is represented as follows: vault ΔE (μm) = 139.415 + 6.295 × SE; the fitting degree of the formula is R = 0.279, R2 = 0.078, correction R2 = 0.066 (Figure 5).
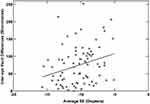 |
Figure 5 Association between average SE and inter-eye vault differences after implantable collamer lens implantation. |
Discussion
We retrospectively analyzed the data of 81 patients one month after ICL implantation to determine the expected range of the difference and identify the factors affecting the difference. The vault was reported to be stable one month after ICL implantation.18 Through correlation and regression analyses, we found that the vaults of eyes with similar anatomy were similar. The result is similar to the study of Martínez‑Plaza et al16 who reported that the vault obtained in the second implanted eye was highly related to the vault observed in the first one during the whole follow-up. However, the mean ΔE of the vault was 74.59 ± 55.59 μm, and the 95% CI was −34.4 ~ 183.6 μm one month after surgery. Schmidinger et al19 reported the mean and range of vault ΔE consistent with our study.
The current vault prediction formulas9–14 rely solely on preoperative biometry and lens parameters, which may need to be supplemented by additional factors. Currently, the prediction of the vault in the eyes is limited to 81%.20–22 It is suggested that some factors affect the vault. One of them may regard unilateral iridociliary cysts. According to a study, 36.1% of patients with myopic ICL had cysts; approximately 80% were unilateral.23 Although the central vault did not differ between eyes with and without cysts, the average vault in eyes with cysts was 100μm higher than in eyes without. The resting position of ICL haptics in the posterior chamber is another factor contributing to inter-eye differences. Due to a larger sulcus-to-sulcus distance, haptics resting in the sulcus may present a lower compression. The degree of forward bulging of ICL varies due to different compression forces that, in turn, will affect the vault. Choi et al24 and Elshafei et al25 reported that 64.7% and 78.9% of their lenses, respectively, rested on the ciliary sulcus; moreover, Kojima et al26 reported that 35.3% rested on the ciliary body. Therefore, even if the same ICL size is implanted in both eyes, there will be a difference in the vault.
The correlation between vault ΔE and the vault was r = 0.005 (P = 0.961), indicating that the vault of both eyes did not affect the difference of vault between both eyes. However, according to the 95% CI of the three groups, the difference between the vault of the two eyes increases with an increase in the vault of the two eyes. The results of Cerpa et al17 showed that the mean vault ΔE of the low, optimal, and high vault groups were significantly different. Compared with the low- and optimal vault groups, the high vault group had a larger vault ΔE. Their results showed the same trend as the results of this study in that the vault was higher than the optimal range, and the difference between the two vaults was greater.
It did not appear that vault ΔE among ICL/TICL size groups in this study differed significantly, and the means and ranges were similar among the four groups. The results of Cerpa et al17 were the same as those of the present study. However, their results showed that the larger the size of the ICL implantation, the greater the difference in the vault.
Spearman correlation analysis showed that ICL SE positively correlated with the difference in the binocular vault one month after surgery (P < 0.05). Multiple linear stepwise regression analysis revealed the following results: ICL SE was an independent factor (P < 0.05), and ICL SE could cause a change of 6.3 μm vault difference with every change of −1 D. This may be because, compared with the high-diopter ICL, the periphery of the low-diopter ICL is thinner, which makes the ICL-iris diaphragm move forward more, and the vault changes significantly. Xiong et al27 and Xu et al28 demonstrated that the ICL SE is negatively correlated with the vault after ICL/TICL implantation. The smaller the ICL SE, the higher the vault after ICL/TICL implantation. It is inferred that the less myopic, the higher the binocular vault and the greater the difference thereof.
The AS-OCT was performed to measure the vault under dark ambient illumination (0.5 lux) in the study. The changes in pupil diameter under different light conditions after the implantation of an ICL are related to the postoperative vault.29,30 All patients were measured in the same illumination to avoid errors from different light conditions.
This study had some limitations. First, there was only one case in the low vault group without statistical analysis. Second, there was only one case in the 13.7 mm size group without statistical analysis. Third, the vault was measured only once per eye per follow-up rather than the average of the three measures. Small differences in the AS-OCT scan location likely affected the accuracy of the vault measurement. However, the examinations were performed by the same physician. Fourth, the maximum follow-up was 1 postoperative month. There is a lack of long-term follow-up, and the long-term effect needs further study. Finally, this study involved a limited number of patients, and the results may have been biased.
