Back to Journals » Psychology Research and Behavior Management » Volume 16
Alleviating the Effects of the COVID-19 Pandemic on the Physical, Psychological Health, and Wellbeing of Students: Coping Behavior as a Mediator
Authors Younas M , Dong Y, Menhas R , Li X, Wang Y, Noor U
Received 19 October 2023
Accepted for publication 14 December 2023
Published 28 December 2023 Volume 2023:16 Pages 5255—5270
DOI https://doi.org/10.2147/PRBM.S441395
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Muhammad Younas,1 Yan Dong,1 Rashid Menhas,2 Xinyi Li,1 Yu Wang,1 Uzma Noor3
1School of Educational Technology, Faculty of Education, Beijing Normal University, Beijing, People’s Republic of China; 2Research Center of Sport and Social Sciences, Soochow University, Suzhou, Jiangsu Province, People’s Republic of China; 3School of Education, Soochow University, Suzhou, Jiangsu Province, People’s Republic of China
Correspondence: Yan Dong, School of Educational Technology, Faculty of Education, Beijing Normal University, Beijing, People’s Republic of China, Email [email protected]
Background: Public health procedures under the COVID-19 pandemic lockdown policy negatively affect people’s health. Students’ physical issues have been increased due to restrictions which further impact their psychological and overall well-being.
Objective: The research looks at the influence of coping behavior in mitigating the impact of the COVID-19 epidemic on students’ physical/psychological health and general well-being.
Methods: The study’s participants were chosen from a pool of 2200 people using convenience sampling. Using an anonymous online poll, the main data were gathered. The collected data were analyzed by using Smart-PLS.
Results: From eight direct correlations, seven were found to be true, except the route pandemic -> overall wellbeing, which was not true. Furthermore, it was shown that the mediating effect of coping behavior was statistically significant in the routes of mediation.
Conclusion: Coping strategies have a significant role in how a person responds to trying circumstances. Our study’s results suggest that coping strategies had a statistically significant mediation role in reducing the effects of the COVID-19 pandemic. It is concluded that appropriate coping strategies are an effective adaptation of a protective barrier against the damaging effects of COVID-19 on health.
Keywords: coping behavior, pandemic, students, physical health, psychological health
Introduction
The pandemic was described as a worldwide public health emergency by the World Health Organization (WHO). Currently, the coronavirus is linked to over 18 million confirmed cases worldwide. Several countries used proactive and preventive measures, such as population home confinement, to restrict the spread of the pandemic. Other studies examined anxiety and depression among nurses battling COVID-19.1,2 Medical professionals who actively treat COVID-19 patients, such as doctors and nurses, have been the subject of research to look at the relationship between perceived risk and problems connected to mental health.3–5 In addition to providing useful advice for leading active lifestyles during pandemics, the study assesses whether the sense of control mediates the good benefits of physical exercise on positive or negative mental health under unforeseen unexpected situations.6,7
 |
Figure 1 Model of the study. |
 |
Figure 2 Study Demographics. |
 |
Figure 3 PLS-SEM. |
 |
Figure 4 Bootstrapping results. |
To review the psychological effect of quarantine utilizing three internet databases and analyze individuals’ mental health throughout the first 6 weeks of lockdown.8,9 It’s generally accepted that COVID-19 may have a significant impact on people’s mental and emotional health and that we should thus be ready for an onslaught of mental and behavioral problems. Recent studies have investigated COVID-19 from a psychological, social, and neurological perspective, proposing both immediate goals and longer-term efforts for mental health.10–12
Health and Well-Being in COVID-19 Epidemic
Researchers attempted to quantify the incidence of depressive/anxiety symptoms, and sleeping difficulties in the Italian population during the lockdown by integrating available research on COVID-19’s impact on psychological outcomes and risk variables.13–16 Studies looked at the impact of adolescents’ perceptions of Coronavirus occurrence and dread on mental health and well-being, as well as the potential preventive role of physical exercise.17,18 According to studies, it is impractical to organize psychological intervention teams in many places due to the lack of specialists. The impact of coping mechanisms on the HRQoL of jobless individuals has not yet been researched and these cognitive emotion control techniques relate to the HRQoL of jobless persons and how the virus has a substantial impact on citizens’ everyday lives.19,20 Examining the link between PA and mental health on a national scale, these studies found a positive correlation between the two. At COVID-19’s conclusion, participants reported positive effects on their mental health soon after outdoor activity.21,22 Anxiety is common and has been linked to physical inactivity (PA) and a lack of social connections (evident by feelings of isolation), both of which have negative impacts on health and fitness at any age.23,24 During the new coronavirus illness (COVID-19) epidemic, public health advice, and government policies imposed social separation, isolation, and house confinement.25,26
Exercise Activities and Well-Being During COVID-19
Given the current situation, there is a strong medical case for regular at-home exercise as a method of maintaining health and a well-functioning immune system.27–29 Some studies examine gender and socioeconomic discrepancies in physical activity (PA) and dietary behavior, as well as relationships with country-level indicators of PE curriculum time distribution, wealth, and income inequality.30,31 Guidelines advocate a healthy lifestyle and frequent physical activity (PA), and empirical research on the links between fundamental tenets of SDT and actions promoting physical activity and health.32–34 To maximize beneficial impacts, treatments and policy recommendations about the link between physical exercise and mental health must take context into account. This involves examining how various forms of exercise and fitness routines carried out at home assist individuals in managing psychological problems and the effects on their physical well-being.35–37 Research indicates that insufficient physical activity and social interaction are associated with severe sleep disorders and mental health conditions. Deprivation and prolonged periods of inactivity may cause depression and present a range of health risks.38,39 Construct definitions are often absent from output variables measuring people’s well-being, and research on the effectiveness of PA and exercise as treatments for most chronic conditions pays little attention to moderating and mediating factors.40,41
