Back to Journals » OncoTargets and Therapy » Volume 10
ALK and ROS1 concurrent with EGFR mutation in patients with lung adenocarcinoma
Received 26 January 2017
Accepted for publication 12 April 2017
Published 11 July 2017 Volume 2017:10 Pages 3399—3404
DOI https://doi.org/10.2147/OTT.S133349
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr XuYu Yang
Yanjiao Mao, Shixiu Wu
Department of Radiotherapy Oncology, Hangzhou Cancer Hospital, Hangzhou, People’s Republic of China
Purpose: The purpose of this study was to explore the frequencies of ALK and ROS1 fusion genes in EGFR-mutant lung adenocarcinoma patients and examine the therapeutic efficacies of EGFR-tyrosine kinase inhibitors (TKIs).
Materials and methods: A total of 421 EGFR-mutated patients taking EGFR-TKIs were examined for ALK and ROS1 fusion genes based on reverse transcription-polymerase chain reaction (RT-PCR). Progression-free survival (PFS) and overall survival (OS) were evaluated by the Kaplan–Meier method and compared by the log-rank test.
Results: The mutations of ALK rearrangement (n=10) and ROS1 rearrangement (n=3) were detected. All the patients received EGFR-TKIs, and eight took subsequent ALK/ROS1 inhibitor. PFS was longer in single EGFR mutants (n=408) than in EGFR/ALK or EGFR/ROS1 counterparts (n=13; 10.7 vs 6.6 months, P=0.004). No difference in OS existed between single EGFR and EGFR/ALK or EGFR/ROS1 mutants (21.0 vs 23.0 months, P=0.196). The median PFS of eight patients treated with ALK/ROS1 inhibitor was 6.0 months.
Conclusion: Concomitant ALK/ROS1 fusion genes occurred in 3.1% EGFR-mutated lung adenocarcinoma patients. Concomitant ALK/ROS1–EGFR mutations may influence the therapeutic efficacy of EGFR-TKIs.
Keywords: epidermal growth factor receptor, ALK, ROS1, lung adenocarcinoma, efficacy
Introduction
It is well known that the mutations of EGFR act as one of the most frequent driver genes in non-small cell lung cancer (NSCLC) patients, especially among East Asian female lung adenocarcinoma patients.1,2 Previous studies have shown that EGFR-tyrosine kinase inhibitors (EGFR-TKIs) could achieve a high response rate and yield a promising efficacy for EGFR mutants.3–6
Despite a response rate of 60%–70% in EGFR-mutated lung cancer patients treated with EGFR-TKIs, 10%–20% of individuals developed primary resistance.4–6 The mechanism is currently ill defined. Possible contributing factors included T790M mutation, MET amplification and PIK3CA mutation.7–9 Concomitant genetic alterations were found to be associated with primary resistance in EGFR-mutated NSCLC patients.10,11 However, the studies were somewhat limited, and only several case series were reported. Furthermore, the efficacies of EGFR-TKIs have remained elusive.
Here, ALK and ROS1 fusion gene panel was used for screening the patients harboring EGFR-mutated samples and further detecting the therapeutic efficacies of EGFR-TKIs.
Materials and methods
Patient samples
Consecutive EGFR-mutated patients receiving EGFR-TKIs for lung adenocarcinoma were screened at Hangzhou Cancer Hospital between 2009 and 2015. The inclusion criteria were as follows: 1) uses of EGFR-TKIs during advanced stage; 2) sufficient residual tissues for detecting ALK and ROS1 fusion genes and 3) confirmed as having sensitive EGFR mutation. Resistant mutations such as T790M, S768I and exon 20 insertions were excluded. The study protocol was approved by the ethics committee of Hangzhou Cancer Hospital, and written informed consents were obtained from all patients.
