Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
An Investigation into the Characteristics and Distribution Patterns of Diseases Detected via Gastroscopy in Northern Xinjiang, China
Authors Wang FF, Li N, Wang JJ, Muyesai N, Fu H
Received 10 August 2023
Accepted for publication 29 December 2023
Published 16 January 2024 Volume 2024:17 Pages 229—235
DOI https://doi.org/10.2147/JMDH.S434846
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Fei-Fei Wang,1,* Nan Li,1,* Jing-Jing Wang,1 Nijiti Muyesai,1 Haiyan Fu2
1The People’s Hospital of Xinjiang Uygur Autonomous Region, Xinjiang Emergency Care Center, Urumqi, Xinjiang Uygur Autonomous Region, 830000, People’s Republic of China; 2Department of Gastroenterology, Urumqi Friendship Hospital, Urumqi, Xinjiang Uygur Autonomous Region, 830000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Haiyan Fu, Department of Gastroenterology, Urumqi Friendship Hospital, 558, Shengli Road, Urumqi, Xinjiang Uygur Autonomous Region, 830000, People’s Republic of China, Tel/Fax +8618599026892, Email [email protected] Nijiti Muyesai, The People’s Hospital of Xinjiang Uygur Autonomous Region, Xinjiang Emergency Care Center, the People’s Republic of China, No. 91, Tianchi Road, Tianshan District, Urumqi, 830000, People’s Republic of China, Tel/Fax +86 13899955322, Email [email protected]
Objective: The aim of this study is to examine the distribution and features of gastroscopy in northern Xinjiang, a province in China.
Methods: We included a group of 895 patients diagnosed with digestive diseases at Urumqi Friendship Hospital and analyzed their gastroscopic results and baseline data.
Results: Among patients aged 12 to 86 years in the specified region, females exhibited a heightened susceptibility to esophageal-gastrointestinal and intestinal disorders compared to males. The mean age for chronic gastritis onset was determined to be 54.79 years. In the context of esophageal-gastric-intestinal disorders, the distribution across various ethnic groups manifested as follows: the Han, Uygur, Hui, and Kazakh populations comprised 53.97%, 23.91%, 7.15%, and 3.46%, respectively. Through principal component-based dimension reduction analysis, we identified chronic non-atrophic gastritis with erosive gastritis, duodenal bulb inflammation, and chronic non-atrophic gastritis (predominantly in the gastric antrum) as pivotal factors contributing to differences in hiatal hernia. Multiple linear regression models were established for different ethnic groups, duodenal bulb inflammation, and hiatal hernia by age. The results revealed a heightened risk of duodenal bulb inflammation (P < 0.01) in Han, Kazakh, Hui, Mongolian, and Uygur women, while the risk of hiatal hernia exhibited a positive correlation with age (P = 0.001).
Conclusion: Among patients undergoing gastrointestinal examinations in northern Xinjiang, the most prevalent pathological condition was identified as chronic gastritis. Notably, within this subgroup, the prevalence of duodenal bulb inflammation was found to be greater in women than in men. The ethnic composition within this context encompassed patients from the Han, Kazakh, Hui, and Mongolian ethnic groups. Furthermore, a positive correlation was identified between the incidence of esophageal hiatal hernia and age.
