Back to Journals » Lung Cancer: Targets and Therapy » Volume 12
An Observational Study to Assess the Molecular Epidemiology and Direct Medical Costs of Epidermal Growth Factor Receptor (EGFR) Mutations in Patients with Advanced EGFR Mutation-Positive Non-Small Cell Lung Cancer Treated with Afatinib in Real-World Clinical Settings in Greece
Authors Mountzios G , Lampaki S, Koliou GA, Vozikis A , Kontogiorgos I, Papantoniou P , Koufaki MI , Res E, Boutis A , Christopoulou A, Pastelli N, Grivas A, Aravantinos G , Lalla E, Oikonomopoulos G, Koumarianou A, Spyratos D, Bafaloukos Snr D, Rigakos G, Papakotoulas P, Fountzilas G, Linardou H
Received 29 April 2021
Accepted for publication 9 July 2021
Published 30 August 2021 Volume 2021:12 Pages 93—102
DOI https://doi.org/10.2147/LCTT.S318007
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sai-Hong Ignatius Ou
Giannis Mountzios,1 Sofia Lampaki,2 Georgia-Angeliki Koliou,3 Athanassios Vozikis,4 Ioannis Kontogiorgos,4 Panagiotis Papantoniou,4 Margarita-Ioanna Koufaki,4 Eleni Res,5 Anastasios Boutis,6 Athina Christopoulou,7 Nicoleta Pastelli,8 Anastasios Grivas,9 Gerasimos Aravantinos,10 Efthalia Lalla,11 Georgios Oikonomopoulos,12 Anna Koumarianou,13 Dionisios Spyratos,2 Dimitrios Bafaloukos Snr,14 Georgios Rigakos,15 Pavlos Papakotoulas,6 George Fountzilas,16– 18 Helena Linardou19
1Fourth Department of Medical Oncology and Clinical Trials Unit Henry Dunant Hospital Center, Athens, Greece; 2Pulmonary Department, Lung Cancer Oncology Unit, Aristotle University of Thessaloniki, G. Papanicolaou Hospital, Thessaloniki, Greece; 3Section of Biostatistics, Hellenic Cooperative Oncology Group, Athens, Greece; 4Laboratory of Health Economics and Management, Department of Economics, University of Piraeus, Piraeus, Greece; 5Third Department of Medical Oncology, Agii Anargiri Cancer Hospital, Athens, Greece; 6First Department of Clinical Oncology, Theagenio Hospital, Thessaloniki, Greece; 7Medical Oncology Unit, S. Andrew Hospital, Patras, Greece; 8Department of Pathology, G. Papanicolaou Hospital, Thessaloniki, Greece; 9Second Department of Internal Medicine, Agios Savvas Cancer Hospital, Athens, Greece; 10Second Department of Medical Oncology, Agii Anargiri Cancer Hospital, Athens, Greece; 11Third Department of Clinical Oncology, Theagenio Hospital, Thessaloniki, Greece; 12Second Department of Medical Oncology, Metropolitan Hospital, Piraeus, Greece; 13Hematology-Oncology Unit, Fourth Department of Internal Medicine, Attikon University Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece; 14First Department of Medical Oncology, Metropolitan Hospital, Piraeus, Greece; 15Third Department of Medical Oncology, Hygeia Hospital, Athens, Greece; 16Laboratory of Molecular Oncology, Hellenic Foundation for Cancer Research/Aristotle University of Thessaloniki, Thessaloniki, Greece; 17Aristotle University of Thessaloniki, Thessaloniki, Greece; 18Department of Medical Oncology, German Oncology Center, Limassol, Cyprus; 19Fourth Oncology Department, Metropolitan Hospital, Athens, Greece
Correspondence: Giannis Mountzios
Fourth Department of Medical Oncology and Clinical Trials Unit, Henry Dunant Hospital Center, Messoghion Av. 107, Athens, 11526, Greece
Tel +2106972000
Email [email protected]
Purpose: Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) are the preferred first-line option for patients with advanced, EGFR-mutant non-small cell lung cancer (NSCLC). Afatinib, a second-generation irreversible EGFR-TKI, has been extensively used in Greece in this setting; however, real-world data regarding molecular epidemiology and financial implications of afatinib use are lacking.
