Back to Journals » Advances in Medical Education and Practice » Volume 11
An Undergraduate Surgery Interest Group: Introducing Premedical Students to the Practice of Surgery
Authors Vakayil V, Chandrashekar M, Hedberg J, Bauman BD, Malik S , Yerxa D, Hendrickson LG , Kernahan P, Hadley ME , Harmon JV
Received 10 January 2020
Accepted for publication 18 April 2020
Published 13 May 2020 Volume 2020:11 Pages 339—349
DOI https://doi.org/10.2147/AMEP.S245234
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Victor Vakayil, 1 Malavika Chandrashekar, 1 Jack Hedberg, 2 Brent D Bauman, 1 Shray Malik, 2 Derek Yerxa, 2 Lois G Hendrickson, 3 Peter Kernahan, 1, 3 Megan E Hadley, 1 James V Harmon 1
1Department of Surgery, University of Minnesota, Minneapolis, MN, USA; 2College of Biological Sciences, University of Minnesota, St. Paul, MN, USA; 3Owen H. Wangensteen Historical Library of Biology and Medicine, University of Minnesota, Minneapolis, MN, USA
Correspondence: Victor Vakayil Tel +1 612 625 7129
Fax +1 612 626 0439
Email [email protected]
Purpose: Early exposure and surgical mentorship can augment interest in surgery. We evaluate the effect and feasibility of offering education and mentorship opportunities in surgery to premedical students at our institution through an undergraduate surgery interest group (USIG).
Materials and Methods: We conducted a 1-year assessment of our USIG and reviewed its organizational structure, funding resources, media promotion, and educational activities. Our USIG hosted introductory-level surgical skills workshops, guest lectures by surgeons, and various facility tours. To assess participants’ interests, as well as the influences on them to pursue a surgical profession, we analyzed pre- and post-event questionnaires. Similar questionnaires were completed by medical students in our medical student surgery interest group to compare any differences in perception between premedical and medical students.
Results: Our USIG currently has 378 undergraduate student members, with a higher proportion of women than in our medical student surgery interest group (P < 0.003). Neurosurgery was the most popular career choice among undergraduate participants. Participants reported the highest satisfaction with suturing and high-fidelity trauma surgery skills workshops. Undergraduate participants indicated that their intrinsic interest in the sciences is the highest motivation to pursue a surgical profession. Resident lifestyle and social obligations of a surgical career were actually positive influences for undergraduate participants; in contrast, medical students viewed those variables as negative factors.
Conclusion: Our USIG was met with enthusiasm by premedical students and faculty alike. Participation strengthened premedical students’ interest in pursuing surgery and increased their understanding of the surgical profession. Early mentorship may positively influence premedical students’ perception of surgical careers. USIG is economically feasible and time-efficient; we encourage other academic institutions and educators to consider investing in similar interest groups.
Keywords: premedical education, surgical education, mentorship, premedical vs medical, surgical skills, career choice
A Letter to the Editor has been published for this article.
Introduction
A surgical career provides a unique opportunity to combine clinical knowledge and proficiency with procedural skill-based practice.1 Multiple studies1–9 have evaluated factors affecting medical student career choice; students who pursue surgical careers are more likely to be interested in procedural skill development and are more willing to sacrifice lifestyle to attain career goals. In 2018, despite a high overall match rate into a surgical residency, only 76% of surgical residency positions were occupied by US senior medical students:10 a considerable drop from 87% more than 30 years ago.11 The percentage of US medical students ranking general surgery as their first choice fell from 10.7% in the mid-1980s to less than 5% in the early 2000s.12 The reasons have been attributed to gender and generational differences.13,14
Current surgical trainees value protected personal time in their professional careers, which represents a considerable change from past generations.1,2,13–19 National efforts to improve matriculation rates now include improvements in resident well-being and the incorporation of the 80-hour resident workweek.20 Research to identify solutions to resident attrition and burnout are ongoing.21–25 Multiple studies acknowledge the positive impact of early surgical mentorship for medical students: lack of such surgical mentorship can reduce the probability of a surgical career.3,6,14,26–28 Furthermore, routine mentoring that starts during 3rd-year clinical rotations is insufficient to generate adequate levels of interest among medical students.1,13,14,27,28 Moreover, a 2-decade-long focus by medical schools to actively promote primary care has also dissuaded many medical students from pursuing surgical careers.2,29,30 For example, about half of the medical students who initially express interest in general surgery change their minds during medical school.31 Innovative educational solutions that promote student interest, well-being, and student-surgeon interactions can augment interest in surgery.