Coping Behavior in the COVID-19 Period
In the COVID-19 pandemic, studies on coping strategies, social and educational influences on behavior, scientific assertions, moral judgment, guidance, and stress and coping mechanisms are examined to ascertain the prevalence of severe stress disorder and factors associated with inner distress.42,43 Studies analyze how preventative measures improve health and fitness, provide new information for fighting COVID-19, and highlight existing problems.42,44 Studies have attempted to incorporate the physical and psychobiological aspects of home-based physical activity while addressing the worldwide problem of social isolation. Some research suggests that people’s mental health and quality of life may improve from exercising by analyzing the effects of the activity on self-esteem and self-perception and by raising self-esteem.45,46 The COVID-19 pandemic causes increased emotional distress in people, but it’s unclear whether this affects coping mechanisms in ways that go beyond current theories to investigate psychological discomfort associated with the virus among Southern Germans and their coping mechanisms.47,48 The research revealed discomfort, fear, and coping methods during the epidemic, and continuous mental health assistance is needed to avert pandemic mental illness.49 As the COVID-19 pandemic spreads, it is crucial to discover the coping strategies associated with poor psychosocial outcomes in postpartum women.50 The COVID-19 epidemic has added to the previously high levels of stress practiced by nursing students. There is a need for nurses to have acceptable and adaptable ways of dealing with stress in clinical practice earlier, during, and subsequently, the COVID-19 pandemic, so that the healthcare system may remain robust during and after the pandemic.51,52
Theoretical Framework
Protection motivation theory (PMT) covers people’s risk awareness and examines the desire to take defensive actions, which are highly impacted by high levels of apparent risk. The hypothesis says public insight into a disease’s harshness and susceptibility impacts risk perception. It’s been commonly utilized to explain why people engage in protective activities when they feel in danger.53,54 Social-cognitive models of health behavior highlight cognitive procedures in health-related decision-making and have helped expose psychological aspects behind the desire to conduct healthy activities like exercise.55 The protection motive hypothesis explains how fear appeals affect health attitudes and actions.56 A threat appraisal and a coping appraisal are used to explain health-related behavior change. People may initially be exposed to threat-increasing information, such as cardiovascular disease if they do not exercise. Technology acceptance is the approval, positive reception, and continuous usage of innovative equipment and systems.57 It is established the first technology acceptance model (TAM), which showed that apparent utility and ease of using impact consumer attitudes toward new technologies. Rogers’ Protection Motivation Theory (PMT) has been included in health.58–60 Health care wearables capture users’ personal health information continuously, raising data privacy concerns. An individual’s choice to embrace health care wearable technologies involves a confidentiality calculus, in which handlers may weigh the supposed benefit and privacy risk. Active video games and exergaming may employ virtual reality (VR) as a rehab aid. VR games increase motor learning, and brain plasticity, and may supplement traditional workouts. VR games may improve motor skills by integrating physical and cognitive training.61,62 Strong autonomous motivation makes people more active than guilt, shame, or peer pressure. Two components make up what we call “autonomous motivation”: (1) motivational regulation motivated by the pleasure one experiences from the behavior itself (intrinsic motivation); and 2) motivational regulation motivated by objectives outside the behavior but compatible with the individual’s values and sense of self. Interventions for autonomous motivation may vary. The goals of self-determination therapy are autonomy, competence, and relatedness.63 Digital interference may provide a sense of closeness by exhibiting good intentions. Take the user’s viewpoint with empathy, express appreciation or care, engage the person, learn about them pay close attention, and be there when needed.64
The research looks at how coping behaviors might work as a mediator to lessen the detrimental consequences of COVID-19 on one’s emotional and physical well-being. A conceptual framework (see Figure 1) and research hypotheses (see Supplementary hypotheses of the research) were created by adhering to the aforementioned literature debate.
Research Method
Study Locale
The current study was conducted in two Pakistani cities: Islamabad, the country’s capital, and Lahore, which is located in the Punjab Province. The World Medical Helsinki Policy was followed in this study and was approved by the School of Physical Education, Soochow University ethics committee. Before commencing the conclusive stage of data collection, the study participants needed to provide their informed consent. The participants were provided with an explanation regarding the objective of the study and were given reassurance that their comments would be utilized exclusively for research purposes.
Participants
During the lockdown, the existing study population involved (+21) people from Lahore, Punjab Province, and Islamabad, Pakistan’s capital region. By sending out an online survey to residents in both areas, we were able to gather this data using a convenience sample methodology. In all, 2295 individuals responded to the online survey. After data quantification, the final data analysis was based on the answers of 2200 people, 1254 from Lahore and 946 from Islamabad. Because there was insufficient data, the 95 respondents’ replies were ignored. The bulk of survey respondents, or around (57%), lived in Lahore, Punjab Province, where the initial lockdown was imposed due to the severity of the COVID-19 pandemic, while approximately (43%) lived in Islamabad, the capital territory at the time of the lockdown.
After studying relevant literature and some studies in the socio-economic and COVID-19 pandemic standpoint,65,66 the present study included living place (Islamabad, Lahore), gender (male, female), age (21–27, 28–35, 36–43, 44–51 and above 51 years old), marital status (single, married, widowed, and divorced), and education (high school, to a doctoral degree). All demographic characteristics were provided by survey participants. The COVID-19 pandemic affects people’s social and economic lives. It affects their daily lives, where they go, what they buy, and how they do business. (Please see Figure 2).