Materials and Methods: This was an observational, non-interventional, multicenter, retrospective cohort study, based on real-world data collected from the medical charts/records of patients treated with afatinib between 15/03/2015 and 25/06/2020 and were recorded on a web-based data capture system. Cox models were used to assess the prognostic significance of clinicopathological parameters with respect to clinical outcomes of interest. Cost analysis was conducted from a public third-payer perspective, and only direct medical costs reimbursed by the payer were considered.
Results: A total of 59 patients were treated with afatinib for their EGFR mutation-positive advanced NSCLC; the median age was 61 years (range: 37– 91). Performance status was zero in 61%, and brain metastases were present in 13.6%. Forty-four patients (74.6%) had a deletion in exon 19 only, while nine (15.3%) had a mutation in exon 21, 8 of them in L858R and one in L861Q. At a median follow-up of 41.8 months (95% CI 35.9– 51.4), the median PFS was 14.3 months (95% CI 12.2– 16.4), and the median OS was 29 months (95% CI 25.6– 33.4). Corresponding values for patients with deletion 19 only were 14.3 months (95% CI 11.5– 18.5) and 28.1 months (95% CI 21.1– 32.6), respectively. The mean expenditure for the treatment of each patient equals € 25,333.68; with € 21,865.06 being attributed to drug acquisition costs, € 3325.35 to monitoring costs and € 143.27 to adverse event treatment-related costs.
Conclusion: Long-term data in the real-world setting in Greece confirm activity, tolerability and cost-effectiveness of afatinib as first-line treatment of patients with advanced EGFR-mutant NSCLC.
Clinical Trial Registration: Clinicaltrials.gov NCT04640870.
Keywords: lung cancer, epidermal growth factor receptor, EGFR, afatinib, molecular epidemiology, cost-effectiveness
Introduction
In 2018, tracheal, bronchus and lung cancer was the leading cause of cancer-related deaths worldwide and in particular in Greece, a country that ranked fourth among 185 countries regarding the age-standardized incidence rate of lung cancer (40.5 per 100,000).1,2 Non-small cell lung cancer (NSCLC) is diagnosed in approximately 80–85% of lung cancer cases, with patients often carrying driver mutations in the gene encoding for epidermal growth factor receptor (EGFR).1 Advancements in the identification of molecular carcinogenesis have established EGFR tyrosine kinase inhibitors (TKIs) as the standard first-line therapy for NSCLC patients with activating EGFR mutations.3 Administration of EGFR-TKI therapy has been associated with both improved outcomes and a better quality of life compared with doublet chemotherapy, as shown in several randomized Phase III clinical trials.3–8
No general consensus for a choice among any of the currently available first- and second-generation EGFR-TKIs in the first-line setting currently exists.3 The only available data come from the randomized phase IIB LUX-Lung 7 trial, which showed similar objective response rates (ORR) and overall survival (OS),9,10 and a modest difference in progression-free survival (PFS) for the second-generation EGFR-TKI afatinib compared to the first-generation gefitinib, and the randomized phase III ARCHER 1050 trial, where the second-generation inhibitor dacomitinib was proven to be more efficacious than the first-generation EGFR-TKI, gefitinib.11,12 Nevertheless, the diverse safety profiles of first- and second-generation EGFR-TKIs contribute to the complexity of treatment decision-making in routine clinical practice.
