Back to Journals » Patient Preference and Adherence » Volume 16
An Observational Cohort Study to Evaluate the Impact of a Tailored Medicines Optimisation Service on Medication Use, Accident and Emergency Department Visits, and Admissions Among Patients Identified with Medication Support Needs in Secondary Care
Authors Harrap N , Wells J , Howes K, Kayyali R
Received 18 June 2022
Accepted for publication 12 October 2022
Published 28 October 2022 Volume 2022:16 Pages 2947—2961
DOI https://doi.org/10.2147/PPA.S376686
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Nicola Harrap,1 Joshua Wells,1 Katherine Howes,2 Reem Kayyali1
1Department of Pharmacy, Kingston University, Kingston, KT1 2EE, UK; 2Lewisham Integrated Medicines Optimisation Service, Pharmacy Department, Lewisham & Greenwich NHS Trust, London, SE13 6LH, UK
Correspondence: Reem Kayyali, Department of Pharmacy, Kingston University, Penrhyn Road, Kingston, KT1 2EE, UK, Tel/Fax +44 208 417 2561, Email [email protected]
Purpose: Quantifying the impact of pharmacy interventions, such as tailored medicines optimisation, can be challenging owing to the sometimes-indirect nature of their effect on patient outcomes such A&E (Accident & Emergency) attendance, hospital admission and length of stay. This study aimed to assess the impact of the, Lewisham Integrated Medicines Optimisation Service (LIMOS) on medicines self-management, A&E attendances and hospital admissions.
Patients and Methods: The study was conducted as a retrospective and prospective observational evaluation of patients referred to LIMOS at University Hospital Lewisham between April and September 2016. Only patients with an appropriate referral that received a LIMOS intervention within the study period were considered eligible. The main outcomes examined pre- and post-LIMOS included medicines self-management, A&E attendance, number of admissions, as well as length of stay.
Results: Data were collected for a total of 193 patients. Over half (56.4%, n = 109) identified as female with a mean age of 78 years at the time of referral. The number of hospital admissions decreased significantly post-LIMOS (− 0.36 ± 1.87, 95% CI − 0.63– 0.10). Furthermore, the mean reduction in length of stay was significant and decreased by over a week (19.58 vs 11.09 days post-LIMOS, − 7.67 ± 48.57, 95% CI − 14.57–− 0.78). There was a significant increase in A&E visits observed post-intervention (0.78 ± 1.93, 95% CI 0.50– 1.06); however, the majority (63%, n =165/261) occurred over 90 days post-intervention. There was a significant reduction in the number of patients self-managing medication post-LIMOS, with the number of patients receiving additional support with their medication increasing (− 0.38 ± 0.50, 95% CI − 0.45–− 0.31). LIMOS, therefore, successfully identified patients who were unable to manage their medicines.
Conclusion: Specialist pharmacy interventions, which include support with medicines management, have a positive impact on admission avoidance and length of hospital stay.
Keywords: medicines optimisation, admission, medication adherence, social care, polypharmacy
Introduction
Medicines are the most widely used intervention in healthcare, yet they are associated with several issues such as poor adherence and a lack of optimisation that can often contribute to inappropriate polypharmacy.1–5 Patients with chronic diseases have been shown to have poor medication adherence, ranging from 10% to 75%.6–8 These findings are particularly true for older patients and those affected by multimorbidity, common presentations seen not only in Accident & Emergency (A&E) departments across the UK, but more widely in healthcare settings across the globe.9,10 A 2015 review by Prince et al9 attributes 23.1% of global disease burden to individuals aged 60 years and over, with chronic non-communicable conditions being the greatest contributor. The impact of this burden is further compounded by widening disparities in socio-economic status (SES), which most notably affects individuals belonging to lower SES groups who are exposed to both poorer health outcomes and worsening health-related quality of life.11,12
Pharmacological therapy has a role in supporting patients with chronic comorbidities and age-related health issues. However, over, or inappropriate prescribing of medicines can also play a part in worsening mortality, more frequent and early hospital readmission, as well as higher rates of adverse effects and drug–drug interactions.13–15 Interventions to tackle medicines-related issues are essential, yet the approach to do so becomes increasingly complex when considering the current landscape of social care provision. Crawford et al16 highlight that per person spending on social care for people over the age of 65 has fallen by £375 between 2010 and 2016. The knock-on effect is felt across the entire secondary care pathway, with both increased attendances to A&E as well as delays to discharge.16,17 Moreover, for each £100 cut from social care spending, the cost to provide A&E care increases by £3 per resident. This is of particular concern for patients that are housebound or receiving care, who are more prone to early hospital readmission.18,19 Furthermore, these patients often experience loneliness and isolation, two factors that exacerbate significant risks such as falls and declining cognitive function, both of which may contribute to hospitalisation and multimorbidity if improperly managed.20,21
The interdependency between hospital and social care is evident, hence interventions that look to tackle individual patient issues may fail to be sustainable. Therefore, integrated approaches that can address the entire care pathway may be better suited to support the most vulnerable patients. Medicines optimisation (MO) interventions can play a pivotal role in improving the safety and quality of care that patients receive in secondary,22 community,23 and care home24 settings. Furthermore, MO provides strong health economic value through the reduction of medication related harm and waste, estimated to cost the UK National Health Service £98m25 and £300m26 respectively each year. The emphasis on a “systems approach” MO service is clear from a recent 2021 NHS Clinical Commissioners report by Rule and Jones27 that highlights how essential these interventions will be with the introduction of Integrated Care Systems (ICS) in England. These systems aim to support more collaboration between health and care services with a focus on improving health outcomes and financial sustainability across established cross-organisation networks.
