Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
An Online Structured Diabetes Self-Management Education and Support Programme Improves Glycaemic Control in Young Adults with Type 1 Diabetes
Authors An L, Yeh KC, Liu Y, Wang D, Li X, Tang Q, Lu J
Received 24 March 2023
Accepted for publication 15 August 2023
Published 7 September 2023 Volume 2023:16 Pages 2641—2654
DOI https://doi.org/10.2147/JMDH.S414102
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Lingwang An,1 Kuei-Chun Yeh,1 Yunxia Liu,1 Dandan Wang,1 Xianglan Li,1 Qi Tang,1 Juming Lu1,2
1Department of Endocrinology, Beijing Ruijing Diabetes Hospital, Beijing, 100079, People’s Republic of China; 2Department of Endocrinology, The General Hospital of the People’s Liberation Army, Beijing, 100853, People’s Republic of China
Correspondence: Juming Lu, Department of Endocrinology, The General Hospital of the People’s Liberation Army, No. 28 of Fuxing Road, Haidian District, Beijing, 100853, People’s Republic of China, Tel +86 10 8822 9999, Email [email protected]
Objective: We explore the effect of a structured online DSMES program on glycaemic control and the self-management behaviour of adolescents and young adults with T1DM.
Methods: We used a pre–post uncontrolled intervention design over a period of 6 months. A total of 37 youths with T1DM aged 10– 45 years were enrolled. The intervention comprised 11 structured online DSMES course sessions; these were video-based and delivered by a diabetes specialist, nurses and a dietitian. The primary outcome was a change in (glycated hemoglobin) HbA1c. The secondary outcomes were changes in hypoglycaemia frequency, time in target range (TIR) among patients using a continuous glucose monitoring (CGM) system and self-management behaviour; the latter was measured using a T1DM self-management scale for Chinese adults (SMOD-CA) and the Chinese version of the diabetic behaviour rating scale in adolescents with T1DM (DBRS).
Results: Twenty-three (85.2%) participants attended ≥ 8 of the online sessions. There was a significant reduction in HbA1c (from 6.92% to 6.47%, P = 0.002), hypoglycaemic episodes (from 6.0 to 4.0 during the preceding month, P = 0.026) and a significant increase in TIR (from 74.0% to 80.5%, P = 0.027) and an increase in the SMOD-CA score (from 79.6 to 84.6, P = 0.026) in young adults. No significant change in glucose control, hypoglycaemic events or DBRS score were found among children and adolescents. The score of the 12-item version of the Barrett–Lennard Relationship Inventory (B-L RI:mini) indicated that more than half of the participants experienced congruence, positive regard, and an empathic understanding in this programme.
Conclusion: The online structured DSMES programme was effective in improving the glycaemic control and self-management behaviour of young adults with T1DM; however, integrating offline visits or appointments with online consultations may be necessary for youth patients.
Keywords: children and adolescents, youth, type 1 diabetes, structured diabetes self-management education and support, online
Introduction
Type 1 diabetes mellitus (T1DM) is a long-term chronic disease that has an important impact on the lives of patients and their families. Glycaemic control is challenging and was found to be sub-optimal in Chinese patients with T1DM with a median glycated hemoglobin (HbA1c) level of above 8.5% among children, adolescents and adults.1–3 Structured courses for diabetes self-management education and support (DSMES) are suggested to provide those living with T1DM (and their caregivers, where applicable) with the knowledge, skills and confidence to successfully self-manage their condition, and to empower them with an emphasis on shared decision-making and active collaboration with the health-care team, thereby reducing the risks of acute and long-term complications while maintaining quality of life.4 Structured DSMES programs for T1DM often include multiple components and cover a broad range of topics, from pathophysiology to medical technology and healthy coping mechanisms and have been proven considerably beneficial for achieving lower HbA1c levels, less hypoglycaemia and improved quality of life.5–9
Face-to-face DSMES in hospitals has many disadvantages, including inconvenience, lacking of individualization and low efficiency.10 The Corona Virus Disease-19 (COVID-19) pandemic has initiated rapid reconsideration of how health care is delivered. Globally, 30% of patients reported that the pandemic had affected their healthcare access due to cancelled physical appointments with their health-care providers.11 An education program based on an internet platform was considered popular as it presented the convenience of repeatable learning, flexibility, and improved glycaemic control.12,13 Considering that programmes that are based on mobile health (mHealth) applications (apps) require a significant demand for technical and/or digital support, more convenient and accessible platforms, eg WeChat or video conference, will be more practical for a medical team to use when providing their own education projects. WeChat and Tencent video conference platforms are widely used among smartphone users and had been adopted by health-care professionals in China.14–17
Our team has provided DSMES for patients with T1DM since 2016 with a professional team that includes doctors, certified nurses and a dietitian and has published our work in this field to promote behavioural change and glycaemic control among patients with T1DM.18 Thus, we further collated and updated existing DSMES courses according to the latest guidelines and evidence and presented them in video form in 2021. This study explores the effect of this structured online DSMES programme, based on a series of video courses on glycaemic control and self-management behaviour, for adolescents and young adults with T1DM.
