Back to Journals » Journal of Pain Research » Volume 15
Analgesic Outcomes in Opioid Use Disorder Patients Receiving Spinal Anesthesia with or without Intrathecal Clonidine for Cesarean Delivery: A Retrospective Investigation
Authors Cook MI, Kushelev M , Coffman JH, Coffman JC
Received 27 January 2022
Accepted for publication 10 April 2022
Published 21 April 2022 Volume 2022:15 Pages 1191—1201
DOI https://doi.org/10.2147/JPR.S358045
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Timothy Atkinson
Meghan I Cook,1 Michael Kushelev,1 Julie H Coffman,2 John C Coffman1
1Department of Anesthesiology, The Ohio State University Wexner Medical Center, Columbus, OH, USA; 2Department of Internal Medicine, Riverside Methodist Hospital, Columbus, OH, USA
Correspondence: Meghan I Cook, The Ohio State University Wexner Medical Center, Department of Anesthesiology, N411 Doan Hall, 410 West 10th Ave, Columbus, OH, 43210, USA, Tel +1 614 293 8487, Fax +1 614 293 8153, Email [email protected]
Background: Intrathecal (IT) clonidine has been observed to reduce 24-hour opioid requirements and time to first analgesic request after cesarean delivery, but has not been specifically studied in patients with opioid use disorder (OUD).
Methods: Patients with OUD undergoing cesarean delivery under spinal or combined spinal-epidural (CSE) anesthesia at our institution from 2011 to 2020 were identified, and only patients with OUD were included in this study. Subjects that received IT clonidine were compared to a control group that did not receive IT clonidine to observe potential differences in analgesic outcomes (24-hour opioid requirements, pain scores and time to first post-operative pain medication) or side-effects (hypotension, vasopressor dosing and bradycardia).
Results: A total of 160 patients were included (clonidine n = 22, controls n = 138). For the clonidine group, the median IT clonidine dose was 30μg. Clonidine group patients were observed to have greater dose of IT bupivacaine (12 vs 12.75mg; p = 0.01) and IT morphine (100 vs 200μg; p < 0.001). The clonidine group was also observed to have greater incidence of intraoperative hypotension (20% vs 45%; p = 0.01) and maximum phenylephrine dose (50 vs 57.5 μg/min; p < 0.001). The time to first analgesic request (minutes) after surgery was significantly longer for the clonidine group (153.5 vs 207 min; p < 0.001). The average oral oxycodone equivalents taken per 24 hours of hospital admission were significantly less in the clonidine group (82.36 vs 41.67mg; p < 0.001), and the clonidine group also had significantly less oxycodone equivalents taken for each post-operative day.
Conclusion: IT clonidine was observed to result in reduced 24-hour opioid consumption in patients with OUD and may be useful as part of a multimodal analgesic regimen. The incidence of hypotension and vasopressor doses were greater in patients receiving IT clonidine, and this should be anticipated if IT clonidine is being administered.
Keywords: opioid use disorder, cesarean analgesia, clonidine, enhanced recovery
Introduction
The prevalence of opioid use disorder (OUD) has risen among obstetric patients over time in parallel with the opioid epidemic in the United States, with one study reporting the incidence of OUD increased from 1.5 to 6.5 per 1000 delivery hospitalizations from 1999 to 2014.1 Opioid abuse or dependence in pregnancy increases the risk for adverse maternal and fetal outcomes including maternal death, cardiac arrest, placental abruption, preterm labor, intrauterine growth restriction, stillbirth and neonatal abstinence syndrome.2–4 In addition, it can be particularly challenging to effectively manage postoperative pain after cesarean delivery in this patient population. Compared to control patients, previous retrospective studies have demonstrated patients maintained on either buprenorphine or methadone maintenance therapy have significantly higher daily opioid requirements after cesarean delivery, receiving approximately oral oxycodone 80–90mg per 24 hours.5–7 Uncontrolled pain following delivery is also independently predictive of both chronic pain and postpartum depression at 8 weeks.8 There are, however, only a few published case reports and small case series to guide pain management strategies for these patients. Previous authors have described intravenous (IV) patient-controlled analgesia (PCA), IV ketamine and dexmedetomidine infusions, regional blocks, and continuous epidural infusions containing combinations of local anesthetic, opioids and clonidine.9–15
The use of neuraxial clonidine has demonstrated prolonged sensory and motor blockade, reduced 24-hour opioid consumption, and longer time to first analgesic request after cesarean delivery compared to control patients not receiving clonidine.16,17 However, the effects of intrathecal (IT) clonidine have not been specifically studied in obstetric patients with OUD. Neuraxial clonidine may be of particular benefit in patients with OUD given that it is a non-opioid medication and these patients can be resistant to the effects of opioids.4,14 Clonidine also has analgesic properties, working in part by stimulating post-synaptic alpha 2 adrenergic receptors in the dorsal horn of the spinal cord and reducing afferent transmission of painful stimuli.16–18 Given the potential analgesic benefits of IT clonidine coupled with the lack of published material on the use of this medication in obstetric patients with OUD, we were compelled to complete a retrospective investigation among patients that delivered at our institution. In this retrospective study we sought to compare OUD patients undergoing cesarean delivery that received IT clonidine to a control group that did not receive IT clonidine and observe potential differences in analgesic outcomes (24-hour opioid requirements, pain scores, time to first post-operative pain medication, IV patient-controlled analgesia (PCA) use and regional nerve blocks) or side-effects (hypotension, vasopressor dosing and bradycardia).