One such example of an embedded across-system intervention is the Lewisham Integrated Medicines Optimisation Service (LIMOS). The service provides a formal pathway for the referral of patients with medicines-related problems identified in primary and secondary care for management by a specialist pharmacy team. The team, comprising of specialist pharmacists and pharmacy technicians, assesses, supports, and follows referrals with the aim of providing an integrated and deliverable pharmaceutical care plan. The aim is to enable patients, particularly those who are at high risk of admission, to get the most from their medicines whilst remaining independent and safe. The service is conducted in hospital, patients’ homes and in care homes.
There are several alternative examples of clinical pharmacy interventions and services that have demonstrated a reduction in the length of stay in hospital, hospital readmissions, and A&E attendances, however none have done so using a validated intervention tool.28–30 Thus, the impact of clinical pharmacy interventions remains difficult to quantify and any outcome in healthcare that may occur due to a pharmacist’s intervention may not be directly attributed to that action. Therefore, the key objective of this study was to undertake an external evaluation of the LIMOS service.
As part of the evaluation process, the study aimed to describe the population who received care by the LIMOS team, their risk of admission and potential differences between risk groups, the types of contribution made by the LIMOS team and the impact of LIMOS pre- and post-intervention on primary outcomes such as medicines self-management, A&E attendances, and admissions at University Hospital Lewisham (UHL). Additionally, the study sought to explore the routes and types of LIMOS referrals, as well as evaluate changes in social care need and medication support among patients referred to LIMOS.
Materials and Methods
Study Design
The study followed an observational design in line with the STROBE Cohort guidelines and is reported as such.31 Patients referred to the LIMOS service between 01/04/2016 to 30/09/2016 that received an intervention were retrospectively and prospectively monitored for a period of 12 months pre- and post-intervention. Ethics approval was obtained from Kingston University Delegated Research Ethics Committee (Ref: 1415/035) and approved by the R&D department by UHL as a service evaluation. Data from patients who had previously accessed the LIMOS service were assessed retrospectively via the secure internal trust database. Hence, patients were not actively involved in a research process and therefore informed consent was not required and waived by the ethics committee and R&D department for UHL. All data were handled in accordance with UHL’s data protection and patient confidentiality policies.
Sample Size and Characteristics
The LIMOS service can be accessed by any patient registered with a Lewisham GP where medicines support is required and one of the referral criteria are met. Only patients with valid referrals to LIMOS were considered for data extraction. Referral criteria included issues pertaining to the safe and effective use of medicines such as: history of a mental health issue, medicines-related admission/readmission, initial care home admission review, post-discharge care home review, medication adherence support eg, “blister pack” (a monitored dosage system (MDS)) initiation, support with adherence and review of level of medication support as a package of care (POC). More specifically, referral for a POC review would relate to a change in health status that may result in either an increased or decreased need for support with medications administration at home via a POC. Levels of medicines support were quantified as 1, 2 and 3 which indicated assistance with medicines (eg, reminders/ordering), administration support (eg, from a care worker) or specialist administration support (eg, insulin injection) respectively.
Patient details were extracted for all patients discharged from the LIMOS service over a six-month period in 2016 (01/04/2016 to 30/09/2016). The Raosoft32 sample size calculator was used to determine the size of a representative sample from this period. A total of 376 patients were discharged from the LIMOS service in the six-month period (01/04/2016 to 30/09/2016). A final minimum sample size of 191 patients was calculated (margin of error 5%; confidence level 95%).
Any patient discharged from the LIMOS service between 01/04/2016 and 30/09/2016 that received an intervention were considered eligible for inclusion in the study. Prospective monitoring continued for 12-months post-recruitment, hence the final date for collection of data was 30/09/2017.
Internal Validation of LIMOS
LIMOS has specific outcomes through which impact measurement can be derived. These include, in part, improved medication adherence (addressing both intentional and non-intentional adherence issues), reduction of hospital admissions/readmissions related to medicines, reduction in medicine waste, cost associated with number of medicines stopped and improved patient experience. To provide a quantitative estimate for the reduction of A&E and hospital admissions, LIMOS adapted the National Patient Safety Agency (NPSA) risk matrix,33 a tool for risk managers that provides an outcome measure of associated risks (Table 1). The adapted tool scores the impact of an intervention in the context of risk of A&E attendance and hospital admission if the holistic intervention had not taken place.
 |
Table 1 Adapted LIMOS Risk Matrix Tool |
The LIMOS tool scores the risk by considering the likelihood and consequence of a medicines–related problem to occur. This together with more concrete and easier to measure interventions, such as the value of medicines stopped and the number of social care interventions avoided, have allowed the service to internally demonstrate significant financial value with £2 saved across the health and social care economy for each £1 spent.