Importantly, approximately 20% to 30% of EGFR-mutated NSCLC patients experience primary resistance to EGFR-TKIs, commonly attributed to specific genetic events, such as exon 20 insertions and the de novo T790M point mutation in the same exon.3,4 Inevitably, even among patients with an initial response, the vast majority eventually progress after approximately 9 to 14 months of treatment with an EGFR-TKI.9–12 Several mechanisms have been implicated in the development of acquired resistance to EGFR-TKIs, with the presence of the T790M mutation considered to be the most frequent,13 identified in up to 40% of patients treated with first-generation or second-generation EGFR-TKIs.14 For patients with systemic progression and a T790M mutation confirmed either with tissue biopsy or circulating-tumor DNA (ctDNA) plasma testing (and tissue re-biopsy if plasma test is negative), administration of the third-generation EGFR-TKI, osimertinib, is the treatment of choice, while for patients who are not candidates for rebiopsy or for whom a T790M mutation is not detected, the current European Society for Medical Oncology guidelines recommend switching to platinum-based chemotherapy.3
The aforementioned underscore the need for real-world evidence regarding the treatment paradigms, the use of second-generation EGFR inhibitors, namely afatinib, the molecular epidemiology, frequencies of acquired resistance mechanisms and co-occurring mutations, as well as clinical outcomes in patients with advanced or metastatic EGFR-mutant NSCLC in the frontline setting. Scarce such evidence is available in routine care settings in Greece.
Materials and Methods
Study Design and Setting
This was an observational, non-interventional, single-country, multicenter, retrospective cohort study, based on real-world data collection, of patients with locally advanced or metastatic EGFR mutation-positive NSCLC who had been treated with afatinib at any line. The study was carried out by hospital-based oncologists/pulmonologists specializing in lung cancer under real-world conditions of daily clinical practice. Investigators were selected through a documented and structured feasibility process which took into consideration the physicians’ qualifications, previous participation and experience in other clinical studies, recruitment potential, consistency and retention capability. In addition, in order to represent variations in current real-world patterns of care, research sites were recruited from various geographic regions in Greece, taking also into consideration the regional setting and type of healthcare site/institution (public or private specialized oncology or pulmonology clinic, academic or general hospital environment).
The study mainly involved collecting primary data, obtained retrospectively from the medical charts/records of patients treated with afatinib between 15/03/2015 and 25/06/2020. Data were recorded on a web-based data capture system, which adheres to all applicable data protection regulations and requirements concerning electronic records and database validation.
The study was designed and conducted in compliance with all applicable local laws and regulations, the Good Pharmacoepidemiology Practices of the International Society for Pharmacoepidemiology and the ethical principles laid down in the Declaration of Helsinki. The study was approved by the Institutional Review Board of Henry Dunant Hospital (113/3-11-2020). All patients had provided written informed consent.
Statistical Considerations
Descriptive statistics were used to summarize patient and tumor characteristics. Categorical data, including frequencies and percentages, were summarized by contingency tables, while continuously scaled measures were described by the median and range values.
The primary endpoint of the study was progression-free survival, defined as the time from treatment initiation with afatinib as a first or second-line treatment until the first documented disease progression, death from any cause or last follow-up, whichever occurred first (PFS1). Secondary endpoints included overall survival (OS), defined as the time from treatment initiation with afatinib until death from any cause or last follow-up, second progression-free survival (PFS2), defined as the time interval from the initiation of next treatment following discontinuation of afatinib to the date of progression, death or last contact, and assessment of the safety profile of afatinib. Survival distributions were estimated using the Kaplan-Meier method. PFS1 was assessed among patients treated with first or second-line afatinib, while OS was examined in the entire cohort. Cox models were used to assess the prognostic significance of clinicopathological parameters of interest with respect to PFS1 and OS. The SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) and R studio 3.5.0 were used for data manipulation and statistical analysis.
Cost Analysis
The cost analysis was conducted from a public third-payer (National Organization for Healthcare Services Provision (EOPYY)) perspective, and only direct medical costs reimbursed by the payer were considered. In particular, only drug acquisition costs, monitoring costs and adverse event treatment-related costs were evaluated. All costs refer to the year 2021 (€).