Conclusion
This study showed that in eyes with similar anatomic structures in the anterior segment, there is a 95% probability that the vault will vary from −34.4 μm to −183.6 μm at 1 month postoperatively when a similar ICL is implanted. These results can help surgeons select an appropriate ICL size to achieve an ideal vault. The smaller the SE, the larger the difference between the two vaults, which provides a reference for selecting the ICL size in moderate myopia.
Abbreviations
ACD, Anterior chamber depth; BDVA, Best-corrected distance visual acuity; BCVA, Best-corrected visual acuity; CI, Confidence interval; ICC, Intraclass correlation coefficient; ICL, Implantable Collamer Lens; LT, Lens thickness; OCT, Optical coherence tomography; SD, Standard deviation; SE, Spherical equivalent; UDVA, Uncorrected distance visual acuity; WTW, White-to-white.
Data Sharing Statement
The datasets used and /or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Medical Ethics Committee of Shanxi Eye Hospital and was conducted in accordance with the principles of the Declaration of Helsinki. Patients provided informed consent on admission to hospital that their deidentified data may be used for research.
Funding
Supported by the Science Foundation of Health and Family Planning Commission of Shanxi Province (2021097).
Disclosure
Xin Tan, Wenjie Liu, Ying Chang, Wanmin Wu, Lichun Yang, and Jiewei Liu declare that they have no conflict of interest.
References
1. Sanders DR, Doney K, Poco M.; ICL in Treatment of Myopia Study Group. United States food and drug administration clinical trial of the implantable collamer lens (ICL) for moderate to high myopia: three-year follow-up. Ophthalmology. 2004;111(9):1683–1692.
2. Sanders DR, Schneider D, Martin R, et al. Toric implantable collamer lens for moderate to high myopic astigmatism. Ophthalmology. 2007;114(1):54–61. doi:10.1016/j.ophtha.2006.08.049
3. Reinstein DZ, Lovisolo CF, Archer TJ, Gobbe M. Comparison of postoperative vault height predictability using white-to-white or sulcus diameter-based sizing for the Visian implantable collamer lens. J Refract Surg. 2013;29(1):30–35. doi:10.3928/1081597X-20121210-02
4. Gimbel HV, LeClair BM, Jabo B, Marzouk H. Incidence of implantable Collamer lens-induced cataract. Can J Ophthalmol. 2018;53(5):518–522. doi:10.1016/j.jcjo.2017.11.018
5. Guber I, Mouvet V, Bergin C, Perritaz S, Othenin-Girard P, Majo F. Clinical outcomes and cataract formation rates in eyes 10 years after posterior phakic lens implantation for myopia. JAMA Ophthalmol. 2016;134(5):487–494. doi:10.1001/jamaophthalmol.2016.0078
6. Chun YS, Park IK, Lee HI, Lee JH, Kim JC. Iris and trabecular meshwork pigment changes after posterior chamber phakic intraocular lens implantation. J Cataract Refract Surg. 2006;32(9):1452–1458. doi:10.1016/j.jcrs.2006.04.023
7. Ye C, Patel CK, Momont AC, Liu Y. Advanced pigment dispersion glaucoma secondary to phakic intraocular collamer lens implant. Am J Ophthalmol Case Rep. 2018;10:65–67. doi:10.1016/j.ajoc.2018.01.046
8. Montés-micó R, Ruiz-Mesa R, Rodríguez-prats JL, et al. Posterior-chamber phakic implantable collamer lenses with a central port: a review. Acta Ophthalmol. 2021;99(3):e288–e301. doi:10.1111/aos.14599
9. Dougherty PJ, Rivera RP, Schneider D, et al. Improving accuracy of phakic intraocular lens sizing using high-frequency ultrasound biomicroscopy. J Cataract Refract Surg. 2011;37(1):13–18. doi:10.1016/j.jcrs.2010.07.014
10. Packer M. Meta-analysis and review: effectiveness, safety, and central port design of the intraocular collamer lens. Clin Ophthalmol. 2016;10:1059–1077. doi:10.2147/OPTH.S111620
11. Kojima T, Yokoyama S, Ito M, et al. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. 2012;153(4):632–637, 637.e1. doi:10.1016/j.ajo.2011.06.031
12. Igarashi A, Shimizu K, Kato S, et al. Predictability of the vault after posterior chamber phakic intraocular lens implantation using anterior segment optical coherence tomography. J Cataract Refract Surg. 2019;45:1099–1104. doi:10.1016/j.jcrs.2019.02.020