Medical student surgery interest groups (MSIGs) at several institutions have demonstrated success in improving interest and rates of matriculation in surgery.28,32–37 For pre-clerkship medical students, such groups provide a realistic look at the clinical and academic attributes of surgical specialties in an informal, low-stress environment. Such groups and rotations allow medical students to develop professional relationships with surgical faculty and residents leading to a sustained interest in a surgical career.28,32–36,38
In an attempt to evaluate the impact of early mentorship and the success of student interest groups, we explored the feasibility of extending surgical education to undergraduate premedical students through our undergraduate surgery interest group (USIG). To identify potential opportunities for educational reform, we evaluated and compared the perceptions of both our USIG and MSIG participants.
Materials and Methods
The USIG is a registered student group that provides a platform for over 35,000 undergraduate students to explore their career interests. The group facilitates communication between surgeons, surgical residents, and medical students. Instituted in 2015, it is an initiative led by our Department of Surgery faculty that offers introductory-level surgical skills workshops, focused group activities, along with high- and low-fidelity simulation-based exercises. Surgery laboratory tours, hospital and adjunct facility tours, surgeon-led research drives, guest lectures by surgeons, interactive panel discussions, and social gatherings are some of the various activities organized by the group. (Table 1)
 |
Table 1 Event Information for the Undergraduate Surgery Interest Group |
The objectives of USIG are to: 1) bolster interest in surgery; 2) enable undergraduate students to evaluate their aptitude for a surgical career; 3) provide hands-on experiences; 4) facilitate mentorship by surgeons, residents, and medical students; and 5) discuss the ethics of patient autonomy. The group currently has 378 undergraduate student members. All activities are organized by a 5-member student leadership board, which meets every other week to coordinate monthly events. Department of Surgery faculty advisers oversee the activities and help the students secure resources, schedule events, and identify speakers. Since USIG’s inception in 2015, more than 50 surgeons and surgical residents have participated, including community and academic surgeons, research faculty, and residents from our institution as well as neighboring institutions. Activities have been supported by small grants and funds obtained from the University’s Student Union and Activities Office and from the Student Association.
Topics from the MSIG workshop served as a template for our USIG events. Our educational framework followed Kolb’s theory of experiential learning which included creating concrete experiences, reflective observation, abstract conceptualization, and active experimentation.39 Most events focused on active skills acquisition where students were shown how to perform a particular task such as suturing, knot tying, trauma resuscitation etc., by faculty or residents. They would then attempt each task under supervision, rotate through various stations and return to practice. This gave them time to reflect on and conceptualize the learned task, and then reattempt these tasks to augment skill and technique.
The surgical skills workshops were popular events that provided hands-on experiences in basic procedural skills, emphasizing dexterity and encouraging students to evaluate their aptitude for a career in surgery. All workshops were held at either American College of Surgeons (ACS)-accredited simulation center, that provided patient simulators (SimManⓇ), or at the University's Historical Library of Biology and Medicine.
On the pre-event surveys, premedical students indicated a strong interest in trauma surgery; as a result, many of the workshops focused on basic aspects of trauma resuscitation. Several low-fidelity amputation workshops, using easy-to-assemble training models, taught students the relevant surface anatomy of the lower limbs. Surgical instructors guided students through a rapid trauma assessment and highlighted the core concepts of trauma resuscitation. Simulated gunshot wounds introduced students to the management of penetrating trauma using SimManⓇ. High-fidelity simulation-based workshops provided realistic trauma simulations and encouraged critical thinking and teamwork. Instructors provided brief clinical vignettes and assigned students clinical roles, such as a trauma surgeon, an assistant surgeon, and a second assistant. Students were taught how to glove and gown, taught trauma assessment protocols, and were given access to standard-of-care technology, such as ventilation equipment, vital signs monitoring devices, and mock intravenous medications. To elicit student assessments and encourage interventions, administrative staff and technicians modified the mock vital signs and simulated physical findings using SimManⓇ to adapt to student assessments and interventions. These simulated trauma scenarios promoted dialogue between instructors, staff, and students and permitted evaluation of mock clinical handoffs.