Drug acquisition costs per 28-day treatment cycle were calculated, taking into account the average dose per cycle of the patients included in the cohort and the price reimbursed from EOPYY. As afatinib is exclusively provided by a hospital or EOPYY pharmacies, its official hospital price, minus the compulsory hospital rebate (5%) was considered the price reimbursed by the public payer, which is equal across all different strengths of afatinib.15 The calculation of the hospital price was in line with the pricing methodology legislated by the Ministry of Health (MoH) and the latest Drug Price Bulletin issued by the MoH (December 2020).15–17
Monitoring costs were estimated based on the utilization of monitoring services by the cohort both prior treatment initiation and during treatment with afatinib. The unit costs per monitoring service were obtained from the national tariff of medical practices published by EOPYY.18 Moreover, adverse event treatment-related costs were only considered for Grade 3–4 adverse events, with their reimbursement costs being obtained from the corresponding Diagnosis Related Group (DRG) tariffs issued by the MoH.19
Results
Clinicopathological Characteristics
From 15/03/2015 through 25/06/2020, a total of 59 patients were treated with afatinib for their EGFR mutation-positive advanced lung cancer. More patients were of younger age (<65 years, 59.3%), with PS 0 (61.0%) and no brain metastases (86.4%) at the time of afatinib administration. The median age was 61 years (range 37–91). Patient and tumor characteristics are displayed in Table 1.
 |
Table 1 Patient and Tumor Characteristics |
Afatinib was administered as first-line treatment in 86.4% of the study cohort (n=51 patients), second-line treatment in five patients (8.5%) and as third-line and beyond in three patients (5.1%). Most patients initially received afatinib at a dose of 40 mg/day (53 patients; 89.8%), while in five patients (8.5%) the drug was administered at a dose of 30 mg/day in the first cycle of treatment and one patient received 4 cycles of afatinib at a dose of 20 mg/day per cycle.
Molecular Epidemiology
Forty-four patients (74.6%) had a deletion in exon 19 only, while nine (15.3%) had mutation in exon 21; 8 of them in L858R and one in L861Q. In addition, one patient carried EGFR co-mutations in G719X in exon 18 and in L861Q in exon 21. Two additional patients harbored a deletion in exon 19 along with a T790M mutation in exon 20, respectively. In three patients, the mutations were observed in exon 20 and 21; two of them had mutation in T790M and L858R and one in R776S and L858R, respectively (Figure 1).
 |
Figure 1 Type of EGFR mutation detected. |
PFS1
At a median follow-up of 41.8 months (95% CI 35.9–51.4), 48 PFS1 events had been reported among patients who received afatinib as a first- or second-line treatment (85.7%) and 40 patients (67.8%) had died overall. The median PFS1 was 14.3 months (95% CI 12.2–16.4) and the median OS was 29 months (95% CI 25.6–33.4) (Figure 2). The median PFS1 and OS for patients with deletion 19 only was 14.3 months (95% CI 11.5–18.5) and 28.1 months (95% CI 21.1–32.6), respectively. All seven patients with uncommon mutations died of their disease. Out of eight patients with L858R mutations, seven (87.5%) had experienced a disease progression and three had died (37.5%) at the time of the analysis. The Kaplan-Meier curves with respect to PFS1 and OS by EGFR mutation type are presented in Figure 3A and B, respectively.
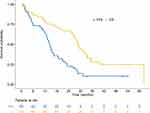 |
Figure 2 Kaplan-Meier curves with respect to PFS1 and OS. |
 |
Figure 3 Kaplan-Meier curves based on the type of EGFR mutation with respect to (A) PFS1 and (B) OS. |
The patient with an L861Q EGFR mutation only was a 73-year-old male who progressed after 6 months of afatinib treatment and died 6 months later. Additionally, a 44-year-old female patient carrying EGFR mutation in G719X and L861Q progressed within 4 months upon administration of afatinib and died 10 months after progressive disease documentation. Both patients with a deletion 19 and a T790M mutation progressed in 12.9- and 9.4-months post afatinib initiation, respectively. Of them, the first patient died 19.7 months and the other one 9.4 months since treatment initiation. Performance status was the only parameter that showed prognostic significance for OS with patients with PS 1–3 being at higher risk for death as compared to those with PS 0 (HR=2.23, 95% CI 1.17–4.24, Wald’s p=0.015), while no significance was reached in terms of PFS1 (p=0.96). The rest of the examined clinicopathological parameters were not found to be prognostic for either PFS1 or OS (data not shown). At the cut-off date for the analysis (November 2020), 7 patients (11.9%) were still on active treatment with afatinib. All of them had deletion in exon 19 only. The median time to treatment discontinuation was 14.1 months (95% CI 10.3–16.4).
