Back to Journals » Advances in Medical Education and Practice » Volume 13
Agreement of Nurses’ and Physicians’ Attitudes on Collaboration During the Covid-19 Pandemic Using the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration
Authors Shields HM , Pelletier SR, Zambrotta ME
Received 15 April 2022
Accepted for publication 4 August 2022
Published 19 August 2022 Volume 2022:13 Pages 905—912
DOI https://doi.org/10.2147/AMEP.S370912
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Helen M Shields,1 Stephen R Pelletier,2 Marina E Zambrotta1
1Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, USA; 2Office of Educational Quality Improvement, Harvard Medical School, Boston, MA, USA
Correspondence: Helen M Shields, Department of Medicine, Brigham and Women’s Hospital, Boston, MA, USA, Tel +1 (617) 678-6077, Email [email protected]
Background: Collaboration between physicians and nurses has been shown to lead to better patient outcomes. However, studies have shown differing physicians’ and nurses’ responses to survey questions about physician-nurse collaboration. We surveyed physicians and nurses during the Covid-19 pandemic for their attitudes toward collaboration.
Methods: In August 2021, during the Covid-19 pandemic, we surveyed physicians and nurses throughout an urban, academic teaching hospital over a consecutive twenty-day period using the validated Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration. Anonymous surveys were obtained from nurses and physicians on duty at the hospital. Demographic data from each survey included gender, age, profession of nurse or physician, degree, and specialization.
Results: Four hundred and fifteen (415) unique paper surveys were collected from 308 nurses and 107 physicians over the twenty-day period. Five nurses and two physicians declined to complete the survey (1.6%). Using the Independent t-test of Means, total score and sub-scores were analyzed. Physicians and nurses scored the paper surveys in a similar manner. No statistically significant differences between the scores of physicians and nurses were found for any of the fifteen Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration questions, except for the youngest age group (20– 29-year-old) having a significantly more positive response to doctors being the dominant authority on all health matters (p-value=0.011). Gender and nursing degree did not make a significant difference. Surgical Specialties (167), Medical Specialties (196), Intensive Care Unit (21), and the Emergency Department (43) survey responses did not differ significantly from each other.
Conclusion: One and a half years into the Covid-19 pandemic, physicians and nurses at an urban, academic teaching hospital were in agreement with their responses on the validated Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration. Our data may reflect a catalytic and positive effect of the Covid-19 pandemic on physician and nurse attitudes toward collaboration.
Keywords: physician-nurse collaboration, Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration, interprofessional education, Covid-19 pandemic
Background
Multiple definitions of the word “collaboration” exist.1 Pike et al defined collaboration as the “process of working one with another”.2 They noted that “Collaboration involves trust and respect not only of one another, but also of the work and perspectives each contributes.” “It incorporates … a synergistic alliance that maximizes the contributions of each participant.”1,2 The patient safety movement led to the realization that physicians’ and nurses’ collaboration with each other was important because better collaboration has been associated with improved patient outcomes.3
In November 2019, before the pandemic started in the United States, we completed a pilot study of an innovation “Nurse-Doctor Co-Teaching” on a single, urban, academic teaching hospital floor.4 To measure collaboration in the nine consecutive days before and after the co-teaching innovation, we used a non-validated survey for nurses and residents.4 Our data did not show significant improvement in the attitudes of nurses and residents toward collaboration.4
The Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration (JSAPNC) is a validated 15-item survey that was developed by Dr. Mohammedreza Hojat to measure attitudes toward physician-nurse collaboration and has been used internationally to study collaboration.5–9 We received Hojat’s approval to utilize this validated scale to define collaboration attitudes throughout our hospital between physicians and nurses. In August 2021, eighteen months into the Covid-19 pandemic in the United States, we surveyed physicians and nurses on inpatient medical floors, surgical floors, Intensive Care Units (ICU) and the Emergency Department over a consecutive twenty-day period using the Jefferson Scale to determine physicians’ and nurses’ attitudes toward collaboration.5–9 We asked the question “Has the Covid-19 pandemic changed the traditional outcomes of physicians’ and nurses’ responses to the Jefferson Scale of Attitudes Toward Collaboration?” We knew that physicians and nurses had previously shown divergent opinions about collaboration using the Jefferson Scale.5–11
Methods
Time Frame
From Sunday, August 1st to Friday, August 20th, staff nurses and physicians throughout the Brigham and Women’s Hospital were asked to fill out the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration.