In addition to hands-on workshops and simulation-based exercises, our USIG has emphasized the historical foundations of surgery, in order to facilitate a broader understanding of the surgical field. Curator- and faculty-guided seminars were held at the University’s Historical Library of Biology and Medicine, which houses a nationally recognized collection of more than 80,000 rare books, surgical manuscripts, and artifacts. Facebook and Twitter were used to promote events and member engagement. These networks provided pre-event advertisements, invitations, reminder notifications, and post-event reviews. Our USIG website,40 which is entirely student-run, provides access to preparatory surgical training resources, including basic online skills-training modules and links to current journal articles. The website also provides information on how to obtain clinical observership opportunities in surgery.
Lastly, we also observed a high level of interest for research among USIG participants. The USIG provides its members with ways to engage in surgical research and present abstracts and oral papers at various local and national meetings.
Data Collection
Students attending USIG surgical skills workshops were asked to complete voluntary pre- and post-event questionnaires, which addressed not only their interest in surgery but also their confidence in performing surgical skills. Subsequently, we assessed the influence of various academic, social, and lifestyle factors on their interest in surgery. Responses were ranked on a 5-point Likert-type scale (1 = very negative influence, 2 = negative influence, 3 = neutral, 4 = positive influence, 5 = very positive influence). The MSIG leadership coordinated the administration of similar questionnaires to their medical student members, so that we could compare and contrast any differences in opinion between our USIG and MSIG participants. Our Institutional Review Board deemed this education-based study exempt from review (study number: 1210E2318).
Statistical Analysis
We used nonparametric statistical tests to compare the results of our USIG and MSIG questionnaires. Continuous and ordinal variables were analyzed using the Mann–Whitney U and Kruskal–Wallis H-tests. To analyze categorical data, we used a chi-square test while correlations between variables were measured using a Spearman’s rho. Independent proportions z tests were used to compare proportions. Descriptive statistics include the total number and median (interquartile range [IQR]), where appropriate. A 2-tailed P value < 0.05 was considered statistically significant. For all our data analysis, we used IBM SPSS Statistics for Windows software, version 21.0 (IBM Corporation, Armonk, NY).
Results
Since its inception in 2015, our USIG has grown. The popularity of online social networks served to effectively facilitate communication within our USIG; membership spiked after each event (approximately 50 members per new event), complemented by an increase in social media activity.
Each event hosted an average of 40 participants. Most USIG participants were women (75%, n = 30). Most USIG participants were enrolled in a biological sciences program (Figure 1, 68.6%, n = 24); participation did not vary by undergraduate year of enrollment (P = 0.303). More than one quarter of participants (27.5%, n = 11) wanted to pursue neurosurgery; other popular surgical subspecialties included trauma and cardiothoracic surgery (Figure 2). More than one quarter of participants (26.2%, n = 11) had already decided to pursue a surgical profession; another one third indicated (33.3%, n = 14) they were highly interested in surgery but were undecided about whether they wanted to pursue it as a career (Figure 3A).
 |
Figure 1 Pie chart of undergraduate majors (%) of USIG participants (n = 35). Abbreviation: USIG, undergraduate surgery interest group. |
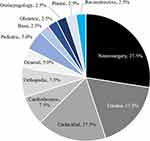 |
Figure 2 Pie chart of surgical specialties (%) that USIG members (n = 40) are interested in. Abbreviation: USIG, undergraduate surgery interest group. |
The post-event USIG questionnaires indicated that the high-fidelity surgical skills workshops were more effective than the low-fidelity workshops (median score, 5; IQR, 4.5 to 5). Premedical students thought that the use of high-fidelity medical equipment, isolation gear, and standardized surgical protocols simulated realistic medical trauma experiences (median score, 4; IQR, 3 to 5). They also noted that the guidance by surgeons and residents during these exercises improved their overall experience (median score, 5; IQR, 5 to 5).