Internal validation of the LIMOS tool was conducted by a panel of specialists drawn from both primary and secondary care who rated the interventions performed by the service.34 An audit of scores by the panel showed similarity of scores per case. The LIMOS team internally scored the impact of their intervention and presented a random sample of cases to the panel for scoring. An analysis conducted in July 2015 during the first year of the evaluation of the service showed an 88% similarity in risk rating scores. There were some instances where the panel scored higher than the assessment made by the LIMOS pharmacist. The annual service report for 2015/16 by LIMOS revealed that of 706 cases seen, 228 were deemed to be either high or very high risk of admission if intervention had not taken place. This equated to a potential cost avoidance value of £118K.
Research Instruments
For retrospective data collection, a tool was designed to record patient details including their age, gender, ethnicity, patient group stratified by risk, reason for referral, date and source of referral, LIMOS discharge date, numbers of prescribed medicines, A&E admission dates and reasons and A&E attendance dates and reasons for UHL admission. Furthermore, LIMOS service details that were collected included: medicines management on initial assessment and at discharge, types of medicines-related problems identified, actions taken by the LIMOS team and the numbers of phone calls and appointments conducted while on the service. Medication adherence issues were classified as either intentional or unintentional upon discussion with a patient and/or a care provider. For example, quantitative reporting of intentional non-adherence may include patients who decided to stop their medicines due to side-effects, whereas unintentional non-adherence may be the result of forgetfulness. The risk of admission score was captured using the adapted LIMOS NPSA matrix that was also collated within the retrospective data collection tool. Data were derived from the UHL records system (UHLiCARE) and the primary care record (EMIS).
A prospective data collection tool was designed to collect data from UHLiCARE only. This included the number and timing of A&E attendances and hospital admissions for 12 months following the LIMOS intervention, providing data for pre- and post-intervention analyses.
Data Analysis
Data obtained from EMIS and UHLiCARE were entered into Microsoft Excel prior to extraction and further analysis in SPSS. Descriptive statistics were used to analyse socio-demographic and cohort level data in addition to univariate analysis to examine between-group differences. A p-value of <0.05 was considered significant. For categorical data, such as risk-score, a Chi-Square analysis was performed followed by additional post-hoc testing using Bonferroni correction to identify significant relationships between variables prior to an Odds Ratio (OR) estimation. Paired sample t-tests were conducted to provide mean differences in outcomes pre- and post-LIMOS. Data were reported at 95% Confidence Intervals (CI) in addition to Cohen’s d for effect size estimation. Analyses were conducted at a total cohort level prior to stratification by admission risk score.
Results
Socio-Demographic Characteristics and Admission Risk
Data were collected for a total of 193 patients of whom 109 identified as female (56.4%). The mean age at referral was 78 years (range 30–101). Ethnicity data were recorded for 86% (n = 165) of the participants with the largest cohort recorded as White British (n =71/165, 36.8%). Most of the sample (78%, n = 150) were assigned low and medium admission risk scores using the LIMOS tool with the remaining sample assigned high risk (n = 43). Table 2 summarises the patients’ characteristics by allocated admission risk score.
 |
Table 2 Patients’ Characteristics by Allocated Admission Risk Score |
Socio-Clinical Analyses
Between group analyses for admission risk scores were conducted for socio-clinical data pertaining to patient age, gender, ethnicity, duration on the LIMOS service, number of medicines, and number of comorbidities (Table 2). The mean time spent on the service for the total sample with available duration data (99.5%, n = 192/193) was 98.3 ± 71.2 days (Table 2). Fewer patients had a full data set for their medication history (95.3%, n = 184); however, the mean number of prescribed medicines for the cohort was 8.1 ± 3.8. Complete comorbidity data were lacking; full reports were available for only 69.4% (n = 134) of the cohort with the mean number of comorbidities being 7.9 ± 3.7. As admission risk score increased, so did the mean number of medicines, comorbidities, and duration on the LIMOS service, however these were all non-significant (p>0.05). Furthermore, univariate analysis of demographic factors by risk score did not identify any significant difference (p>0.05) between groups based on age, gender, or ethnicity.
Referrals to LIMOS
Roughly a quarter (24.4%, n = 47/193) of all the patients within the study cohort were first seen in the hospital setting, whilst around 74.6% (n = 144) of referrals were first seen in primary care. Of those who were considered a high-risk of admission, 32.6% (n = 14/43) were first seen in hospital compared with 16% (n = 12/75) for those considered medium-risk and 28% (n = 21/75) of those considered a low-risk. Referrals from GPs and social care teams comprised the largest route of referrals across all risk groups (Figure 1). Patients can have more than one reason for referral. Figure 2 gives details of the total cohort stratified by risk-group and referral criteria.
 |
Figure 1 Source of referral to LIMOS. |
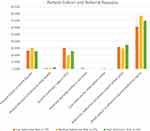 |
Figure 2 Patient cohort and referral criteria. |
Adherence support with a medication regimen was the most common reason for referral across all risk-groups (Figure 2). Excluding this referral type, the low-risk group had the highest referral rate for a medicines support review in a POC (30.6%, n = 23/75). The medium-risk group represented the most referrals for patients with a personal history of a mental disorder (30.7%, n = 23). The largest proportion of referrals for compliance support with an MDS were observed in the high-risk group (34.9%, n = 15/43). Referrals due to medicines related hospital admissions, initial post discharge reviews in a care home, or care home visits were limited.
