Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
An Evidence-Based Nursing Intervention Decreases Anxiety, Depression, Sleep Quality and Somatic Symptoms of Patients with Acute Ischemic Stroke
Authors Gao WJ, Bao WJ, Sun SJ
Received 4 June 2022
Accepted for publication 15 September 2022
Published 25 October 2022 Volume 2022:18 Pages 2443—2451
DOI https://doi.org/10.2147/NDT.S377340
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Wen-Juan Gao,1,* Wen-Juan Bao,2,* Su-Juan Sun3
1Neurology, Hebei General Hospital, Shijiazhuang City, Hebei 050051, People’s Republic of China; 2Department of Hepato-Biliary-Pancreatic Surgery, Hebei General Hospital, Shijiazhuang City, Hebei, 050051, People’s Republic of China; 3Nursing Department, Hebei General Hospital, Shijiazhuang City, Hebei, 050051, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Su-Juan Sun, Nursing Department, Hebei General Hospital, 348 Heping West Road, Xinhua District, Shijiazhuang City, Hebei Province, 050051, People’s Republic of China, Tel +86 0311-85988114, Fax +86 85988318, Email [email protected]
Purpose: This study aimed to explore the effects of evidence-based nursing (EBN) intervention on anxiety, depression, sleep quality and somatic symptoms of patients with acute ischemic stroke (AIS).
Methods: The eligible AIS patients were randomized into the intervention group and control group in a 1:1 ratio. Patients in both groups received routine nursing care. On the basis of routine nursing, patients in the intervention group also received EBN. Self-rating anxiety scale (SAS), self-rating depression scale (SDS), Pittsburgh Sleep Quality Index (PSQI), and the Patient Health Questionnaire-15 (PHQ-15) were used to assess patients’ anxiety, depression, sleep quality, and somatic symptoms at baseline (T0) and 6 months after intervention (T1), respectively.
Results: There was no difference in SAS, SDS, PSQI, and PHQ-15 scores at T0 between the 2 groups (all P > 0.05). Comparing to the control group, the intervention group had significantly lower SAS and SDS scores at T1 (P = 0.002, P < 0.001, respectively). The SAS and SDS score changes (T1-T0) were more evident in the intervention group than in the control group (all P < 0.001). No difference of PSQI or PHQ-15 score between the 2 groups was observed at T1. However, the PSQI and PHQ-15 score changes were more evident in the intervention group than in the control group (P = 0.044 and P = 0.007, respectively).
Conclusion: EBN invention significantly improved anxiety, depression, sleep quality and somatic symptoms of patients with AIS.
Keywords: stroke, outcome, stroke aftercare, evidence-based nursing, post-stroke complications, somatic dysfunction, emotional distress
Introduction
Stroke is the second-most cause of mortality worldwide, and there are about 2.5 million new stroke cases occurring in China each year.1,2 The leading subtype of stroke is acute ischemic stroke (AIS), which is triggered by cerebral ischemia, leading to the dysfunction of brain vascular components.3 It has been reported that a large number of AIS patients faced serious post-stroke complications such as depression and anxiety after stroke.2 Given its great incidence following stroke, stroke-induced PTSD may be a substantial new risk factor for recurrent stroke, which is also rather prevalent.4 These post-stroke complications can adversely affect stroke clinical outcomes, increase the risk of functional dependence and reduce the quality of life (QOL).5 Depressive feelings and a lack of self-efficacy in the rehabilitation process are linked to a poor level of physiotherapy effectiveness6 Therefore, effective management to reduce post-stroke complications in AIS patients is essential.
Biopsychosocial factors, such as a patient’s age, gender, and time since the onset of stroke, as well as socioeconomic status and the effectiveness of formal and informal care, appear to be the most important areas of study in post-stroke rehabilitation. This is because the factors that affect a patient’s recovery after a stroke can differ greatly from person to person. As a result, bio-psychosocial assessment of patients and evidence-based nursing interventions is essential to their recovery.