Materials and Methods
Participants
The target population were children, adolescents (or their caregivers) and youth with T1DM who believed their glycaemic control to be suboptimal or had difficulties dealing with fluctuations in blood glucose. Participants who had received a diagnosis of T1DM based on hospital records or met the diagnostic criteria for T1DM according to the 1999 World Health Organization (WHO) report19 were considered eligible. Detailed inclusion and exclusion criteria are listed in Table 1. Online advertising about this project, which included short video courses, was published on WeChat public accounts and WeChat groups for T1DM patients. Interested respondents were provided with details about the trial and were assessed for their eligibility by the project doctor via WeChat or mobile phone calls.
 |
Table 1 Eligibility Criteria |
Design
This study was a pre–post uncontrolled intervention study of an online DSMES intervention for people with T1DM over 24 weeks conducted in Beijing, China.
Setting
The trial setting was a primary care hospital, Beijing Ruijing Diabetes Hospital, which focuses on delivering person-centred diabetes care and management. We collected and screened the information provided by individuals with T1DM.
Measures
Information on demographic characteristics, anthropometric measurements, biochemical indicators, duration of diabetes (years), the presence of macrovascular and microvascular diabetes complications, past medical history and questionnaires were collected. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Biochemical indicators included fasting plasma glucose (FPG) and HbA1c, and blood lipid profiles were tested by a local medical institution laboratory close to where the patient lived. An episode of hypoglycaemia was defined as a glucose value (by self-monitoring) below 3.9 mmol/L or presentation with classic symptoms. The primary outcome was a change in HbA1c from baseline over a period of 6 months. The secondary outcomes were changes in hypoglycaemic frequency, time in target range (TIR) for patients using a continuous glucose monitoring (CGM) system and self-management behaviour. Whether HbA1c improved or was maintained below the age target (HbA1c <7.0% for adults, HbA1c <7.5% for patients younger than 18 years) was also accessed as a secondary outcome. Behavioural changes were measured using the self-management scale for T1DM for Chinese adults (SMOD-CA)20 and the Chinese version of the diabetic behaviour rating scale in adolescents with T1DM (DBRS).21 The 12-item version of the Barrett–Lennard Relationship Inventory (B-L RI:mini) was used to specifically evaluate the extent to which people experienced the facilitative conditions of congruence, unconditional positive regard, and empathic understanding.22 The detailed items included controlling emotion to avoid affecting blood glucose, adjusting insulin doses according to blood glucose level, diet and exercise, checking blood glucose levels regularly using a meter, establishing why blood glucose levels were too high/too low, keeping blood glucose in the normal range and preventing and monitoring acute and chronic complications. Participants’ responses to the items of the SMOD-CA were in a five-point scale range, and the total score was obtained by adding together the scores of all items.20 The higher the SMOD-CA score (range, 0–120), the better the self-management ability. The DBRS and B-L RI:mini scores were calculated according to the corresponding method.21,22 The insulin-injection version of the DBRS has 36 items, and the pump version has 37 items. The DBRS score was calculated as a proportion of the maximum possible score (possible scores of 0.0–1.00) with high scores reflecting greater adherence and stronger self-management ability. The higher the B-L RI:mini score, the higher the extent to which people experienced congruence, positive regard and empathic understanding.
Intervention
The intervention included two modules: (1) a series of online structured DSMES video-based course sessions and personalised or specific discussion about any possible confusion; (2) interactions and support via the WeChat platform through text, audio or video. The DSMES team for this T1D-SDOS project consisted of clinicians, a psychologist, certified nurses and dietitians with profound experience in the medical care of patients with T1DM and who were trained specifically for this project. The 11 structured DSMES sessions (Table 2) were produced and conducted by them. All the video DSMES courses were reviewed by diabetes specialists before and after production.
 |
Table 2 Key Contents of DSMES Video Courses |
After enrolment and comprehensive personalised assessment, all participants were offered 11 structured DSMES sessions over 3 months. Date and time were agreed on for each session, at which time the patient and the DSMES team met on the Tencent video conference platform to watch video courses and have discussions by voice or typing in real-time. Each session lasted 60–90 min. Peers with experience were invited to share on the platform and were required to prepare the shared content in advance for professional review. Each enrolled participant had one case manager and one personal WeChat group with his/her DSMES team for real-time interactions. The individual problems of patients were discussed in his/her personal WeChat group via text message or voice calls during this period of time and in the month after that for follow-up. The two age groups were applied to the same intervention.
Ethics
Informed consent by WeChat or telephone was obtained from all participants, and a photo of the hard copy signed consent form was sent and received via WeChat. For participants under 18 years of age, a parent or legal guardian also provided informed consent. The study was carried out in accordance with the principles of the Declaration of Helsinki and received ethics approval from the ethics committee of the Beijing Ruijing Diabetes Hospital (2021 Ethics Approval [Department] no. 010).