Medication Adherence and Access
Medication adherence was a significant issue for LIMOS patients (Figure 3). Overall, intentional, and unintentional poor adherence was identified in 21.2% (n = 41/193) and 67.9% (n = 131/193) of the cohort respectively. Adherence can be affected by the ability to request, access, and order medication, or through lack of coordination of prescriptions.
 |
Figure 3 Types of medication problems identified. |
The medium-risk group had the highest proportion of patients identified with intentional medication non-adherence, unintentional non-adherence, and issues accessing or requesting medication, with those affecting 29.3%, 80.0%, and 38.6% of this risk-group respectively (Figure 3). The most common problem identified unanimously across all three risk-groups was unintentional non-adherence. When conducting a Chi-Square analysis, this was the only factor found to differ significantly (X2=9.03, p=0.01) between risk groups. Additional post-hoc testing using Bonferroni correction identified a significant difference (p=<0.01) between the low-risk and medium-risk group. Patients in the medium-risk group were almost three times as likely to be identified as unintentionally non-adherent when compared to low-risk patients (OR 2.98, 95% CI 1.44–6.16, X2=8.96, p=<0.01).
LIMOS Interventions and Outcomes
Interventions Delivered
Medication adherence discussions were the most common interventions conducted by the LIMOS team across all risk groups (Figure 4); proportionally, high-risk patients were most likely to receive this intervention (81.4%, n = 35/43). High-risk patients also received the greatest number of medication reminder charts (30.2%), pharmacist medication reviews (8.2%), and MDS discontinuation (16.3%). Clinical interventions were most predominant in medium-risk patients, with an average of 1.24 interventions per patient, compared to 0.32 and 0.65 in the low and high-risk groups respectively. Medium-risk patients were also the most likely to have unnecessary medication stopped by the LIMOS team, with this intervention being delivered in almost a third of this cohort (29.3%, n = 22/75). The average number of medicines stopped per patient by risk group were 0.25 (Low), 0.48 (Medium), 0.37 (High). Across the entire cohort, a total of 32 patients (16.6%, n = 32/193) were initiated on an MDS. However, it is important to recognise that a total of 61 (31.6%) requests for an MDS were made. Notably, 29 (47.5%, n = 29/61) requests were therefore prevented as the intervention was found to be inappropriate in almost half of those patients referred for an MDS; this finding was most prominent in high-risk patients where 16.3% (n=7/43) of the cohort were prevented from receiving an inappropriate MDS.
 |
Figure 4 LIMOS interventions. Abbreviations: LIMOS, Lewisham integrated medicines optimisation service; MDS, monitored dosage system. |
Outcomes: Medicines Management and Receipt of Care
The most impactful change observed pre- and post-LIMOS for the entire cohort was number of patients recorded as self-managing their medicines (57%, n = 110/193 vs 18.7%, n = 36). There was a significant decrease (Cohen’s d=0.77, −0.38 ± 0.50, 95% CI −0.45–−0.31, p<0.01) in medication self-management across the entire cohort as well as each risk group, however the strongest effect size was observed in low-risk patients (Cohen’s d=0.91, −0.45 ± 0.50, 95% CI −0.57–−0.34, p<0.01) (Table 3). This indicates that these patients were correctly identified as being unable to cope with their medicines and required additional support with medicines-management by the LIMOS team. At a total cohort level, there was also a significant reduction in the number of compliance aids used by patients (p<0.05). Furthermore, the number of patients moving to a POC with medicines support (Level 1, 2, or 3) and number of paid care visits increased significantly (p<0.01). Only the increase in number of paid care visits remained significant when stratified across all risk groups (p<0.05). Interestingly, a significant increase in informal care was observed for both the low and medium-risk groups only (p<0.01).
 |
Table 3 Medicines Management, Care Needs, and Medication Support Pre- and Post-LIMOS |
Outcomes: A and E Visits, Admissions and Length of Stay
Data were available for 168 (87.0%, n = 168/193) patients when conducting the analyses on outcomes related to A&E visits, admissions, and length of stay pre- and post-LIMOS (Table 4). All outcomes were found to be significant for the whole cohort (p<0.05). The total number of admissions reduced significantly (p<0.01), however a significant result was not observed when stratified by risk group. Moderate effects sizes were reported for both the observed mean increase in A&E visits (Cohen’s d = 0.40, 0.78 ± 1.93, 95% CI 0.50–1.06) and mean increase in A&E visits followed by an admission (Cohen’s d = 0.40, 0.90 ± 1.39, 95% CI 0.46–1.34). These outcomes were found to be significant when stratified by risk group (p<0.05), excluding A&E visits followed by an admission in high-risk patients (p=0.35). In total, 112 additional A&E visits post-LIMOS were reported for the total cohort; the average income cost of an A&E attendance at the time of the study was £147, therefore the increase would have cost £16,464 (112 extra visits x £147).
 |
Table 4 A and E Visits, Admissions, and Length of Stay Pre- and Post-LIMOS |
Medium-risk patients were the only risk-group to observe a significant mean reduction in admission rates per patient (Cohen’s d=0.34, −0.21 ± 0.62, 95% CI −0.36–−0.07, p<0.01). Notably, the medium-risk group observed the highest number of significant outcomes pre- and post-LIMOS of any risk group. Furthermore, the medium-risk group was associated with the largest mean increase in A&E visits followed by an admission when compared to both the total cohort, as well as low and high-risk groups; the effect size for this outcome was particularly strong (Cohen’s d = 0.91, 1.08 ± 1.19, 95% CI 0.36–1.79, p<0.01).