In recent years, evidences from previous studies have indicated that the specialized nursing care contributed to the improvement of post-stroke depression and anxiety.2,5 For example, Verberne et al found that nurse-led stroke aftercare, which included the procedures such as psychoeducation, cognitive and emotional screening, and specialist care, showed beneficial for emotional well-being in comparison to care-as-usual.5 Zhang et al2 demonstrated that a newly designed intensive caregiver education program conducted by nurses could effectively reduce anxiety and depression in patients with AIS.
Evidence-based nursing (EBN) intervention is a nursing strategy that uses credible scientific research results as evidence in combination with patient needs to implement patient care, providing patients with personalized nursing services.6,7 EBN has been widely applied in clinical practice and makes great progress in the management of diseases such as chest pain,8 postpartum depression6 and acute coronary syndrome.9 For stroke, previous studies have shown that using EBN theories could reduce the morbidity and mortality associated with stroke.10,11
Based on previous research results on post-stroke depression and anxiety, we hypothesized that EBN might have benefits on improving psychiatric outcomes of patients with AIS. Thus, we established an EBN team which composed of the head nurse and the nurses in charge of the Department of Neurology in our hospital. We aimed to explore the effects of EBN intervention on anxiety, depression, sleep quality and somatic symptoms of patients with AIS.
Methods
Patients
This prospective single-center study was approved by the Ethics Committee of Hebei General Hospital (Ethical Committee Decision number 13.01.2020/19-218) in accordance with the Declaration of Helsinki. All participants written provided informed consent before participating in the study.
The inclusion criteria for AIS patients included (1) first diagnosed as AIS through transcranial computed tomography (CT) and magnetic resonance angiography (MRI) examinations; (2) aged within 50–85 years old; (3) with the ability to complete the questionnaire evaluation independently; (4) had at least one caregiver in their family; (5) voluntary to cooperate with the study evaluation.
The exclusion criteria were as followed: (1) with evidence of hemorrhagic stroke; (2) secondary AIS; (3) cognitive impairment; (4) uncontrolled concomitant diseases such as significant heart or lung dysfunction.
The eligible patients were randomized into the intervention group and control group in a 1:1 ratio. A thorough randomization technique was used to generate the patient allocation sequence by performing the online Research Randomizer Program (www.randomizer.org). The allocation of patients was performed by an independent nurse. Researchers involved in the data collection and analysis were blind to the group allocation.
Nursing Intervention
Patients in both groups (the intervention and control groups) received routine nursing care including health education, rehabilitation training, psychological counseling and close observation of patient’s condition. The treatment was governed by protocols, and it was uniform across all sites. Both the length of time spent on the intervention and the way it was carried out were identical for each individual patient. The therapy process was provided by multidisciplinary teams led by a consultant psychiatrist. In addition to psychiatrists and psychologists on these teams were social workers and nurses. The nursing supervisor and psychologist in each department kept a close check on the quality of this study the rest of the time because it was a clandestine study. On the basis of routine nursing, patients in the intervention group also received EBN. The procedure of evidence‐based nursing was as followed:
Question Proposing
- How to effectively improve the patient’s depression, anxiety, sleep quality and somatic symptoms after stroke;
- How to implement effective psychological suggestion for patients with stroke;
- How to improve the patient’s post-stroke nursing effect.
Evidence‐Based Method
Relevant stroke nursing literatures were collected through databases such as PubMed, Web of Science and CNKI. Search terms included stroke, depression, anxiety, etc. Excluded were research studies conducted without statistical analysis, nursing methods lacking accuracy, and indicators without review. Then, the relevant data were discussed by EBN team to obtain nursing evidence.
Evidence‐Based Support
The same number of sessions was given to each patient. In every given six-month period, psychotherapy was performed. The same treatment protocol was implemented, which covers three aspects as follows.