Methods
This was a single-center retrospective investigation of obstetric patients with OUD that underwent cesarean delivery under spinal or combined spinal-epidural (CSE) anesthesia, with or without IT clonidine, at The Ohio State University Wexner Medical Center between January 1, 2011 and September 14, 2020. Ethical approval was obtained from the Ohio State University Institutional Review Board (IRB) prior to beginning this investigation (IRB#: 2020H0208). Because this was a retrospective study, no signed patient consent forms were required by the IRB. After IRB approval, patient data were obtained from their electronic medical records by approved study personnel and data was stored in a password-protected electronic research database. Patient confidentiality was maintained, and this study was conducted in accordance with the Declaration of Helsinki.
Patients were included if they were ≥18 years old, had a documented history of OUD, received spinal or CSE anesthesia, and their intraoperative records were available for review. For the purposes of this study, the definition of OUD was kept consistent with the American College of Obstetricians and Gynecologists (ACOG) committee opinion for management of patients with OUD, “a pattern of opioid use characterized by tolerance, craving, inability to control use, and continued use despite adverse consequences”.4 Patients were excluded from this investigation if they had cesarean delivery and hysterectomy in the same surgical procedure, a continuous epidural infusion was used for post-operative analgesia, the spinal block failed and required conversion to general or epidural anesthesia prior to skin incision, or if they were incarcerated. Subjects were identified through Substance abuse Treatment Education and Prevention Program (STEPP) obstetric clinic records at our institution and also patients receiving clonidine were identified by pharmacy-generated list of all obstetric patients for which clonidine was removed from the medication dispensing system in the labor ward during the study period. After patients were identified, data were collected through retrospective chart review and recorded in an electronic database set up for this study. The objective of this study was to determine if including IT clonidine with other spinal medications results in improved analgesia after cesarean delivery in patients with OUD. The primary outcome of interest was opioid consumption per 24 hours during the hospitalization after cesarean delivery. Opioid consumption is reported in oral oxycodone equivalents in milligrams (oral oxycodone 5mg = 7.5mg oral morphine equivalents (OME))19 given that oxycodone is the most commonly administered oral opioid medication for breakthrough pain in many practices in the United States and thus it is likely to be clinically relevant to many providers. Previous retrospective studies on post-cesarean analgesia in OUD patients have also reported opioid consumption in oral oxycodone equivalents.5–7 Secondary analgesic outcomes of interest include administration of supplemental intravenous (IV) opioid or non-opioid medications during surgery, time from spinal dose to first post-operative analgesic medication, maximum and lowest pain scores for each 24-hour period after delivery, IV patient-controlled analgesia (PCA) requirement, and regional block requirement for post-operative analgesia.
Maternal and fetal characteristics were collected for all patients and were compared between patients that received IT clonidine (study group) and a control group that did not receive IT clonidine. The demographic items reported included maternal age, race, height, weight, body mass index (BMI), maintenance therapy (buprenorphine, methadone or none), maintenance therapy dose at delivery, insurance, marital status, smoking status, depression, hepatitis C, HIV, gravidity, parity, gestational age at delivery, number of previous cesarean deliveries, birth weight and Apgar scores.
