Back to Journals » Journal of Pain Research » Volume 17
Analgesic Therapy with the Opioids Fentanyl and Morphine by Ambulance Personnel in Rural Areas: An Observational Study Over 7 Years
Authors Scharonow O, Vilcane S, Weilbach C, Scharonow M
Received 19 September 2023
Accepted for publication 25 December 2023
Published 25 January 2024 Volume 2024:17 Pages 345—355
DOI https://doi.org/10.2147/JPR.S437131
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Timothy Atkinson
Olga Scharonow,1 Signe Vilcane,2 Christian Weilbach,2 Maximilian Scharonow2
1Department of Internal Medicine, St. Josefs-Hospital Cloppenburg (Academic Teaching Hospital of the MHH Hannover), Cloppenburg, Germany; 2Department of Anaesthesiology, Intensive Care Medicine, Emergency Medicine and Pain Therapy, St. Josefs-Hospital Cloppenburg (Academic Teaching Hospital of the MHH Hannover), Cloppenburg, Germany
Correspondence: Maximilian Scharonow, Department of Anaesthesiology, Intensive Care Medicine, Emergency Medicine and Pain Therapy, St. Josefs-Hospital Cloppenburg (Academic Teaching Hospital of the MHH Hannover), Krankenhausstrasse 13, Cloppenburg, 49661, Germany, Email [email protected]
Background: The treatment of severe pain is one of the basic procedures of emergency medicine. In rural regions, longer arrival times of the emergency doctor prevent the earliest possible treatment of pain. Since 2014, a project for independent analgesia by ambulance personnel has been introduced in our ambulance service area.
Methods: Over a period of 7 years the mission protocols were recorded and statistically evaluated within the framework of an observational study. Among other things, the attendance and transport times, vital signs, pain level, symptom groups (body region) and classification according to disease or accident mechanism were recorded. Treatment data by medication, including dosages, were recorded for fentanyl (monotherapy), morphine (monotherapy) and a combination (change from morphine to fentanyl, additional application of esketamine, metamizole or butylscopolamine).
Results: In 659 patients, the opioids fentanyl and morphine were used by the ambulance staff, 596 data sets could be evaluated. When an emergency physician was requested, the average time of presence at the scene was 34.8 +- 11.7 min, in cases of unavailability it was 29.0 +-9.8 min (p< 0.0001). Analgesic therapy resulted in a reduction of pain from NRS 8.4 (+-1.3) to NRS 3.5 +-1.8 (p< 0.0001). Pain intensity after treatment by emergency paramedics compared to emergency physicians was not significantly different with NRS 3.5 +- 1.7 versus NRS 3.6 +-1.9 (p=0.788). Fentanyl was used at a mean dose of 0.18mg +- 0.11 and morphine at a mean dose of 4.4mg +- 3.6mg. There was no clinically relevant decrease in oxygen saturation or respiratory rate in any of the treatment groups. Antagonisation of the opioid effect with naloxone was not necessary in any case.
Conclusion: Analgesia with morphine and fentanyl by specially trained ambulance personnel according to defined rules of use is a safe and necessary procedure for patients, especially in rural regions.
Keywords: prehospital, analgesia, opioids, paramedics
Introduction
The treatment of severe pain (NRS ≥ 6) is one of the basic procedures in emergency medicine. The incidence of acute (moderate to severe) pain is in the order of 20% to 30% of patients treated.1–3 The need to improve analgesic therapy in the ambulance service arises from clinical studies.2,4,5 The use of effective medication by the emergency physician is part of this procedure; until August 2023, only the licensed physician in Germany was allowed to apply opioid analgesics.6 In the amending resolution for the Narcotic Drugs Act and the Narcotic Drugs Ordinance, the independent administration of opioids by emergency paramedics is now permissible if an emergency doctor is not available in time, there is a risk to the patient due to secondary damage (eg to the myocardium due to pain-induced tachycardia/hypertonia) or there is an unreasonable (traumatising) disturbance of the patient’s state of mind due to the strongest pain.6 In rural areas, longer arrival times of the emergency physician interfere with the earliest possible treatment of pain. With a lower density of emergency physician bases, the availability of the emergency physician is not guaranteed at any time. The longer distances between the emergency physician’s base and the scene of the emergency as well as the distances to the next suitable clinic lead to an increased time commitment of the emergency physician. The number of physician-assisted transfers from the hospitals of the districts to specialized centres, for which no rescue vehicle (intensive care ambulance, rescue helicopter) is separately available, is also greater in rural regions than in conurbations.7
Therefore, a situation arises again and again in which patients suffer from severe and most severe pain without adequate medicinal pain treatment being able to be carried out in a reasonable time by an emergency physician.7 Several working groups investigated the use of strong painkillers by non-medical ambulance staff.7–15 Telemedicine-guided analgesia is currently only possible at a few locations due to demanding technical requirements and uneven mobile network coverage.16,17
Objective
The aim of this study is to investigate the safety and effectiveness of the use of strong opioid analgesics fentanyl and morphine by non-physician paramedics. In addition, factors influencing the quality and course of prehospital pain management (eg duration of deployment, additional analgesia by the emergency physician.) were investigated.