The mean reduction in average length of stay for patients post-LIMOS was −7.67 ± 48.57 (Cohen’s d = 0.16, 95% CI −14.57–−0.78, p=0.03). This reduction was not significant when stratified by risk group, however the mean reduction in average length of stay increased in tandem with the admission risk assigned to each cohort, ranging from −5.55 ± 42.33 to −11.12 ± 41.22 in the low and high-risk groups respectively. With the average cost per bed day in COE being £300, this finding has significant cost-saving implications. The reduction in bed days (Pre-LIMOS, n = 3778 vs Post-LIMOS, n = 2297) for this sample represents a saving of £444,300 (n = 1481 x £300).
As there was limited access to clinical information to relate the causes of the A&E attendance/admission reasons to a patient’s profile, the authors felt it was useful to consider how long after the LIMOS intervention the A&E attendances and admissions occurred. Although the number of A&E attendances increased post-LIMOS, most visits (63%, n = 165/261) occurred more than 90 days post LIMOS discharge (Supplementary File 1). The greatest percentage of A&E visits after 90 days was in the low-risk group (66%, n = 80/121). Similarly with hospital admissions, the majority (66%; n = 100/152) occurred after 90 days with greatest percentage observed in the high-risk group (69%; 23/33).
In summary, the medium-risk group were most likely to present with problems related to medication adherence and access, whilst also receiving the highest number of clinical interventions. This group observed a significant shift in terms of medicines self-management and receiving care pre- and post-LIMOS. Furthermore, this was the only risk-group to report a significant reduction in admission rate per patient post-LIMOS. Hence, the evidence suggests that this risk group was seen to benefit most from LIMOS.
Discussion
An increasing trend in population dependency on health and social care services is apparent both within this study and the wider literature.16,17 Across all risk groups, rising numbers of patients starting on a POC or being moved to a higher level of support was reported. This included an increased demand for paid carers, reflecting the impact of social needs, in addition to medical needs on the variable risk of admission.15 These findings alone underpin the role for effective integration of services across the care pathway to provide appropriate support, referral and communication during episodes of transition of care for patients. This study highlighted the value of LIMOS across all risk groups but mainly those classified as medium-risk, however it also identified the need for repeated interventions given that the benefit of the interventions did not extend beyond 90 days where an increase in A&E admission rates was observed.
Most LIMOS referrals were received from GPs and social care workers. It may well be that these are identifying the reality of how patients are coping with their medicines in a domiciliary setting and therefore recognising the need for additional intervention or support in those with social care issues. There has been a significant reduction in both public health and social care spending within the last decade that has directly contributed to increasingly mortality, specifically in people over the age of 60.35 Interestingly, reduced social care spending was the more significant factor on the shift in mortality in this group, hence services such as LIMOS that look to bridge the gap may become even more essential in addressing this health inequality. Beyond the avoidance of mortality alone in this patient group, especially those without adequate social support, pharmacist-led MO services delivered through standardised methodologies can also play an important role in decreasing cost and medication-related harm, reducing hospital admissions, and improving medication adherence.33,36–39 These outcomes can also be attributed to reductions in hospital length of stay and increased support with medicines management. Encouragingly, several of these findings were demonstrated in this study.
The number of medicines per patient did positively correlate with the adapted LIMOS risk score. The medium-risk group had the highest percentage of problems identified in terms of medication non-adherence and access to their medicines. When addressing adherence issues, commonly attributed to inappropriate polypharmacy, it is also prudent to consider the types of prescribed agents too. Those that increase the risk of falls, are excessively sedating or increase the risk of bleeds are of particular concern in elderly patients.40 Therefore, a holistic review of medicines, not solely the number of prescribed agents, is needed when addressing worsening medication-related outcomes and medicines waste linked to non-adherence – a service well suited to the expertise of pharmacy teams. Community pharmacists are well placed to provide medication reviews and tackle difficulties in patients accessing medicines, particularly in deprived areas where most populations live in closer proximity to a pharmacy than a GP surgery (p<0.05).41 Furthermore, a new NHS Discharge Medicines Service was established in 2021 that aims to reduce avoidable harm caused by changes to medicines in hospital by referring patients to community pharmacy for additional support.42 This new addition to the community pharmacy essential contract provides evidence of the growing recognition of pharmacy in the UK to deliver on patient outcomes as part of an integrated medicines optimisation service.
Despite the increasing demand for pharmacy-led medication interventions, evidence to demonstrate the efficacy of one of the most widely used tools, namely MDS, is limited. MDS are commonly used in patients with multimorbidity, however recent work by Counter et al43 has emphasised that they may in fact contribute to inappropriate polypharmacy, especially among patients living in socio-economically deprived areas. Lewisham remains one of the most deprived local authorities in London.44 It was therefore encouraging to observe that the high-risk group, who are arguably the most vulnerable to medicines mismanagement, had the highest percentage of requests for MDS diverted to other potential solutions and the greatest number of adherence discussions and medicine reminder charts provided during the study.