Statistical Analyses
All statistical analyses were performed using the SPSS V.22.0 software. Continuous variables were expressed as mean ± standard deviation (SD) for normally distributed variables, and median (25% and 75% quartile) for variables not normally distributed. Categorical variables were expressed as numbers (%). The changes from baseline to follow-up for an individual were examined using a paired t-test for normally distributed variables, Wilcoxon–Mann–Whitney test for skewed distributed variables and a chi-square test for categorical variables. The changes in HbA1c, frequency of hypoglycaemia, TIR, time below range (TBR), time above range (TAR), SMOD-CA and DBRS scores were tested. Significance was established based on a two-tailed P-value of ≤0.05.
Results
Of the 46 people who consented to be included in the study, 9 (19.6%) were excluded from the final analysis for not attending any of the online sessions (1 person) or not completing any follow-up biochemical measurements and questionnaires (8 people). A total of 37 (81.4%) subjects were enrolled in the final analysis; among them, 27 (73.0%) were young adults above 18 years and 10 (27.0%) were children and adolescents younger than 18 years (Figure 1).
 |
Figure 1 Study design and flow chart of the participant recruitment and follow-up. |
Baseline Characteristics and Online DSMES Courses Attendance
Among the young adults, 7 (25.9%) were men, the mean age was 31.0 ± 5.9 years, the duration of diabetes was 5.1 (2.4 ~ 11.2) years, 10 were pump users (37.0%) and 24 were CGM users (88.9%), 23 (95.8%) of whom provided a CGM report. The mean HbA1c was 6.9% ± 0.8%, and the mean TIR was 74.6% ± 12.0%. Twenty-three (85.2%) participants attended ≥8 online sessions. For the four online sessions in the first month about knowledge and skills for blood glucose control, 25 (92.6%) completed all 4 sessions. Among the children and adolescents, 2 (20.0%) were men, the mean age was 12.1 ± 2.0 years, the duration of diabetes was 1.4 (0.5 ~ 2.0) years, 5 were pump users (50.0%) and 10 were CGM users (100.0%), only 3 of whom successfully (30.0%) provided a recent CGM report. Participants who attended ≥8 online sessions and completed all previous 4 sessions numbered 6 (60.0%) and 8 (80.0%), respectively (Table 3). The mean HbA1c was 7.3% ± 1.4%, and the mean TIR was 82.4% ± 12.3%.
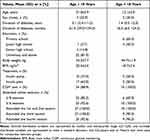 |
Table 3 Baseline Characteristics of Study Participant |
Changes in Glycaemic Control
It was suggested that the HbA1c level be measured at 12 and 24 weeks following recruitment. However, due to the impact of COVID-19 prevention and control measures and the inconvenience of undergoing medical and laboratory examinations, most participants only completed data for only one follow-up. The follow-up HbA1c data were provided at 3 months by 14 (51.9%) and at 4–6 months by 13 (48.1%) young adults, while the data for children and adolescents were 50% vs 50%. The follow-up CGM data were provided by 22 (81.5%) young adults and by 10 (100.0%) children and adolescents, however, only 21 young adults and 3 adolescents had paired baseline and follow-up CGM data (Table 4).
 |
Table 4 Changes in HbA1c, TIR and Hypoglycemic Event in Study Population from Baseline to Follow-Up |
Glucose control improved after online DSMES intervention. There was a significant reduction in HbA1c (from 6.92% to 6.47%, P = 0.002), an increase in TIR (from 74.0% to 80.5%, P = 0.027) and a reduction in hypoglycaemic episodes (from 6.0 to 4.0, P = 0.026) in last month in young adults. There was a modest but not significant reduction in TAR (from 19.8% to 13.6%, P = 0.057). No change was observed in the TBR. No significant change was found in glucose control and hypoglycaemic events among children and adolescents (Table 4). The mean TIR, TBR and TAR of the 10 children and adolescents at follow-up were 76.8%, 4.8% and 18.4%, respectively; these are shown in Table 4.
Changes in Self-Management Behaviour
A total of 35 participants completed the baseline and follow-up questionnaires for self-management behaviour. One adult did not submit SMOD-CA data. For participants aged ≥18, there was a significant improvement in SMOD-CA score (79.6 ± 14.1 vs 84.6 ± 14.4, P = 0.026), primarily in the domains of coping with disease-related problems (7 items scoring 0 ~ 28) and the goals of disease management (6 items scoring 0 ~ 24). Daily performance (6 items scoring 0 ~ 24), such as recording blood glucose measurements, carrying sweets, sugary biscuits or sugary drinks, showed relatively good results with modest but non-significant improvements being observed. No significant change was found in the domains of disease management and collaboration (11 items scoring 0 ~ 44) (Table 5).
 |
Table 5 Changes in Behavior and Life Quality Score |
For detailed items of disease management and collaboration, similar trends were found at baseline and follow-up: (1) around 75% of patients often followed the doctor’s advice regarding monitoring and the daily management plan; (2) about 80% of patients often learned from experienced diabetic patients and obtained diabetes information from relevant books and websites; (3) more than 85% of patients did not often work with medical staff to create an individualised diet plan and exercise regimen; (4) around 75% of patients did not often discuss diabetes issues with family members or friends.