Keywords: age, ethnicity, esophageal-gastric-intestinal disease, gastroscopy, gender, northern Xinjiang
Introduction
Digestive system diseases presently constitute the most prevalent health issues affecting the human population. The primary causes of digestive diseases, particularly those affecting the gastroduodenal region, are attributed to dietary patterns characterized by high sugar and fat intake, tobacco consumption, and elevated levels of work and life-related stress, all of which significantly jeopardize human well-being. Consequently, there has been a steady rise in the incidence of malignant tumors within the digestive tract, with gastroduodenal diseases standing out as the most prevalent among them. Based on statistical data, gastrointestinal diseases rank as the second most prevalent worldwide in terms of both incidence (26.3%) and mortality (35.4%) rates, surpassing various other diseases.1 This escalating trend has led to an increased number of people placing impetus on gastrointestinal diseases.2,3 Endoscopy, comprising gastroscopy for upper digestive tract examination and colonoscopy for inspecting the colon and rectum, is the primary modality for assessing the gastrointestinal tract.4,5 In Xinjiang Province, situated in northwest China and characterized by a diverse population primarily composed of Han, Uyghur, and Kazakh ethnic groups, variations in dietary structures among these ethnicities contribute to differing groups of chronic atrophic gastritis.6,7 This retrospective study involves a comprehensive analysis, encompassing esophageal-gastrointestinal diseases and gender, age, ethnicity, and diseases, among 895 patients in northern Xinjiang. The objective is to systematically assess disease incidence in northern Xinjiang, considering key demographic factors. We hope that our study offers valuable insights that can potentially serve as a guide for prognostic considerations and lifestyle interventions.
Methodology
Study Participants
The participants included in our study were patients who underwent their initial gastroscopy with simultaneous pathological biopsy between November 17, 2020, and November 17, 2022, at You Yi Hospital in Urumqi, Xinjiang Province. Inclusion criteria comprised patients aged between 12 and 86 years who, following discomfort, underwent histopathological examination for the initial time during gastroscopy, revealing upper gastrointestinal mucosal lesions. Exclusion criteria encompassed women who were pregnant or lactating, individuals with a prior history of digestive system diseases, heart and vascular failure, severe endocrine diseases, severe liver and kidney disorders, pulmonary respiratory ailments, blood disorders, malignancies, and other systemic diseases, as well as those experiencing infectious diseases or had taken antibiotics, gastric acid secretion inhibitors, microecological agents, immunosuppressants, cytotoxic agents, cytokines, hormones, or other medications impacting gastric flora, within the preceding month. All participants in our study were 12 years of age or older, culminating in a total enrollment of 895 patients. In cases where a patient received multiple diagnoses, the most severe diagnostic outcome was considered the final diagnosis. The age range of the participants spanned from 12 to 86 years, with a mean age of 54.79 years.
This study adhered to the principles outlined in the Declaration of Helsinki and obtained approval from the Ethics Committee of Urumqi Friendship Hospital (2022NO.11). Written informed consent was obtained from participants over 18 years old and guardians of minors under 18 years old.
Methods
The gastroscopic procedures were conducted by specialized digestive practitioners who had undergone rigorous professional training. The Pentax EG-2970k electronic gastroscope, manufactured by Hya Corporation, was utilized for the examination. During the examination, patients were placed in the left lateral decubitus position with their head leaning forward, jaw slightly moved towards the center, and supported in a single position. Routine local anesthesia was administered during the procedure. The electronic gastroscope was introduced into the stomach to meticulously observe morphological changes in the gastric area and small grooves, facilitating the identification of lesion locations. Disposable electronic gastroscopy was used in the observation group, specifically the XZING-W200B model from Huizhou Xianzan Technology Co., Ltd. Prior to the examination, patients in the observation group were subjected to a 6-hour fasting period and administered compound polyethylene glycol electrolyte for intestinal preparation. Following conventional left lateral positioning and anesthesia, the disposable electronic gastroscope, as well as the conventional electronic gastroscope, were gradually maneuvered through the esophagus, cardia, observation, gastric body, antrum, pylorus, and duodenum. Subsequently, the gastroscope was slowly withdrawn following a systematic examination of each corresponding anatomical section. The acquired data from the examination process were uploaded to the instrument-supporting workstation for imaging processing, and the diagnostic evaluation was carried out collaboratively by two doctors. The electronic gastroscopy images were interpreted as positive if an ulcer area was visually identified and negative otherwise. Lesion specimens were meticulously labeled based on their anatomical locations and subjected to pathological examination. All biopsy samples were fixed in 10% formalin, embedded in paraffin, and stained with hematoxylin and eosin (HE). Histopathological diagnoses of the biopsies were conducted by two experienced pathologists.