Post-Afatinib Treatment and PFS2
Out of the 46 patients with a documented disease progression after afatinib administration, 37 (80.4%) received other treatments including immunotherapy alone (n=3; 8.1%), TKIs only (n=18; 48.6%), TKI with immunotherapy (n=1; 2.7%), combination chemotherapy (n=3; 8.1%), chemotherapy alone (n=2; 5.4%), chemotherapy combined with immunotherapy (n=6; 16.2%), and chemotherapy in combination with immunotherapy and anti-VEGF (n=4; 10.8%). Of note, one patient with R776S+L858R EGFR mutation received afatinib beyond disease progression. Details of subsequent treatment after failure of afatinib therapy per patient are presented in Supplementary Table 1. Thirty-five of them (94.6%) had received afatinib as a first-line treatment, while the drug was administered as a second-line therapy in the remaining two patients. Upon failure of afatinib as a second-line therapy, one patient carrying a deletion 19 and T790M EGFR mutation was treated with osimertinib and one with a G719X and L861Q EGFR mutation received pemetrexed and carboplatin. The median time to the next treatment was 17 days upon the last cycle of afatinib. Thirty-three of the 37 patients (89.2%) experienced a second progression and the median PFS2 was 6.3 months (95% CI 3.0–9.3).
Adverse Events
Overall, 42 patients (71.2%) experienced at least one adverse event during afatinib treatment and 7 (11.9%) had grade 3 or 4 events. The incidence of all adverse events during afatinib treatment is depicted in Table 2. Two grade 4 events of rash and clinic infection were reported in one patient who discontinued afatinib due to soft tissue infection. Three additional patients discontinued treatment with afatinib due to non-fatal toxicity, while no fatal adverse events were reported throughout treatment. The most commonly reported adverse events were diarrhea (29 patients; 49.2%) followed by rash (24 patients; 40.7%) and were mostly of grade 1 or 2.
 |
Table 2 Incidence of Grade 1–4 Toxicities Throughout Afatinib Treatment |
Cost Analysis
Drug acquisition costs per 28-day cycle of treatment are equal to €1385.15 regardless of the afatinib strength administered to the cohort (Table 3).
 |
Table 3 Drug Acquisition Costs |
In addition, costs associated with monitoring services utilized prior treatment initiation equal €453.16, while after initiation of afatinib monitoring costs equal €181.95 per 28-day cycle (Table 4).
 |
Table 4 Monitoring Costs |
Lastly, adverse event treatment-related cost per patient was estimated to equal €143.27 per 28-day cycle (Table 5).
 |
Table 5 Adverse Event Treatment-Related Costs |
Moreover, taking into consideration that each member of the cohort remained on treatment with afatinib for an average of 15.79 treatment cycles, the mean expenditure for EOPYY for the treatment of each patient with afatinib equals €25,333.68; with €21,865.06 being attributed to drug acquisition costs, €3325.35 to monitoring costs and €143.27 to adverse event treatment-related costs (Table 6).