Detection of EGFR/ALK/ROS1 fusion gene
EGFR gene was detected by amplification refractory mutation system (ARMS)-based kit (Amoy, Xiamen, China). It was capable of detecting the following 23 mutations: three in exon 18 (G719A, G719C and G719S), 13 deletions in exon 19, two mutations in exon 20 (T790M and S768I), three insertions in exon 20 and two mutations in exon 21 (L858R and L861Q).
The ALK and ROS1 fusion mRNAs were detected by polymerase chain reaction (PCR) using fusion gene detection kit (Amoy). Briefly, total RNA was extracted using Qiagen (Dusseldorf, Germany) RNeasy FFPE kit. mRNA was reverse transcribed into cDNA for 1 h at 42°C. β-actin was used as an internal control. The conditions of reverse transcription-polymerase chain reaction (RT-PCR) were as follows: initial denaturation at 95°C for 5 min, followed by 95°C for 25 s, 64°C for 20 s and 72°C for 20 s for ensuring specificity and 31 cycles at 93°C for 25 s, 60°C for 35 s and 72°C for 20 s. Data collection and sensitivity analysis were detailed previously.12 The subtypes of EGFR/ALK/ROS1 genes are summarized in Table S1.
Evaluations of TKI treatment
Tumors were evaluated during the treatment with EGFR-TKIs or ALK/ROS1 inhibitor every 8 weeks. Objective tumor responses were evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST 1.1). Objective response rate (ORR) included complete response (CR), partial response (PR), stable disease (SD) and progressive disease (PD).
Statistical analyses
The Kaplan–Meier method was used for survival analysis. Progression-free survival (PFS) of TKIs was defined as the time from initiating TKI treatment to documented progression or mortality from any cause. Statistical analysis was performed using the SPSS 18 software (SPSS Inc., Chicago, IL, USA). The median follow-up period was 28.5 months (4.5–65 months). The last follow-up time was October 31, 2016.
Results
Patient characteristics
A total of 421 patients were enrolled, and their clinical characteristics are summarized in Table 1. Among the patients, 13 were confirmed as having concomitant ALK/ROS1 fusion gene. Their clinical characteristics are summarized in Table 2. There were six males and seven females with a median age of 55 years. One patient was a former smoker and 12 had never smoked. The comparisons of single EGFR versus concomitant gene mutations are listed in Table 1.
  | Table 1 Characteristics of the study population and comparison (n=421) |
Gene profiles
The genetic details of 421 EGFR mutations are as follows: exon 19 deletions (n=217), L858R mutation in exon 21 (n=169), G719X in exon 18 (n=21) and L861Q (n=14). Concomitant gene fusions were identified in 13 patients (3.1%), including ALK (n=10, 2.4%) and ROS1 (n=3, 0.7%). Their profiles are detailed in Table 2.
Efficacy of TKIs
All 421 patients received EGFR-TKIs. Among 13 patients with concomitant genes, eight switched to crizotinib after ineffective EGFR-TKIs. The agents of EGFR-TKIs included erlotinib (n=71), gefitinib (n=126) and icotinib (n=224). None of them received any second-generation EGFR-TKI since so far none have been approved in China.
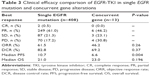
The clinical efficacies of 408 single EGFR-mutated patients included CR (n=2, 0.5%), PR (n=249, 61.0%), SD (n=87, 21.3%) and PD (n=70, 17.2%). In concomitant ALK/ROS1 mutants, the outcomes of EGFR-TKIs were PR (n=6), SD (n=3) and PD (n=4). The efficacy comparisons between single EGFR and concomitant gene mutations are shown in Table 3.
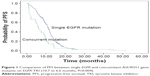
The overall value of PFS was 10.7 months (95% CI, 10.0–11.4). The median values of PFS were 10.7 and 6.6 months in mutants of single EGFR and concomitant ALK/ROS1 fusion gene, respectively (Figure 1, P=0.004). For eight patients on crizotinib, the value of PFS was 6.0 months for concomitant ALK/ROS1 fusion gene mutations (95% CI, 3.2–8.8).