Data Collection Process
About lockdown policy, physical and psychological health (PH, PsH), physical fitness (PA), and overall well-being, the COVID-19 pandemic (CP) and lockdown policies (LP) effects were evaluated (OW). The main information was gathered from the targeted demographic in the cities of Lahore and Islamabad using an online questionnaire survey approach. The basic data for the present investigation was gathered using the survey approach. Before conducting the survey, A meeting was scheduled with the local authorities provided with an explanation regarding the objective of the study, and permission and reasonable support were granted from authorities for the data collection process. The participants were provided with an explanation regarding the objective of the study. Also, reassurance was given to participants that their comments would be utilized exclusively for research purposes. After reviewing the data from earlier research studies on SARS and influenza epidemics, the questionnaire was created.67 Before performing the final survey for data collection, pre-tests of the questionnaire were conducted with members of the intended population in Islamabad and Lahore. After the complete questionnaire was pre-tested, several items were revised and its wording was adjusted to get the highest response rate possible from the study participants. From June 16 to September 30, 2020, an online poll through WhatsApp groups was conducted in these two cities, to assess the COVID-19 pandemic and lockdown measures as well as the health-related quality of life. Closed-ended 5-point Likert scale questions about the respondents’ demographics, the COVID-19 pandemic, the COVID-19 lockdown policy, coping behaviors, physical and psychological health, participation in physical fitness, and general well-being during the COVID-19 lockdown period made up the bulk of the questionnaire. All research participants provided permission after being informed of the investigation’s goal. The anonymized data was subjected to a quality review by the researchers for correctness, relevance, and completeness. Everyone who participated in the study was informed that their data would only be used for research purposes.
Measurement of Study Variables
In this research, the COVID-19 pandemic and lockdown policy were independent factors. Lahore and Islamabad’s COVID-19 pandemic risk perceptions and beliefs were analyzed. Due to climate change, the COVID-19 pandemic caused dread and anxiety, the perception that COVID-19 is a danger to mankind, and the significance of making health and well-being on top precedence after COVID-19. A lockdown was enacted to combat the outbreak. Many initiatives were implemented to preserve public health. In this research, lockdown policy initiatives were questioned (staying at home, social distancing, wearing a face mask, washing hands with sanitizer, quarantining, and avoiding areas where the pandemic is severe).
The study’s intermediate variable is coping techniques. During the lockdown, participants reported how they regulated their emotions for psychological, physical, and olfactory health (such as seeking comfort and understanding from another person, using substances to feel better, accepting reality and learning how to deal with it safely, keeping a good outlook, working out to relieve tension and anxiety, and coming up with innovative solutions to the troublesome issue). In a pandemic, emotional stability may be challenging. Unpredictable event planning jeopardizes health. Infectious illness outbreaks never stop; therefore, people are continuously at risk.42
During the COVID-19 lockdown, the participants’ levels of physical activity, emotional stability, and physical and mental health were all studied. Each dependent variable’s set of question statements on the Likert scale focuses on either physical health (did you practice good particular hygiene for the anticipation of disease), mental health (did you experience anxiety or depression?), or social health (did you feel isolated from others?). Ability to maintain physical fitness for the sake of health; urging others, including loved ones, to do the same; experiencing a decline in fitness during the isolation; experiencing an increase in fitness during the isolation; or maintaining a level of fitness that is roughly equivalent to that experienced before the lockdown. Health-related superiority of life is based on a person’s level of physical, mental, and social health. Health-related quality of life is a public health paradigm that takes into account not only physical health but also mental health, social health, and physical fitness.68
Data Analysis and Results
Smart-PLS 3.2.9 is used to analyze research data.69 Univariate and multivariate techniques were adopted. Univariate analysis analyses survey participants’ demographic information. Multivariate analysis used SEM to investigate the research variables’ connections. SEM data analysis consists of two processes. Utilizing the measurement model, first evaluate concept validity, reliability, and convergent validity. Second, a structural model was created to test the theory.70,71
Assessment of the Measurement Model
All three types of validity (convergent, discriminant, and internal consistency) of the measurement model were tested and found to be satisfactory (see Table 1). Cronbach’s Alpha (CA) ranged from (0.823) to (0.966), and composite reliability (CR) ranged from (0.876) to (0.975) when used to assess the instruments’ internal consistency.72 By determining the average variance extracted (AVE) and the factor loadings (FA) of each item, we were able to test for convergent validity. Convergent validity was demonstrated because the AVE for every single construct was more than 0.5 and the loading for every single item was greater than 0.6. The results are illustrated in Figure 3 and detailed in Table 1.
 |
Table 1 Factor Loadings, Construct Reliability and Validity |
Discriminant Validity
Fornell Lacker and Hetro Trait-Mono Trait are two approaches to determining discriminant validity (HTMT). To start the process of establishing discriminant validity, it is necessary to verify the Fornell-Lacker criterion. For this particular technique to be effective, it is necessary for the inter-correlations between the constructs to exceed the square root of the average variance extracted (AVE) of one of the constructs. A construct’s components must show greater variance for it to be distinguished from the other constructs in the model. Table 2 shows that for all structures, the square roots of the AVEs are greater than the values of the conforming inter-correlations.
 |
Table 2 Discriminant Validity: Fornell Larcker (N=2200) |
Heterotrait-Monotrait Ratio (HTMT)
The Heterotrait-Monotrait Ratio (HTMT) technique, which assesses discriminant validity among each pair of variables, was created in terms of discriminant validity.73 The HTMT values are less than the 0.90 standards, as shown in Table 3.
 |
Table 3 Discriminant Validity (HTMT) |
Assessment of the Structural Model
The construction of structural equations that evaluate the inner route model is made possible by the structural model, which serves as a tangible basis. Significant metrics used to analyze the structural model in this work were the route coefficient (p), coefficient of determination (R2) for endogenic variables, effect size (f2), prediction significance (q2), and multicollinearity (inner VIF).74–76 The starting value and justification for each benchmark are provided in Table 4 of the structural model below.
 |
Table 4 Assessment of Structural Model |
Model Fit Summary
The fitness model analysis before SEM is shown in Table 5. Model fitness metrics include chi-square, normed fit index, squared Euclidean distance (d_ULS), geodesic distance (d_G), and standardized root mean square residual (SRMR). The structural equations from the structural model may be used to evaluate the inner route model. The structural model was evaluated using the coefficient of determination, path coefficient, effect size, prediction significance, and multicollinearity of endogenous variables. The beginning value and rationale for each statistic are provided in Table 5 of the structural model.