- Emotional nursing: Instrumentation and evaluation of emotional reactivity We evaluated three important characteristics of emotional reactivity: subjective emotional experience, facial expression, and physiological response. EBN was delivered by multidisciplinary teams under the guidance of a consultant psychiatrist. These teams included psychiatrists, nurses, psychologists, occupational therapists, psychotherapists, family therapists, and social workers. The frequency of trips to PTSD-specific clinics was used to gauge the effectiveness of the psychotherapy for the condition. In every given six-month period, psychotherapy was categorized as zero visits, one to three visits, or minimally adequate treatment duration when the number of visits ranged from one to three. According to the patient’s personality, family, and psychological characteristics, psychological intervention was conducted. Several randomized controlled studies have confirmed that emotional nursing can reduce the level of negative emotion after stroke.12 Emotional nursing is a systematic nursing scheme under the theory of traditional Chinese medicine. It can transfer the patient’s attention of the disease to good external conditions, urge the patient to maintain a good state of mind, establish confidence to overcome the disease and improve patient compliance.12 Emotional nursing was given to the patients once a week in the hospital and discharge stages. Each therapy was 60 min in duration through face-to-face communication.
- Caregiver education: caregiver education was given within 7 days after the patient’s hospitalization. The education consisted of the following topics: first, the patients’ caregivers were taught to know the basic knowledge of stroke, which included risk, causes, symptoms, therapies, drug side effects and managements of stroke; second, the caregivers were taught necessary skills to help patients perform daily rehabilitation training; third, the caregivers were taught the methods to help patients manage stress, anxiety, depression, and other unstable moods; fourth, the caregivers were taught the importance of family members in assisting rehabilitation of the patients and how to establish effective communication with patients; finally, the caregivers were taught about healthy diet and appropriate method for feeding, in order to increase the food appetite of patients.
- Early rehabilitative training: the patients were encouraged to implement early rehabilitation when they were in stable conditions. At first, passive movements in bed were performed. Then, short distances walking, independently urinate, climb stairs, etc. were encouraged to be performed in order to gradually improve the patient’s ability to take care of themselves.
Instruments
Anxiety was measured by Zung’s self-rating anxiety scale (SAS), which includes 20 items using a 4-grade scoring method with a maximum score of 100 points.13,14 Usually, SAS score has the 4 categories: no anxiety (<50), mild anxiety (50–59), moderate anxiety (60–70) and severe anxiety (>70). A greater score indicates the higher degree of anxiety.13
Depression was measured by Zung’s self-rating depression scale (SDS). The SDS also employs a 4-grade scoring method with a maximum score of 100 points.14 A higher SDS score indicates a severe depression, which was classified as: <50, no depression; 50–59, mild depression; 60–70, moderate depression; >70, severe depression.15
The sleep quality was measured by Pittsburgh Sleep Quality Index (PSQI). PSQI, an 18-item questionnaire with 7 subscales, is the most commonly used instrument to assess the subjective sleep quality. Each subscale of PSQI has a score of between 0 and 3, with a total score of 0–21. A higher score reflects poorer sleep quality.16
Somatic symptoms of patients were measured by the Patient Health Questionnaire-15 (PHQ-15), which comprises 15 most typical somatic complaints in primary care. Each item is scored from 0 to 2, with a higher score indicating more severe somatic symptoms.17
The above questionnaires/scales were performed at baseline (T0, pre-intervention) and six months after T0 (T1). All questionnaires and scales were completed by patients themselves independently or with the assistance of their caregivers.
Statistical Analysis
The data in this study were analyzed by the SPSS (version 22.0). The categorical data were described as numbers (percentages) and compared using the χ2 test or Fisher’s exact test. The quantitative data were described as mean ± standard deviation (SD) and compared using the t-test between 2 groups. Analysis of normal distribution was performed. Data with normal distributions were analyzed by parametric tests, whereas data with non-normal distributions were analyzed by non-parametric tests. A p-value <0.05 considered as statistically significant.
