Back to Journals » Journal of Inflammation Research » Volume 16
Analysis of Correlation Between Serum Oncostatin-M and Disease Severity and Mortality in Hospitalized Patients with Community-Acquired Pneumonia
Authors Teng P, Zhang X , Wang H, Han X , Liu X
Received 19 October 2023
Accepted for publication 12 December 2023
Published 21 December 2023 Volume 2023:16 Pages 6257—6269
DOI https://doi.org/10.2147/JIR.S445484
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Peikun Teng,1 Xingyu Zhang,2 Hong Wang,3 Xiudi Han,4 Xuedong Liu4
1General Medicine Dapartment, Qingdao Municipal Hospital, Qingdao, 266000, People’s Republic of China; 2Human Resources Department, Qingdao Municipal Hospital, Qingdao, 266000, People’s Republic of China; 3Hospital-Acquired Infection Control Department, Qingdao Municipal Hospital, Qingdao, 266000, People’s Republic of China; 4Department of Respiratory and Critical Care Medicine, Qingdao Municipal Hospital, Qingdao, 266000, People’s Republic of China
Correspondence: Xuedong Liu; Xiudi Han, Department of Respiratory and Critical Care Medicine, Qingdao Municipal Hospital, Qingdao, 266000, People’s Republic of China, Email [email protected]; [email protected]
Purpose: The aim of this study was to investigate the level of serum tumor suppressor factor (Oncostatin-M, OSM) in patients with community-acquired pneumonia (CAP) and evaluate its predictive value for the severity and prognosis of pneumonia, so as to improve the ability to identify the risk of death in CAP patients.
Patients and Methods: A total of 110 patients with CAP admitted to the hospital from November 2020 to November 2021 were enrolled in this prospective study. Clinical data of all patients were collected. According to the 2016 edition of “Guidelines for the Diagnosis and Treatment of Community-acquired Pneumonia in Chinese Adults”, the patients were divided into non-severe CAP (NSCAP)(n=55) and severe CAP (SCAP)(n=55). At the same time, they were divided into a survival group (n=96) and a death group (n=14) by tracking the survival of patients in the hospital. The OSM concentration of CAP patients on the first day after admission was determined by enzyme-linked immunosorbent assay. All clinical data were statistically and graphed using SPSS V23.0 and Grahpad Prim 8.
Results: Compared with NSCAP, patients with SCAP had higher serum OSM concentration on the day of admission, which was negatively correlated with LYM and positively correlated with WBC, NEU, CRP, IL-6, IL-8, IL-10, CURB-65 score, and PSI score. The level of OSM in the dead patient group was significantly higher than that in the surviving patient group. OSM and PSI scores were independent risk factors for in-hospital mortality in CAP patients. Kaplan-Meier survival curve showed that OSM≥ 76pg/mL was more advantageous in predicting mortality in patients with CAP.
Conclusion: The level of the OSM is closely related to the severity and prognosis of CAP and may be a new biomarker for the prognosis of CAP patients.
Keywords: community-acquired pneumonia, severity of disease, oncostatin-M, mortality
Introduction
Community-acquired pneumonia (CAP) is a common respiratory infectious disease, which is one of the main causes of high morbidity and mortality worldwide, especially in children and adults over 60 years of age. According to the retrospective data analysis of adult CAP cases in 23 provinces in 2016 by Cao Bin et al, the total incidence of CAP in China was 7.13 person-years per thousand.1 Despite the implementation of measures such as early vaccination and antimicrobial treatment, the high incidence and mortality of CAP still bring serious health problems and economic burdens to the world. Although pneumonia severity index (PSI) and confusion, urea, respiratory rate, blood pressure, and age 65 (CURB-65) score are widely used in clinical diagnosis, it is difficult to use them together due to the inconsistency, specificity or complexity of different scoring systems. Therefore, there is an urgent need for a new, rapid, and effective biomarker to identify the progression of mild pneumonia to severe CAP (SCAP), so as to reduce the mortality rate of CAP patients and improve the survival rate and the prognosis of patients.