The post-event questionnaires among USIG participants demonstrated that the very high pre-event levels of interest in surgery were sustained (median score, 5; IQR, 4 to 5; P = 0.696). Participants felt that the USIG had a high positive impact on their interest in surgery (median score, 5; IQR, 4 to 5) and that they were highly likely to attend another USIG event (median score, 5; IQR, 4 to 5). Their knowledge and degree of confidence in performing basic clinical and surgical skills significantly increased (P < 0.001) (Figure 3B).
Post-event comments on the questionnaires further substantiated student satisfaction. Sample comments included the following:
“I left the event feeling empowered and excited about what the future holds for my medical career. Thank you for this wonderful opportunity.”
“I think tonight’s event was an eye-opening experience. As a premed student, such a quick and realistic exposure to the surgical field isn’t always available … Thank you for extending your hand to students and making this a learning process.”
Influential Factors and Motivations
USIG participants were asked to evaluate the influence of various factors on their interest in surgery. They rated their intrinsic interest in the basic sciences as the highest positive factor. Other positive factors included surgeons’ opportunities to help patients on a personal level, the nobility of the profession, research opportunities in the surgical field, the influence of a surgical mentor, and resident lifestyle. Somewhat surprisingly, variables such as length of training, financial indebtedness, surgeon workload, and lifestyle and social obligations had no effect on their interest in surgery (Figure 4A, Total n = 40). Print and electronic media had a negative influence on their interest in surgery (median score, 2; IQR, 1 to 3).
When we compared our USIG (n = 40) and MSIG (n = 58) questionnaire results, we found several statistically significant differences (Figure 4B). Our USIG had a much higher proportion of female participants (75%, n = 30) than our MSIG (41.4%, n = 24; P = 0.0003). USIG participants rated variables such as resident lifestyle, social obligations, and research opportunities in the surgical field to have a positive influence on their interest in surgery (P < 0.01), whereas MSIG participants rated those factors as having a negative influence (P < 0.01). However, the influence of financial indebtedness, surgeon workload, length of training, a surgical mentor, and family opinions (all rated as either neutral or positively influential) were not significantly different between USIG and MSIG participants.
Discussion
Our USIG represents one of the first attempts to extend surgical education to undergraduate premedical students. Most educational endeavors have sought to increase enrollment into surgical training programs through interventions directed to either medical students or residents;13,25 USIG’s success is substantiated by the increase in its membership, and the positive feedback we have received from members and faculty alike. Our USIG participants reported a high level of interest in surgery pre- and post-event, with a significant increase in post-event confidence and knowledge in performing various surgical skills. We demonstrate how a simple educational model, implemented well before surgical training, can stimulate interest in the field. The funding required to run 8 workshops during a 1-year period was just over $2500. More than 40 surgeons and residents participated over the year, translating to a 2-hour commitment per faculty member, per year.
Multiple studies1–7,9,41 have evaluated the factors that affect medical students’ career choices, yet considerable debate continues on the best formula for choosing a surgical specialty. Passion, personality fit, quality of life, future income, program competitiveness, and mentorship all contribute to medical students’ choices. Studies evaluating temporal changes in attitudes concede that this process is dynamic: with certain factors being transitory, and other factors being permanent with a progressive impact.31 Our attempt to evaluate those factors during the undergraduate premedical years of training yielded valuable insights. For example, we found that the gender composition of our USIG and MSIG participants differed significantly, with a larger proportion of female participants in our USIG. Although 50% of all medical students in the United States are now women, only 24% of newly matriculating surgical residents are women.14 Female gender has been shown to be an independent negative predictor for pursuing a career in general surgery.14 Some authors partly attribute the declining interest in general surgery to the increased number of women enrolling in medical school.42,43 Increasing female surgical matriculation may mandate intervening at an earlier stage of education. Some studies have shown that students’ interactions early in medical school with at least 1 strong, positive role model, especially of the same gender, increase the propensity to choose the role model’s specialty.28,34–36 These dynamics are important to address as considerations of equity and diversity are made when intervening earlier. Neumayer et al44 noted that medical schools with a higher percentage of female surgeons have higher proportions of female medical students choosing surgery. Our USIG provides ample opportunity for students to interact with female surgical mentors and female surgical residents; our “meet-the-surgeon” sessions particularly focus on work-life balance and the challenges and rewards of a surgical career.