Results
From January 2020 to September 2021, a total of 178 patients with AIS were screened for eligibility, and 60 patients did not meet inclusion criteria and were excluded. Subsequently, the remaining 118 patients were randomized at a ratio of 1:1 into the intervention group (n = 59) and the control group (n = 59). In the intervention group, 3 patients withdrew, including 2 losses to follow-up (3.39%) and 1 relapses or deaths (1.69%), leaving 56 patients (94.92%) that completed the 6-month follow-up. In the control group, 5 patients withdrew including 4 losses to follow-up (6.78%) and 1 relapses or deaths (1.69%), leaving 54 patients (91.53%) completed the entire study. Finally, 56 patients of intervention group and 54 patients of control group were included in the final analysis.
The mean ages of patients in the intervention group and control group were 64.07 ± 9.02 and 64.63 ± 8.20, respectively (P = 0.734). The male/female ratios were 25/31 in the intervention group and 25/29 in the control group (P = 0.865). There was no difference in SAS, SDS, PSQI, and PHQ-15 scores at T0 between the 2 groups (all P > 0.05). The baseline characteristics of the 2 groups are shown in Table 1.
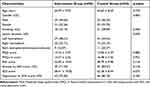 |
Table 1 Baseline Characteristics of Patients |
As shown in Figure 1, patients in the intervention group had significantly lower SAS scores measured at T1 than those in the intervention group (P = 0.002). The SAS score change (T1-T0) was also decreased in the intervention group compared with the control group (P < 0.001, Figure 1B). According to the SAS scores at T0, patients were divided into 2 subgroups (patients with and without anxiety at T0). For patients with anxiety at T0, SAS scores were evidently reduced from T0 to T1 in the intervention group compared with the control group (P < 0.001, Table 2). For patients without anxiety at T0, the SAS score change in the intervention group was not significantly different from that in the control group (P = 0.316, Table 2).
 |
Table 2 Subgroup Analyses of SAS and SDS Scores |
Comparing to the control group, the intervention group had significantly lower SDS scores at T1 (P < 0.001, Figure 2A). The SDS score change was more evident in the intervention group than in the control group (P < 0.001, Figure 2B). According to the SDS scores at T0, patients were divided into 2 subgroups (patients with and without depression at T0). The SAS scores were evidently reduced (T1-T0) in the intervention group compared with the control group in both subgroups of patients. Our data indicated that EBN was effective in reducing depression in AIS patients with and without depression at baseline.
No difference of PSQI scores between the intervention group and the control group was observed at T0 and T1 (all P > 0.05) (Figure 3A). However, the PSQI score change was more evident in the intervention group than in the control group (P = 0.044, Figure 3B). As for somatic symptoms assessed by PHQ-15, the score in the intervention group was not significantly different from that in the control group at T0 and T1, while the PHQ-15 score change (T1-T0) was more significant in the intervention group (P = 0.007, Figure 4).
Discussion
Although the survival rate of AIS has been markedly improved by AIS therapies in recent years, the number of patients suffered from post-stroke complications such as anxiety and depression was not reduced significantly.2 In this study, we found that EBN intervention could improve anxiety, depression, sleep quality and somatic symptoms of patients with AIS. Our results provided a new strategy to manage post-stroke complications.
EBN is developed on the basis of evidence-based medicine, which is formed by 3 factors: selection of the best research basis, consideration of the patient’s needs, and improvement clinical experiences and skills of the nurses.18 Currently, EBN has become an important clinical nursing method.19 Based on the EBN theory, we first established an EBN team, and each team member was trained to improve the evidence-based ability. Then, we collected a large number of valuable studies, and summarized the evidence-based points to form a nursing plan. From previous studies, we found that emotional nursing based on the theory of traditional Chinese medicine could transfer the patient’s attention of the disease to good external conditions, urge the patient to maintain a good state of mind, establish confidence to overcome the disease and improve patient compliance.12 Several randomized controlled studies have confirmed the important role of emotional nursing to improve the cognitive function and reduce anxiety and depression after stroke.12 Thus, emotional nursing was put into our EBN intervention plan. It has been reported that about 3.5 million individuals with stroke received care from their caregivers.20,21 Caregivers are important to improve stroke patients’ medical and rehabilitation outcomes.21 Several studies showed that caregivers of stroke patients also faced many psychological problems such as depression, anxiety and exhaustion.22 As mood and behavior changes in caregivers dramatically affecting the outcomes of stroke patients,23 the education care programs for caregivers seem to be important. Zhang et al found that the intensive caregiver education program effectively reduced cognitive impairment, anxiety and depression in patients with AIS,2 emphasizing the significance of caregiver education for AIS patients. Based on these evidences, caregiver education was also put into our EBN intervention plan.