Oncostatin-M (OSM), a pleiotropic-cytokine in the IL-6 family, was first released and isolated from U937 histiocytic lymphoma cells in 1986 and was named for its ability to inhibit the proliferation of melanoma cells.2,3 Previous literature has also reported that the secretion of OSM is involved in the immunopathogenesis of various tumors, and abnormal expression of this cytokine has been reported in various cancers.2,4–6 In addition, OSM is closely related to the pathogenesis of a variety of human inflammatory diseases, including inflammatory bowel disease,7,8 sepsis,9 acute intestinal ischemia-reperfusion injury,10 pulmonary interstitial fibrosis,11 etc. In recent years, studies on the regulatory mechanism of OSM in mouse models of pneumonia have become increasingly apparent.12–14 At the same time, in this convalescent and serum-antibody positive COVID-19 patient, the significant increase in serum OSM may be related to activated macrophage monocytes. Studies on the immune regulatory mechanisms of OSM in various signaling pathways in animal models are relatively mature. Many studies have confirmed that blocking OSM activity may reduce abnormal inflammatory damage, delay disease progression, and improve prognosis. However, studies on the level of serum OSM in pneumonia patients and its correlation with inflammatory indicators and prognosis are still scarce, and there is still a lack of relevant population epidemiological and laboratory research support.
Therefore, it is necessary to conduct this study to further detect the serum OSM level and evaluate its correlation with disease severity and prognosis of hospitalized CAP patients, which is expected to greatly improve the ability to identify the death risk of CAP patients and provide a certain reference value for clinical diagnosis and treatment.
Materials and Methods
Ethics
The protocol of this study was approved by the Ethics Committee of the Qingdao Municipal Hospital (Approval No. 2020CXJJ001-052). This study was in compliance with the Declaration of Helsinki and informed consent was obtained from all patients or their families before this study. For some patients with severe pneumonia, especially in cases of consciousness disturbance, tracheal intubation, etc., where the patient is unable to express his or her subjective will, the opinion of the immediate family (spouse, parents, or children) is sought and the consent of the hospital ethics committee is obtained.
Patients and Inclusion Criteria
This is a prospective study, whose subjects were hospitalized CAP patients who were finally diagnosed in the department of respiratory and critical care medicine, emergency ward, and ICU of Qingdao Municipal Hospital from November 2020 to November 2021.
The diagnostic criteria of all included subjects strictly met the Guidelines for the Diagnosis and Treatment of Community-Acquired Pneumonia in Chinese Adults (2016 revision).15 Patients with CAP had to meet criterion A, criterion C, and any one the conditions of criterion B to be included in the study. (A) Onset in the community setting. (B) Relevant clinical manifestations of pneumonia, including (1) new onset of cough or expectoration or aggravation of existing symptoms of respiratory tract diseases, with or without purulent sputum, chest pain, dyspnea, or hemoptysis; (2) fever; (3) signs of pulmonary consolidation and/or moist rales; and (4) peripheral white blood cell (WBC) count >10 × 109/L or <4 × 109/L, with or without a left shift. (C) Chest radiograph showing new patchy infiltrates, lobar or segmental consolidation, ground-glass opacities, or interstitial changes, with or without pleural effusion.
Severe pneumonia definition (Severe pneumonia was diagnosed if one of the following major criteria or three or more of the following minor criteria were met.):
Major criteria: 1) Mechanical ventilation with tracheal intubation is required; 2) Septic shock still requires vasoactive drug therapy after active fluid resuscitation. 2. Secondary criteria: 1) Respiratory rate ≥30 times/min; 2) Oxygenation index (PO2/FiO2) ≤250mmHg; 3) Multiple lung lobe infiltration; 4) Disturbance of consciousness and/or disorientation; 5) Blood urea nitrogen ≥7.14mmol/L; 6) Systolic blood pressure < 90mmHg requires active fluid resuscitation.
Exclusion criteria: 1) patients with hospital-acquired pneumonia or ventilator-associated pneumonia; 2) non-infectious diseases, such as pulmonary infarction, pulmonary interstitial disease, pulmonary vasculitis, tumor or pulmonary edema; 3) severely immunocompromised patients, including HIV infection, chemotherapy/radiotherapy within three to six months, 10 mg prednisone or equivalent per day for ≥ 2 weeks (receiving immunosuppressive therapy), active tuberculosis, organ/bone marrow transplantation, splenectomy, malignancy; 4) have been hospitalized within 4 weeks; 5) pregnant or lactating pregnant women; 6) use of antibiotics (including oral and intravenous fluids) in the 3 days prior to admission.