For participants aged <18, there were no significant changes in DBRS scores and their domains (Table 5). The score for daily prevention (~0.75) and intervention (~0.65) behaviours were relatively high at baseline and follow-up, indicating very good adherence to the doctor’s advice concerning, eg food plans and weighing, regular exercise, blood glucose monitoring and recording, insulin use and changing the injection site. When participants experienced “low” or “high” blood sugar symptoms, the correct actions were also often taken by the participants.
The score for modification to a diabetes care plan was less than 0.6 and was not improved after intervention, indicating that modification to self-management behaviour did not occur often, including changing meals, implementing snacks and insulin dose according to the amount of exercise or adjusting insulin dose according to meals and blood glucose. The score for other diabetes care practices was also below 0.6; this also reflected no improvement, indicating a lack of support among friends, teachers, clinic doctors or nurses.
The Relationship Between HbA1c Change and Self-Management Behaviour
Overall, there were no significant differences between HbA1c change and the frequency of online course attendance and behavioural scores. The number of cases in which HbA1c had not improved, or where participants failed to maintain a low target level, comprised only 3 in the group aged ≥18 and 1 in the group aged <18. There were neither consistent nor obvious differences in the number of attended online courses and behaviour scores between these 4 participants nor those who achieved an improvement in HbA1c levels or maintained it below the target.
In the group aged ≥18, the HbA1c increased by 0.2%, 0.3% and 1.6% among 3 patients. HbA1c at follow-up were 7.2%, 7.1% and 8.0%, respectively, and were not maintained within the target range of <7.0%. One participant had an increased HbA1c level from 6.4% to 8.0% but a SMOD-CA score increase by 18. The participant’s HbA1c increased because she had been inactive for a month and a half. The reasons for this lack of activity were a fall on a rainy day, although no fractures really affected her physical activity as a result, as well as isolation policies concerning COVID-19 prevention and control. The participants' work pressure during this period was also quite high.
In the group aged <18, participant 31 had an increased HbA1c level from 7.1% to 7.5%, which was the age target threshold. This participant encountered a problem related to parent–child communication. Her mother did not allow her to use insulin independently at school or gatherings or when eating with classmates, nor did she allow any adjustments to insulin doses. Sometimes, the mother was unsure whether her daughter told her the truth about what and how much she ate. One participant experienced an increase in hypoglycaemic episodes by 6, but a decrease in HbA1c level. She had been quarantined with her mother, could only obtain fast food and had difficulty obtaining insulin degludec.
The Experience of Congruence and Positive Regard for the Programme
The B-L RI:mini score was 24.3 ± 5.3 in the group aged ≥18 with 15 (55.6%) participants scoring above 24.0; the score was 24.3 ± 4.2 in the group aged <18 with 5 (50.0%) participants scoring above 24.0. This indicates that more than half of the study population experienced congruence, positive regard and empathic understanding through their involvement in the programme. This means that they experienced affection, understanding and feelings of being valued by the DSMES team. Despite being unable to see each other face to face, participants agreed that the DSMES team understood what they meant to say or what they felt and shared their true impressions and feelings with them.
No significant difference was found between groups for B-L ≥24 and B-L <24 scores in terms of HbA1c change, hypoglycaemic episode changes, follow-up behaviour scores, age, sex, duration of diabetes, insulin treatment device, living area, or medical insurance in both groups aged ≥18 and <18. For the group aged <18, no significant differences were found in terms of parents’ education level or whether classmates or teachers knew about their T1DM diagnosis. However, more participants aged ≥18 in the B-L <24 score group showed improved scores for coping with disease-related problems, as well as in other diabetes care practices than in the group aged <18 (Table 6).
 |
Table 6 The Characters Comparison Between Groups of Changes in Behavior and Life Quality Score |
Discussion
Changes in Glycaemic Control and Behaviour in the Group Aged ≥18
The COVID-19 pandemic affected healthcare delivery and led to difficulties attending or the cancellation of physical appointments with health-care providers. The high programme attendance and improvements in glycaemic control and SMOD-CA scores in patients aged ≥18 demonstrated that the online structured DSMES programme was feasible and helpful.