Statistic Analysis
The clinical data of all participants were entered in Microsoft Excel and subsequently analyzed using IBM SPSS 20.0 statistical software. Continuous data are presented as the mean ± standard deviation or 95% confidence interval, while categorical variables are expressed as percentages. The chi-squared or Fisher’s exact test was employed for comparative analyses of categorical variables. The Kruskal–Wallis test was used for the comparison of continuous data. A significance level of P < 0.05 was considered indicative of a statistically significant difference.
Results
Demographic Profile and Age-Associated Trends Among the Study Participants
Based on the gastroscopic examination, among the 895 patients undergoing their initial gastroscopic examination, 430 patients (48%) were males, while 465 patients (52%) were females. The age range of the 895 participants spanned from 12 to 86 years, with an average age of 54.79 years. A graphical representation of age distribution based on gender is presented in Figure 1. Specifically, male participants exhibited an age range of 16 to 86 years, while female participants ranged from 12 to 84 years. Notably, the average age of onset for esophageal, stomach, or intestinal diseases was observed to be between 55 to 60 years for women and between 65 to 70 years for men.
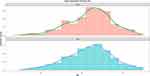 |
Figure 1 Age distribution density map for esophageal-gastric-duodenal disease in northern Xinjiang. |
Ethnic-Based Distribution and Prevalence of Gastrointestinal Diseases Among the Study Participants
The distribution of diseases based on ethnic groups, as depicted in Figure 2, is outlined below. Based on ethnic groups, the distribution of gastrointestinal diseases is 53.97%, 23.91%, 7.15%, and 3.46% among Han, Uyghur, Hui, and Kazakh ethnic groups, respectively. Specifically, chronic non-atrophic gastritis with erosion, duodenal bulb inflammation, chronic non-atrophic gastritis (predominantly located in the gastric antrum), and grade A reflux esophagitis manifest at proportions of 25.36%, 15.20%, 6.48%, and 5.92%, respectively.8
 |
Figure 2 The distribution characteristics of esophageal-gastric-duodenal disease by ethnic group in northern Xinjiang. |
Principal Component Analysis
The principal component analysis scree plot is illustrated in Figure 3. Herein, the horizontal coordinate represents the number of components, while the vertical coordinate denotes the variance of these components. The turning point in the graph, where the curve transitions from steep to flat, designates the optimal number of principal components to be selected. The cumulative variance contribution rate was determined using the formula: the variance of each individual component divided by the sum of the variances of all components. Upon completion of dimensionality reduction through principal component analysis, the cumulative variance contribution rates for the first three principal components were computed as 0.02, 0.03, and 0.05, respectively. Notably, the first, second, and third principal components explained the variances in hiatal hernia at percentages of 23%, 5%, and 2%, respectively.
 |
Figure 3 The underlying diagram for an analysis of the key components of esophageal-gastric-duodenal disease in northern Xinjiang. |
Multivariate Regression Analysis
We established multiple linear regression models by integrating ethnicity, age, duodenal bulb inflammation, and hiatal hernia. The analysis revealed a significant likelihood for females to develop duodenal bulb inflammation compared to males (P = 6.8E-10). Moreover, ethnic groups including Han, Kazakh, Hui, Mongol, and Uyghur exhibited a higher propensity for duodenal bulb inflammation (P < 0.01, as depicted in Figure 4). Additionally, the risk of developing hiatal hernia was found to increase with advancing age (P = 0.001).