Data Collection
Clinical data of the patients were collected, including demographic data, clinical symptoms and signs, laboratory examination items (blood routine, C-reactive protein, biochemistry, procalcitonin, etc.) within 24 hours of admission, imaging features, treatment plan, and prognosis. At the same time, the corresponding CURB-65 score and PSI score were performed for each patient’s condition. According to the severity of the disease, the patients were divided into non-severe CAP (NSCAP) and SCAP, and according to the survival situation in the hospital, they were divided into survival group and death group.
Measurement of Serum OSM, IL-6, IL-8 and IL-10 Levels
4 mL of peripheral venous blood was collected in a non-anticoagulant sterile test tube within 24 hours after admission, centrifuged at 4°C (3000 r/min) for 10 minutes, and the supernatant was taken, labeled and subpacked, and frozen at −80 °C. ELISA was used to determine its concentration. The kit was purchased from Wuhan Bode Biological Engineering Co., LTD.
Statistical Analysis
All data were recorded into SPSS 23.0 software for statistical analysis. Continuous variable data with non-normal distribution were represented by median and quartile, and the difference between the two groups was compared by Manne-Whitney U-test. The categorical variables were represented by frequency and percentage, and Chi-square test or Fisher exact probability method was used for comparison between groups. P < 0.05 indicates that the difference was statistically significant. Spearman correlation analysis was used to analyze the correlation between OSM and inflammatory factors or disease severity scores. The variables were divided into two groups, and the variables with P < 0.05 were included in the binary Logistic regression model for multi-factor analysis. To compare the predictive value of biomarkers and severity scores, the receiver operating curve (ROC) was constructed and the area under the curve (AUC) was determined. Kaplan-Meier survival curve was used to analyze the optimal variables affecting in-hospital mortality in CAP patients.
Results
Patient Characteristics
According to the inclusion and exclusion criteria, a total of 110 patients with pneumonia were statistically analyzed. Among them, 55 cases were NSCAP and 55 cases were SCAP. Compared with the NSCAP group, patients in the SCAP group were older, had more underlying diseases, a higher risk of inhalation, and had more severe disease severity (P < 0.001), as shown in Table 1.
 |
Table 1 Demographic Characteristics of the CAP Patients |
Patients with SCAP had higher rates of fever, altered consciousness, increased respiratory rate (RR ≥ 30 beats/min), and increased heart rate (> 100 beats/min). Compared with the NSCAP group, patients with SCAP were more likely to show multiple pulmonary infiltration (78.2%) and pleural effusion (43.6%). There were no significant differences in cough/sputum, chest pain, muscle soreness, and blood pressure, as shown in Table 2.
 |
Table 2 Clinical and Imaging Characteristics of the CAP Patients |
Compared with NSCAP patients, patients with SCAP had higher inflammatory indicators (WBC, NEU, PCT, CRP, etc.), significantly lower LYM, and were more likely to have “hematocrit < 30%, hypoproteinemia, hepatic and renal insufficiency, and elevated blood glucose”. There was no significant difference in platelet count between the two groups (P > 0.05). It was worth noting that compared with the NSCAP group, the concentrations of cytokines OSM, IL-6, IL-8, and IL-10 in patients with SCAP were higher on the day of admission, with significant statistical significance (P < 0.01), as shown in Table 3 and Figure 1.
 |
Table 3 Comparison of Laboratory Indexes Between the Two Groups |
 |
Figure 1 Comparison of serum OSM levels between the two groups on the first day of admission. |
Treatment with hormones, vasoactive drugs, the need for mechanical ventilation, hospitalization in ICU, hospitalization mortality, and the proportion of hospital days were significantly higher in SCAP patients than in the NSCAP group. Respiratory failure (47.3%), new heart failure (34.5%), and multiple organ failure (25.5%) were the most common complications in the SCAP group, and the incidence of respiratory failure was significantly higher than that in the NSCAP group (P < 0.001), as shown in Table 4.