Intraoperative anesthetic details and post-operative analgesic outcomes were collected for all patients and compared between patients that received IT clonidine and those that did not. Given that this was a retrospective investigation, adherence to a standard anesthetic regimen was not required and all intraoperative medications administered were at the discretion of the anesthesia providers. Anesthetic details reported include dosing of spinal medications (bupivacaine, fentanyl, morphine, clonidine), volume of epidural local anesthetic (if patient had a CSE), requirement for IV opioids, requirement for non-opioid medications for sedation or analgesia, intraoperative hypotension (defined as systolic blood pressure (SBP) <80% of baseline or SBP < 90mm Hg), vasopressor doses, intraoperative bradycardia (heart rate <50 beats per minute (bpm)), and complications of anesthesia. Patient electronic medical records were examined for potential anesthetic complications including accidental dural puncture (ADP), postdural puncture headache (PDPH), neurologic injury, failed spinal block, conversion to other type of anesthesia, postoperative respiratory depression or naloxone administration. Postoperative analgesic and other parameters reported include opioid consumption per 24 hours of hospitalization after delivery (oxycodone equivalents (mg)), time from spinal dose to first post-operative opioid medication, maximum and minimum pain score recorded for each 24 hour period after delivery, cumulative 24-hour IV ketorolac dose (given from 0 to 24 hours after delivery), daily oral ibuprofen dose (given from 24 hours after delivery until discharge), daily acetaminophen dose, incidence of IV PCA use, incidence of regional blocks, delivery-to-discharge interval and hospital readmission within 30 days of delivery.
The analgesic regimen after cesarean delivery at our institution commonly includes IV hydromorphone as needed for breakthrough pain in the surgical recovery area, scheduled ketorolac from 0 to 24 hours after delivery, scheduled oral ibuprofen from 24 hours post-delivery until discharge, oral oxycodone as needed for breakthrough pain, and oral acetaminophen as needed. Patients on opioid maintenance therapy (including buprenorphine and methadone) have these medications continued preoperatively and in the postpartum period, consistent with the ACOG committee opinion for management of patients with OUD.4 Obstetric providers may occasionally elect to withhold ketorolac or ibuprofen post-delivery in patients with preeclampsia, medication allergies or concern for postpartum bleeding complications. Oral oxycodone is commonly initially dosed in the 5–10mg range, and dosing ranges are escalated by physician providers depending on the pain level reported by each patient. IV PCAs are most commonly reserved for patients with severe, refractory pain after surgery, and use is limited to the first 24 hours after cesarean delivery. Regional anesthesia blocks, including transversus abdominis plane (TAP) blocks and ilioinguinal-iliohypogastric blocks, are most commonly performed after surgery in patients with severe pain. In recent years at our institution, many patients with OUD have received continuous epidural infusions after cesarean delivery, though patients receiving continuous epidural analgesia were excluded for the purposes of this retrospective investigation.
Among the patients receiving IT clonidine, selected outcomes were also examined to observe if there was a relation between the clonidine dose administered and analgesic outcomes (eg, IV medications during surgery, opioid consumption, time from spinal dose to first opioid after surgery, pain scores) or important side effects such as hypotension or bradycardia. Linear regressions were performed using clonidine dose to predict each outcome.
Statistical Methods
Patient characteristics (see Table 1), anesthetic details (Table 2), and analgesic outcomes (Table 3) were summarized using counts and percentages for binary variables and 25th, 50th, and 75th percentiles otherwise. In all tables, statistics reported separately for control and clonidine groups, with comparisons done using a test of proportion for binary variables and a rank-sum otherwise. Ordinary least squares regression is used to measure effect of clonidine dose on analgesic outcomes (Table 4), running separate regressions for each outcome using same, standard set of controls. Significance of regression estimates measured by standard t-test. Analyses were performed in StataMP 16 (Stata Corp., College Station, TX, USA).
 |
Table 1 Demographic Summary by Control Group or Clonidine Group |
 |
Table 2 Anesthetic Details by Control Group or Clonidine Group |
 |
Table 3 Analgesic Outcomes by Control Group or Clonidine Group |
 |
Table 4 Clonidine Dose Relation to Analgesic Outcomes and Side Effects (Linear Estimates) |
Results
A total of 143 OUD obstetric patients receiving spinal or CSE anesthesia for cesarean delivery were identified for the control group that did not receive IT clonidine as part of their anesthetic. Five control group subjects had excluding factors (epidural infusion for post-cesarean analgesia (n=1), no OUD diagnosis (n=1), cesarean-hysterectomy (n=1), incarcerated (n=1), failed spinal block that converted to epidural anesthesia (n=1)) and thus 138 subjects were included in the analysis for the control group. A total of 37 obstetric patients were identified that received IT clonidine during the study period. However, 15 of these study group patients had excluding factors (epidural infusion for post-cesarean analgesia (n=7), no OUD diagnosis (n=7), patient received epidural clonidine (n=1)) and thus 22 subjects were included in data analysis for the study group that received IT clonidine.