 |
Table 6 Mean Expenditure for EOPYY per Patient Treated with Afatinib |
Discussion
The current study was the first attempt to record the molecular epidemiology of patients treated with afatinib for advanced, EGFR-mutated NSCLC in Greece. We found that real-life clinical practice treatment patterns reflected the outcomes of larger randomized trials that led to its approval. Afatinib was mainly used as first-line treatment, based on its superior efficacy as compared to the first-generation inhibitors and its presumed activity in rare mutations.14,20 The majority of patients harbored deletion 19 mutation, which reflects the reported higher efficacy of afatinib in this specific mutation type.21,22 Tumors with exon 19 deletion are known to carry a better prognosis, as compared to other mutations and especially the L858R point mutation in exon 21.14,20–22 Regarding afatinib, combined analysis of the LUX-LUNG 3 and LUX-LUNG 6 phase III trials has shown that in the subgroup of patients whose tumors harbored an exon 19 deletion, treatment with afatinib was associated not only with a PFS benefit, but also with a substantial and clinically significant survival benefit, as compared to first-generation inhibitors.6,7 This notion is presumed to have affected the clinical practice patterns of oncologists and pneumonologists in Greece who were more likely to prescribe afatinib for patients with exon 19 deletion.
Another important aspect of afatinib administration is its use in the uncommon EGFR mutations, based on preclinical data suggesting that it is active against a broad spectrum of uncommon mutations, especially in eons 18 and 29, due to its unique action as a pan-EGFR inhibitor.23–26 These properties lead to its approval by FDA for the treatment of patients with uncommon mutations, where it exerts higher activity than erlotinib or gefitinib, albeit some uncommon mutations are notoriously refractive to treatment, even with afatinib and carry a poor prognosis.24,26,27 These results were confirmed in our cohort, where patients with uncommon mutations or with co-existence of a common and uncommon mutation had poorer clinical outcomes with afatinib treatment, as compared to the Deletion 19 subgroup. A special reference should be made to the T790M resistance mutation, which is notoriously refractory to all first-generation inhibitors, including erlotinib and gefitinib, and is held responsible for primary resistance to these drugs, at least in a subset of patients.27,28 Afatinib has been shown to be active against the T790M mutation in vitro, but this activity has not been consistently translated into substantial clinical benefit in clinical trials.26,28 This observation was consistent with our findings, with mixed responses to afatinib in patients with tumors harboring the T790M mutation, ranging from 9 to 17 months, in terms of overall survival. The advent of the third-generation EGFR-TKI osimertinib with a documented activity against T790M has completed transformed the landscape of the treatment of EGFR-mutant NSCLC, and currently osimertinib dominates the first-line treatment in this setting, due to its high activity and favorable toxicity.29,30 Nevertheless, it should be noted that osimertinib was not available in Greece for the largest period during the accrual period of the study. Notably, a sequential strategy with afatinib as first-line treatment, followed by osimertinib at the time of development of the exon 20 T790M-resistance mutation has been shown to be both feasible and efficient in real-world clinical settings.33 This concept is further facilitated by the use of liquid biopsy to identify the T790M mutation in the blood with digital droplet PCR.34
Afatinib is considered to be more toxic than first-generation inhibitors, especially in terms of diarrhea, due to its mechanism of action, which blocks the action of all proteins of the HER family of receptors and not just EGFR.25–27 In our cohort, we confirmed that acmoid rash and diarrhea are the two main concerns with afatinib safety profile, but, similar to the clinical trials, in the vast majority of cases adverse events were manageable and did not lead to discontinuation of the drug.
Finally, the cost analysis conducted demonstrated that the mean cost associated with afatinib treatment reimbursed from EOPYY equaled €25,333.68 per patient, with costs related to drug acquisition forming the primary cost driver. The findings of the analysis conducted are consistent with two other published economic evaluation studies conducted in France and China.31,32 Both studies assessed the cost-effectiveness of afatinib versus comparator treatments and concluded that the major cost component associated with afatinib treatment is drug acquisition costs followed by the monitoring and the adverse event treatment-related costs.31,32
Acknowledgments
The authors would like to thank Maria Moschoni for data coordination and the data managers of the participating centers for data collection.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was supported by a Hellenic Cooperative Oncology Group internal research grant (HE_TRANS_NSCLC).