 |
Table 4 Comparison of Treatment and Complication Between the Two Groups |
Spearman correlation analysis was conducted between OSM level and WBC, NEU, LYM, CRP, and PCT. The results showed that OSM level was negatively correlated with LYM (r = −0.49, P < 0.0001) (Figure 2c), and positively correlated with WBC, NEU, CRP, PCT, IL-6, IL-8, and IL-10 (P < 0.05) (Figure 2a, b and d-h). OSM level was positively correlated with CURB-65 score (r = 0.57, P < 0.0001) and PSI score (r = 0.59, P < 0.0001), as shown in Figure 3a and b.
 |
Figure 3 Scatter plot of correlation analysis between OSM and CAP disease severity scores.(a and b) Analysis of correlation between OSM concentration and CURB-65 score and PSI score, respectively. |
Comparison of Clinical Characteristics Between Dead and Surviving Groups
Patients with pneumonia were divided into survival and death groups, and the overall clinical characteristics of the two groups were analyzed. The results showed that the in-hospital fatality rate of pneumonia patients was 12.7%. Most of the dead group were male (85.7%), and they were more prone to dyspnea, disturbance of consciousness, rapid respiratory rate, and pleural effusion (P < 0.05). Also, there were statistically significant differences between the two groups with elevated inflammatory indexes, hypoproteinemia, and renal insufficiency (P < 0.05). The levels of OSM, IL-6, IL-8, and IL-10 in the dead group were significantly higher than those in the surviving group (P < 0.05), as shown in Table 5.
 |
Table 5 Comparison of Clinical Features Between Dead and Surviving Groups |
Binary Logistics Risk Regression Analysis of Factors Affecting in-Hospital Mortality Rate in CAP Patients
The variables with P < 0.05 in the single factor statistical analysis were included in the binary Logistic multivariate regression analysis, and the results showed that OSM (OR: 1.01, 95% CI: 1.003–1.018, P = 0.006) and PSI score (OR: 1.027, 95% CI: 1.009–1.045, P = 0.004) were independent risk factors for death in patients with CAP, as shown in Table 6.
 |
Table 6 Independent Risk Factors for in-Hospital Mortality in Patients with CAP |
The Area Under the Curve for Predicting Death in CAP Patients with Different Risk Factors
Based on the binary logistic multivariate regression analysis of the regression coefficients of the two independent variables related to hospitalization mortality, a new prognostic score - OSM+PSI score - was derived using the following mathematical formula: OSM+PSI score = constant (−6.297) + PSI score × 0.026 + OSM concentration (pg/mL) × 0.01. To determine whether OSM concentration, PSI score, and OSM+PSI score can predict death in patients with pneumonia and applied clinically, a receiver operating curve (ROC) was established. The area under the curve (AUC) was OSM (AUC = 0.8824, 95% CI: 0.8183–0.9466, P < 0.0001), OSM+PSI score (AUC = 0.8750, 95% CI: 0.8067–0.9433, P < 0.0001), PSI score (AUC = 0.8404, 95% CI: 0.7631–0.9178, P < 0.0001), as shown in the Figure 4.
 |
Figure 4 ROC curve of death in patients with CAP predicted by different risk factors. |
Analysis of Kaplan-Meier Survival Curves for OSM Levels Predicting Mortality in Patients with CAP
The cut-off value of OSM was calculated as 76pg/mL, corresponding to a sensitivity of 0.929 and a specificity of 0.823. Kaplan-Meier survival curves for patients diagnosed with CAP were analyzed based on OSM ≥ 76 pg/mL and OSM < 76 pg/mL in the derived cohort. The results showed that OSM ≥ 76 pg/mL was more advantageous in predicting the mortality of CAP patients (P < 0.0001), as shown in Figure 5.
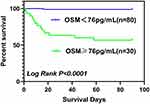 |
Figure 5 Survival curves of OSM concentrations predicting mortality in patients with CAP. |
Discussion
It has been recognized worldwide that CAP is a common respiratory disease with high incidence and is an important cause of death from infectious diseases, with a heavy disease burden and great social harm. When NSCAP develops into SCAP, it can lead to systemic multiple organ failure.16 Studies have found that the morbidity and mortality of patients with moderate to SCAP are high, and the mortality of critically ill patients hospitalized with CAP ranges from 5% to 30–50%.17 Therefore, early assessment of disease severity in CAP patients and identification of major risk factors affecting the prognosis of patients can improve the success rate of treatment, improve the efficiency of medical resources and reduce the burden of disease. The clinical scoring system has its own limitations, and the emergence of biomarkers in the early identification of SCAP high-risk groups plays an important role in the development of the potential.