Materials and Methods
Since the beginning of the project (2014), training (script for 4-week self-study, 8-hour advanced training) and examinations of the participating rescue service personnel have taken place annually; the approval is valid for two years in each case.
Opioids are administered according to defined algorithms, which are updated every two years. Morphine is administered in a dosage of 2 mg and fentanyl in boluses of 0.05–0.1 mg every 3–5 minutes with the goal of an NRS <3 (maximum dose: fentanyl 0.3 mg, not defined for morphine).
The evaluation of the application protocols in the period from 01.01.2016 to 31.12.2022 (DIVIDOK® version EPRO-01030801 as well as DIVI versions 6.0) was carried out within the framework of quality management.
The times in the protocol were automatically recorded via radio for authorities and organizations with security tasks (BOS), the following data were transmitted: alarm and departure time, arrival at the scene, start of transport and arrival of the patient at the hospital. From this, the variables “presence time on scene” (from arrival to start of transport) and “transportation time” (from start of transport to arrival at the hospital) were calculated.
The categorization of the missions was done according to symptom groups (trauma pain, thoracic pain, visceral pain, colic, back pain and other pain), according to diagnosis groups or accident mechanisms (acute coronary syndrome, acute abdomen, lumbago, other thoracic diseases, traffic accident, other accident, fall, burns/scalds and other) as well as in the emergency categories (disease and injury). Pain intensity before and after analgesia on handover in the hospital was assessed using the numerical rating scale (NRS scale), with 0 corresponding to no pain, 3 to 4 to an acceptable level of pain, and 10 to the most severe pain imaginable.
Treatment data by medication, including dosages, were recorded in a total of three groups: fentanyl (monotherapy), morphine (monotherapy) and combination (change from morphine to fentanyl, additional application of esketamine, metamizole or busocopane). Opioids were administered exclusively via sufficient i.v. access. The data sets with incomplete documentation of the dosages were excluded from the group analysis. Statistical analysis of the data was done using IBM SPSS version 20. Comparison of the non-normally distributed dependent variables (before and after treatment) was done using Wilcoxon signed-rank test (NRS, GCS, RR, BPsys, HR, spO2). Group comparison of the independent non-normally distributed variables was calculated using the Mann–Whitney U-test (NRS initial and at handover, medication doses). Prehospital operating times in different groups were examined using Kruskal–Wallis test and ANOVA. The influence of gender, NACA, emergency category, symptom or diagnosis/accident mechanism groups on analgesic therapy was assessed using a chi-square test and Bonferroni correction for significant values in the post-hoc analysis.
Ethics Approval
The Ethics Committee of the Lower Saxony Medical Association gave a positive vote for the retrospective evaluation of the anonymised intervention data (statement by the Ethics Subcommittee of the Lower Saxony Medical Association dated 12 January 2017).