13. Nakamura T, Isogai N, Kojima T, et al. Implantable collamer lens sizing method based on swept-source anterior segment optical coherence tomography. Am J Ophthalmol. 2018;187:99–107. doi:10.1016/j.ajo.2017.12.015
14. Nakamura T, Isogai N, Kojima T, et al. Optimization of implantable collamer lens sizing based on swept-source anterior segment optical coherence tomography. J Cataract Refract Surg. 2020;46(5):742–748.10. doi:10.1097/j.jcrs.0000000000000134
15. Kamiya K, Shimizu K, Ando W, Igarashi A, Iijima K, Koh A. Comparison of vault after implantation of posterior chamber phakic intraocular lens with and without a central hole. J Cataract Refract Surg. 2015;41(1):67–72. doi:10.1016/j.jcrs.2014.11.011
16. Martínez-Plaza E, López-Miguel A, López-de la Rosa A, Maldonado MJ. Inter-eye and postoperative prediction of vault after implantation of EVO + Visian phakic implantable collamer lens. Int Ophthalmol. 2022;43:1501–1510. doi:10.1007/s10792-022-02546-5
17. Cerpa Manito S, Sánchez Trancón A, Torrado Sierra O, Baptista AM, Serra PM. Inter-eye vault differences of implantable collamer lens measured using anterior segment optical coherence tomography. Clin Ophthalmol. 2020;14:3563–7353. doi:10.2147/OPTH.S258817
18. Kamiya K, Shimizu K, Kawamorita T. Changes in vaulting and the effect on refraction after phakic posterior chamber intraocular lens implantation. J Cataract Refract Surg. 2009;35(9):1582–1586. doi:10.1016/j.jcrs.2009.03.052
19. Schmidinger G, Lackner B, Pieh S, Skorpik C. Long-term changes in posterior chamber phakic intraocular collamer lens vaulting in myopic patients. Ophthalmology. 2010;117(8):1506–1511. doi:10.1016/j.ophtha.2009.12.013
20. Lee DH, Choi SH, Chung ES, et al. Correlation between preoperative biometry and posterior chamber phakic Visian Implantable Collamer Lens vaulting. Ophthalmology. 2012;119(2):272–277. doi:10.1016/j.ophtha.2011.07.047
21. Zheng QY, Xu W, Liang GL, et al. Preoperative biometric parameters predict the vault after ICL implantation: a retrospective clinical study. Ophthalmic Res. 2016;56(4):215–221. doi:10.1159/000446185
22. Lee H, Kang DSY, Choi JY, et al. Analysis of preoperative factors affecting range of optimal vaulting after implantation of 12.6-mm V4c implantable collamer lens in myopic eyes. BMC Ophthalmol. 2018;18:163. doi:10.1186/s12886-018-0835-x
23. Li Z, Xu Z, Wang Y, Liu Q, Chen B. Implantable collamer lens surgery in patients with primary iris and/or ciliary body cysts. BMC Ophthalmol. 2018;18(1). doi:10.1186/s12886-018-0935-7
24. Choi K, Chung SE, Chung TY, Chung ES. Ultrasound biomicroscopy for determining Visian implantable contact lens length in phakic IOL implantation. J Refract Surg. 2007;23(4):362–367. doi:10.3928/1081-597X-20070401-08
25. Elshafei AM, Genaidy MM, Moharram HM. In vivo positional analysis of implantable collamer lens using ultrasound biomicroscopy. J Ophthalmol. 2016;2016:4060467. doi:10.1155/2016/4060467
26. Kojima T, Maeda M, Yoshida Y, et al. Posterior chamber phakic implantable collamer lens: changes in vault during 1 year. J Refract Surg. 2010;26(5):327–332. doi:10.3928/1081597X-20090617-11
27. Xiong Y, Mao YY, Zhang Q, et al. Influencing factors of vault after implantable collamer lens with central port implantation. Ophthalmol China. 2020;29:448–452.
28. Xu J, Luo Y, Lin YN, Li Y. Changes in the central vault after collamer lens implantation and its impact. Chin J Optom Ophthalmol Vis Sci. 2016;18:714–718.
29. Gonzalez-Lopez F, Bouza-Miguens C, Tejerina V, et al. Dynamic assessment of variations in pupil diameter using swept-source anterior segment optical coherence tomography after phakic collamer lens implantation. Eye Vision. 2021;8(1). doi:10.1186/S40662-021-00262-2
30. Gonzalez-Lopez F, Bouza-Miguens C, Tejerina V, Mompean B, Ortega-Usobiaga J, Bilbao-Calabuig R. Long-term assessment of crystalline lens transparency in eyes implanted with a central-hole phakic collamer lens developing low postoperative vault. J Cataract Refract Surg. 2021;47(2):204–210. doi:10.1097/J.JCRS.0000000000000425
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