OSM is a very important pleiotropic cytokine in the IL-6 family, and its secretion has been found to be involved in the immune pathogenesis of various tumors. OSM is involved in the pathogenesis of a variety of human inflammatory diseases including lung disease, including intestinal perfusion injury, inflammatory bowel disease, and pulmonary interstitial fibrosis. In recent years, more and more studies have been conducted on the role of OSM in pulmonary infectious diseases, especially on the regulation of immune mechanisms in mouse models of pneumonia. A prospective study of adenovirus-infected mouse models reported that IL-6 plays a pivotal role in the immunomodulation of pulmonary infection, but OSM was shown to induce B cell activation and broncho-associated lymphoid tissue independently of IL-6 and exert pro-inflammatory effects.12 Machiyama et al proved for the first time that OSM-mediated pulmonary inflammation depended on TRAF5, which induced the expression of VCAM-1 through OSM signal.13 The OSM-TRAF5-VCAM-1 axis is expected to be a new target for the treatment of pulmonary inflammation.13 In addition, it was also found in a mouse model of pneumonia infected by experiments on mouse lung tissue and alveolar lavage fluid confirmed that OSM can rapidly induce pulmonary epithelial cells to activate transcription and activate STAT3, promote the expression of neutrophil chemokine CXCL5, and then play a pro-inflammatory role.14 Studies on the immune regulatory mechanisms of OSM in various signaling pathways in animal models are relatively mature. However, there have been few studies on the severity of disease in OSM and CAP patients. This study analyzed the difference in OSM across disease severity and its predictive value for mortality in hospitalized patients with CAP, which is expected to become a new clinical biomarker for CAP patients.
A prospective study of 49 patients found that on the first day of ICU admission, serum OSM levels in patients with sepsis were significantly higher than those in controls (patients with multiple injuries, brain trauma, intracranial hemorrhage, cerebrovascular accident, and hypertension in emergency departments) and healthy volunteers.9 Another study showed that bacterial DNA content in severe COVID-19 patients was significantly correlated with inflammatory mediators IL-6 and OSM.18 In this study, OSM levels in patients with SCAP on the first day of admission were significantly higher than those in patients without SCAP, which was consistent with the above findings, suggesting that OSM levels were elevated in patients with severe infection regardless of the site of infection. Part of the apparent increase in cytokines release may be due to increased bacterial products in the lung or other tissues, in conjunction with activated macrophage monocytes. Another study of 50 antibody-positive patients (39 asymptomatic and 11 symptomatic) who were included in the 7-8-month recovery period of SARS-CoV-2 infection found that serum OSM levels were elevated in the antibody-positive group.19 This suggests that it is necessary to monitor OSM levels in CAP patients with or without clinical symptoms at a later stage, and the clinical value of OSM in the prognosis of CAP patients can be studied by increasing the samples in the future.
During the progression of CAP disease, a variety of inflammatory mediators (WBC, NEU, CRP, IL-6, IL-8, IL-10, etc.) are increased, resulting in systemic inflammatory response, which can lead to multiple organ failure or even death in severe cases. As the severity of CAP increases, the above inflammatory mediators can partly reflect the severity of CAP and predict the prognosis of the disease. In previous sepsis patients, OSM level was significantly correlated with the increase of PCT and WBC on the day of admission.18 In this study, OSM levels were positively correlated with inflammatory mediators (WBC, NEU, CRP, PCT) and cytokines (IL-6, IL-8, IL-10), but negatively correlated with LYM. At present, clinical assessment of disease severity of CAP patients relies on the CURB-65 score and PSI score. Especially in the outpatient consultation process, where the steps of CURB-65 score are relatively simple. It is more helpful for doctors to have a preliminary understanding of the patient’s condition before deciding on a diagnosis and treatment plan. This study found that OSM level was positively correlated with CURB-65 score (r=0.57, P < 0.0001) and PSI score (r=0.59, P < 0.0001). In summary, there is a significant correlation between the level of OSM and the degree of inflammation and the severity of the disease during the progression of CAP disease. Clinical detection of OSM levels can provide a basis for the development of further treatment plans.