Results
Population, Mission Times and Development Numbers
In the investigated period of 7 years (01.01.2016 to 31.12.2022), the opioids fentanyl and morphine were used in 659 patients, 596 data records could be evaluated. There was a steady increase in the independent use of opioids by ambulance staff from 18 uses in 2016 to 200 in 2022. The ambulance service area under study consists of 3 ambulance + emergency physician vehicle sites (I to III), each of which is located at the hospital, and one ambulance site (IV). The number of applications of opioids was 304 (51.0%), 42 (7.0%) and 138 (23.2%) at sites I to III and 112 (18.8%) at site IV (Table 1). Of the 596 patients, 279 (46.8%) were male and 317 (53.2%) female. The mean age of the patients was 52.6 +- 22.9 (min. 8 and max. 97) years, with male patients being significantly younger (p<0.0001/Mann–Whitney U-test) at 47.9 +- 22.0 years than females at 56.6 +- 23.0 years (Table 1).
 |
Table 1 Population, Mission Times and Pain Intensity |
Symptom Groups, Diagnosis Groups and Accident Mechanisms
The most common symptom group for analgesic therapy was “trauma pain” (n=376/63.1%) followed by “visceral pain” (n=73/12.2%), “back pain” (n=69, 11.6%), “thoracic pain” (n=28/4.7%), other combined pain (n=26/4.3%) and with n=24/4.0% “colic” (Table 1).
The most frequent diagnosis groups/accident mechanisms were “fall” (n=249/41. 8%), “acute abdomen” (n=96/16.1%), “other accidents” (n=66/11.1%), “lumbago” (n=65/10.9%), “traffic accidents” (n=50/8.4%), “other diagnoses” (n=36/6.0%), “acute coronary syndrome” (n=24/4.0%), “burns/scalds” (n=6/1.0%) and “other thoracic diseases” (n=4/0.7%) (Table 1).
Time on Scene
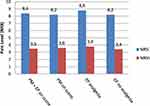
A time of presence at the place of emergency could be determined in 565 (85.7%) cases, which amounted to an average of 33.6 +- 11.6 min (Figure 1 and Table 1). The emergency doctor could be called to the scene in 473 cases (79.4%). In 123 cases (20.6%), the emergency physician was unable to reach the scene within a reasonable period of time due to various reasons (unavailability, supra-regional request). In the case of a successful request for an emergency doctor, the average time of presence at the scene was 34.8 +- 11.7 min, in cases of unavailability this was significantly shorter at 29.0 +-9.8 min (p<0.0001/Mann–Whitney-U-Test).
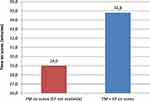 |
Figure 1 Time on scene (min)P. Abbreviations: EP, emergency physician; PM, paramedic. |
With an average presence time of 37.6 (+-12.5) min, the time of operation at the site with supraregional emergency physician vehicle coverage was significantly longer compared to the other sites (p<0.0001/Kruskal–Wallis test). However, in the case of non-availability of the emergency physician, a significant reduction of the attendance time was shown for this site (29.0 +-11.0 min/n=13 vs 38.8 +- 12.3 min/n=94 when waiting for the emergency physician/p=0.01/Mann–Whitney U-test). No correlation could be found between symptom groups and the time spent at the scene of the accident (p=0.072/Kruskal–Wallis test or p=0.154 ANOVA). A significant difference in the time spent on site (p<0.0001/Kruskal–Wallis test or p<0.0001/ANOVA) was only found between the accident mechanism “fall” (n=232/35.6 +-11.6 min) and “other accident” (n=64/28.7 +-9.9 min).
Transportation Time to the Hospital
The average transport time to the destination hospital was 20.6 +- 13.0min, with a significantly longer transport time at the site with supraregional emergency physician vehicle coverage (27.7 +- 11.5min, p<0.0001/Kruskal–Wallis test).
Medical Discipline and Target Department
The majority of patients were assigned to trauma surgery (n=452/75.8%) followed by internal medicine (n=68/11.4%), visceral surgery (n=40/6.7%) and urology (n=21/3.5%). The other specialties each accounted for less than 1% of all patients. 6.7% of patients (n=40) were referred to surgical shock room management, in 7 cases the destination department was not clear.
Pain Intensity
In the entire patient collective, the initial NRS value was 8.4 (+-1.3) and 3.5 (+-1.8) after analgesic therapy at handover in hospital (p<0.0001/Wilcoxon sign rank test) (Table 1).