The number of occasions when medication reviews were recorded as conducted by pharmacists was fairly low; 4% (n = 3) in low-risk, 2.7% (n = 2) medium-risk and 7% (n = 3) in the high-risk cohort. It should be noted that “medication review” was only to be ticked on the EMIS template when the pharmacist reviews all medicines that the patient is prescribed/taking. This is to ensure the annual medication review by the GP is not recorded as complete if only a partial review has been conducted by LIMOS. It is clear that the LIMOS team would need to review a patient’s medicines in order to make recommendations such as to stop an unnecessary medication, change frequency of administration or change the formulation, however this review is not recorded as such or may be included in the discussion around medication adherence data.
Unfortunately, the number of patients visiting A&E and the number of A&E visits increased significantly across the cohort (p<0.01), particularly 90 days post-intervention. However, this phenomenon has been observed following other medication review-based interventions.45 This finding is attributed to patients and/or carers identifying problems or warning signs earlier, thus increasing their willingness to access healthcare services. This finding may also reflect the need for repeated interventions, as over time (specifically over 90 days post-LIMOS in this study) the benefit will eventually decline without repeat engagement. Therefore, pharmacy-led interventions in the domiciliary setting, such as LIMOS, can be successful in identifying the needs of housebound patients and may continue to alleviate pressure on secondary care as part of an integrated care model in the future but will require on-going investment to deliver continuity of care, with multilayered interventions if they are to demonstrate sustainable impact on patient care.19
There was a significant increase in the percentage of A&E visits leading to a UHL admission in both the low and medium-risk groups (p<0.01). Although this might suggest the validity of the use of A&E by the patients, it may be that the increase is due to greater use of the admissions unit and not full admissions. The UHL Information Management department confirmed that few patients end up being sent to other hospitals from the UHL A&E department, therefore the assumption that those not admitted to UHL are sent home is correct.
Length of stay is an important performance metric that has previously been significantly associated with demographic and clinical factors such as utilisation of social care services, disease severity and inadequate homecare provision.46,47 The number of local authorities involved in the commissioning of social care services at discharge for a hospital is directly correlated with post-operative length of stay, as highlighted by Fernandez et al.47 The authors emphasise the potential benefit that integrated information systems and joint assessment could systemically have on health service outcomes. Encouragingly, the average length of stay per patient in this study was significantly reduced post-LIMOS intervention.
As outlined previously, two-thirds of A&E visits and hospital admissions occurred more than 90 days after discharge from the LIMOS service. This finding is positive when considering the potential cost avoidance provided by the LIMOS intervention through the reduction of early readmission and late readmission for UHL. This finding also highlights the need for recurrent intervention post-discharge from LIMOS for sustainable avoidance of admissions. The annual cost of the service to run was £741,000 in 2016. Although the A&E attendances for this sample significantly increased post-LIMOS, the significant decrease in the number of hospital days stay per patient, considering a care of the elderly/medical bed day costs approximately £300, is a clear positive outcome for the LIMOS service. Annualised cost savings for this cohort would have been £1,810,944 (£1,876,800–65,856; (reduced days stay) - (increased A&E visits)), bearing in mind admissions pre- and post-LIMOS to other institutions are unknown. The shift of costs to social care, in terms of increased numbers of paid carers and number of daily visits, as patients moved to higher levels of medication support, must be considered.
This study was limited by the lack of a controlled population group that did not receive the LIMOS service. This would be a valuable comparison given the increasing frailty of participants as they got older, therefore post-LIMOS events could well be attributable to natural deterioration in their health. Furthermore, there were incomplete data to include all participants in pre- and post-LIMOS analysis for A&E visits, admissions, and length of stay, hence these results should be treated cautiously. The authors also note that these data were collected in 2016, with 12-month prospective monitoring toward the end of 2017. The study was designed as part of a two-arm retrospective and prospective evaluation of LIMOS. This study included prospective monitoring for patients who were already on the LIMOS service, however the full prospective arm sought to follow-up patients from the point of initial referral. This publication was held with a view to carry out the full prospective arm to include in the analysis, however there were significant delays to ethical approval at UHL, which was only granted at the start of 2020 shortly prior to the Covid-19 pandemic. The authors for this study are pharmacists, as such, during the pandemic they were redeployed to support with additional Covid-19 pressures that led to the cancellation of the final prospective arm, hence this manuscript was not submitted until a later date. However, LIMOS is still operational and unique as the only service of its kind nationally to our knowledge. LIMOS continues to be delivered, even throughout the Covid-19 pandemic, and has not changes in its specification, interventions of risk-stratification process to support patients. Therefore, these results reflect the experiences of both previous and current patients referred to LIMOS.
Conclusion
Overall, the study has demonstrated that the LIMOS service has a positive impact on admission avoidance regardless of the admission risk score allocated to each patient. The adapted risk score provided a validated approach to stratifying risk scores across the study population and identifying risk-group specific outcomes and evidence of cost saving. Those assigned a medium-risk score appeared to benefit the most from the LIMOS intervention, however specific reductions to length of stay and MDS commencement were significant for low-risk and high-risk groups respectively, indicating value across the entire patient cohort. It is evident that pharmacy-led MO interventions can support the gap across care pathways as part of an integrated model, particularly with respect to admission avoidance in secondary care, however the consequence of increased demand on social care services as a result should be considered and requires further investigation.