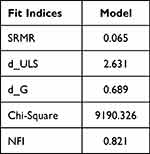 |
Table 5 Model Fit Summary |
Hypothesis Testing
Table 6 shows the results regarding our direct hypotheses, although all of the eight direct correlations were found to be true, except the route P -> O-Wb, which was not true since the p-value was greater (0.998) than 0.05. However, P -> PF, P -> Ps-H, and LDp -> Ps-H exhibited a positive impact. Significant associations such as P -> PH-H, LDp -> O-Wb, LDp -> PF, and LDp -> PH-H revealed the negative direction. Table 6 and Figure 4 include all the relations that have been established.
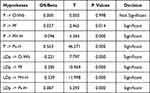 |
Table 6 Path Coefficient (Direct Effect) Result |
Furthermore, it was shown that the coping behavior had a statistically significant mediating influence along the mediated channels, P->CB->O--Wb, LDp->CB->O-Wb, P->CB->PF, LDp->CB->PF, P->CB->PH-H, and LDp->CB->PH-H since the t-values are larger than 1.96 and the p-values are less than 0.05. The confidence interval findings for those associations further supported the mediation effect by indicating that both LL and UL are negative values (ie, “0” is not in between). Except the mediation P -> CB -> O-Wb, which is complete mediation since the direct influence between P and O-Wb was found to be small, all substantial mediation effects are also determined to be partial because their direct links are also shown to be significant. However, since their p-values are larger than 0.05 and there is a 0 between LL and UL, two mediation paths—P->CB->Ps-H and LDp->CB->Ps-H—revealed no significant mediation. As a consequence, Table 7 exhibits all of the aforementioned findings.
 |
Table 7 Mediation (Indirect Effect) Result |
Discussion
During the COVID-19 pandemic isolation period, the study aimed to ascertain how COVID-19 influenced university education and the role of virtual reality fitness in boosting overall well-being.77–79 These investigations, which were conducted during the height of the global COVID-19 epidemic,80,81 seek to evaluate the overall psychological health of those in the middle and later stages of life, along with related elements and the possible moderating role of coping strategies. The COVID-19 pandemic is hurting people’s mental health and standard of living. However, few research detail appropriate ways to cope with these effects, thus 14 coping strategies were evaluated to determine whether they were linked.23 COVID-19’s impact on healthcare workers (HCW) has yet to be completely documented. As a result of the COVID-19 occurrence, we looked into how New York City’s healthcare workers dealt with their feelings of anxiety, stress, and loneliness.82 Previous research has connected COVID-19 stresses to a range of coping techniques; however, it is unclear whether these coping strategies serve as a proxy for the relationship between stressful COVID-19 events and poor mental health in college students.83,84
The goal of the research was to determine if the COVID-19 lockdown limitations had a significant effect on students studying for healthcare professions’ mental health, which is linked to lifestyle choices and coping mechanisms.85,86 The COVID-19 pandemic’s effects on future public health and preventive medicine practitioners are unclear in nations with few resources. Adults’ responses to the COVID-19 restrictions are examined in terms of their coping mechanisms, perceived threats, and sources of social support.87,88 During the ongoing COVID-19 pandemic, previous research examined stress, coping, and drug use to see whether changes in subjective well-being could be anticipated. Choices in lifestyle and methods of self-care were also investigated.89,90 Adults with continuing diseases who reported their apparent levels of domestic and international stress were asked about COVID-19-associated stress and coping strategies. The role of their coping mechanisms as mediators during the initial stages of the pandemic was also studied.91,92
To this end, it could be instructive to look at differences in objective measures of PA and the obstacles people face in trying to become more active.93,94 This brief review seeks to summarize the most recent empirical data regarding the COVID-19 pandemic’s effects and examines the part of community settings in encouraging or discouraging people’s outside physical actions and inactive behavior.95,96 To prevent the spread of COVID-19, the people of England were instructed to stay indoors and only go out for necessities like grocery shopping, medical appointments, getting to and from work or getting some exercise. It’s unclear how this will affect people’s daily routines.97,98 Regular exercise has been linked to improved mental and physical health during physical separation in people of all ages and from all over the world, according to a study on COVID-19.99 Through the control of physiological mechanisms made possible by exercise, the hypothalamic-pituitary-adrenal (HPA) axis, which controls a variety of tension hormones, and the sympathetic immune system are all affected by exercise, one can improve their mental health.100 The constructive effects of exercise on mental health have been predictable, and there are several possible mechanisms at play, whether one lives in a group or alone. The psychological, cognitive, and physiological benefits of exercise have been shown to alleviate depression, even amid a pandemic.101
Conclusion
Our study accomplishes that the COVID-19 countermeasures have negative impressions on overall well-being in the framework of physical and psychological health and physical fitness. Individual responses and coping strategies that emerge during this stressful time have become a primary goal in understanding the general population’s emotional and cognitive responses to the COVID-19 pandemic and the psychopathology it causes. The coping methods adopted by the general public during an ongoing pandemic appear to change based on the limits imposed, and these constraints differ depending on the level of risk of infection Coping behavior positively influences study participants’ emotions towards physical fitness, psychological and physical health which further contributes in the subjective wellbeing. Mental and behavioral skills (formed in response to a stressful incident) are coping strategies to reduce brief unpleasant aspects and improve personal control perception. To cope with hardship or traumatic situations, people practice a variety of coping strategies. Positive coping can elicit positive emotions and behavior’s, leading to improved responses to adversity, but negative coping techniques are not ideal for anxiety and stress management.
Study Limitations
The study includes several restrictions. The study’s use of self-report measures brings possible biases into the data collection. Participants may misremember or interpret their coping mechanisms, physical and psychological health, and general well-being erroneously. Additionally, social desirability bias could lead participants to portray themselves in a more favorable light, which might influence the validity of the findings. To mitigate these limitations, future studies could consider using objective measures and multiple data sources, such as physiological indicators and observational data, so that a more complete and precise evaluation of the factors under study may be made. Second, it’s hard to conclude cause and effect since the study was cross-sectional, between coping strategies and improvements in physical, psychological, and overall well-being. The study captures the data at a sole point in time, failing to account for the temporal dynamics and potential changes throughout the pandemic. The longitudinal studies that follow participants over a prolonged period would provide a good understanding of how coping behavior evolves and its impact on students’ well-being. Additionally, experimental designs, such as randomized controlled trials, could investigate the causal effects of specific coping strategies on physical and psychological health outcomes, thereby addressing the limitations associated with observational designs.