There was no significant difference in baseline NRS between patients who received analgesic treatment only by ambulance personnel when the emergency physician was not available (n=120/20.7%, NRS 8.2+- 1.3) and those who had an emergency physician present at the scene (n=461/79.3%, NRS 8.4 +- 1.3; p=0.24/Mann–Whitney U-test). Pain intensity was also not significantly different between the two groups at handover at the hospital (emergency physician on site: NRS 3.5 +- 1.7 vs no emergency physician on site: NRS 3.6 +-1.9, p=0.788/Mann–Whitney U-test) (Figure 2). In 65.9% of the patients (n=393), analgesia was provided exclusively by the emergency paramedics. In 203 cases (34.1%), patients were additionally treated with analgesia by the emergency physicians. There was a higher baseline NRS in patients who required additional analgesic therapy by emergency physicians (NRS 8.8 +-1.2 vs 8.2 +- 1.3; p=0.0001/Mann–Whitney U-test) (Figure 2 and Table 1).
There was also a significant difference in pain intensity between these two groups when the patients were handed over at the hospital, with the patients who received additional treatment from the emergency physician showing a higher pain level of NRS 3.8 +- 1.9 compared to the patients without the need for emergency medical therapy (NRS 3.4 +- 1.6/ p=0.036 /Mann–Whitney-U-Test) (Table 1 and Figure 2).
Factors Influencing Additional Analgesia by Emergency Physicians
The next question to be answered was which factors influence the need for additional analgesia by emergency physicians. Patient sex (p=0.301/Chi-square test), emergency category (p=0.583/Chi-square test) and NACA (p=0.229/Chi-square test) showed no influence on the need for additional analgesia by emergency physicians. No significant association could be found between the need for additional analgesia by the emergency physician and the diagnosis/accident mechanism groups (p=0.249/Chi-square test) or symptom groups (p=0.117/Chi-square test). The transport time to the hospital showed no influence on the total dose of fentanyl (p=0.571/Pearson’s correlation) or morphine (p=0.757/Pearson’s correlation) administered by the emergency paramedics. Likewise, there was no correlation between the dose of fentanyl (p=0.075/Pearson) or morphine (p=0.955/Pearson) administered by the emergency physicians and the transport time to the hospital.
Combination Therapy of Analgesics
In 23 patients (3.9%), several analgesics were used simultaneously. In all 23 cases, morphine was the primary analgesic used by the emergency paramedics and was combined with another analgesic in the further course (metamizole: n=8, butylscopolamine: n=8). In 2 cases, the emergency physician switched to the use of fentanyl, in 10 patients metamizole was additionally applied and in 2 cases butylscopolamine.
In the combination therapy group, although there was no significant difference in pain level between monotherapy with morphine or fentanyl and combination of multiple analgesics simultaneously (3.5 +- 1.7 and 3.7 +- 2.3, respectively; p=0.942) at handover in hospital, there was a significantly higher baseline pain level in patients treated with multiple analgesics (9.1 +- 1.2 vs 8.3 +- 1.4; p=0.005/Mann–Whitney U-test).
Dosages
Fentanyl
The opioid fentanyl (monotherapy) was used by paramedics and emergency physicians in 512 (85.9%) patients at a mean dose of 0.18mg +- 0.11mg. The mean total dose administered to patients treated by paramedics alone (n=341/66.2%) was 0.15mg +- 0.07 mg, and to patients treated by emergency physicians (n=171/33.4%) was 0.25mg +- 0.13mg (p<0.001/Mann–Whitney U-test). There was no correlation between the dose of fentanyl administered by the emergency paramedics and the need for additional analgesia by the emergency physicians (p=0.051/Chi-square test). The algorithm released for the emergency paramedics provides for a maximum dose of 0.3mg fentanyl, this was exceeded in a total of only 8 cases (1.6%) by the emergency paramedics after telephone consultation with the emergency physician in charge. When looking at the total dose of fentanyl administered, it was also found that patients with the most severe pain at handover in hospital (NRS>6, n=23) actually received higher doses of more than 0.3mg of fentanyl (p<0.0001/Chi-square test). Overall, a fentanyl dose greater than 0.3mg was used in 9.4% (n=56) of cases.
Morphine
The opioid morphine was used by paramedics in 84 cases in total (14.1%) and of these, as sole agent in 61 cases during the period studied. When used alone, the average dose was 4.4mg +- 3.6mg. There was a significant difference in total dose between patients treated by paramedics alone (n=45) (3.2mg +- 2.3mg) and those receiving an additional dose of morphine from the emergency physician (n=16) (7.9mg +- 4.3mg/p<0.001/Mann–Whitney U-test).