Excitingly, in the present study, we found that our EBN invention significantly improved anxiety, depression, sleep quality and somatic symptoms of patients with AIS, compared with routine nursing. Evidences indicated that psychological disorders including anxiety and depression might affect more than 50% of AIS patients, which were associated with poor QOL of AIS patients.2 In this research, SAS and SDS scores were employed to evaluate the severity of anxiety and depression at baseline and follow-up. We found that the SAS score change (T1-T0) was significantly decreased in the intervention group compared with the control group, mainly occurring in patients with anxiety at T0. The SDS score change was also more evident in the intervention group than in the control group regardless of the status of depression at T0. The above results were similar to previous reports that an effective nursing intervention alleviated depression and anxiety after stroke.2,5 PSQI and PHQ-15 scores were used in this study to assess sleep quality and somatic symptoms of patients. Correspond to the SAS and SDS changes, EBN intervention also resulted in significant PSQI score and PHQ-15 score changes compared with routine nursing. Sleeping problems are an important manifestation of anxiety and depression.24,25 Our EBN invention to reduce anxiety and depression might contribute to the improvement of sleep quality. In our EBN intervention, we also used an early rehabilitative training to improve patients’ somatic symptoms. A link of anxiety and depression symptoms and somatic symptoms has been established in the previous studies.26 Thus, the strategy to improve somatic symptoms also helps reduce anxiety and depression.
The presence of cognitive impairment or depression can significantly hinder the rehabilitation process and alter its final result, making evidence-based nursing care for patients with co-occurring mood disorders critical. Physical and emotional well-being, as well as acceptance of one’s condition and a belief in one’s own ability to recover, were all included in this study when evaluating the benefits of EBN. Pain was also evaluated as a secondary outcome. Results show that a patient’s mental health at the time of admission is a powerful indicator of how well he or she would recover functionally and psychologically.27 Screening for mood disorders, low self-acceptance, and low self-efficacy can all be easily detected using simple screening measures in the earliest stages of rehabilitation.28 With therapeutic treatments, all of the above traits can be altered. Stroke patients’ sense of self-efficacy is still being overlooked far too often. Medication-based and medically supervised physiotherapy has become increasingly popular. At each level of post-stroke rehabilitation, it is feasible to establish a number of exercises and tasks.
Rehabilitation centers, hospitals, and nursing homes that treat stroke patients must promote patients’ sense of self-efficacy in their treatment plans. As part of their policy, they must ensure that nurses have the chance to teach patients about self-efficacy as well as practice and share their own experiences with other patients. Routine self-efficacy testing upon admission to a rehabilitation facility appears to be more significant than testing for depression.29 When it comes to depression, medication is typically the quickest fix, but this robs individuals of their ability to take charge of their own mental health. Increasing self-efficacy in the rehabilitation process, in our opinion, should be given top priority because it is quite likely that improvement in the functional condition would lead to a decrease in depressive symptoms.30 Psychologically, this is preferable because the change is directly linked to the patient’s own activities and not to the use of any psychoactive substances.