Disclosure
Dr Giannis Mountzios report personal fees from Roche Hellas, personal fees from BMS Greece, personal fees from MSD Greece, personal fees from AstraZeneca Greece, personal fees from Pfizer Greece, personal fees from Takeda Greece, personal fees from Boehringer Greece, outside the submitted work; Professor Athanassios Vozikis report personal fees from BMS, personal fees from Roche, personal fees from TAKEDA, personal fees from ANGELINI, outside the submitted work; Dr Anastasios Grivas report personal fees, non-financial support from Bristol-Myers Squibb, personal fees, non-financial support from LEO Pharma, personal fees, non-financial support from Novartis Greece, personal fees, non-financial support from AstraZeneca, personal fees, non-financial support from Amgen, personal fees, non-financial support from Pierre Fabre, personal fees, non-financial support from Boehringer Ingelheim, personal fees, non-financial support from Roche, outside the submitted work; Dr Georgios Rigakos report grants from pfizer, grants from Merck, grants from roche, outside the submitted work; Professor George Fountzilas report personal fees from Pfizer, personal fees from Novartis, personal fees from Roche, personal fees from AstraZeneca, outside the submitted work; and Stock ownership: Genprex, Daiichi Sankyo, ARIAD, RFL Holdings, FORMYCON. Dr Helena Linardou report personal fees from Roche, personal fees from Astra Zeneca, personal fees from Novartis, personal fees from MSD, personal fees from BMS, personal fees from Merck, personal fees from Pfizer, personal fees from Amgen, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. International Agency for Research on Cancer. Estimated number of new cases in 2018. Global Cancer Observatory: Cancer Today. 2020.
2. Lung cancer statistics. World Cancer Research Fund International. Available from: https://www.wcrf.org/dietandcancer/cancer-trends/lung-cancer-statistics.
3. Planchard D, Popat S, Kerr K, et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl4):iv192–iv237.
4. Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362(25):2380–2388.
5. Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised Phase 3 trial. Lancet Oncol. 2010;11(2):121–128.
6. Inoue A, Kobayashi K, Maemondo M, et al. Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naive non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Ann Oncol. 2013;24(1):54–59.
7. Wu YL, Zhou C, Hu CP, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(2):213–222.
8. Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–246.
9. Park K, Tan EH, O’Byrne K, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-Lung 7): a Phase 2B, open-label, randomised controlled trial. Lancet Oncol. 2016;17(5):577–589.
10. Paz-Ares L, Tan EH, O’Byrne K, et al. Afatinib versus gefitinib in patients with EGFR mutation-positive advanced non-small-cell lung cancer: overall survival data from the phase IIb LUX-Lung 7 trial. Ann Oncol. 2017;28(2):270–277.
11. Wu YL, Cheng Y, Zhou X, et al. Dacomitinib versus gefitinib as first-line treatment for patients with EGFR-mutation-positive non-small-cell lung cancer (ARCHER 1050): a randomised, open-label, phase 3 trial. Lancet Oncol. 2017;18(11):1454–1466.
12. Mok TS, Cheng Y, Zhou X, et al. Improvement in overall survival in a randomized study that compared dacomitinib with gefitinib in patients with advanced non-small-cell lung cancer and EGFR-activating mutations. J Clin Oncol. 2018;36(22):2244–2250.
13. Wang J, Wang B, Chu H, Yao Y. Intrinsic resistance to EGFR tyrosine kinase inhibitors in advanced non-small-cell lung cancer with activating EGFR mutations. Onco Targets Ther. 2016;9:3711–3726.
14. Gainor JF, Shaw AT. Emerging paradigms in the development of resistance to tyrosine kinase inhibitors in lung cancer. J Clin Oncol. 2013;31(31):3987–3996.