Abbreviations
CB, coping behavior; CP, covid-19 pandemic; L-Dp, lockdown policy; O-Wb, overall wellbeing; PF, physical fitness; Ph-H, physical health; Ps-H, psychological health; LL, lower limit; UL, upper limit.
Acknowledgments
The participants in our study’s survey are acknowledged and we appreciate all the researchers who helped with data gathering and processing. We also appreciate the reviewers who offered us their insightful criticism to support the work.
Funding
The study is funded by the General Program of the National Natural Science Foundation of China. “Research on Brain Synchronization Mechanisms and Strategies of Multi-person Interaction in STEM Educational Context”, Beijing Normal University [grant number 62177011] and Funded by the International Joint Research Project of Huiyan International College, Faculty of Education, Beijing Normal University.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Azizi A, Achak D, Saad E., et al. Health-Related Quality of Life of Moroccan COVID-19 Survivors: a Case-Control Study. Int J Environ Res Public Health. 2022;19(14):8804. doi:10.3390/ijerph19148804
2. Pang Y, Fang H, Li L, Chen M, Chen Y, Chen M. Predictive factors of anxiety and depression among nurses fighting coronavirus disease 2019 in China. Int J Mental Health Nursing. 2021;30(2):524–532. doi:10.1111/inm.12817
3. Yıldırım M, Arslan G, Özaslan A. Perceived Risk and Mental Health Problems among Healthcare Professionals during COVID-19 Pandemic: exploring the Mediating Effects of Resilience and Coronavirus Fear. Int J Ment Health Addict. 2022;20(2):1035–1045. doi:10.1007/s11469-020-00424-8
4. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1):e32. doi:10.1192/j.eurpsy.2020.35
5. Rossi R, Socci V, Talevi D, et al. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front Psychiatry;2020. 11. doi:10.3389/fpsyt.2020.00011
6. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–818. doi:10.1001/jamainternmed.2020.1562
7. Precht L-M, Margraf J, Stirnberg J, Brailovskaia J. It’s all about control: sense of control mediates the relationship between physical activity and mental health during the COVID-19 pandemic in Germany. Curr Psychol. 2023;42(10):8531–8539. doi:10.1007/s12144-021-02303-4
8. Bentlage E, Ammar A, How D, et al. Practical Recommendations for Maintaining Active Lifestyle during the COVID-19 Pandemic: a Systematic Literature Review. Int J Environ Res Public Health. 2020;17(17):6265. doi:10.3390/ijerph17176265
9. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/S0140-6736(20)30460-8
10. O’Connor RC, Wetherall K, Cleare S, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. 2021;218(6):326–333. doi:10.1192/bjp.2020.212
11. Villani L, Pastorino R, Molinari E, et al. Impact of the COVID-19 pandemic on psychological well-being of students in an Italian university: a web-based cross-sectional survey. Globalization Health. 2021;17(1):39. doi:10.1186/s12992-021-00680-w
12. Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi:10.1016/S2215-0366(20)30168-1
13. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affective Disorders. 2020;277:55–64. doi:10.1016/j.jad.2020.08.001
14. Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 Lockdown on Mental Health and Sleep Disturbances in Italy. Int J Environ Res Public Health. 2020;17(13):4779. doi:10.3390/ijerph17134779
15. Wang Y, Lugo A, Amerio A, et al. The impact of COVID-19 lockdown announcements on mental health: quasi-natural experiment in Lombardy, Italy. European Journal of Public Health. 2022;32(3):488–493. doi:10.1093/eurpub/ckac035
16. Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Globalization Health. 2020;16(1):57. doi:10.1186/s12992-020-00589-w
17. Antunes R, Frontini R, Amaro N, et al. Exploring Lifestyle Habits, Physical Activity, Anxiety and Basic Psychological Needs in a Sample of Portuguese Adults during COVID-19. Int J Environ Res Public Health. 2020;17(12):4360. doi:10.3390/ijerph17124360
18. Wright LJ, Williams SE, Veldhuijzen van Zanten JJCS. Physical Activity Protects Against the Negative Impact of Coronavirus Fear on Adolescent Mental Health and Well-Being During the COVID-19 Pandemic. Front Psychol. 2021;12.
19. Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):300–302. doi:10.1016/S2215-0366(20)30073-0
20. Extremera N, Rey L. Health-related quality of life and cognitive emotion regulation strategies in the unemployed: a cross-sectional survey. Health Qual Life Outcomes. 2014;12(1):172. doi:10.1186/s12955-014-0172-6
21. Jenkins M, Houge mackenzie S, Hodge K, Hargreaves EA, Calverley JR, Lee C. Physical Activity and Psychological Well-Being During the COVID-19 Lockdown: relationships With Motivational Quality and Nature Contexts. Front Sports Act Living. 2021;3. doi:10.3389/fspor.2021.637576
22. Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does Participating in Physical Activity in Outdoor Natural Environments Have a Greater Effect on Physical and Mental Wellbeing than Physical Activity Indoors? A Systematic Review. Environ. Sci. Technol. 2011;45(5):1761–1772. doi:10.1021/es102947t
23. Menhas R, Dai J, Ashraf MA. Physical Inactivity, Non-Communicable Diseases and National Fitness Plan of China for Physical Activity. Risk Manag Healthc Policy. 2021;14:2319–2331. doi:10.2147/RMHP.S258660
24. Hawkley LC, Capitanio JP. Perceived social isolation, evolutionary fitness and health outcomes: a lifespan approach. Philos Trans R Soc B. 2015;370(1669):20140114. doi:10.1098/rstb.2014.0114
25. Low RST, Overall NC, Chang VT, Henderson AME, Sibley CG. Emotion regulation and psychological and physical health during a nationwide COVID-19 lockdown. Emotion. 2021;21(8):1671–1690. doi:10.1037/emo0001046
26. Ammar A, Chtourou H, Boukhris O, et al. COVID-19 Home Confinement Negatively Impacts Social Participation and Life Satisfaction: a Worldwide Multicenter Study. Int J Environ Res Public Health. 2020;17(17). doi:10.3390/ijerph17176237
27. Marconcin P, Werneck AO, Peralta M, et al. The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review. BMC Public Health. 2022;22(1):209. doi:10.1186/s12889-022-12590-6
28. Bourdas DI, Zacharakis ED. Impact of COVID-19 Lockdown on Physical Activity in a Sample of Greek Adults. Sports. 2020;8(10):139. doi:10.3390/sports8100139
29. Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9(2):103–104. doi:10.1016/j.jshs.2020.02.001
30. Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6):1583. doi:10.3390/nu12061583
31. Bann D, Scholes S, Fluharty M, Shure N. Adolescents’ physical activity: cross-national comparisons of levels, distributions and disparities across 52 countries. Int J Behav Nutr Phys Act. 2019;16(1):141. doi:10.1186/s12966-019-0897-z
32. Dinas PC, Koutedakis Y, Flouris AD. Effects of exercise and physical activity on depression. Irish J Med Sci. 2011;180(2):319–325. doi:10.1007/s11845-010-0633-9
33. Hanke AA, Sundermeier T, Boeck HT, et al. Influence of Officially Ordered Restrictions during the First Wave of COVID-19 Pandemic on Physical Activity and Quality of Life in Patients after Kidney Transplantation in a Telemedicine Based Aftercare Program—A KTx360° Sub Study. Int J Environ Res Public Health. 2020;17(23):9144. doi:10.3390/ijerph17239144
34. Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9(1):78. doi:10.1186/1479-5868-9-78
35. White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C. Domain-Specific Physical Activity and Mental Health: a Meta-analysis. Am J Preventive Med. 2017;52(5):653–666. doi:10.1016/j.amepre.2016.12.008
36. Kaur H, Singh T, Arya YK, Mittal S. Physical Fitness and Exercise During the COVID-19 Pandemic: a Qualitative Enquiry. Front Psychol. 2020;11:11. doi:10.3389/fpsyg.2020.00011
37. Chtourou H, Trabelsi K, H’mida C, et al. Staying Physically Active During the Quarantine and Self-Isolation Period for Controlling and Mitigating the COVID-19 Pandemic: a Systematic Overview of the Literature. Front Psychol. 2020;11.
38. Jurak G, Morrison SA, Leskošek B, et al. Physical activity recommendations during the coronavirus disease-2019 virus outbreak. J Sport Health Sci. 2020;9(4):325–327. doi:10.1016/j.jshs.2020.05.003
39. Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Prog Cardiovasc Diseases. 2020;63(3):386–388. doi:10.1016/j.pcad.2020.03.009
40. Lehnert K, Sudeck G, Conzelmann A. Subjective well-being and exercise in the second half of life: a critical review of theoretical approaches. Eur Rev Aging Phys Activity. 2012;9(2):87–102. doi:10.1007/s11556-012-0095-3
41. Menhas R, Qin L, Saqib ZA, Younas M. The association between COVID-19 preventive strategies, virtual reality exercise, use of fitness apps, physical, and psychological health: testing a structural equation moderation model. Front Public Health. 2023;11.
42. Bavel JJV, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Human Behav. 2020;4(5):460–471. doi:10.1038/s41562-020-0884-z
43. Shahrour G, Dardas LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nursing Manage. 2020;28(7):1686–1695. doi:10.1111/jonm.13124
44. Lesser IA, Nienhuis CP. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int J Environ Res Public Health. 2020;17(11):3899. doi:10.3390/ijerph17113899
45. de Oliveira Neto L, Elsangedy HM, de Oliveira Tavares VD, Teixeira CVLS, Behm DG, Da Silva-Grigoletto ME. # TrainingInHome-Home-based training during COVID-19 (SARS-COV2) pandemic: physical exercise and behavior-based approach. Revista Brasileira de Fisiologia do Exercício. 2020;19(2):9–19. doi:10.33233/rbfe.v19i2.4006
46. Fox KR. The effects of exercise on self-perceptions and self-esteem. Phys Activity Psychol Well-Being. 2000;13:81–118.
47. Fluharty M, Fancourt D. How have people been coping during the COVID-19 pandemic? Patterns and predictors of coping strategies amongst 26,016 UK adults. BMC Psychol. 2021;9(1):107. doi:10.1186/s40359-021-00603-9
48. Elsayed M, Schönfeldt-Lecuona C, Welte XA, et al. Psychological Distress, Fear and Coping Strategies During the Second and Third Waves of the COVID-19 Pandemic in Southern Germany. Front Psychiatry. 2022;13.
49. Chair SY, Chien WT, Liu T, et al. Psychological Distress, Fear and Coping Strategies among Hong Kong People During the COVID-19 Pandemic. Curr Psychol. 2023;42(3):2538–2557. doi:10.1007/s12144-021-02338-7
50. Werchan DM, Hendrix CL, Ablow JC, et al. Behavioral coping phenotypes and associated psychosocial outcomes of pregnant and postpartum women during the COVID-19 pandemic. Sci Rep. 2022;12(1):1209. doi:10.1038/s41598-022-05299-4
51. Hamadi HY, Zakari NMA, Jibreel E, Al Nami FN, Smida JAS, Ben Haddad HH. Stress and Coping Strategies among Nursing Students in Clinical Practice during COVID-19. Nursing Reports. 2021;11(3):629–639. doi:10.3390/nursrep11030060
52. Rahman A. A scoping review of COVID-19-related stress coping resources among nurses. Int J Nurs Sci. 2022;9(2):259–267. doi:10.1016/j.ijnss.2022.02.008
53. Cacioppo JT, Petty RE, Tassinary LG. Social psychophysiology: a new look. In: Advances in Experimental Social Psychology. Vol. 22. Elsevier; 1989:39–91.