In our study, we found that resident lifestyle, traditionally viewed as long and demanding,14 was a positive influence among premedical students. Among medical students, however, resident lifestyle had a negative influence. Both our USIG and MSIG participants stated that family and surgical mentors were a positive influence. Many studies14,17,18,45 have stated the importance of a controllable lifestyle on residency choice, showing that both male and female students desire protected time. Sanfey et al14 observed that both male and female medical students were concerned with the work-life balance of their attending surgeons and surgical residents—and that both male and female students were equally discouraged from a career in surgery by the opinions of a spouse, family member, or significant other. The long hours and rigors of surgical residency often predispose trainees to depression.46 Many investigators1,18,26,42,47–49 have recommended surgical program and clerkship directors modify medical students’ surgery curricula to minimize exposure to the most rigorous aspects of resident life. Other program directors are highly skeptical, arguing that such an approach would be unethical and misleading since lifestyle concerns extend well beyond residency.50
Many educators agree that intervention strategies should optimally involve effective mentorship that starts early in medical school.13 Our study demonstrates a disparity in opinions between undergraduates and medical students. Reviewing this data, especially those concerning surgeon and resident lifestyle and social obligations, it may suggest that undergraduate premedical students may be naïve about the challenges of a surgical career. Even though our USIG provides an excellent opportunity for early mentorship, it aims to convey realistic insights into a surgeon’s life. During our workshops and discussions, faculty and residents have highlighted both the highs and lows of a surgical career. In our view, building a passionate, enthusiastic, and resilient workforce entails attracting the brightest, most appropriate students even in their undergraduate education. Erzurum et al26 have observed that students likely to pursue surgery were more resilient and willing to oversee the hardships of residency, and that such students were encouraged by those surgeons who have rewarding careers. However, students unlikely to pursue surgery were most discouraged by the lack of work-life balance among surgeons and surgical residents.4,14,50
Achievements in surgery can often be traced back to early educational experiences and effective mentorship. Effective mentorship fosters a sense of belonging, social support, well-being in the work place, and a sense of personal transformation.51 Today, ample opportunities exist for medical students to be dissuaded from pursuing surgery. Surgery, perhaps more so than other specialties, stands to lose substantially in terms of accruing and retaining resident applicants. Attrition rates for general surgery residents are nearly 20%.21,52 To address the attrition rate in general surgery and the decreased matriculation rates, the Blue Ribbon Committee on Surgical Education convened in 2004 and produced recommendations for surgical program directors across the nation.13 The committee’s report called for rapid innovations to surgical education and medical student curriculum development. This included training surgical mentors who are involved with medical students early, possibly from the first year of medical school, to ensure medical students’ early exposure to surgical experiences.13 We believe that the objectives of our USIG fall well within the recommendations made by the committee. Several studies have confirmed that earlier exposure to surgical experiences improves the likelihood of surgical matriculation.28,32–37 Several studies35,53 show that early interventions such as a summer program consisting of academic research, clinical observership, and mentorship could favorably influence the choice of surgery as a career.
We acknowledge several limitations of our study. First, the administration of our questionnaires and the collection of our data were limited to 2 skills workshops. Because of space constraints, not all registered members of our USIG could attend each workshop. Second, we designed our questionnaires to subjectively assess skills, confidence, and interest, but those metrics were not objectively assessed by an independent observer; consequently, we did not ascertain congruence between actual and perceived change. This was deemed acceptable as the rationale behind our workshops was to foster interest in surgery and to encourage faculty and mentor interactions, rather than to definitively impart and measure knowledge and know-how. Third, we concede our questionnaires, particularly questions regarding influential factors, may be susceptible to interpretation bias as many premedical students can be unaware of the various nuances of a surgical residency and lived-experiences of residents. Fourth, our study was a 1-year review; in the future, we hope to collect long-term, follow-up data to assess whether or not participants’ interest, knowledge, and skills were sustained. Furthermore, evaluating if USIG participants entered medical school or a surgical residency was beyond the scope of our study. Even if this were the case, proving causality would be onerous and arguably inaccurate. Our aim with USIG was to provide educational exposure to undergraduate premedical students to help them make an informed career choice, which may or may not be general surgery.