Although the baseline glycaemic control of the young adults enrolled in the study was good, significant improvements were still found for HbA1c, TIR and hypoglycaemic events. The improvement in HbA1c (–0.45%) was comparable with a previous study examining the effect of diabetes-focused cognitive behavioural therapy via a secure online real-time instant messaging system (mean HbA1c change: –0.57%)23 among patients with a high baseline HbA1c level. The effect of high engagement via a mobile peer support community using the mHealth application (mean HbA1c change: –0.4% to –0.6%)24 among T1DM patients with a relatively low HbA1c level was also observed. Similar improvements in TIR were found in another study evaluating the efficacy of structured telemedicine visits among CGM users with T1DM under the extreme circumstances of COVID-19.25 Although these studies were not designed as randomised controlled trials (RCTs), the effect of online intervention showed consistent results. The effect of the online DSMES programme on hypoglycaemic episodes was also found in a 4-week, partly web-based group intervention study called HypoAware.26,27 The pre–post pilot study showed significant improvement in not worrying about hypoglycaemia and diabetes distress and a rise in self-care confidence,26 while the subsequent cluster RCT study reported fewer severe hypoglycaemic episodes, significantly improved hypoglycaemia awareness and less hypo-distress.27
Behaviour is central to the management of diabetes, both for patients and for healthcare professionals delivering evidence-based care. Although self-management behaviour may not lead to an improvement in glycaemic control, effective behaviour management and psychological well-being are foundational for achieving treatment targets for people with diabetes.28,29 Components of the course curricula that were perceived as fundamental by diabetes educators included carbohydrate counting, insulin-dose adjustment, hypoglycaemia management, group work, goal setting and empowerment and confidence and control.30 The broad areas of self-management behaviour identified were carbohydrate counting and awareness, insulin-dose adjustment, self-monitoring of blood glucose, managing hypoglycaemia, managing equipment and injection sites and accessing health care30 These elements were implemented as key components of our structured online DSMES programme using video-based courses and were discussed accordingly during online attendance. The significant improvement in the self-management behaviour of the 18–45-year-old young adults in our study in the domains of coping with disease-related problems and disease management goals indicated the success of this structured online DSMES programme. The high proportion of patients who often followed the doctor’s advice for monitoring and a daily management plan and who learned from other diabetic patients and relevant books and websites at both the baseline and follow-up indicated that an understanding of the importance of these aspects was consistent and undisputed. All of these results may to some extent have contributed to the improvement in HbA1c levels and the decrease in hypoglycaemic events.
We did not further explore the reason for the low proportion of patients who worked alongside medical staff to create individualised diet and exercise regimens. The reasons for this were similar to those of a previous study that explored the barriers to non-attendance in diabetes education, eg learning about diabetes from other sources (55.5%) and patients feeling able to cope on their own (52.9%).10 Individualised adjustments were quite complex, and patients may have had their own preferred dietary habits. An investigation31 of the current status of nutrient intakes and glycaemic control in adults with T1DM showed that only 43.9% of participants reached the energy proportion of carbohydrates recommended in the Chinese Dietary Guidelines for Diabetes (2017);32 50.9% showed an excess fat intake and 52.6% an excess protein intake. During the first courses of healthy eating and insulin use in our programme, we introduced the impact of a diverse dietary composition (eg carbohydrates, fats, protein, glycaemic index and glycaemic load) on glucose levels and how to use insulin. Since patients are more familiar with their own lives than medical staff, their theoretical knowledge and personal experience accumulation will be useful for learning to use insulin flexibly to meet their daily needs and to control personal glycaemic responses to different foods.33,34 We did not explore the reasons for the low proportion of patients who discussed their condition with family members or friends. The reasons for this deficiency may be a lack of understanding about T1DM among the public and some participants hiding their diabetes as noted in a previous report.35
Changes in Glycaemic Control and Behaviour in the Group Aged <18
There was no programme effect on HbA1c among the children and adolescent groups. The small sample size, relatively good baseline glycaemic control, lack of traditional face-to-face communication and the fact that the programme was not specifically designed for adolescents may have been possible reasons for this. The benefit of programmes that are specific to diabetes-related challenges in adolescents and that incorporate technology or social media with T1DM was demonstrated in a previous study.36 A structured educational programme with intensive coaching at scheduled outpatient appointments and supported with extensive telephone calls and emails also demonstrated significant improvements in glycaemic control among children aged 5–11.9 years of age with a high baseline HbA1c.5 Thus, integrating offline courses and appointments with the structured online DSME programme may be of great importance for children and adolescents with T1DM. As recommended in the current global standard of care for children and adolescents with T1DM, quarterly visits with diabetes educator and endocrinologist, diabetes camps and other forms of real-time education are all worth considering.37 For negative results concerning glycaemic control, the influence of a treatment regimen, hormonal changes and interactions with others (especially parents) is also of great significance.38,39 A study identified the health-care needs of patients with T1DM during the adolescence-to-adulthood transition period; the results showed that being understood and accepted and being given appropriate autonomy to develop independence and responsibility were two important needs of the internal support dimension.39 Although adolescent patients want their parents to be involved, they also fear being controlled by their parents. The situation is complex with no perfect solution; this was the case for participant 31 in our study.