54. Milne S, Sheeran P, Orbell S. Prediction and Intervention in Health-Related Behavior: a Meta-Analytic Review of Protection Motivation Theory. J Appl Social Psychol. 2000;30(1):106–143. doi:10.1111/j.1559-1816.2000.tb02308.x
55. Maddux JE. Social cognitive models of health and exercise behavior: an introduction and review of conceptual issues. J Appl Sport Psychol. 1993;5(2):116–140. doi:10.1080/10413209308411310
56. Rogers RW, Deckner CW. Effects of fear appeals and physiological arousal upon emotion, attitudes, and cigarette smoking. Journal of Personality and Social Psychology. 1975;32(2):222–230. doi:10.1037/0022-3514.32.2.222
57. Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13(3):319–340. doi:10.2307/249008
58. Rogers RW. A Protection Motivation Theory of Fear Appeals and Attitude Change1. J Psychol. 1975;91(1):93–114. doi:10.1080/00223980.1975.9915803
59. Sun Y, Wang N, Guo X, Peng Z. Understanding the acceptance of mobile health services: a comparison and integration of alternative models. J Electron Commerce Res. 2013;14(2):183.
60. Dai J, Sang X, Menhas R, et al. The Influence of COVID-19 Pandemic on Physical Health–Psychological Health, Physical Activity, and Overall Well-Being: the Mediating Role of Emotional Regulation. Front Psychol. 2021;12:667461. doi:10.3389/fpsyg.2021.667461
61. Deutsch JE, Westcott McCoy S. Virtual Reality and Serious Games in Neurorehabilitation of Children and Adults: prevention, Plasticity, and Participation. Pediatr Phys Ther. 2017;29:S23–S36. doi:10.1097/PEP.0000000000000387
62. Molina KI, Ricci NA, de Moraes SA, Perracini MR. Virtual reality using games for improving physical functioning in older adults: a systematic review. J Neuroeng Rehabil. 2014;11(1):156. doi:10.1186/1743-0003-11-156
63. Webber KH, Tate DF, Ward DS, Bowling JM. Motivation and Its Relationship to Adherence to Self-monitoring and Weight Loss in a 16-week Internet Behavioral Weight Loss Intervention. J Nutr Educ Behav. 2010;42(3):161–167. doi:10.1016/j.jneb.2009.03.001
64. Silva MN, Marques MM, Teixeira PJ. Testing theory in practice: the example of self-determination theory-based interventions. Eur Health Psychol. 2014;16(5):171–180.
65. Sang X, Menhas R, Saqib ZA, et al. The Psychological Impacts of COVID-19 Home Confinement and Physical Activity: a Structural Equation Model Analysis. Front Psychol. 2021;11.
66. Yang J, Menhas R, Dai J, et al. Virtual Reality Fitness (VRF) for Behavior Management During the COVID-19 Pandemic: a Mediation Analysis Approach. Psychol Res Behav Manag. 2022;15:171–182. doi:10.2147/PRBM.S350666
67. Rubin GJ, Potts HWW, Michie S. The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: results from 36 national telephone surveys in the UK. Health Technol Assess. 2010;14(34):34. doi:10.3310/hta14340-03
68. Sitlinger A, Zafar SY. Health-Related Quality of Life: the Impact on Morbidity and Mortality. Surgical Oncol Clin North Am. 2018;27(4):675–684. doi:10.1016/j.soc.2018.05.008
69. Ringle CM, Wende S, Becker JM. SmartPLS 3. Boenningstedt SmartPLS GmbH. 2015;2015:56.
70. Anderson JC, Gerbing DW. Assumptions and comparative strengths of the two-step approach: comment on Fornell and Yi. Sociological Methods. 1992;20(3):321–333. doi:10.1177/0049124192020003002
71. Hair JF, Hult GTM, Ringle CM, Sarstedt M, Thiele KO. Mirror, mirror on the wall: a comparative evaluation of composite-based structural equation modeling methods. J Academy Marketing Sci. 2017;45(5):616–632. doi:10.1007/s11747-017-0517-x
72. Henseler J, Hubona G, Ray PA. Using PLS path modeling in new technology research: updated guidelines. Ind Manage Data Syst. 2016;116(1):2–20. doi:10.1108/IMDS-09-2015-0382
73. Henseler J, Ringle CM, Sinkovics RR. The use of partial least squares path modeling in international marketing. In: Sinkovics RR, Ghauri PN, editors. New Challenges to International Marketing. Vol. 20. Emerald Group Publishing Limited; 2009:277–319.
74. Chin WW. How to Write Up and Report PLS Analyses. In: Esposito Vinzi V, Chin WW, Henseler J, Wang H, editors. Handbook of Partial Least Squares: Concepts, Methods and Applications. Berlin, Heidelberg: Springer Berlin Heidelberg; 2010:655–690.
75. Tenenhaus M, Vinzi VE, Chatelin Y-M, Lauro C. PLS path modeling. Comput. Stat. Data Anal. 2005;48(1):159–205. doi:10.1016/j.csda.2004.03.005
76. Götz O, Liehr-Gobbers K, Krafft M. Evaluation of Structural Equation Models Using the Partial Least Squares (PLS) Approach. In: Esposito Vinzi V, Chin WW, Henseler J, Wang H, editors. Handbook of Partial Least Squares: Concepts, Methods and Applications. Berlin, Heidelberg: Springer Berlin Heidelberg; 2010:691–711.
77. Peng X, Menhas R, Dai J, Younas M. The COVID-19 Pandemic and Overall Wellbeing: mediating Role of Virtual Reality Fitness for Physical-Psychological Health and Physical Activity. Psychol Res Behav Manage. 2022;15:1741–1756. doi:10.2147/PRBM.S369020
78. Noor U, Younas M, Saleh Aldayel H, Menhas R, Qingyu X. Learning behavior, digital platforms for learning and its impact on university student’s motivations and knowledge development. Front Psychol. 2022;13.