Physician Identification
Physicians were identified only as physicians and not as residents or attending physicians given the JSAPNC survey did not ask whether a physician was a resident or attending.
Ethical Approvals
We received written permission from Dr. Mohammedreza Hojat, to use the copyrighted Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration for this study on March 18, 2021.5–9 Mass General Brigham’s (MGB) Institutional Review Board (IRB) approved the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration Survey Distribution to physicians and nurses on July 8, 2021.
Hospital Setting
The hospital is an urban, academic, 793-bed hospital. We used the Jefferson Scale (JSAPNC) as a paper survey given to physicians (residents and attending physicians) and staff nurses to fill out anonymously while on duty on inpatient floors, Intensive Care Units and Emergency Department. Completion of the one-page survey of 15 questions indicated verbal consent. Participation was voluntary. No compensation was given. Each survey took approximately 3–5 minutes to complete.10
Inclusion Criteria
Every inpatient floor was surveyed. In addition, Emergency Department nurses and physicians were surveyed.
Exclusion Criteria
Two adjacent units on the floor where the pilot study of Nurse-Doctor Co-Teaching had taken place4 were excluded, and one Oncology Floor where the nurses were employed by the affiliated cancer center (Dana-Farber Cancer Institute), instead of the Brigham and Women's Hospital, was excluded.
Collection of Data
Paper surveys were filled out at the time of distribution and collected immediately after completion; on rare occasions, surveys were picked up later that day or the next day from the unit secretary or physician workroom. One hundred and seven physicians (107) and three hundred and eight nurses (308) completed the survey for a total of 415 unique, anonymous paper surveys.
Incomplete Surveys
Four hundred and one (401) surveys were completely filled out. Fourteen of the 415 surveys were noted to have a blank item(s) (3.4%). Thirteen subjects left one item blank, while one subject left two items blank. No survey had less than 12 of the 15 questions answered. Therefore, no survey was excluded from the analysis in accordance with Hojat’s guidelines for scoring the survey.7,8 In the case of a respondent with three or fewer unanswered items, the missing values were replaced, as recommended by Hojat’s guidelines,7,8 with the mean score calculated from items completed by the respondent.
JSAPNC
The Four Factors (Categories of Questions) are as Follows:
- Shared Education and Team Work
- Caring versus Curing
- Nurses’ Autonomy
- Physicians’ Authority
Total scores for the instrument as a whole and for the sub-scores of the four factors (categories of questions)7,8 were analyzed for the 415 voluntary, anonymous, and uncompensated survey completions.
Statistical Analyses
All paper surveys were scanned, and data were entered into an Excel Spread Sheet Data Base. Total score and four sub-score factors (categories of questions) means were analyzed using Independent t-tests and, where appropriate, analysis of variance. In cases of multiple-comparisons, Bonferroni corrections were calculated.
Results
Four hundred and fifteen (415) unique surveys were collected from 107 physicians (25.8%) and 308 nurses (74.2%) over a consecutive twenty-day period in August 2021 at an urban, academic teaching hospital. Five nurses and two physicians declined to complete the survey (1.6%). Incomplete surveys were returned by 14 subjects (3.4%) with 13 subjects leaving one item not circled and one subject leaving two items not circled. However, no survey was excluded because no survey respondent left more than three items blank.