The present study has several limitations: First, this study was carried out in a single center with small sample size. A multi-center with a larger sample is needed to confirm the conclusions of this study. Second, the follow-up duration of this study was only 6 months, which was relatively short. Thus, the long-term benefits of our EBN intervention on anxiety, depression, sleep quality and somatic symptoms in AIS patients were unclear. Third, only SAS and SDS scales were used to evaluate the severity of anxiety and depression in this study. Questionnaires such as Hospital Anxiety and Depression Scale (HADS) were also needed to confirm our conclusions.
Conclusions
In conclusion, we reported a positive impact of a 6‐months EBN intervention on post-stroke complications of AIS patients. We demonstrated that EBN invention has the potential to significantly improve anxiety, depression, sleep quality and somatic symptoms of patients with AIS.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hadanny A, Rittblat M, Bitterman M, et al. Hyperbaric oxygen therapy improves neurocognitive functions of post-stroke patients - a retrospective analysis. Restor Neurol Neurosci. 2020;38:93–107. doi:10.3233/rnn-190959
2. Zhang L, Zhang T, Sun Y. A newly designed intensive caregiver education program reduces cognitive impairment, anxiety, and depression in patients with acute ischemic stroke. Braz J Med Biol Res. 2019;52:e8533. doi:10.1590/1414-431x20198533
3. Herpich F, Rincon F. Management of Acute Ischemic Stroke. Crit Care Med. 2020;48:1654–1663. doi:10.1097/ccm.0000000000004597
4. Kronish IM, Edmondson D, Goldfinger JZ, Fei K, Horowitz CR. Posttraumatic stress disorder and adherence to medications in survivors of strokes and transient ischemic attacks. Stroke. 2012;43:2192–2197. doi:10.1161/STROKEAHA.112.655209
5. Naess H, Lunde L, Brogger J. The effects of fatigue, pain, and depression on quality of life in ischemic stroke patients: the Bergen Stroke Study. Vasc Health Risk Manag. 2012;8:407–413. doi:10.2147/vhrm.s32780
6. Kobylańska M, Kowalska J, Neustein J, et al. The role of biopsychosocial factors in the rehabilitation process of individuals with a stroke. Work. 2018;61:523–535. doi:10.3233/WOR-162823
7. Verberne DPJ, van Mastrigt G, Ponds R, van Heugten CM, Kroese M. Economic evaluation of nurse-led stroke aftercare addressing long-term psychosocial outcome: a comparison to care-as-usual. BMJ open. 2021;11:e039201. doi:10.1136/bmjopen-2020-039201
8. Meng J, Du J, Diao X, Zou Y. Effects of an evidence-based nursing intervention on prevention of anxiety and depression in the postpartum period. Stress Health. 2021;38:435–442. doi:10.1002/smi.3104
9. Kaldan G, Nordentoft S, Herling SF, et al. Evidence characterising skills, competencies and policies in advanced practice critical care nursing in Europe: a scoping review protocol. BMJ open. 2019;9:e031504. doi:10.1136/bmjopen-2019-031504
10. Shen Y, Zhou Y, Hou J, Hu J. Application effects of evidence-based nursing in pain nursing of advanced lung cancer. Am J Transl Res. 2021;13:9479–9484.
11. Liu J, Zhong Z, Ou S, Peng K. Application effect of evidence-based nursing in perioperative period of acute coronary syndrome. Am J Transl Res. 2021;13:2653–2661.
12. Lo SHS, Chau JPC. Exploring community-dwelling stroke survivors’ experiences of receiving a nurse-led theory-based stroke self-management programme: a qualitative study. Medicine. 2021;100:e27256. doi:10.1097/md.0000000000027256
13. Adams H, Adams R, Del Zoppo G, Goldstein LB. Guidelines for the early management of patients with ischemic stroke: 2005 guidelines update a scientific statement from the Stroke Council of the American Heart Association/American Stroke Association. Stroke. 2005;36:916–923. doi:10.1161/01.STR.0000163257.66207.2d
14. Yang Y, Zhang M, Zhao J, et al. Effect of traditional Chinese medicine emotional therapy on post-stroke depression: a protocol for systematic review and meta-analysis. Medicine. 2021;100:e25386. doi:10.1097/md.0000000000025386
15. He X, Wang X, Fu X. The effects of the quality nursing mode intervention on the psychological moods, postoperative complications, and nursing satisfaction of breast cancer surgery patients. Am J Transl Res. 2021;13:11540–11547.