The overall median value of OS was 21.0 months (95% CI, 18.9–23.4). No survival difference existed between single EGFR mutants and those with concomitant ALK/ROS1 fusion gene mutations (21.0 vs 23.0 months, P=0.196; Figure 2).
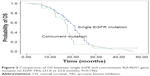  | Figure 2 Comparison of OS between single EGFR and concomitant ALK/ROS1 gene mutants on EGFR-TKIs (21.0 vs 23.0 months, P=0.196). |
Discussion
Our results showed that 3.1% of EGFR-mutated lung adenocarcinoma Chinese patients harbored ALK/ROS1 fusion genes. Concurrent ALK/ROS1 gene decreased the therapeutic efficacy of EGFR-TKIs. However, it had no impact on the overall survival (OS).
Although gene alterations were presumably mutually exclusive in lung adenocarcinoma,13 some reports revealed that genes might occur concomitantly.14,15 With the emerging of high-throughput sequencing, many concomitant genes have been detected. The frequency of concomitant EGFR/ALK or EGFR/ROS1 mutations was 3.1% in the present study, and this figure was consistent with previous reports.16–19
Owing to a low frequency of concomitant genes in EGFR-mutated lung cancer patients, the efficacy of EGFR-TKIs is largely unknown. The median PFS of first-generation EGFR-TKIs was 11.2 months in patients harboring concomitant EGFR/ALK genes in one report by Yang et al.20 For concomitant ALK/ROS1 and EGFR mutants, there was a practical dilemma of therapeutic sequence of EGFR-TKIs and ALK/ROS1 inhibitors. Relative levels of phospho-EGFR or ALK could predict the efficacy of targeted treatment in EGFR/ALK mutants in the study of Yang et al.20 In the present study, all patients took EGFR-TKIs initially and eight took subsequent ALK/ROS1 inhibitor. The median value of PFS was 6.6 months for 13 patients on EGFR-TKIs. However, among eight patients on crizotinib, six obtained disease control. Owing to efficacy difference for dosing order of targeted therapy, despite a low frequency, there is a future need of using a useful marker for selecting targeted treatment in patients with concomitant genes. Except at the level of phosphorylation, abundance of gene was identified previously as a predictor of targeted therapy;21 the abundance level of different genes in one sample should be detected for patients with concomitant genes.
A small sample size was a major drawback of the present study. Second, not all patients received crizotinib after ineffective EGFR-TKIs. As a result, the clinical efficacy of further treatment could not be fully evaluated. Third, only RT-PCR was used for ALK/ROS1 genes so that false positives might ensue. Moreover, RT-PCR could not provide convincing evidence for the dominance of expression for one oncogene aberration over another in the same samples. In addition, it was impossible to check whether individual tumor cells had these two mutations simultaneously or singly.22 However, our findings are meaningful for clinical practice.
Conclusion
A total of 3.1% of EGFR-mutated patients harbored ALK/ROS1 fusion genes. Concomitant genes of ALK/ROS1 might decrease the therapeutic efficacy of EGFR-TKIs.
Disclosure
The authors report no conflicts of interest in this work.