Vital Signs and Critical Side Effects
An overview of the vital signs before and after analgesic therapy is shown in Table 2.
 |
Table 2 Vital Parameters of Patients Before and After Analgesia |
Critical situations and side effects were evaluated in the entire patient population (n=659). During the study period, after analgesia by emergency paramedics, 7 patients had to be instructed to breathe (command breathing). In no case was mask ventilation or antagonisation of the effect of opioids with naloxone necessary.
Accompaniment of the Transport by Emergency Physician
71.1% (n=424) of patients were not accompanied by emergency physicians during transport to hospital after analgesia, 27% (n=161) were transported to hospital, in 1.8% (11 cases) the status of transport was not clear. No significant difference in baseline pain intensity was found between the accompanied and unaccompanied patients (8.2 +- 1.3 vs 8.4 +- 1.6, p=0.186/ Mann–Whitney U-test). There was also no difference in pain intensity between the groups on arrival at hospital (3.4 +- 1.9 Vs 3.6 +- 1.7, p=0.205/ Mann–Whitney U-test). The patients in the morphine group were significantly more often accompanied to the hospital by the emergency physicians (p<0.001/ Chi-square test).
Especially for symptom groups “chest pain” and the accident mechanism “traffic accident” as well as for the diagnosis group “acute coronary syndrome”, the association with accompanied transport was highly significant (p<0.001/Chi-square test).
With regard to the initial vital signs GCS (14.96 vs 14.95, p=0.38), systolic blood pressure (140.79 vs 139.33, p=0.803), heart rate (89.38 vs 88.60, p=0.927) and spO2 (97.59% vs 97.23%, p=0.295), there were no significant differences in the question of accompanying patients to hospital. For the parameter respiratory rate (15.56 vs 16.06, p=0.031), the difference was borderline significant, but not clinically relevant (Mann–Whitney U-tests).
Inadequate Pain Management
Inadequate analgesic therapy was defined as an NRS value at handover > 4. The target NRS of ≤ 4 was achieved in 442 patients (74.2%). In 23.5% (n=140) of the cases, the specified target NRS was not achieved, so that insufficient pain treatment can be assumed.
Telephone Fallback
Within the framework of the project, the possibility of a telephone consultation with the emergency physician on duty was made possible. Contact was made in 24 cases (4%), with fentanyl being used by the emergency paramedics in 23 cases and morphine in combination with other analgesics in one case. In 22 contacts, a maximum of 0.3 mg of fentanyl was used and in one case more than 0.3 mg of fentanyl. Contact with the emergency physician was made almost exclusively in cases of unavailability (n=20, p<0.001/Chi-square test), in 4 cases for consultation during the emergency physician’s journey to the scene. 11 patients in this group (1.8%) had an NRS>4 at handover, 4 of whom suffered from severe pain (NRS > 6).
Discussion
From the perspective of the emergency patient, immediate and adequate analgesic treatment must be given for severe and most severe pain. Whether an effective medication is administered by a licensed physician or, if one is not available, by specially trained emergency service personnel, is of secondary importance for the patient.
To ensure that pain treatment can be initiated as early as possible even in rural areas with limited availability of emergency doctors, a project on the use of strong analgesics (fentanyl and morphine) was started in 2014 with a group of 13 paramedics. From 2016 onwards, the project was extended to the entire ambulance service area with additional questions.
Before the start of the project phase in 2014, no “proven implementation strategy” could be adopted due to a lack of publications on opioid use by non-physician emergency service personnel in Germany. Later, studies on this issue were published,7–16 but these did not result in the need for corrections in the project described here. The opioid analgesics morphine and fentanyl were chosen because of the good experience with these µ-agonists in the medical emergency service. The combination of a high analgesic potency of the µ-agonists with problem-free antagonisability offers, in our opinion, an advantage of these substances over the other analgesics.
Considerations for the selection of substances for the prehospital treatment of severe and most severe pain always include the substance (es)ketamine (in combination with midazolam) because the risk of respiratory depression is lower with this substance. However, in contrast to opioids, there is no possibility of antagonisation, so that if the border between analgosedation and anaesthesia is crossed, the effect cannot be reversed. In this respect, it may also be necessary to secure the airway by endotracheal intubation for (es)ketamine, as with the use of strong opioids (fentanyl, morphine, sufentanil).14,15 In a review article by Sobieraj et al, the quality of analgesia was compared between opioids and (es) ketamine, showing fewer side effects for opioids compared to (es)ketamine with equivalent pain reduction.18 The increasing number of opioid applications from 16 in 2016 to 200 in 2022 reflects, on the one hand, the actual need for prehospital pain therapy on the part of the patients and, on the other hand, the increasing acceptance of the measure among the emergency service personnel. Participation in the project is voluntary, but all emergency paramedics in our rescue service area now take part in the training program and the examinations.