Conclusion
Our USIG provides unique opportunities for undergraduate premedical students to gain exposure to the field of surgery. Instituted at the request of premedical students interested in surgery and led by Department of Surgery faculty, it has garnered immense enthusiasm and robust participation by undergraduates and faculty alike. Participants’ post-event evaluations indicate a strong interest in pursuing surgery and an increased confidence in surgical knowledge and skills. Our data supports the merit of extending such educational opportunities to undergraduate premedical students and we lay a framework for other universities and educators to follow. At present, surgical education in the United States begins late in medical school training and continues through residency and fellowship training; we believe that implementing early educational initiatives, like ours, that provide hands-on experiences and realistic insights into surgery, can be immensely valuable.
Ethical Approval
This study was granted exemption status from the institutional review board of the University of Minnesota (study number: 1210E2318).
Acknowledgment
The authors thank Mary E. Knatterud, PhD, for her assistance in editing and reviewing this manuscript. We also acknowledge Marissa Peyer, BS, and Raghav Vadhul, BS, for their assistance in creating figures and tables. We would like to thank the Mick Lord Medical Education Fellowship Fund, James Lord Surgical Fellowship Fund, and William W Harmon Surgery Education and Research Fund. An earlier version of this article was presented at the American College of Surgeons Clinical Congress in Washington, DC, in 2016.
Funding
We did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. KI B, Isaacs G. Contemporary trends in student selection of medical specialties: the potential impact on general surgery. Arch Surg. 2002;137(3):259–267. doi:10.1001/archsurg.137.3.259
2. Gelfand DV, Podnos YD, Wilson SE, Cooke J, Williams RA. Choosing general surgery: insights into career choices of current medical students. Arch Surg. 2002;137(8):941–947. doi:10.1001/archsurg.137.8.941
3. Marshall DC, Salciccioli JD, Walton S-J, Pitkin J, Shalhoub J, Malietzis G. Medical student experience in surgery influences their career choices: a systematic review of the literature. J Surg Educ. 2015;72(3):438–445. doi:10.1016/j.jsurg.2014.10.018
4. Cochran A, Melby S, Neumayer LA. An Internet-based survey of factors influencing medical student selection of a general surgery career. Am J Surg. 2005;189(6):742–746. doi:10.1016/j.amjsurg.2005.03.019
5. Rudnicki J, Zyśko D, Kozłowski D, et al. The choice of surgical specialization by medical students and their syncopal history. PLoS One. 2013;8(1):e55236. doi:10.1371/journal.pone.0055236
6. Al-Heeti KNM, Nassar AK, DeCorby K, Winch J, Reid S. The effect of general surgery clerkship rotation on the attitude of medical students towards general surgery as a future career. J Surg Educ. 2012;69(4):544–549. doi:10.1016/j.jsurg.2012.04.005
7. Barshes NR, Vavra AK, Miller A, Brunicardi FC, Goss JA, Sweeney JF. General surgery as a career: a contemporary review of factors central to medical student specialty choice. J Am Coll Surg. 2004;199(5):792–799. doi:10.1016/j.jamcollsurg.2004.05.281
8. Wilson I, Cowin LS, Johnson M, Young H. Professional identity in medical students: pedagogical challenges to medical education. Teach Learn Med. 2013;25(4):369–373. doi:10.1080/10401334.2013.827968
9. Miah S, Pang KH, Rebello W, et al. What factors influence UK medical students’ choice of foundation school? Adv Med Educ Pract. 2017;8:293–297. doi:10.2147/amep.s134081