Of the included patients (control group n=138, clonidine group n=22), demographic and obstetric characteristics compared between study groups were mostly similar, though differences between groups were observed for maternal age, gravidity and percentage of patients on methadone for maintenance therapy (Table 1). Although the clonidine group subjects were observed to have greater gravidity (median 4.5 [interquartile range (IQR) 3, 6] vs 3 [2, 5]; p=0.03), parity and number of previous cesarean deliveries were noted to be similar between groups (Table 1).
Details regarding the intraoperative anesthesia care are summarized in Table 2. The clonidine group was observed to have received greater doses of IT bupivacaine (median 12 [12, 12.75] vs 12.75 mg [12, 13.5]; p=0.01) and IT morphine (median 100 [100, 100] vs 200 µg [100, 200]; p<0.001). For the clonidine group, the median IT clonidine dose was 30 µg [30, 50]. The control and clonidine groups were similar in percentage of patients receiving any form of intraoperative supplemental (sedation/analgesia/anxiolysis) IV medications (54% vs 50%; p=0.73), as well as percentages receiving IV anxiolytic/non-opioid medications (47% vs 45%; p=0.91) or IV opioid medications (26% vs 14%; p=0.22). The clonidine group was also observed to have greater incidence of intraoperative hypotension (20% vs 45%; p=0.01), maximum phenylephrine dose (median 50 [30, 50] vs 57.5 µg/min [50, 75]; p<0.001), and percentage of patients receiving a second vasopressor medication (6% vs 27%; p<0.001). Ephedrine was the second-line vasopressor administered in all patients that received one, and no patients received more than two types of vasopressor medications intraoperatively. The clonidine group also had greater incidence of hypotension in the recovery area (9 vs 27%; p=0.01). All cases of hypotension in the recovery area resolved with IV fluid boluses, no vasopressor medications were administered in the recovery area after surgery. Two control group patients were observed to have complications, one had a failed spinal block on the first attempt requiring repeat spinal block and the other patient required conversion to general anesthesia due to a long operative time. No patients were documented to have post-operative respiratory depression or naloxone administration.
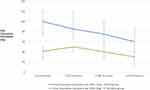
Post-operative analgesic outcomes were compared between control and clonidine groups and is presented in Table 3. The patients that received IT clonidine were observed to have shorter delivery-to-discharge interval (3 [3, 4] vs 3 days [3, 3]; p=0.01). The time to first analgesic request (minutes) after surgery was significantly longer for the clonidine group (153.5 [122, 192.5] vs 207 min [168, 323]; p<0.001). The average oral oxycodone equivalents taken per 24 hours of hospital admission was significantly less in the clonidine group (82.36 [67.78, 109.44] vs 41.67 mg [33.33, 48.33]; p<0.001), and the clonidine group also had significantly less oxycodone equivalents taken for each post-operative day (Table 3, Figure 1). For the most part, maximum and minimum verbal pain scores (0–10) did not differ between control and clonidine group subjects, though the clonidine group was observed to have lower minimum pain scores on day 0 (3 [2, 4] vs 2.5 [0, 3]; p=0.01). The clonidine group received greater daily doses (mg per 24 hours) of ibuprofen (2933.33 [2666.67, 3200] vs 3200 mg [3200, 3200]; p=0.01) and acetaminophen (568.75 [108.33, 1516.67] vs 1895.84 mg [433.33, 2383.33]; p<0.001). Hospital readmission within 30 days of delivery was similar between groups (4% vs 5%; p=0.97), though none of these hospital readmissions were due to poor pain control (Table 3).
To observe any potential impact of IT clonidine dose on analgesic outcomes or side-effects, linear regressions were performed using IT clonidine dose as the variable to predict each outcome (Table 4). In this sample of 22 obstetric patients with OUD that received IT clonidine, the IT clonidine dose was not observed to be related to differences in analgesic outcomes (24-hour oral oxycodone equivalents, first analgesic request after surgery, pain scores) or side-effects including hypotension, vasopressor doses or bradycardia.