In rural regions, where arrival, presence and transport times are already prolonged, waiting times for the emergency doctor should be critically questioned as to their unavoidability.19 Fok et al studied the presence time at the scene of 506 patients in Australia. The mean time from arrival to start of transport of 34 minutes was comparable to the presence time of our patient collective. Procedures such as intubation, creation of an arterial line. significantly prolonged the duration of the operation.20 In our study, waiting for the emergency physician prolonged the time of presence at the scene by an average of 5.8 minutes, and at the location with supraregional emergency physician vehicle coverage even by 9.8 minutes. The pain intensity at handover in hospital was not significantly different with and without the presence of the emergency physician at the scene, but the length of stay at the scene was on average 5 min shorter when the emergency physician was not available.
Both emergency physicians together with paramedic personnel and emergency paramedics alone achieved a target NRS of ≤ 4 in the majority of cases. Thus, with regard to the quality of analgesia, there seems to be no significant difference between physician and nonphysician pain management. An improvement in pain therapy with fentanyl can be achieved if the lower time limit (3 minutes) and the upper single dose limit (0.1mg) are chosen for application by emergency paramedics. For the patients with insufficient pain relief, the dosages chosen by the emergency physician arriving later were still below the guidelines of the algorithm for emergency paramedics and obviously below the need. Basically, the question arises why fentanyl was not administered in sufficient dosage by the emergency physicians. A total dose of significantly more than 0.3mg may be necessary in certain cases (eg fracture in malposition.) to achieve sufficient pain relief.
The same applies to the use of morphine; here, too, neither the approved framework of upper dosage limits for emergency paramedics nor the possibilities of increasing the dose by emergency physicians were exhausted in patients with NRS > 4 at handover in hospital. Studies name as factors for the quality of prehospital analgesia, among others, the qualification and specialization of emergency physicians,21 lack of guidelines and knowledge deficits.22 In the context of this project, morphine was originally provided as an opioid analgesic for visceral pain, but due to poorer treatment results in an interim evaluation and a lack of rationale (no literature evidence), it has now been replaced by fentanyl in the algorithm.
In our patient collective, 23.5% of patients with an NRS > 4 were inadequately treated with analgesics at handover in hospital; this is a reason for further development of our treatment algorithms. However, these NRS values are of a similar order of magnitude in other studies.2,5,7,13 Analgesic therapy showed no clinically relevant change in important vital signs. Other research groups showed similar results.7,23 No critical side effects were observed during the project. With a decreasing effect of the analgesics during a longer transport time, we would have expected a higher total dose of opioids. The reason for the independence of the total dosage from the transport time is most likely to be found in the long duration of action of the substances used and sufficient immobilisation of the patients. Particularly in rural areas, the reduction of the commitment times for the emergency ambulance vehicles to the necessary level (in order to be ready for a mission again) has a special significance.
By increasing the dosages of fentanyl and morphine within the framework of the algorithms for emergency paramedics, the need for the presence of the emergency physician at the scene and thus the commitment time of the emergency physician vehicle can be significantly reduced. For conditions requiring initial emergency physician medical care, the accompaniment by the physician is independent of the pain event and the use of opioids (eg ACS.).
Limitations
One source of error in recording the level of pain is the subjectivity of the information. The principle of the NRS scale must be explained to the patient.
In a prospective study design, the possibility of comparing strong-acting opioids with (es)ketamine/midazolam would be given.
Conclusions
- Adequate analgesia (NRS ≤ 4) was achieved by emergency paramedics in 65.9% of cases.
- Analgesic therapy with opioids by emergency paramedics is safe.
- The time of presence at the scene of the emergency is reduced by an average of about 5 min when the emergency physician is not available, and by about 10 min in rural regions.
- The quality of analgesia was inadequate in about 20% of patients regardless of the presence of the emergency physician at the scene.