The behaviour change wheel theory indicated that capability (the necessary knowledge and skills), motivation (all of the brain processes that energise and direct behaviour) and opportunity (all the factors making the behaviour or motivation possible) interacted to generate behaviour and the outcome of glycaemic control.40 In our online DSMES programme, no significant changes in self-management behaviours were found in children and adolescents (measured using DBRS). The average DBRS score (0.62, out of 1) was less than that in another study focused on adolescents with T1DM (3.5 ~ 4.0, measured using a 5-point scale).41 The high score for daily prevention behaviours (~0.75) and intervention behaviours (~0.65), the low score for modifications to a diabetes care plan (~0.60) and other diabetes care practices (~0.60) indicated the need for additional research in the area of flexible behavioural modification, adjusting insulin use and support from other aspects. The establishment of accurate disease knowledge and the cultivation of disease management capabilities were very important health-care needs.
The Experience of Congruence and Positive Regard in This Program
Only slightly more than half of the participants had a B-L RI:mini score above 24.0. Although this score did not contribute to glycaemic control or changes in behaviour aspects, more efforts are needed to improve the experience of the type of online DSMES programme presented herein. Based on consensus among patients, primary caregivers and health-care providers, providers should (1) replace accusations with gentle reminders and avoid words that convey indifference and impatience; (2) understand the respective concerns and needs of the primary caregiver and the patient during a consultation with a physician; (3) provide healthcare guidance that meets the cognitive development and disease needs of patients of all ages.39 Integrating offline courses and appointments into a structured online DSME programme could also be useful.
Limitations
This study is limited by its relatively small sample size (n = 37), short duration of follow-up (6 months) and lack of randomisation. Therefore, the results should be interpreted with caution until they can be replicated in a larger and more rigorous study. Despite these limitations, the results have several important clinical practice implications. First, as demonstrated by the outcome improvements in the group of young adults, the online DSMES courses and meeting with a diabetes educator and endocrinologist online indicate positive efficacy in the Chinese context. This type of approach could be offered as an alternative or integrated with typical visits. Second, since patients with T1DM in China are widely dispersed across counties and provinces, and 60.6% of newly diagnosed T1DM patients in China are younger than 30,42 the online structured DSMES video courses could be disseminated in clinics and as online media to improve public knowledge and skills of T1DM management. Third, the offline DSME programme, visits or appointments may be very important for children and adolescents with T1DM and their parents and should be integrated with the online DSMES courses.
Conclusion
A three-month online structured DSMES programme based on a set of video courses enabled most participants to experience a feeling of congruence, positive regard and empathic understanding and improved the glycaemic control and self-management behaviour of young adults with T1DM. Offline DSMES courses, visits or appointments may be of significant importance for children and adolescents with T1DM and their parents and should be integrated with online structured DSMES courses.
Acknowledgments
The authors thank all the experts, all the children and adolescents and youth with T1DM involved in this work. This research was supported by the Hunan Province Sinocare Diabetes Foundation (Grant Number: 2021SD10).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Hunan Province Sinocare Diabetes Foundation Sweet Doctor Project Approval 2021SD10.
Disclosure
The authors declare that there is no conflict of interest associated with this manuscript.
References
1. Wu D, Gong CX, Meng X, Wei YL. Glycemic control and management of type 1 diabetes mellitus children in Beijing during 10 years. Chin J Appl Clin Pediatr. 2013;28(14):1096–1098. doi:10.3760/cma.j.issn.2095-428X.2013.14.017
2. Liu L, Yang D, Zhang Y, et al. Glycaemic control and its associated factors in Chinese adults with type 1 diabetes mellitus. Diabetes Metab Res Rev. 2015;31(8):803–810. PMID: 26386354. doi:10.1002/dmrr.2716
3. Huo L, Deng W, Shaw JE, et al. Factors associated with glycemic control in type 1 diabetes patients in China: a cross-sectional study. J Diabetes Investig. 2020;11(6):1575–1582. PMID: 32323910. doi:10.1111/jdi.13282