Acknowledgments
The authors would like to thank the wider LIMOS team for supporting the project and UHL for hosting this research study.
Disclosure
The authors report no conflicts of interest in this work. This work was supported by the Health Innovation Network Grant.
References
1. Duerden M, Avery T, Payne R. Polypharmacy and medicines optimisation: making it safe and sound. Available from: www.kingsfund.org.uk.
2. Pasina L, Brucato AL, Falcone C, et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31:283–289. doi:10.1007/s40266-014-0163-7
3. Payne RA. The epidemiology of polypharmacy. Clin Med. 2016;16(5):465. doi:10.7861/CLINMEDICINE.16-5-465
4. Seng JJB, Tan JY, Yeam CT, Htay H, Foo WYM. Factors affecting medication adherence among pre-dialysis chronic kidney disease patients: a systematic review and meta-analysis of literature. Int Urol Nephrol. 2020;52(5):903–916. doi:10.1007/S11255-020-02452-8
5. Yeam CT, Chia S, Tan HCC, Kwan YH, Fong W, Seng JJB. A systematic review of factors affecting medication adherence among patients with osteoporosis. Osteoporos Int. 2018;29(12):2623–2637. doi:10.1007/S00198-018-4759-3
6. Cheen MHH, Tan YZ, Oh LF, Wee HL, Thumboo J. Prevalence of and factors associated with primary medication non-adherence in chronic disease: a systematic review and meta-analysis. Int J Clin Pract. 2019;73(6):e13350. doi:10.1111/IJCP.13350
7. Lemstra M, Nwankwo C, Bird Y, Moraros J. Primary nonadherence to chronic disease medications: a meta-analysis. Patient Prefer Adherence. 2018;12:721. doi:10.2147/PPA.S161151
8. Doggrell SA. Adherence to medicines in the older-aged with chronic conditions. Drugs Aging. 2012;27(3):239–254. doi:10.2165/11532870-000000000-00000
9. Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–562. doi:10.1016/S0140-6736(14)61347-7
10. Bentley J, Meyer J. Repeat attendance by older people at accident and emergency departments. J Adv Nurs. 2004;48(2):149–156. doi:10.1111/J.1365-2648.2004.03182.X
11. Scarborough P, Bhatnagar P, Wickramasinghe KK, Allender S, Foster C, Rayner M. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: an update to 2006–07 NHS costs. J Public Health. 2011;33:4. doi:10.1093/pubmed/fdr033
12. Mielck A, Vogelmann M, Leidl R. Health-related quality of life and socioeconomic status: inequalities among adults with a chronic disease. Health Qual Life Outcomes. 2014;12(1):1–10. doi:10.1186/1477-7525-12-58/TABLES/4
13. Cahir C, Moriarty F, Teljeur C, Fahey T, Bennett K. Potentially inappropriate prescribing and vulnerability and hospitalization in older community-dwelling patients. Ann Pharmacother. 2014;48(12):1546–1554. doi:10.1177/1060028014552821
14. Mannucci PM, Nobili A, Pasina L, et al. Polypharmacy in older people: lessons from 10 years of experience with the REPOSI register. Intern Emerg Med. 2018;13(8):1191–1200. doi:10.1007/S11739-018-1941-8
15. Kayyali R, Funnell G, Odeh B, et al. Investigating the characteristics and needs of frequently admitting hospital patients: a cross-sectional study in the UK. BMJ Open. 2020;10(9):e035522. doi:10.1136/BMJOPEN-2019-035522
16. Crawford R, Stoye G, Zaranko B. The impact of cuts to social care spending on the use of accident and emergency departments in England; 2018. Available from: https://www.econstor.eu/handle/10419/200304.
17. Gaughan J, Gravelle H, Siciliani L. Testing the bed-blocking hypothesis: does nursing and care home supply reduce delayed hospital discharges? Health Econ. 2015;24(Suppl1):32. doi:10.1002/HEC.3150
18. Davies LE, Spiers G, Kingston A, Todd A, Adamson J, Hanratty B. Adverse outcomes of polypharmacy in older people: systematic review of reviews. J Am Med Dir Assoc. 2020;21(2):181–187. doi:10.1016/J.JAMDA.2019.10.022
19. Kayyali R, Funnell G, Harrap N, Patel A. Can community pharmacy successfully bridge the gap in care for housebound patients? Res Social Adm Pharm. 2019;15(4):425–439. doi:10.1016/J.SAPHARM.2018.06.011
20. Evans IEM, Martyr A, Collins R, Brayne C, Clare L. Social isolation and cognitive function in later life: a systematic review and meta-analysis. J Alzheimers Dis. 2019;70(s1):S119–S144. doi:10.3233/JAD-180501
21. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi:10.1016/J.MATURITAS.2013.02.009
22. Saeed D, Carter G, Parsons C. Interventions to improve medicines optimisation in frail older patients in secondary and acute care settings: a systematic review of randomised controlled trials and non-randomised studies. Int J Clin Pharm. 2021;1:1–12. doi:10.1007/S11096-021-01354-8/FIGURES/2
23. Alton S, Farndon L. The impact of community pharmacy-led medicines management support for people with COPD. Br J Community Nurs. 2018;23(6):266–271. doi:10.12968/BJCN.2018.23.6.266/ASSET/IMAGES/LARGE/BJCN.2018.23.6.266_T02.JPEG
24. Jordan S, Prout H, Carter N, et al. Nobody ever questions—polypharmacy in care homes: a mixed methods evaluation of a multidisciplinary medicines optimisation initiative. PLoS One. 2021;16(1):e0244519. doi:10.1371/JOURNAL.PONE.0244519
25. Elliott RA, Camacho E, Jankovic D, Sculpher MJ, Faria R. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf. 2021;30(2):96–105. doi:10.1136/BMJQS-2019-010206
26. Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence clinical guideline; 2009. Available from: www.nice.org.uk/guidance/cg76.