10. Charting Outcomes in the Match: U.S. Allopathic Seniors. National Resident Matching Program.
11. National Resident Matching Program. NRMP.
12. NRMP Historical reports: main residency match 1984–2002. National Resident Matching Program.
13. Debas HT, Bass BL, Brennan MF, et al. American surgical association blue ribbon committee report on surgical education: 2004. Ann Surg. 2005;241(1):1–8. doi:10.1097/01.sla.0000150066.83563.52
14. Sanfey HA, Saalwachter-Schulman AR, Nyhof-Young JM, Eidelson B, Mann BD. Influences on medical student career choice: gender or generation? Arch Surg. 2006;141(11):1086–1094. doi:10.1001/archsurg.141.11.1086
15. Tambyraja AL, McCrea CA, Parks RW, Garden OJ. Attitudes of medical students toward careers in general surgery. World J Surg. 2008;32(6):960–963. doi:10.1007/s00268-008-9529-5
16. Yu T-C, Jain A, Chakraborty M, Wilson NC, Hill AG. Factors influencing intentions of female medical students to pursue a surgical career. J Am Coll Surg. 2012;215(6):878–889. doi:10.1016/j.jamcollsurg.2012.08.018
17. Schwartz RW, Haley JV, Williams C, et al. The controllable lifestyle factor and students’ attitudes about specialty selection. Acad Med. 1990;65(3):207–210. doi:10.1097/00001888-199003000-00016
18. Evans S, Sarani B. The modern medical school graduate and general surgical training: are they compatible? Arch Surg. 2002;137(3):274–277. doi:10.1001/archsurg.137.3.274
19. Schwartz RW, Simpson WG, Strodel WE, Jarecky RK, Griffen WO
20. Hutter MM, Kellogg KC, Ferguson CM, Abbott WM, Warshaw AL. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006;243(6):864–875. doi:10.1097/01.sla.0000220042.48310.66
21. Gifford E, Galante J, Kaji AH, et al. Factors associated with general surgery residents’ desire to leave residency programs: a multi-institutional study. JAMA Surg. 2014;149(9):948–953. doi:10.1001/jamasurg.2014.935
22. Dodson TF, Webb ALB. Why do residents leave general surgery? The hidden problem in today’s programs. Curr Surg. 2005;62(1):128–131. doi:10.1016/j.cursur.2004.07.009
23. Yaghoubian A, Galante J, Kaji A, et al. General surgery resident remediation and attrition: a multi-institutional study. Arch Surg. 2012;147(9):829–833. doi:10.1001/archsurg.2012.1676
24. Dimou FM, Eckelbarger D, Riall TS. Surgeon burnout: a systematic review. J Am Coll Surg. 2016. doi:10.1016/j.jamcollsurg.2016.03.022
25. Hale AJ, Ricotta DN, Freed J, Smith CC, Huang GC. Adapting maslow’s hierarchy of needs as a framework for resident wellness. Teach Learn Med. 2019;31(1):109–118. doi:10.1080/10401334.2018.1456928
26. Erzurum VZ, Obermeyer RJ, Fecher A, et al. What influences medical students’ choice of surgical careers. Surgery. 2000;128(2):253–256. doi:10.1067/msy.2000.108214
27. Chapman SJ, Hakeem AR, Marangoni G, Raj Prasad K. How can we enhance undergraduate medical training in the operating room? A survey of student attitudes and opinions. J Surg Educ. 2013;70(3):326–333. doi:10.1016/j.jsurg.2013.01.008
28. Patel MS, Khalsa B, Rama A, et al. Early intervention to promote medical student interest in surgery and the surgical subspecialties. J Surg Educ. 2013;70(1):81–86. doi:10.1016/j.jsurg.2012.09.001
29. Council on Graduate Medical Education (COGME) ER. Patient Care Physician Supply and Requirements: Testing COGME Recommendations. Maryland; 1996.
30. Nash DB, Veloski JJ. Emerging opportunities for educational partnerships between managed care organizations and academic health centers. West J Med. 1998;168(5):319–327.