 |
Figure 4 Gender characteristics of gastroduodenal and esophageal disease among diverse ethnic groups in northern Xinjiang. |
Discussion
Upper gastrointestinal tract diseases represent a significant health concern that profoundly impacts the quality of life of individuals. Based on the 2012 Global Cancer Statistics, gastric cancer ranks as the third and fourth most common malignant tumor worldwide.9 Peptic bleeding, such as gastric ulcer bleeding and intestinal bleeding, is a major cause of acute fatalities, posing serious threats to human health. It can be seen that esophageal and stomach diseases have caused significant life and property damage to human health. The northern region of Xinjiang province in China, characterized by its expansive territory and diverse population comprising over a dozen ethnic groups, exhibits variations in economic structure, dietary habits, lifestyle, environment, and geographical location. For comprehensive correlation analysis, we included 895 patients in this study. Our analysis revealed that 430 patients (48%) were male, and 465 patients (52%) were female. Interestingly, the incidence of esophagogastric and duodenal diseases was found to be higher in women than in men, contrasting with previous studies that reported a lower incidence in women. The mean age of onset for esophageal gastrointestinal diseases was determined to be 54.79 years, with a notable increase in incidence within the age range of 50 to 75 years, followed by a gradual decline after the age of 75. Women in this age group, often experiencing menopause, undergo a series of psychological and physiological changes attributed to a substantial reduction in estrogen.
Jacenik discovered that in women over 50 years old, the protein level of ER α (estrogen receptor) increased in inflammatory diseases of the digestive tract.10 The dysregulation of estrogen receptors in the mucosa suggests that estrogen signaling may play a role in the local immune response and maintain epithelial homeostasis in a sex- and age-dependent manner. Further exploration is needed to determine the relevance of estrogen signaling to inflammatory diseases of the upper digestive tract, such as esophagitis, gastritis, and other mucosal lesions. In the current study, ethnic distribution of these diseases was observed among Han, Uygur, Hui, and Kazakh ethnic groups. Varied eating habits were noted among different ethnic groups, with Han participants consuming more vegetables and fewer meat and dairy products compared to Uygur and Kazakh participants. The potential relationship between diet and the occurrence of these diseases necessitates further discussion. The occurrence of esophageal hiatal hernia was found to increase with age. We propose that changes in the proportion of elastic fibers and collagen fibers in connective tissue undergo and stress changes with age. Additionally, the prevalence of digestive zone diseases varied among different ethnic groups, both regionally and ethnically. In a 2013 meta-analysis conducted in China, covering 25 provinces and 69 clinical studies from 2000 to 2011, the overall endoscopic detection rate of Barrett’s esophagus (BE) was 1.0%, with a mean patient age of 49.07 ± 5.09 years.11 The study posited potential factors contributing to the lower detection rate, encompassing changes in environmental risk factors, diverse genetics, and different medical practices, such as diagnostic criteria for BE and expertise in endoscopy. Notably, the study revealed differences in the incidence and mortality of gastric cancer among different ethnic groups, with Uygur and Han ranking first and second, respectively.12 Given the distinctive characteristics observed in northern Xinjiang and among different ethnic groups, these findings may serve as a foundation for future epidemiological investigations.
The International Agency for Research on Cancer (IARC) currently designates chronic atrophic gastritis as a precancerous disease.13 Helicobacter pylori infection is identified as a prominent cause of chronic atrophic gastritis.13,14 In our study, chronic atrophic gastritis constituted 6.48% of cases, ranking third among upper gastrointestinal tract diseases. Balendra et al reported that patients diagnosed with gastric cancer exhibited a higher median sodium intake compared to healthy controls.15 Notably, H. pylori infection emerged as another risk factor, particularly impacting patients with elevated daily sodium intake. Thus, epidemiological findings suggest that reducing salt intake and employing antimicrobial therapy may diminish individual susceptibility to gastric cancer. Further research and discussion are needed to explore whether the high incidence of such diseases is associated with local customs and dietary structures. The identification of diverse characteristics, population distribution, lifestyles, and epidemic patterns of gastrointestinal diseases across different ethnic groups facilitates the formulation of preventive strategies tailored to local conditions. Understanding disease characteristics and implementing lifestyle interventions to impede disease progression has become a crucial focus in addressing esophageal and gastrointestinal diseases, ultimately ensuring the safety of life and property. However, certain limitations exist in our study. For instance, when examining disease distribution among different ethnic groups, detailed subgrouping was not employed, and factors such as age and gender were not consistently controlled, potentially introducing confounding bias into the results. In the follow-up study, we intend to address these limitations to enhance the rigor and reliability of the study.