This study found that the level of OSM on the first day of admission was significantly higher in patients with death than in patients with survival, and OSM concentration was an independent risk factor for death in patients with CAP. A prospective study conducted by Chongqing Medical University to explore the possibility of OSM as a biomarker for predicting mortality in sepsis patients found by binary logistic regression analysis that the level of OSM in sepsis patients on the day of admission to ICU (B = 0.000, OR = 1.000, P = 0.015) and SOFA score (B = 0.180, OR = 1.110, P = 0.020) were independent risk factors for 28-day mortality.9 The addition of a specific biomarker, OSM, may improve the accuracy of risk stratification and prognosis assessment in patients with CAP.
In this study, OSM concentration (AUC = 0.8824, 95% CI: 0.8183–0.9466, P < 0.0001) was a simple and reliable predictor of CAP inpatient mortality, significantly better than the current PSI score (AUC = 0.8404, 95% CI: 0.7631–0.9178, P < 0.0001) and OSM+PSI score (AUC = 0.8750, 95% CI: 0.8067–0.9433, P < 0.0001). Especially when the OSM concentration is ≥76 pg/mL, clinicians should attach great importance to the possibility of death in patients with SCAP and have better clinical diagnostic efficacy. China’s 2016 Adult CAP Guidelines clearly point out that it is recommended to combine CURB-65 score with clinical practice to predict the risk of death, especially high-risk patients with scores≥3 should be hospitalized early. The 2019 American Infectious Diseases Society/Thoracic Society (ATS/IDSA) Guidelines for the management and treatment of CAP patients suggest that PSI score can better predict mortality.20 A prospective study published in Chest in 2021 for predicting mortality in patients with SARS-CoV-2 CAP and non-SARS-CoV-2 CAP performed ROC analysis on PSI scores.21 AUC values for SARS-CoV-2 CAP and non-SARS-CoV-2 CAP patients were 0.82 (95% CI: 0.78–0.86) and 0.79 (95% CI: 0.77–0.80). For the CURB-65 score, ROC analysis showed an AUC of 0.79 (95% CI: 0.75–0.84) and 0.75 (95% CI: 0.73–0.77) for both groups, respectively.
Therefore, the authors suggest that the PSI and CURB-65 scores are sufficient to predict mortality in clinical practice. Marta et al also came to the same conclusion.22 The severity score of PSI is largely dependent on advanced age and complications,23,24 but the reported occurrence of 2009 H1N1 influenza virus infection in healthy young adults (32–35 years of age) may be one of the reasons why PSI scores do not predict case fatality. Another possible explanation is that current CAP severity scores are focused on CAP patients with both typical and atypical bacterial pneumonia. It is worth noting that the calculation of PSI score is relatively complicated, which limits its application to some extent. As for the CURB-65 score, although it is simple to operate in outpatient applications, its specificity is relatively poor. In addition, the CURB-65 and PSI scores were biased in evaluating the severity of viral pneumonia, and in fact, preferred the oxygenation index combined with the absolute reduction of peripheral blood lymphocytes to predict the mortality of viral pneumonia. The clinical value of detecting OSM concentration in predicting mortality in patients with CAP should not be underestimated.
In recent years, serum IL-37,25 IL-17,26 soluble urokin-type plasminogen activator receptor (suPAR),27 progranulin (PGRN),28 and other new cytokines are predicted CAP patients have important value in disease severity and prognosis. However, a cytokine with high specificity and sensitivity for the prognosis of SCAP has not yet been identified, and the use of a new biomarker, OSM, has the potential to stratify patients with CAP and identify patients with severely life-threatening infections earlier and better, which is important for personalized treatment in the future.
In SCAP, the search for biomarkers of severity and response to treatment will intensify as research into immunomodulatory therapies intensifies. Only when combined with disease severity scores and biomarkers is it possible to increase diagnostic and predictive value. Identifying risk factors may help develop better strategies for prevention and early identification of SCAP and help identify patients requiring ICU admission to reduce the disease burden of CAP.