Discussion
This 9-year retrospective investigation of obstetric patients with OUD undergoing cesarean delivery observed that patients receiving IT clonidine as part of their anesthetic had significantly reduced oral oxycodone equivalents taken for each post-operative day during their hospital admission (Table 3, Figure 1). The clonidine group also had a longer time to first analgesic medication request after surgery, were less likely to require an IV PCA and had a decreased length of hospital stay. These findings suggest IT clonidine has analgesic benefit as part of a multi-modal medication regimen in OUD patients after cesarean delivery. In previous retrospective investigations, patients with OUD have been observed to have high opioid requirements after cesarean delivery, receiving approximately oxycodone 80–90mg per 24 hours of hospitalization after delivery.5–7 The control group in the present study was similar to these previous reports, receiving oral oxycodone 82.36mg per 24 hours of hospitalization, but in contrast patients receiving IT clonidine only required oral oxycodone 41.67mg per 24 hours of hospitalization. Though patients receiving IT clonidine had reduced opioid requirements after cesarean delivery, maximum and minimum pain scores were observed to be mostly similar between study groups.
While IT clonidine use may provide reduction in opioid requirements after cesarean delivery in patients with OUD, it should be noted that patients in the clonidine group for this retrospective study also received higher doses of IT morphine (median 100 µg [100, 100] vs 200 [100, 200]; p<0.001). A limitation of retrospective investigations is that it is not possible to ensure that medication doses are standardized between study groups. Over the past few years, providers at our institution have begun to increase IT morphine doses in patients with OUD, similar to other institutions,20 in addition to administering IT clonidine to try and improve pain relief after surgery in opioid-tolerant patients. IT morphine is an important part of multi-modal analgesia for patients undergoing cesarean delivery and is utilized in many practices in the United States. A recent meta-analysis compared patients receiving IT morphine 50–100µg to morphine 100–250µg for post-cesarean analgesia. The higher morphine dose group had longer time to first analgesic request, though 24-hour opioid consumption was similar. The higher dose IT morphine also resulted in greater incidence of side-effects.21 Another study examined patients predicted to have severe pain after cesarean delivery, though not specifically patients with OUD. In this study, patients received either IT morphine 300µg or 150µg. The higher dose group had lower 24-hour pain scores, but 24-hour opioid consumption did not differ.22 To our knowledge, no specific studies comparing higher IT morphine doses has been performed in obstetric patients with OUD. It should also be noted that the clonidine group received greater doses of IT bupivacaine (median 12mg [interquartile range (IQR) 12, 12.75] vs 12.75 [12, 13.5]; p=0.01) in this retrospective study, and this may have contributed to the longer time to first post-operative analgesic medication request for these patients.
Clonidine has been examined as an adjunct medication and may be particularly useful in patients with OUD given that it has a different mechanism of action than opioids or local anesthetics. Clonidine is an alpha-2 adrenergic receptor agonist in the spinal cord dorsal horn and the substantia gelatinosa, whereby it decreases afferent norepinephrine-mediated transmission of noxious stimuli.16,17 In opioid-naïve patients (both non-obstetric and obstetric) epidural clonidine has been shown to decrease post-operative analgesic requirements, prolong the duration of analgesia and have a dose sparing effect on local anesthetic.23 A 75 patient randomized control trial by Paech et al examined the addition of clonidine 4.5 µg/mL to epidural medication solution of 0.0625% bupivacaine and fentanyl 2 µg/mL, and found that the clonidine group had less total bupivacaine and fentanyl use as well as fewer supplemental doses, but had higher sedation scores.24 Previous meta analyses have examined clonidine as an analgesic adjunct for cesarean delivery and found that clonidine prolonged motor and sensory blockade and decreased 24-hour opioid consumption. The addition of clonidine also prolonged time to first request for pain medication following cesarean delivery.16,17 It should be noted that these studies did not include patients with OUD. A recent study by Hoyt et al was specifically done in patients with OUD and demonstrated the benefits of epidural clonidine in lieu of fentanyl for both laboring parturients and after cesarean delivery using a CSE technique.14 The study included 14 patients, 7 laboring and 7 presenting for cesarean delivery. The authors substituted their standard 2 µg/mL fentanyl in 0.0625% bupivacaine epidural solution with 2 µg/mL clonidine in 0.0625% bupivacaine, or 1.2 µg/mL clonidine in 0.1% bupivacaine, for labor and post-cesarean analgesia in parturients on buprenorphine therapy. All the laboring patients reported adequate analgesia, with five of seven of those patients avoiding supplemental opioid use postpartum. The epidural catheter was left in situ for 24 hours postoperatively following cesarean delivery and six out of the seven patients reported pain scores less than 5/10 at time of removal, and three patients did not require any additional opioid medication.