4. Holt RIG, DeVries JH, Hess-Fischl A, et al. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2021;64(12):2609–2652. PMID: 34590174. doi:10.1007/s00125-021-05568-3
5. Hawkes CP, Willi SM, Murphy KM. A structured 1-year education program for children with newly diagnosed type 1 diabetes improves early glycemic control. Pediatr Diabetes. 2019;20(4):460–467. PMID: 30932293. doi:10.1111/pedi.12849
6. Humayun MA, Jenkins E, Knott J, et al. Intensive structured education for type 1 diabetes management using BERTIE: long-term follow-up to assess impact on glycaemic control and quality of life indices. Diabetes Res Clin Pract. 2018;143:275–281. PMID: 30076871. doi:10.1016/j.diabres.2018.07.034
7. Elliott J, Jacques RM, Kruger J, et al. Substantial reductions in the number of diabetic ketoacidosis and severe hypoglycaemia episodes requiring emergency treatment lead to reduced costs after structured education in adults with Type 1 diabetes. Diabet Med. 2014;31(7):847–853. PMID: 24654672; PMCID: PMC4264891. doi:10.1111/dme.12441
8. Speight J, Amiel SA, Bradley C, et al. Long-term biomedical and psychosocial outcomes following DAFNE (Dose Adjustment For Normal Eating) structured education to promote intensive insulin therapy in adults with sub-optimally controlled Type 1 diabetes. Diabetes Res Clin Pract. 2010;89(1):22–29. PMID: 20399523. doi:10.1016/j.diabres.2010.03.017
9. Pollard DJ, Brennan A, Dixon S, et al.; REPOSE group. Cost-effectiveness of insulin pumps compared with multiple daily injections both provided with structured education for adults with type 1 diabetes: a health economic analysis of the Relative Effectiveness of Pumps over Structured Education (REPOSE) randomised controlled trial. BMJ Open. 2018;8(4):e016766. PMID: 29627802; PMCID: PMC5893943. doi:10.1136/bmjopen-2017-016766
10. Coates VE, Horigan G, Davies M, Davies MT. Exploring why young people with Type 1 diabetes decline structured education with a view to overcoming barriers. Diabet Med. 2017;34(8):1092–1099. PMID: 28430377. doi:10.1111/dme.13368
11. Scott SN, Fontana FY, Züger T, Laimer M, Stettler C. Use and perception of telemedicine in people with type 1 diabetes during the COVID-19 pandemic-results of a global survey. Endocrinol Diabetes Metab. 2020;4(1):e00180. PMID: 33532617. doi:10.1002/edm2.180
12. Zhang Y, Li X, Luo S, Liu C, Liu F, Zhou Z. Exploration of users’ perspectives and needs and design of a type 1 diabetes management mobile app: mixed-methods study. JMIR Mhealth Uhealth. 2018;6(9):e11400. PMID: 30249580; PMCID: PMC6231832. doi:10.2196/11400
13. Huang F, Wu X, Xie Y, et al. An automated structured education intervention based on a smartphone app in Chinese patients with type 1 diabetes: a protocol for a single-blinded randomized controlled trial. Trials. 2020;21(1):944. PMID: 33225982. doi:10.1186/s13063-020-04835-9
14. Faruque LI, Wiebe N, Ehteshami-Afshar A, et al.; Alberta Kidney Disease Network. Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. CMAJ. 2017;189(9):E341–E364. PMID: 27799615. doi:10.1503/cmaj.150885
15. Zhang X, Wen D, Liang J, Lei J. How the public uses social media wechat to obtain health information in China: a survey study. BMC Med Inform Decis Mak. 2017;17(Suppl 2):66. PMID: 28699549; PMCID: PMC5506568. doi:10.1186/s12911-017-0470-0
16. Xu Y, Xu L, Zhao W, et al. Effectiveness of a WeChat combined continuous flash glucose monitoring system on glycemic control in juvenile type 1 diabetes mellitus management: randomized controlled trial. Diabetes Metab Syndr Obes. 2021;14:1085–1094. PMID: 33727842; PMCID: PMC7955684. doi:10.2147/DMSO.S299070
17. Chen X, Su J, Bressington DT, Li Y, Leung SF. Perspectives of nursing students towards schizophrenia stigma: a qualitative study protocol. Int J Environ Res Public Health. 2022;19(15):9574. PMID: 35954931. doi:10.3390/ijerph19159574
18. Chun Yeh K. Effects of structured education program on Time in Range for people with type 1 diabetes. Abstract number: IDF21-0040. International Diabetes Federation Virtual Congress 2021; 2021. Available from: https://www.morressier.com/o/event/6170301693149ba0784623f2/article/617c37317c09fc044a97524c.
19. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–553. PMID: 9686693. doi:10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
20. Zhu S, Liu F, Li J, et al. Development and validation of a self-management scale of type 1 diabetes for Chinese adults. J Int Med Res. 2020;48(8):300060520947588. PMID: 32865059; PMCID: PMC7469726. doi:10.1177/0300060520947588
21. Xu J, Gu Y, Zhu M, et al. Cross-cultural adaption and reliability and validity test of the Chinese version of diabetic behavior rating scale in patients with adolescent type 1 diabetes. Chin J Diabet. 2018;26(06):463–469. Chinese.