31. Zimmy GH, Senturia AG. A longitudinal study of consistency of medical student specialty choice. Acad Med. 1974;49(12):1179–1181. doi:10.1097/00001888-197412000-00010
32. Ologunde R, Rufai SR, Lee AHY. Inspiring tomorrow’s surgeons: the benefits of student surgical society membership☆? J Surg Educ. 2015;72(1):104–107. doi:10.1016/j.jsurg.2014.06.004
33. Li R, Buxey K, Ashrafi A, Drummond KJ. Assessment of the role of a student-led surgical interest group in surgical education. J Surg Educ. 2013;70(1):55–58. doi:10.1016/j.jsurg.2012.08.002
34. Kozar RA, Lucci A, Miller CC, et al. Brief intervention by surgeons can influence students toward a career in surgery11Presented at the annual meeting of the association for academic surgery, boston, massachusetts, november 2002. J Surg Res. 2003;111(1):166–169. doi:10.1016/S0022-4804(03)00104-5
35. Hernandez J, Al-Saadi S, Boyle R, et al. Surgeons can favorably influence career choices and goals for students interested in careers in medicine. J Am Coll Surg. 2009;209(1):62–67. doi:10.1016/j.jamcollsurg.2009.02.065
36. Sedaghat N, Mondy J, Eslick GD, Cox MR. Exposure of medical students to surgery: the nepean summer vacation surgical program. J Surg Educ. 2012;69(5):580–587. doi:10.1016/j.jsurg.2012.06.003
37. Salna M, Sia T, Curtis G, Leddy D, Widmann WD. Sustained increased entry of medical students into surgical careers: a student-led approach. J Surg Educ. 2016;73(1):151–156. doi:10.1016/j.jsurg.2015.08.012
38. Goldin SB, Schnaus MJ, Horn G, et al. Surgical interest and surgical match for third-year students: results of a prospective multivariate longitudinal cohort study. J Am Coll Surg. 2012;215(5):599–606. doi:10.1016/j.jamcollsurg.2012.06.416
39. Kolb DA, Kolb AY The kolb learning style inventory 4.0: guide to theory, psychometrics, research & applications learning sustainability view project how you learn is how you live view project; 2013. Available from: https://www.researchgate.net/publication/303446688.
40. Undergraduate Surgery Interest Group. Available from: http://usigumn.org/.
41. Pawełczyk AM, Kotlicka-Antczak MZ, Chmielińska A, Pawełczyk TP, Rabe-Jabłońska J. Temperament traits and preference for surgical or nonsurgical specialties in year 6 medical students. Teach Learn Med. 2014;26(4):387–392. doi:10.1080/10401334.2014.945026
42. Wendel TM, Godellas CV, Prinz RA. Are there gender differences in choosing a surgical career? Surgery. 2003;134(4):591–598. doi:10.1016/S0039
43. Lind DS, Cendan JC. Two decades of student career choice at the University of Florida: increasingly a lifestyle decision. Am Surg. 2003;69(1):53–55.
44. Neumayer L, Freischlag J, Levinson W. Demographics of today’s woman surgeon. Bull Am Coll Surg. 1994;79(2):28–33.
45. Novielli K, Hojat M, Park PK, Gonnella JS, Veloski JJ. Change of interest in surgery during medical school: a comparison of men and women. Acad Med. 2001;76(10 Suppl):S58–S61.
46. Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–451. doi:10.1097/ACM.0000000000000134
47. Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003;290(9):1173–1178. doi:10.1001/jama.290.9.1173
48. Polk HCJ. The declining interest in surgical careers, the primary care mirage, and concerns about contemporary undergraduate surgical education. Am J Surg. 1999;178(3):177–179. doi:10.1016/s0002-9610(99)00167-1
49. Bickel J, Brown AJ, Generation X. implications for faculty recruitment and development in academic health centers. Acad Med. 2005;80(3):205–210. doi:10.1097/00001888-200503000-00003
50. Minor S, Poenaru D, Park J. A study of career choice patterns among Canadian medical students. Am J Surg. 2003;186(2):182–188. doi:10.1016/S0002-9610(03)00181-8
51. Afghani B, Santos R, Angulo M, Muratori W. A novel enrichment program using cascading mentorship to increase diversity in the health care professions. Acad Med. 2013;88(9):1232–1238. doi:10.1097/ACM.0b013e31829ed47e
52. Khoushhal Z, Hussain MA, Greco E, et al. Prevalence and causes of attrition among surgical residents a systematic review and meta-analysis. JAMA Surg. 2017;152(3):265–272. doi:10.1001/jamasurg.2016.4086
53. Block L, Wang K, Gao CC, Wu AW, Feldman LS. There’s a lot more to being a physician: insights from an intensive clinical shadowing experience in internal medicine. Teach Learn Med. 2018;30(3):266–273. doi:10.1080/10401334.2017.1415148
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