The adverse effects of IT clonidine can be anticipated and include maternal sedation, hypotension and bradycardia. The clonidine group in the present study did in fact have greater incidence of intraoperative hypotension, higher maximum phenylephrine infusion dose and a higher percentage of patients receiving a second vasopressor medication (IV ephedrine in all cases). We observed similar incidence of hypotension with IT clonidine compared to previous published data.16,17 If IT clonidine is administered, the increased potential for hypotension should be anticipated and can be effectively managed with higher starting dose of phenylephrine infusion and proceeding to a second-line vasopressor relatively quickly if needed. The IT clonidine group in the present study also had greater incidence of hypotension in the recovery area, however these instances of hypotension were not severe and managed with IV fluid boluses only (no vasopressors were administered). It should be recognized that the slightly higher dose of IT bupivacaine may have also contributed to the greater incidence of hypotension observed in the clonidine group in this study. We observed no differences in the incidence of bradycardia or treatment for bradycardia. Lastly, sedation from IT clonidine is an important side-effect and a further limitation of this retrospective study was that we were unable to gain reliable data on patient sedation in the OR or recovery area from retrospective chart reviews. It would be beneficial to be able to ascertain incidence of intraoperative or postoperative sedation from a prospective study. We sought to determine if higher doses of IT clonidine resulted in greater incidence of side effects (Table 4), and in our sample size of 22 subjects we did not observe any difference in analgesic outcomes or side effects with higher doses of IT clonidine.
Pain control is expectedly difficult in obstetric patients with OUD and a plan for pain management should employ a multidisciplinary approach involving the obstetrician and anesthesiologist. This is ideally broached in the antepartum period, involving patient education and expectation management. Moreover, Shah et al have found that providing patient information, having a plan of care both intra- and post-partum, and managing patient expectations improve the patient experience.20 Inadequate pain control postpartum has been associated with increased risk of postpartum depression and chronic pain at 3 and 12 months postpartum.8,25,26 In addition to chronic pain, other factors common in patients with OUD such as tobacco use and anxiety have also been associated with increased postoperative pain.27 Ideally, a multimodal plan for analgesia should be employed for all patients, but especially patients with OUD. This is becoming much more prevalent as enhanced recovery after cesarean delivery (ERAC) protocols are being introduced. Key components of these protocols include multimodal pain medications (scheduled acetaminophen and NSAIDS such as ketorolac or ibuprofen), early ambulation, decreased fasting interval with anticipated goals of decreased length of stay and increased patient satisfaction. At our institution, the timing of hospital discharge is ultimately decided by the obstetricians, and this decision is impacted by a patient’s pain relief, ability to accomplish tasks of daily life, ambulate, bowel function and absence of any complications such as bleeding, infection or preeclampsia. Although formal ERAC protocols are currently under review with our clinical practice guideline committee, many elements common to ERAC protocols have already become incorporated for cesarean deliveries at our institution in recent years and this may have contributed to the earlier discharge times observed in the clonidine group in the present study. Greater emphasis on patients receiving scheduled ibuprofen and acetaminophen was apparent in the present investigation as well, as patients in the IT clonidine group delivering in more recent years were observed to have greater ibuprofen and acetaminophen doses per 24 hours compared to the control group patients. It is also important to consider how pain control is assessed in the postpartum period. Functional pain assessment and/or Quality of Recovery scores are included in ERAC protocols to evaluate pain control without relying on visual analog scales which may not correlate with pain control or recovery, especially in patients with OUD who may experience hyperalgesia and poor pain tolerance. Functional pain assessment tools use focused questions regarding the patient’s ability to carry out activities of daily living, feeding, and caring for her newborn as well as mobility and feeling in control of her recovery.20,28 Medication-assisted therapy (MAT) is the standard of care for this patient population during pregnancy and postpartum per the American College of Obstetrics and Gynecology.4 It is also recommended to continued MAT by the American Society of Addiction Medicine to avoid precipitating neonatal withdrawal.29 MAT with buprenorphine has become more common than methadone for obstetric patients in recent years, as buprenorphine has been associated with longer gestation, greater birth weights and lower incidence of neonatal abstinence syndrome.30 Consistent with this trend, in the present investigation, the percentage of patients on methadone was significantly lower in the IT clonidine group patients, which all delivered in the latter end of the study period compared to the control group.