- A higher baseline pain level is associated with more severe pain on handover in hospital.
- The majority of patients are not accompanied to hospital by emergency physicians after analgesia. Accompaniment by the emergency physician is significantly more frequent in the symptom group “chest pain”, the accident mechanism “traffic accident” and the diagnosis “acute coronary syndrome”.
Abbreviations
NRS, numeric rating scale; NRSi, numeric rating scale, at initial contact with patient; NRSh, numeric rating scale at handover in the hospital; BOS, radio for authorities and organizations with security tasks; EP, emergency physician; PM, emergency paramedic; GCSi, Glasgow Coma Scale at the initial contact; GCSh, Glasgow Coma Scale at handover in the hospital; RRi, respiratory rate at initial contact; RRh, respiratory rate at handover in the hospital; BPsysi, systolic blood pressure at initial contact; BPsysh, systolic blood pressure at handover in the hospital; HRi, heart rate at initial contact; HRh, heart rate at handover in the hospital; spO2i, oxygen saturation at initial contact; spO2h, oxygen saturation at handover in the hospital; NACA, National Advisory Committee for Aeronautics score; MWU, Mann–Whitney-U test; KW, Kruskal–Wallis test; WVR, Wilcoxon signed-rank test.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The Ethics Committee of the Lower Saxony Medical Association gave a positive vote for the retrospective evaluation of the anonymised intervention data (statement by the Ethics Subcommittee of the Lower Saxony Medical Association dated 12 January 2017):
In the opinion of the Subcommittee for the Assessment of Medical Research Involving Human Subjects of the Ethics Committee at the Medical Association of Lower Saxony (ÄKN), the retrospective data evaluation planned by you is not a research project in which the psychological or physical integrity of a human being is interfered with or body materials or data are used that can be assigned to a specific human being.
Provided that the personal patient data do not leave the circle of physicians who are obliged to remain silent anyway and who are involved in the treatment of the patient, including auxiliary staff, consultation with the ethics committee in accordance with § 15 of the professional regulations of the ÄKN is therefore not necessary. We strictly adhered to all provisions.
The study has been performed in accordance with the Declaration of Helsinki. All methods were carried out in accordance with relevant guidelines and regulations in the declaration.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. McLean SA, Maio RF, Domeier RM. The epidemiology of pain in the prehospital setting. Prehosp Emerg Care. 2002;6(4):402–405. doi:10.1080/10903120290938021
2. Friesgaard KD, Riddervold IS, Kirkegaard H, et al. Acute pain in the prehospital setting: a register-based study of 41.241 patients. Scand J Trauma Resusc Emerg Med. 2018;26(1):53. doi:10.1186/s13049-018-0521-2
3. Berben SA, Schoonhoven L, Meijs THJM, et al. Prevalence and relief of pain in trauma patients in emergency medical services. Clin J Pain. 2011;27(7):587–592. doi:10.1097/AJP.0b013e3182169036
4. Studnek JR, Fernandez AR, Vandeventer S, et al. The association between patients’ perception of their overall quality of care and their perception of pain management in the prehospital setting. Prehosp Emerg Care. 2013;17(3):386–391. doi:10.3109/10903127.2013.764948
5. Galinski M, Ruscev M, Gonzalez G, et al. Prevalence and management of acute pain in prehospital emergency medicine. Prehosp Emerg Care. 2010;14(3):334–339. doi:10.3109/10903121003760218
6. Gesetz über den Verkehr mit Betäubungsmitteln (Betäubungsmittelgesetz - BtMG) [Act on the Traffic in Narcotics (Narcotics Act - BtMG)]. Betäubungsmittelgesetz in der Fassung der Bekanntmachung vom 1. März 1994 (BGBl. I S. 358), zuletzt durch Beschlussempfehlung und Bericht des Ausschusses für Gesundheit (14. Ausschuss) v. 21.6.2023 geändert [Narcotics Act in the version published on 1 March 1994 (Federal Law Gazette I p. 358), last amended by the recommendation and report of the Committee on Health (14th Committee) of 21.6.2023]. 2023; Available from: https://www.gesetze-im-internet.de/btmg_1981/index.html#BJNR106810981BJNE000916116; Available from.