This is a single-center study with a small sample size. Larger sample sizes and multi-center studies are needed to compensate for the influence of confounding factors on OSM protein concentrations, which will further confirm the value of OSM in evaluating the disease severity and prognosis of CAP patients. Moreover, the OSM concentrations have been only measured in the serum of CAP patients, and the OSM levels in sputum and bronchial lavage were unknown. No microbiological data were provided, so we could not determine whether the presence of a highly virulent or drug-resistant pathogen had an impact on the outcome of patients with CAP. In the future, we will expand the sample size, set up the control group, and find the critical value of OSM concentration more accurately, so as to provide more favorable evidence for clinical diagnosis and treatment.
Conclusion
Serum OSM has a certain value for the early diagnosis of CAP patients. As a risk factor for the prognosis of CAP patients, OSM has a suggestive and predictive effect on the severity and prognosis of CAP patients.
Data Sharing Statement
The datasets generated and analyzed during the current study are not publicly available due to health privacy concerns but are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The protocol of this study was approved by the Ethics Committee of the Qingdao Municipal Hospital (Approval No. 2020CXJJ001-052). This study was in compliance with the Declaration of Helsinki and informed consent was obtained from all patients or their families before this study.
Acknowledgments
The authors thank all the patients who participated in this study.
Author Contributions
Peikun-Teng, Xiudi Han and Xuedong-Liu contributed to the conception of the study. Peikun-Teng drafted the manuscript under the help of Xiudi-Han and Xuedong-Liu. Xingyu-Zhang and Hong-Wang took part in drafting, revising, conducting statistical analysis or critically reviewing the article. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the Qingdao Municipal Hospital Clinical Diagnosis and Treatment Technology Innovation Fund (CXJJ-034).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sun Y, Li H, Pei Z, et al. Incidence of community-acquired pneumonia in urban China: a national population-based study. Vaccine. 2020;38(52):8362–8370. doi:10.1016/j.vaccine.2020.11.004
2. Zarling JM, Shoyab M, Marquardt H, et al. Oncostatin M: a growth regulator produced by differentiated histiocytic lymphoma cells. Proc National Acad Sci United States Am. 1986;83(24):9739–9743. doi:10.1073/pnas.83.24.9739
3. Malik N, Kallestad JC, Gunderson NL, et al. Molecular cloning, sequence analysis, and functional expression of a novel growth regulator, oncostatin M. Mol Cell Biol. 1989;9(7):2847–2853. doi:10.1128/mcb.9.7.2847-2853.1989
4. Friedrich M, Höss N, Stögbauer F, et al. Complete inhibition of in vivo glioma growth by oncostatin M. J Neurochemistry. 2001;76(5):1589–1592. doi:10.1046/j.1471-4159.2001.00202.x
5. Kim MS, Louwagie J, Carvalho NL, et al. Promoter DNA methylation of oncostatin m receptor-beta as a novel diagnostic and therapeutic marker in colon cancer. PLoS One. 2009;4(8):e6555. doi:10.1371/journal.pone.0006555
6. Courtois-Cox S, Jones SL, Cichowski K. Many roads lead to oncogene-induced senescence. Oncogene. 2008;27(20):2801–2809. doi:10.1038/sj.onc.1210950
7. Verstockt S, Verstockt B, Machiels K, et al. Oncostatin M Is a Biomarker of Diagnosis, Worse Disease Prognosis, and Therapeutic Nonresponse in Inflammatory Bowel Disease. Inflammatory bowel dis. 2021;27(10):1564–1575. doi:10.1093/ibd/izab032
8. West NR, Hegazy AN, et al. Oncostatin M drives intestinal inflammation and predicts response to tumor necrosis factor-neutralizing therapy in patients with inflammatory bowel disease. Nature Med. 2017;23(5):579–589. doi:10.1038/nm.4307