References
Shi Y, Au JS, Thongprasert S, et al. A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology (PIONEER). J Thorac Oncol. 2014;9(2):154–162. | ||
Zhang Y, Sun Y, Pan Y, et al. Frequency of driver mutations in lung adenocarcinoma from female never-smokers varies with histologic subtypes and age at diagnosis. Clin Cancer Res. 2012;18(7):1947–1953. | ||
Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–957. | ||
Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735–742. | ||
Mitsudomi T, Morita S, Yatabe Y, et al; West Japan Oncology Group. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11(2):121–128. | ||
Han JY, Park K, Kim SW, et al. First-SIGNAL: first-line single-agent iressa versus gemcitabine and cisplatin trial in never-smokers with adenocarcinoma of the lung. J Clin Oncol. 2012;30(10):1122–1128. | ||
Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19(8):2240–2247. | ||
Jardim DL, Tang C, Gagliato Dde M, et al. Analysis of 1,115 patients tested for MET amplification and therapy response in the MD Anderson Phase I Clinic. Clin Cancer Res. 2014;20(24):6336–6345. | ||
Li S, Li L, Zhu Y, et al. Coexistence of EGFR with KRAS, or BRAF or PIK3CA somatic mutations in lung cancer: a comprehensive mutation profiling from 5125 Chinese cohorts. Br J Cancer. 2014;110(11):2812–2820. | ||
Kim GW, Song JS, Choi CM, et al. Multiple resistant factors in lung cancer with primary resistance to EGFR-TK inhibitors confer poor survival. Lung Cancer. 2015;88(2):139–146. | ||
Lee JK, Shin JY, Kim S, et al. Primary resistance to epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) in patients with non-small-cell lung cancer harboring TKI-sensitive EGFR mutations: an exploratory study. Ann Oncol. 2013;24(8):2080–2087. | ||
Wu C, Zhao C, Yang Y, et al. High discrepancy of driver mutations in patients with NSCLC and synchronous multiple lung ground-glass nodules. J Thorac Oncol. 2015;10(5):778–783. | ||
Li H, Pan Y, Li Y, et al. Frequency of well-identified oncogenic driver mutations in lung adenocarcinoma of smokers varies with histological subtypes and graduated smoking dose. Lung Cancer. 2013;79(1):8–13. | ||
Song Z, Yu X, Zhang Y. Clinicopathologic characteristics, genetic variability and therapeutic options of RET rearrangements patients in lung adenocarcinoma. Lung Cancer. 2016;101:16–21. | ||
Song Z, Yu X, Zhang Y. Mutation and prognostic analyses of PIK3CA in patients with completely resected lung adenocarcinoma. Cancer Med. 2016;5(10):2694–2700. | ||
Song Z, Yu X, Zhang Y. Clinicopathological characteristics and survival of ALK, ROS1 and RET rearrangements in non-adenocarcinoma non-small cell lung cancer patients. Cancer Biol Ther. Epub 2016 Sep 16. | ||
Won JK, Keam B, Koh J, et al. Concomitant ALK translocation and EGFR mutation in lung cancer: a comparison of direct sequencing and sensitive assays and the impact on responsiveness to tyrosine kinase inhibitor. Ann Oncol. 2015;26(2):348–354. | ||
Zhang X, Zhang S, Yang X, et al. Fusion of EML4 and ALK is associated with development of lung adenocarcinomas lacking EGFR and KRAS mutations and is correlated with ALK expression. Mol Cancer. 2010;9:188. | ||
Chaft JE, Arcila ME, Paik PK, et al. Coexistence of PIK3CA and other oncogene mutations in lung adenocarcinoma – rationale for comprehensive mutation profiling. Mol Cancer Ther. 2012;11(2):485–491. | ||
Yang JJ, Zhang XC, Su J, et al. Lung cancers with concomitant EGFR mutations and ALK rearrangements: diverse responses to EGFR-TKI and crizotinib in relation to diverse receptors phosphorylation. Clin Cancer Res. 2014;20(5):1383–1392. | ||
Zhou Q, Zhang XC, Chen ZH, et al. Relative abundance of EGFR mutations predicts benefit from gefitinib treatment for advanced non-small-cell lung cancer. J Clin Oncol. 2011;29(24):3316–3321. | ||
Cai W, Lin D, Wu C, et al. Intratumoral heterogeneity of ALK-rearranged and ALK/EGFR coaltered lung adenocarcinoma. J Clin Oncol. 2015;33(32):3701–3709. |
Supplementary material
  | Table S1 The subtypes of EGFR/ALK/ROS1 genes |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.