Conclusion
The diverse influences of different ethnic groups, regions, lifestyles, and economic levels in northern Xinjiang contribute to variations in esophageal-gastric-intestinal diseases. Conducting an epidemiological investigation to discern the underlying causes based on these differences holds significant importance for both the treatment and prevention of diseases in future.
Data Sharing Statement
The datasets used or analysed during the current study available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki.This study was conducted with approval from the Ethics Committee of Urumqi Friendship Hospital (2022NO.11). Written informed consent was obtained from participants over 18 years old and guardians of minors under 18 years old.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
This study was supported by a grant from Regional fund of the Natural Science Foundation of the Xinjiang Uygur Autonomous Region (No. 2022D01F76).
Disclosure
None of the authors have any financial disclosure or conflict of interest.
References
1. Lu L, Mullins CS, Schafmayer C, et al. A global assessment of recent trends in gastrointestinal cancer and lifestyle-associated risk factors. Cancer Commun. 2021;41(11):1137–1151. doi:10.1002/cac2.12220
2. Bang CS, Lee JJ, Baik GH. Computer-aided diagnosis of esophageal cancer and neoplasms in endoscopic images: a systematic review and meta-analysis of diagnostic test accuracy. Gastrointest Endosc. 2021;93(5):1006–1015.e13. doi:10.1016/j.gie.2020.11.025
3. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries.CA Cancer. J Clin. 2018;68(6):394–424.
4. Du W, Rao N, Dong C, et al. Automatic classification of esophageal disease in gastroscopic images using an efficient channel attention deep dense convolutional neural network. Biomed Opt Express. 2021;12(6):3066–3081. doi:10.1364/BOE.420935
5. Hu Y, Bao H, Jin H, et al. Performance evaluation of four prediction models for risk stratification in gastric cancer screening among a high-risk population in China. Gastric Cancer. 2021;24(6):1194–1202. doi:10.1007/s10120-021-01204-6
6. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi:10.3322/caac.21338
7. Stene-Larsen G, Weberg R, Frøyshov Larsen I, et al. Relationship of overweight to hiatus hernia and reflux oesophagitis. Scand J Gastroenterol. 1988;23(4):427–432. doi:10.3109/00365528809093890
8. Torre L, Bray F, Siegel RL, et al. Erratum: global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2020;70(4):313.
9. Balakrishnan M, George R, Sharma A, et al. Changing trends in stomach cancer throughout the world. Curr Gastroenterol Rep. 2017;19(8):36. doi:10.1007/s11894-017-0575-8
10. Jacenik D, Cygankiewicz AI, Mokrowiecka A, et al. Sex- and age-related estrogen signaling alteration in inflammatory bowel diseases: modulatory role of estrogen receptors. Int J Mol Sci. 2019;21:20. doi:10.3390/ijms21010020
11. Al Dulaimi D. Recent advances in oesophageal diseases. Gastroenterol Hepatol Bed Bench. 2014;7:1.
12. Zhou L, Lin S, Ding S, et al. Relationship of Helicobacter pylori eradication with gastric cancer and gastric mucosal histological changes: a 10-year follow-up study. Chin Med J (Engl). 2014;127(8):1454–1458.
13. Poplawski T, Chojnacki C, Czubatka A, et al. Helicobacter pylori infection and antioxidants can modulate the genotoxic effects of heterocyclic amines in gastric mucosa cells. Mol Biol Rep. 2013;40(8):5205–5212. doi:10.1007/s11033-013-2622-3
14. Green J, Roddam A, Pirie K, et al.; Million Women Study collaborators. Reproductive factors and risk of oesophageal and gastric cancer in the million women Study cohort. Br J Cancer. 2012;106(1):210–216. doi:10.1038/bjc.2011.525
15. Balendra V, Amoroso C, Galassi B, et al.; High-Salt Diet Exacerbates H. pylori infection and increases gastric cancer risks. J Pers Med. 2023;2023:13.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