15. Health M Bulletin of revised prices for human medicines. Available from: https://www.moh.gov.gr/articles/times-farmakwn/deltia-timwn/8181-tropopoihsh-ths-d3-a-81607-17-12-2020-apofashs-me-thema-deltio-anathewrhmenwn-timwn-farmakwn-anthrwpinhs-xrhshs-dekembrioy-20202020.
16. Drug pricing provision. Tax heaven. Available from: https://www.taxheaven.gr/circulars/307712019.
17. Legislative Affairs. Government Gazette; 2017.
18. (EOPYY) NOfHSP. Categories of Medical Practices. 2021. Available from: https://eopyyfiles.blob.core.windows.net/eopyysite/ServiceCategories/038dc470-fbe3-409b-bdd7-7efb3b37f984.pdf2021.
19. Legislative Affairs. Government Gazette. Vol 946/Β/27.03.2012; 2012.
20. Kim HR, Cho BC, Shim HS, et al. Prediction for response duration to epidermal growth factor receptor-tyrosine kinase inhibitors in EGFR mutated never smoker lung adenocarcinoma. Lung Cancer. 2014;83(3):374–382.
21. Levy BP, Rao P, Becker DJ, Becker K. Attacking a moving target: understanding resistance and managing progression in EGFR-positive lung cancer patients treated with tyrosine kinase inhibitors. Oncology (Williston Park). 2016;30(7):601–612.
22. Cortot AB, Janne PA. Molecular mechanisms of resistance in epidermal growth factor receptor-mutant lung adenocarcinomas. Eur Respir Rev. 2014;23(133):356–366.
23. Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19(8):2240–2247.
24. Blakely CM, Bivona TG. Resiliency of lung cancers to EGFR inhibitor treatment unveiled, offering opportunities to divide and conquer EGFR inhibitor resistance. Cancer Discov. 2012;2(10):872–875.
25. Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3(75):75ra26.
26. Wu SG, Liu YN, Tsai MF, et al. The mechanism of acquired resistance to irreversible EGFR tyrosine kinase inhibitor-afatinib in lung adenocarcinoma patients. Oncotarget. 2016;7(11):12404–12413.
27. Takeda M, Nakagawa K. First- and second-generation EGFR-TKIs are all replaced to osimertinib in chemo-naive egfr mutation-positive non-small cell lung cancer? Int J Mol Sci. 2019;20:1.
28. Oxnard GR, Arcila ME, Sima CS, et al. Acquired resistance to EGFR tyrosine kinase inhibitors in EGFR-mutant lung cancer: distinct natural history of patients with tumors harboring the T790M mutation. Clin Cancer Res. 2011;17(6):1616–1622.
29. Jänne PA, Yang JC, Kim DW, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372(18):1689–1699.
30. Goss G, Tsai CM, Shepherd FA, et al. Osimertinib for pretreated EGFR Thr790Met-positive advanced non-small-cell lung cancer (AURA2): a multicentre, open-label, single-arm, phase 2 study. Lancet Oncol. 2016;17(12):1643–1652.
31. Chouaid C, Luciani L, LeLay K, et al. Cost-effectiveness analysis of afatinib versus gefitinib for first-line treatment of advanced EGFR-mutated advanced non-small cell lung cancers. J Thorac Oncol. 2017;12(10):1496–1502.
32. Gu X, Zhang Q, Chu YB, et al. Cost-effectiveness of afatinib, gefitinib, erlotinib and pemetrexed-based chemotherapy as first-line treatments for advanced non-small cell lung cancer in China. Lung Cancer. 2019;127:84–89.
33. Hochmair MJ, Morabito A, Hao D, et al. Sequential afatinib and osimertinib in patients with EGFR mutation-positive non-small-cell lung cancer: final analysis of the GioTag study. Future Oncol. 2020;16(34):2799–2808.
34. Hochmair MJ, Buder A, Schwab S, et al. Liquid-biopsy-based identification of EGFR T790M mutation-mediated resistance to afatinib treatment in patients with advanced EGFR mutation-positive NSCLC, and subsequent response to osimertinib. Target Oncol. 2019;14(1):75–83.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