Conclusion
In this 9-year retrospective study, IT clonidine was observed to result in greater time to first pain medication request after surgery and reduced 24-hour opioid consumption in patients with OUD and may be useful as part of a multimodal analgesic regimen for these patients. Incidence of hypotension and vasopressor requirements were greater in patients receiving IT clonidine, so providers should anticipate this if IT clonidine is administered. These results should be interpreted with caution, as the clonidine group patients did also receive greater doses of IT bupivacaine and IT morphine compared to the control group. Prospective, controlled investigations are needed to verify the findings of this retrospective study.
Data Sharing Statement
Requests for data should be addressed to the corresponding author.
Ethics and Informed Consent
Ethical approval was obtained from the Ohio State University Institutional Review Board (IRB) prior to beginning this investigation (IRB: 2020H0208). Given this was a retrospective study, no subject consent forms were required by the IRB. Patient confidentiality was maintained, and this study was conducted in accordance with the declaration of Helsinki.
Acknowledgments
The authors would like to extend an enormous thank you to Lucas C. Coffman, PhD, for assistance with statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization - United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2018;67:845–849. doi:10.15585/mmwr.mm6731a1
2. Maeda A, Bateman BT, Clancy CR, Creanga AA, Leffert LR. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. J Am Soc Anesthesiol. 2014;121(6):1158–1165.
3. Patrick SW, Davis MM, Lehmann CU, Cooper WO. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol. 2015;35(8):650–655. doi:10.1038/jp.2015.36
4. Committee on Obstetric Practice, American Society of Addiction Medicine. Committee Opinion No. 711: opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130:e81–e94. doi:10.1097/AOG.0000000000002235
5. Meyer M, Wagner K, Benvenuto A, Plante D, Howard D. Intrapartum and postpartum analgesia for women maintained on methadone during pregnancy. Obstet Gynecol. 2007;110(2 Pt 1):261–266. doi:10.1097/01.AOG.0000275288.47258.e0
6. Meyer M, Paranya G, Norris AK, Howard D. Intrapartum and postpartum analgesia for women maintained on buprenorphine during pregnancy. Eur J Pain. 2010;14(9):939–943. doi:10.1016/j.ejpain.2010.03.002
7. Reno JL, Kushelev M, Coffman JH, et al. Post-cesarean delivery analgesic outcomes in patients maintained on methadone and buprenorphine: a retrospective investigation. J Pain Res. 2020;13:3513–3524. doi:10.2147/JPR.S284874
8. Eisenach JC, Pan PH, Smiley R, Lavand’homme P, Landau R, Houle TT. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140(1):87–94. doi:10.1016/j.pain.2008.07.011
9. Jones HE, Johnson RE, Milio L. Post-cesarean pain management of patients maintained on methadone or buprenorphine. Am J Addict. 2006;15(3):258–259. doi:10.1080/10550490600626721
10. Tith S, Bining G, Bollag L. Management of eight labor and delivery patients dependent on buprenorphine (Subutex): a retrospective chart review. F1000Res. 2018;7:7. doi:10.12688/f1000research.13350.1
11. Leighton BL, Crock LW. Case series of successful postoperative pain management in buprenorphine maintenance therapy patients. Anesth Analg. 2017;125(5):1779–1783. doi:10.1213/ANE.0000000000002498
12. Wasiluk IM, Castillo D, Panni JK, Stewart S, Panni MK. Postpartum analgesia with dexmedetomidine in opioid tolerance during pregnancy. J Clin Anesth. 2011;23(7):593–594. doi:10.1016/j.jclinane.2010.09.013
13. Stanislaus MA, Reno JL, Small RH, et al. Continuous epidural hydromorphone infusion for post-cesarean delivery analgesia in a patient on methadone maintenance therapy: a case report. J Pain Res. 2020;13:837–842. doi:10.2147/JPR.S242271