27. Rule Edward Jones E. Why medicines optimisation is a priority for integrated care systems and how it can be improved the systematisation of medicines optimisation. 2021.
28. Barnett NL, Dave K, Athwal D, Parmar P, Kaher S, Ward C. Impact of an integrated medicines management service on preventable medicines-related readmission to hospital: a descriptive study. Eur J Hosp Pharm. 2017;24(6):327–331. doi:10.1136/EJHPHARM-2016-000984
29. Impact of an integrated pharmacy service on hospital admission costs - the pharmaceutical journal. Available from: https://pharmaceutical-journal.com/article/research/impact-of-an-integrated-pharmacy-service-on-hospital-admission-costs.
30. Dilks S, Emblin K, Nash I, Jefferies S. Pharmacy at home: service for frail older patients demonstrates medicines risk reduction and admission avoidance. Pharm J. 2021. doi:10.1211/PJ.2016.20201303
31. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):e297. doi:10.1371/JOURNAL.PMED.0040297
32. Raosoft I. Raosoft sample size calculator; 2004. Available from: http://www.raosoft.com/samplesize.html.
33. A risk matrix for risk managers; 2008. Available from: www.npsa.nhs.uk.
34. Lai K, Howes K, Butterworth C, Salter M. Lewisham integrated medicines optimisation service: delivering a system-wide coordinated care model to support patients in the management of medicines to retain Independence in their own home. Eur J Hosp Pharm. 2015;22(2):98–101. doi:10.1136/EJHPHARM-2014-000565
35. Watkins J, Wulaningsih W, da Zhou C, et al. Effects of health and social care spending constraints on mortality in England: a time trend analysis. BMJ Open. 2017;7(11):e017722. doi:10.1136/BMJOPEN-2017-017722
36. Rosen OZ, Fridman R, Rosen BT, Shane R, Pevnick JM. Medication adherence as a predictor of 30-day hospital readmissions. Patient Prefer Adherence. 2017;11:801–810. doi:10.2147/PPA.S125672
37. Klopotowska JE, Kuks PFM, Wierenga PC, et al. The effect of structured medication review followed by face-to-face feedback to prescribers on adverse drug events recognition and prevention in older inpatients - a multicenter interrupted time series study. BMC Geriatr. 2022;22:1. doi:10.1186/S12877-022-03118-Z
38. González-Bueno J, Sevilla-Sánchez D, Puigoriol-Juvanteny E, Molist-Brunet N, Codina-Jané C, Espaulella-Panicot J. Improving medication adherence and effective prescribing through a patient-centered prescription model in patients with multimorbidity. Eur J Clin Pharmacol. 2022;78(1):127–137. doi:10.1007/S00228-021-03207-9
39. Comino EJ, Harris MF, Islam MDF, et al. Impact of diabetes on hospital admission and length of stay among a general population aged 45 year or more: a record linkage study. BMC Health Serv Res. 2015;15:1. doi:10.1186/s12913-014-0666-2
40. Dahal R, Bista S. Strategies To Reduce Polypharmacy in the Elderly. StatPearls; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK574550/.
41. Todd A, Copeland A, Husband A, Kasim A, Bambra C. Access all areas? An area-level analysis of accessibility to general practice and community pharmacy services in England by urbanity and social deprivation. BMJ Open. 2015;5(5):e007328. doi:10.1136/BMJOPEN-2014-007328
42. NHS England. NHS discharge medicines service. Available from: https://www.england.nhs.uk/primary-care/pharmacy/nhs-discharge-medicines-service/.
43. Counter D, Stewart D, MacLeod J, McLay JS. Multicompartment compliance aids in the community: the prevalence of potentially inappropriate medications. Br J Clin Pharmacol. 2017;83(7):1515–1520. doi:10.1111/BCP.13220
44. Indices of deprivation - London datastore. Available from: https://data.london.gov.uk/dataset/indices-of-deprivation.
45. Rising K, Padrez K, O’Brien M. Return visits to the emergency department: the patient perspective. Elsevier; 2015. Available from: https://www.sciencedirect.com/science/article/pii/S0196064414006222.
46. Lisk R, Uddin M, Parbhoo A, et al. Predictive model of length of stay in hospital among older patients. Aging Clin Exp Res. 2019;31(7):993–999. doi:10.1007/S40520-018-1033-7/TABLES/3
47. Fernandez JL, McGuire A, Raikou M. Hospital coordination and integration with social care in England: the effect on post-operative length of stay. J Health Econ. 2018;61:233–243. doi:10.1016/J.JHEALECO.2018.02.005
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