7. Friesgaard KD, Nikolajsen L, Giebner M, et al. Efficacy and safety of intravenous fentanyl administered by ambulance personnel. Acta Anaesthesiol Scand. 2016;60(4):537–543. doi:10.1111/aas.12662
8. Scharonow M, Alberding T, Oltmanns W, et al. Project for the introduction of prehospital analgesia with fentanyl and morphine administered by specially trained paramedics in a rural service area in Germany. J Pain Res. 2017;10:2595–2599. doi:10.2147/JPR.S151077
9. Schempf B, Casu S, Haske D. Prähospitale Analgosedierung durch Notärzte und Rettungsassistenten [Prehospital analgesia by emergency physicians and paramedics: comparison of effectiveness]. Anaesthesist. 2017;66(5):325–332. German. doi:10.1007/s00101-017-0288-2
10. Dissmann PD, Maignan M, Cloves PD, et al. A review of the burden of trauma pain in emergency settings in Europe. Pain Ther. 2018;7(2):179–192. doi:10.1007/s40122-018-0101-1
11. Jabourian A, Dong F, Mackey K, et al. Evaluation of safety and efficacy of prehospital paramedic administration of sub-dissociative dose of ketamine in the treatment of trauma-related pain in adult civilian population. Cureus. 2020;12(8):e9567. doi:10.7759/cureus.9567
12. Kiavialaitis GE, Müller S, Braun J, et al. Clinical practice of pre-hospital analgesia: an observational study of 20,978 missions in Switzerland. Am J Emerg Med. 2020;38(11):2318–2323. doi:10.1016/j.ajem.2019.10.033
13. Oberholzer N, Kaserer A, Albrecht R, et al. Factors influencing quality of pain management in a physician staffed helicopter emergency medical service. Anesth Analg. 2017;125(1):200–209. doi:10.1213/ANE.0000000000002016
14. Hebsgaard S, Mannering A, Zwisler ST. Assessment of acute pain in trauma-A retrospective prehospital evaluation. J Opioid Manag. 2016;12(5):347–353. doi:10.5055/jom.2016.0351
15. Hollis GJ, Keene TM, Ardlie RM, et al. Prehospital ketamine use by paramedics in the Australian capital territory: a 12 month retrospective analysis. Emerg Med Australas. 2017;29(1):89–95. doi:10.1111/1742-6723.12685
16. Brokmann JC, Rossaint R, Hirsch F, et al. Analgesia by telemedically supported paramedics compared with physician-administered analgesia: a prospective, interventional, multicentre trial. Eur J Pain. 2016;20(7):1176–1184. doi:10.1002/ejp.843
17. Lenssen N, Krockauer A, Beckers SK, et al. Quality of analgesia in physician-operated telemedical prehospital emergency care is comparable to physician-based prehospital care - a retrospective longitudinal study. Sci Rep. 2017;7(1):1536. doi:10.1038/s41598-017-01437-5
18. Sobieraj DM, Martinez BK, Miao B, et al. Comparative effectiveness of analgesics to reduce acute pain in the prehospital setting. Prehosp Emerg Care. 2020;24(2):163–174. doi:10.1080/10903127.2019.1657213
19. Alruwaili A, Alanazy ARM. Prehospital time interval for urban and rural emergency medical services: a systematic literature review. Healthcare. 2022;10:12.
20. Fok PT, Teubner D, Purdell-Lewis J, et al. Predictors of prehospital on-scene time in an Australian emergency retrieval service. Prehosp Disaster Med. 2019;34(3):317–321. doi:10.1017/S1049023X19004394
21. Schaller SJ, Kappler FP, Hofberger C, et al. Differences in pain treatment between surgeons and anaesthesiologists in a physician staffed prehospital emergency medical service: a retrospective cohort analysis. BMC Anesthesiol. 2019;19(1):18. doi:10.1186/s12871-019-0683-0
22. Teoh SE, Loh CYL, Chong RIH, et al. A scoping review of qualitative studies on pre-hospital analgesia administration and practice. Am J Emerg Med. 2022;57:81–90. doi:10.1016/j.ajem.2022.04.038
23. Friesgaard KD, Kirkegaard H, Rasmussen C-H, et al. Prehospital intravenous fentanyl administered by ambulance personnel: a cluster-randomised comparison of two treatment protocols. Scand J Trauma Resusc Emerg Med. 2019;27(1):11. doi:10.1186/s13049-019-0588-4
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.