14. Hoyt M, Shah U, Cooley J, Temple M. Use of epidural clonidine for the management of analgesia in the opioid addicted parturient on buprenorphine maintenance therapy: an observational study. Int J Obstet Anesth. 2018;34:67–72. doi:10.1016/j.ijoa.2018.01.001
15. Coffman JC, Fiorini K, Small RH. Ilioinguinal-iliohypogastric block used to rescue ineffective transversus abdominis plane block after cesarean delivery. Int J Obstet Anesth. 2015;24(4):394–395. doi:10.1016/j.ijoa.2015.05.003
16. Crespo S, Dangelser G, Haller G. Intrathecal clonidine as an adjuvant for neuraxial anaesthesia during caesarean delivery: a systematic review and meta-analysis of randomised trials. Int J Obstet Anesth. 2017;32:64–76. doi:10.1016/j.ijoa.2017.06.009
17. Allen T, Mishriky B, Klinger R, Habib A. The impact of neuraxial clonidine on postoperative analgesia and perioperative adverse effects in women having elective Caesarean section–a systematic review and meta-analysis. Br J Anaesth. 2018;120(2):228–240. doi:10.1016/j.bja.2017.11.085
18. Filos KS, Goudas LC, Patroni O, Polyzou V. Intrathecal clonidine as a sole analgesic for pain relief after cesarean section. Anesthesiology. 1992;77(2):267–274. doi:10.1097/00000542-199208000-00008
19. McPherson ML. Demystifying Opioids Conversion Calculations: A Guide for Effective Dosing. Bethesda: ASHP; 2009.
20. Shah JR, Ramseyer A, Coker J. Peripartum management for women with opioid dependence. Curr Opin Anaesthesiol. 2021;34(3):226–232. doi:10.1097/ACO.0000000000000996
21. Sultan P, Halpern SH, Pushpanathan E, Patel S, Carvalho B. The effect of intrathecal morphine dose on outcomes after elective cesarean delivery: a meta-analysis. Anesth Analg. 2016;123:154–164. doi:10.1213/ANE.0000000000001255
22. Booth JL, Harris LC, Eisenach JC, Pan PH. A randomized controlled trial comparing two multimodal analgesic techniques in patients predicted to have severe pain after cesarean delivery. Anesth Analg. 2016;122(4):1114. doi:10.1213/ANE.0000000000000695
23. Syal K, Dogra R, Ohri A, Chauhan G, Goel A. Epidural labour analgesia using Bupivacaine and Clonidine. J Anaesthesiol Clin Pharmacol. 2011;27:87–90. doi:10.4103/0970-9185.76658
24. Paech MJ, Pavy TJ, Orlikowski CE, Evans SF. Patient-controlled epidural analgesia in labor: the addition of clonidine to bupivacaine-fentanyl. Reg Anesth Pain Med. 2000;25:34–40. doi:10.1016/s1098-7339(00)80008-5
25. Perkins FM, Kehlet H. Chronic pain as an outcome of surgery. A review of predictive factors. Anesthesiology. 2000;93:1123–1133. doi:10.1097/00000542-200010000-00038
26. Jin J, Peng L, Chen Q, et al. Prevalence and risk factors for chronic pain following cesarean section: a prospective study. BMC Anesthesiol. 2016;16:99. doi:10.1186/s12871-016-0270-6
27. Mehdiratta JE, Saab R, Chen Z, Li YJ, Habib AS. Patient and procedural risk factors for increased postoperative pain after cesarean delivery under neuraxial anesthesia: a retrospective study. Int J Obstet Anesth. 2020;44:60–67. doi:10.1016/j.ijoa.2020.07.006
28. Ciechanowicz S, Howle R, Heppolette C, Nakhjavani B, Carvalho B, Sultan P. Evaluation of the Obstetric Quality-of-Recovery score (ObsQoR-11) following non-elective caesarean delivery. Int J Obstet Anesth. 2019;39:51–59. doi:10.1016/j.ijoa.2019.01.010
29. Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) National Practice Guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9:358–367. doi:10.1097/ADM.0000000000000166
30. Meyer MC, Johnston AM, Crocker AM, Heil SH. Methadone and buprenorphine for opioid dependence during pregnancy: a retrospective cohort study. J Addict Med. 2015;9:81–86. doi:10.1097/ADM.0000000000000092
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.