9. Gong Y, Yan X, Sun X, et al. Oncostatin M Is a Prognostic Biomarker and Inflammatory Mediator for Sepsis. J Infectious Dis. 2020;221(12):1989–1998. doi:10.1093/infdis/jiaa009
10. Young PY, Mueller TF, Sis B, et al. Oncostatin M Plays a Critical Role in Survival after Acute Intestinal Ischemia: reperfusion Injury. Surgical Infections. 2020;21(9):799–806. doi:10.1089/sur.2019.193
11. Mozaffarian A, Brewer AW, Trueblood ES, et al. Mechanisms of oncostatin M-induced pulmonary inflammation and fibrosis. J Immunol. 2008;181(10):7243–7253. doi:10.4049/jimmunol.181.10.7243
12. Botelho FM, Rangel-Moreno J, Fritz D, et al. Pulmonary expression of oncostatin M (OSM) promotes inducible BALT formation independently of IL-6, despite a role for IL-6 in OSM-driven pulmonary inflammation. J Immunol. 2013;191(3):1453–1464. doi:10.4049/jimmunol.1203318
13. Machiyama T, So T, Okuyama Y, et al. TNF receptor associated factor 5 controls oncostatin M-mediated lung inflammation. Biochem. Biophys. Res. Commun. 2018;499(3):544–550. doi:10.1016/j.bbrc.2018.03.186
14. Traber KE, Hilliard KL, Allen E, et al. Induction of STAT3-Dependent CXCL5 Expression and Neutrophil Recruitment by Oncostatin-M during Pneumonia. Am. J. Respir. Cell Mol. Biol. 2015;53(4):479–488. doi:10.1165/rcmb.2014-0342OC
15. Cao B, Huang Y, She DY, et al. Diagnosis and treatment of community-acquired pneumonia in adults: 2016 clinical practice guidelines by the Chinese Thoracic Society, Chinese Medical Association. Clin Respir J. 2018;12(4):1320–1360. doi:10.1111/crj.12674
16. Sligl WI, Marrie TJ. Severe community-acquired pneumonia. Critical Care Clinics. 2013;29(3):563–601. doi:10.1016/j.ccc.2013.03.009
17. Welte T. Risk factors and severity scores in hospitalized patients with community-acquired pneumonia: prediction of severity and mortality. Eur j Clin Microbiol Infect Dis. 2012;31(1):33–47. doi:10.1007/s10096-011-1272-4
18. Arunachalam PS, Wimmers F, Mok CKP, et al. Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans. Science. 2020;369(6508):1210–1220. doi:10.1126/science.abc6261
19. Tserel L, Jõgi P, Naaber P, et al. Long-Term Elevated Inflammatory Protein Levels in Asymptomatic SARS-CoV-2 Infected Individuals. Front Immunol. 2021;12:709759. doi:10.3389/fimmu.2021.709759
20. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45–e67. doi:10.1164/rccm.201908-1581ST
21. Bradley J, Sbaih N, Chandler TR, et al. Pneumonia Severity Index and CURB-65 Are Good Predictors of Mortality in Hospitalized Patients with SARS-CoV-2 Community-Acquired Pneumonia. Chest. 2021;2:565.
22. García Clemente MM, Herrero Huertas J, Fernández Fernández A, et al. Assessment of risk scores in Covid-19. Int J Clin Pract. 2021;75(12):e13705. doi:10.1111/ijcp.13705
23. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Eng j Med. 1997;336(4):243–250. doi:10.1056/NEJM199701233360402
24. Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. doi:10.1136/thorax.58.5.377
25. Wang JL, Chen X, Xu Y, et al. The Associations of Serum IL-37 With the Severity and Prognosis in Patients With Community-Acquired Pneumonia: a Retrospective Cohort Study. Front Immunol. 2021;12:636896. doi:10.3389/fimmu.2021.636896
26. Feng CM, Wang XM, Li MD, et al. Serum interleukin-17 predicts severity and prognosis in patients with community acquired pneumonia: a prospective cohort study. BMC Pulmonary Med. 2021;21(1):393. doi:10.1186/s12890-021-01770-6
27. Song S, Jia Q, Chen X, et al. Serum suPAR associated with disease severity and mortality in elderly patients with community-acquired pneumonia. Scandinavian j Clin Lab Investigation. 2020;80(6):515–522. doi:10.1080/00365513.2020.1795920
28. Luo Q, He X, Zheng Y, et al. Elevated progranulin as a novel biomarker to predict poor prognosis in community-acquired pneumonia. J Infection. 2020;80(2):167–173. doi:10.1016/j.jinf.2019.12.004
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