79. Fang P, Shi S, Menhas R, Laar RA, Saeed MM. Demographic Characteristics and Digital Platforms for Physical Activity Among the Chinese Residents During the COVID-19 Pandemic: a Mediating Analysis. J Multidisciplinary Healthcare. 2022;515–529. doi:10.2147/JMDH.S354984
80. Malek Rivan NF, Shahar S, Singh DKA, et al. Mediation effect of coping strategies on general psychological health among middle-aged and older adults during the COVID-19 pandemic. Aging Mental Health. 2022;26(10):2039–2047. doi:10.1080/13607863.2021.1972281
81. Lorente L, Vera M, Peiró T. Nurses´ stressors and psychological distress during the COVID-19 pandemic: the mediating role of coping and resilience. J Adv Nurs. 2021;77(3):1335–1344. doi:10.1111/jan.14695
82. Shamblaw AL, Rumas RL, Best MW. Coping during the COVID-19 pandemic: relations with mental health and quality of life. Canadian Psychology/Psychologie Canadienne. 2021;62(1):92. doi:10.1037/cap0000263
83. Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General Hospital Psychiatry. 2020;66:1–8. doi:10.1016/j.genhosppsych.2020.06.007
84. Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. Coping strategies mediate the associations between COVID-19 experiences and mental health outcomes in pregnancy. Arch Women’s Mental Health. 2021;24(6):1007–1017. doi:10.1007/s00737-021-01135-2
85. Theis N, Campbell N, De Leeuw J, Owen M, Schenke KC. The effects of COVID-19 restrictions on physical activity and mental health of children and young adults with physical and/or intellectual disabilities. Disability Health J. 2021;14(3):101064. doi:10.1016/j.dhjo.2021.101064
86. Liu R, Menhas R, Dai J, Saqib ZA, Peng X. Fitness Apps, Live Streaming Workout Classes, and Virtual Reality Fitness for Physical Activity During the COVID-19 Lockdown: an Empirical Study. Front Public Health. 2022;10:852311. doi:10.3389/fpubh.2022.852311
87. Mishra J, Samanta P, Panigrahi A, Dash K, Behera MR, Das R. Mental Health Status, Coping Strategies During Covid-19 Pandemic Among Undergraduate Students of Healthcare Profession. Int J Ment Health Addict. 2023;21(1):562–574. doi:10.1007/s11469-021-00611-1
88. Antoniou AS, Greenglass E, Dimopoulos MA, Chrousos G, Papageorgiou C, Tountas Y. Coping strategies, perceived threat and sources of social support in adults during COVID-19 pandemic. Psychology. 2022;26(3):165–180.
89. Thai TT, Le PTV, Huynh QHN, Pham PTT, Bui HTH. Perceived Stress and Coping Strategies During the COVID-19 Pandemic Among Public Health and Preventive Medicine Students in Vietnam. Psychol Res Behav Manage. 2021;14:795–804. doi:10.2147/PRBM.S317059
90. Pigaiani Y, Zoccante L, Zocca A, et al. Adolescent Lifestyle Behaviors, Coping Strategies and Subjective Wellbeing during the COVID-19 Pandemic: an Online Student Survey. Healthcare. 2020;8(4). doi:10.3390/healthcare8040472
91. Bourduge C, Teissedre F, Morel F, Flaudias V, Izaute M, Brousse G. Lockdown Impact on Stress, Coping Strategies, and Substance Use in Teenagers. Front Psychiatry. 2022;12.
92. Girma A, Ayalew E, Mesafint G. Covid-19 Pandemic-Related Stress and Coping Strategies Among Adults with Chronic Disease in Southwest Ethiopia. Neuropsychiatr Dis Treat. 2021;17:1551–1561. doi:10.2147/NDT.S308394
93. Fan X, Menhas R, Laar RA. Repercussions of Pandemic and Preventive Measures on General Well-Being, Psychological Health, Physical Fitness, and Health Behavior: mediating Role of Coping Behavior. Psychol Res Behav Manag. 2023;16:2437–2454. doi:10.2147/PRBM.S405273
94. Farah BQ, Do Prado WL, Malik N, et al. Barriers to physical activity during the COVID-19 pandemic in adults: a cross-sectional study. Sport Sci Health. 2021;17(2):441–447. doi:10.1007/s11332-020-00724-5
95. Park AH, Zhong S, Yang H, Jeong J, Lee C. Impact of COVID-19 on physical activity: a rapid review. J Global Health. 2022;12:05003. doi:10.7189/jogh.12.05003
96. Sari DK, Mani S, Fadli M, et al. Is It Important to Increase Physical Activity Among University Students During the Second-Wave COVID-19 Pandemic in Asian Countries? A Cross-Sectional Study of the Knowledge, Attitudes, and Practices in Asian Countries. J Multidisciplinary Healthcare. 2022;15:1559–1571. doi:10.2147/JMDH.S368635
97. Czyż SH, Starościak W. Perceived physical activity during stay-at-home COVID-19 pandemic lockdown March-April 2020 in Polish adults. PeerJ. 2022;10:e12779.
98. Strain T, Sharp SJ, Spiers A, et al. Population level physical activity before and during the first national COVID-19 lockdown: a nationally representative repeat cross-sectional study of 5 years of Active Lives data in England. Lancet Regional Health. 2022;12.
99. Saqib ZA, Dai J, Menhas R, et al. Physical Activity is a Medicine for Non-Communicable Diseases: a Survey Study Regarding the Perception of Physical Activity Impact on Health Wellbeing. Risk Manag Healthc Policy. 2020;13:2949–2962. doi:10.2147/RMHP.S280339
100. Stranahan AM, Lee K, Mattson MP. Central Mechanisms of HPA Axis Regulation by Voluntary Exercise. NeuroMolecular Med. 2008;10(2):118–127. doi:10.1007/s12017-008-8027-0
101. Cooney GM, Dwan K, Greig CA, et al. Exercise for depression. Cochrane Database Syst Rev. 2013;2013(9). doi:10.1002/14651858.CD004366.pub6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