16. Lei L, Huang X, Zhang S, et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med Sci Monit. 2020;26:e924609. doi:10.12659/msm.924609
17. Luo H, Xu X, Gao H, Zhang J, Zhang Z. Relationship of anxiety and depression with perfectionism in patients with aesthetic all-ceramic repair of anterior teeth. Med Sci Monit. 2021;27:e931593. doi:10.12659/msm.931593
18. Okun ML, Mancuso RA, Hobel CJ, Schetter CD, Coussons-Read M. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J Behav Med. 2018;41:703–710. doi:10.1007/s10865-018-9950-7
19. Chen Y, Fink P, Wei J, et al. Psychometric evaluation of the Whiteley index-8 in Chinese outpatients in general hospitals. Front Psychol. 2021;12:557662. doi:10.3389/fpsyg.2021.557662
20. Melnyk BM, Fineout-Overholt E, Stillwell SB, Williamson KM. Evidence-based practice: step by step: the seven steps of evidence-based practice. Am J Nurs. 2010;110:51–53. doi:10.1097/01.NAJ.0000366056.06605.d2
21. Liu Y, Qu M, Wang N, Wang L. Effects of an evidence-based nursing intervention on neurological function and serum inflammatory cytokines in patients with acute cerebral infarction: a randomized controlled trial. Restor Neurol Neurosci. 2021;39:129–137. doi:10.3233/rnn-201080
22. Lutz BJ, Young ME, Cox KJ, Martz C, Creasy KR. The crisis of stroke: experiences of patients and their family caregivers. Top Stroke Rehabil. 2011;18:786–797. doi:10.1310/tsr1806-786
23. Krishnan S, Pappadis MR, Weller SC, et al. Needs of stroke survivors as perceived by their caregivers: a scoping review. Am J Phys Med Rehabil. 2017;96:487–505. doi:10.1097/phm.0000000000000717
24. Ugur HG, Erci B, Krishnan S. The effect of home care for stroke patients and education of caregivers on the caregiver burden and quality of life. Acta clinica Croatica. 2019;58:321–332. doi:10.20471/acc.2019.58.02.16
25. Tooth L, McKenna K, Barnett A, Prescott C, Murphy S. Caregiver burden, time spent caring and health status in the first 12 months following stroke. Brain Injury. 2005;19:963–974. doi:10.1080/02699050500110785
26. Xiao M, Huang G, Feng L, et al. Impact of sleep quality on post-stroke anxiety in stroke patients. Brain Behav. 2020;10:e01716. doi:10.1002/brb3.1716
27. Kokras N, Kouzoupis AV, Paparrigopoulos T, et al. Predicting insomnia in medical wards: the effect of anxiety, depression and admission diagnosis. Gen Hosp Psychiatry. 2011;33:78–81. doi:10.1016/j.genhosppsych.2010.12.003
28. Niles AN, O’Donovan A. Comparing anxiety and depression to obesity and smoking as predictors of major medical illnesses and somatic symptoms. Health Psychol. 2019;38:172–181. doi:10.1037/hea0000707
29. Szczepańska-Gieracha J, Mazurek J. The role of self-efficacy in the recovery process of stroke survivors. Psychol Res Behav Manag. 2020;13:897–906. doi:10.2147/PRBM.S273009
30. Torrisi M, De Cola M, Buda A, et al. Self-efficacy, poststroke depression, and rehabilitation outcomes: is there a correlation? J Stroke Cerebrovasc Dis. 2018;11:3208–3211. doi:10.1016/j.jstrokecerebrovasdis
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