22. Chen S, Liao F, Murphy D, Joseph S. Development and validation of a 12-item version of the Barrett-Lennard Relationship Inventory (B-L RI:mini) using item response theory. Curr Psychol. 2021. doi:10.1007/s12144-021-02348-5
23. Doherty AM, Herrmann-Werner A, Rowe A, Brown J, Weich S, Ismail K. Feasibility study of real-time online text-based CBT to support self-management for people with type 1 diabetes: the Diabetes On-line Therapy (DOT) Study. BMJ Open Diabet Res Care. 2021;9(1):e001934. PMID: 33452059; PMCID: PMC7813360. doi:10.1136/bmjdrc-2020-001934
24. Liu Z, Wang C, Yang D, et al. High engagement in mobile peer support is associated with better glycemic control in type 1 diabetes: a real-world study. J Diabetes Investig. 2022;13(11):1914–1924. PMID: 35708894; PMCID: PMC9623527. doi:10.1111/jdi.13870
25. Boscari F, Ferretto S, Uliana A, Avogaro A, Bruttomesso D. Efficacy of telemedicine for persons with type 1 diabetes during Covid19 lockdown. Nutr Diabetes. 2021;11(1):1. PMID: 33414391; PMCID: PMC7790327. doi:10.1038/s41387-020-00147-8
26. Rondags SM, de Wit M, Snoek FJ. HypoAware: development and pilot study of a brief and partly web-based psychoeducational group intervention for adults with Type 1 and insulin-treated Type 2 diabetes and problematic hypoglycaemia. Diabet Med. 2016;33(2):184–191. PMID: 26234919. doi:10.1111/dme.12876
27. Rondags SM, de Wit M, Twisk JW, Snoek FJ. Effectiveness of hypoaware, a brief partly web-based psychoeducational intervention for adults with type 1 and insulin-treated type 2 diabetes and problematic hypoglycemia: a cluster randomized controlled trial. Diabet Care. 2016;39(12):2190–2196. PMID: 27797931. doi:10.2337/dc16-1614
28. Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabet Care. 2016;39(12):2126–2140. PMID: 27879358; PMCID: PMC5127231. doi:10.2337/dc16-2053
29. Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabet Care. 2015;38(7):1372–1382. PMID: 26048904. doi:10.2337/dc15-0730
30. Grant L, Lawton J, Hopkins D, et al. Type 1 diabetes structured education: what are the core self-management behaviours? Diabet Med. 2013;30(6):724–730. PMID: 23461799. doi:10.1111/dme.12164
31. Guo HT, Wang CF, Yue T, et al. Current status of nutrient intakes and glycemic control in adults with type 1 diabetes mellitus in Guangdong Province. Chin J Diabet Mellitus. 2021;13(10):991–998.
32. Chinese Nutrition Society. Chinese Dietary Guidelines for diabetes; 2017. [EB/OL]. Available from: https://max.book118.com/html/2019/0703/6013222101002043.shtm.
33. Fu S, Li L, Deng S, Zan L, Liu Z. Effectiveness of advanced carbohydrate counting in type 1 diabetes mellitus: a systematic review and meta-analysis. Sci Rep. 2016;6:37067. PMID: 27841330; PMCID: PMC5107938. doi:10.1038/srep37067
34. Zeevi D, Korem T, Zmora N, et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163(5):1079–1094. PMID: 26590418. doi:10.1016/j.cell.2015.11.001
35. Jaacks LM, Liu W, Ji L, Mayer-Davis EJ. Type 1 diabetes stigma in China: a call to end the devaluation of individuals living with a manageable chronic disease. Diabetes Res Clin Pract. 2015;107(2):306–307. PMID: 25547225. doi:10.1016/j.diabres.2014.12.002
36. Guo J, Luo J, Yang J, et al. School-aged children with type 1 diabetes benefit more from a coping skills training program than adolescents in China: 12-month outcomes of a randomized clinical trial. Pediatr Diabetes. 2020;21(3):524–532. PMID: 31885120. doi:10.1111/pedi.12975
37. Chiang JL, Maahs DM, Garvey KC, et al. Type 1 diabetes in children and adolescents: a position statement by the American Diabetes Association. Diabet Care. 2018;41(9):2026–2044. PMID: 30093549; PMCID: PMC6105320. doi:10.2337/dci18-0023
38. Robling M, McNamara R, Bennert K, et al. The effect of the talking diabetes consulting skills intervention on glycaemic control and quality of life in children with type 1 diabetes: cluster randomised controlled trial (DEPICTED study). BMJ. 2012;344:e2359. PMID: 22539173; PMCID: PMC3339876. doi:10.1136/bmj.e2359
39. Chiang Y, Tsay P, Chen C, et al. A Delphi study on the healthcare needs of patients with type 1 diabetes during the transition from adolescence to adulthood: consensus among patients, primary caregivers, and healthcare providers. Int J Environ Res Public Health. 2021;18(13):7149. PMID: 34281086; PMCID: PMC8296953. doi:10.3390/ijerph18137149
40. Michie S, Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi:10.1186/1748-5908-6-42
41. Holmes CS, Chen R, Mackey E, Grey M, Streisand R. Randomized clinical trial of clinic-integrated, low-intensity treatment to prevent deterioration of disease care in adolescents with type 1 diabetes. Diabet Care. 2014;37(6):1535–1543. PMID: 24623027; PMCID: PMC4030089. doi:10.2337/dc13-1053
42. Weng J, Zhou Z, Guo L; T1D China Study Group, et al. Incidence of type 1 diabetes in China, 2010–13: population based study. BMJ. 360;2018:j5295. doi:10.1136/bmj.j5295
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