Table 1 delineates the demographic information for the 415 study subjects, including gender, age, profession as nurse or physician, and specialty working on a surgical floor, medical floor or in the Emergency Department. Nine surveys were missing an answer to the question on specialization. Therefore, analyses of specialization are based on a denominator of 406 rather than the total 415 surveys collected. Table 2 and Table 3 demonstrate that the physicians (107) and nurses (308) do not show statistically significant differences in their overall responses on the fifteen item Jefferson Scale of Attitudes Toward Collaboration or the four factors of “Shared Education and Team Work”, “Caring versus Curing”, “Nurses’ Autonomy”, or “Physicians’ Authority” whether they were working in the ICU (Table 2) or in another hospital area such as on a medical floor, surgical floor or in the Emergency Department (Table 3).
 |
Table 1 Demographics of 415 Physicians and Nurses Surveyed Using the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration |
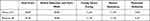 |
Table 2 Physicians and Nurses in the ICU (21) Total Score and Factor Scores on the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration |
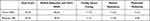 |
Table 3 Physicians and Nurses in All Other Hospital Areas (394) Total Score and Factor Scores on the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration |
Table 4 looks at comparisons between physicians’ and nurses’ total scores and the four factors of the Jefferson Scale. These data show one exception to no statistically significant differences in the scores. This exception is that the youngest age group (20–29-year old, 127 subjects) had a significantly more positive response to doctors being the dominant authority on all health matters (p-value=0.011). This indicates a stronger agreement with the Jefferson Scale survey statement that “Doctors should be the dominant authority on all health matters”. This response was not found in any of the other age groups. In contrast, those who strongly agreed or tended to agree with the survey statement “The primary function of the nurse is to carry out the physician’s orders” showed no gender, age, nurse, physician, specialty, or nurse degree difference. Table 4 also demonstrates that gender did not make a statistically significant difference in responses to the overall four factors (sub-categories). Types of nursing degree (BSN, RN, MSN or Associate’s Degree) did not make a statistically significant difference in the total score or four factor scores. Surgical Specialties, Medical Specialties, ICU and Emergency Department collaboration surveys did not statistically significantly differ in their total scores from each other nor in their responses to the four factor scores.
 |
Table 4 Comparisons Between Physicians’ and Nurses’ Gender, Age and Specialty for Total Score and Four Factor Scores for the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration |
Discussion
In contrast to previous studies using the same validated Jefferson Collaboration Scale,5–9 we demonstrate a remarkable agreement of physicians’ and nurses’ attitudes toward collaboration at an urban, academic teaching hospital eighteen months into the Covid-19 pandemic. To our knowledge, we are the first group to demonstrate uniform and consistent agreement of physicians’ and nurses’ attitudes toward collaboration using the validated Jefferson Scale of Physician-Nurse Attitudes Toward Collaboration.7–9,11–13 In 2001, Hojat et al administered the Jefferson Scale of Attitudes to 639 physicians and nurses in the United States (n = 267) and Mexico (n = 372).7 Profession (nurse or physician), gender (man or woman) and country (United States or Mexico) were used as three independent variables in a three-way factorial analysis of variance.7 Nurses overall demonstrated significantly more positive attitudes toward collaboration (p < 0.01) than did their physician colleagues.7 United States nurses had significantly more positive attitudes than any other group evaluated.7 Hojat et al noted that collaboration may be a more important factor in satisfaction on the job for a nurse than a physician.7 In 2003, Hojat et al surveyed 2522 American, Israeli, Italian and Mexican physicians and nurses using the validated Jefferson Scale.8 Regardless of the country, nurses demonstrated more positive attitudes toward collaboration than did their physician colleagues.8 The highest mean scores for the three areas of “shared education and teamwork”, “caring versus curing” and “nurses’ autonomy” were noted in the American and Israeli nurses and were significantly different from any other group.8 In 2017, Elsous used the Jefferson Scale to assess the attitudes of 414 nurse (313) and physician (101) respondents in two referral hospitals in the Gaza Strip.11 They noted that nurses’ overall scores (51.12, SD 4.55) had overall more positive attitudes than physicians’ overall scores (45.28, SD 5.30) toward collaboration on the Jefferson Scale (p < 0.001).11 How long the person had been practicing as a nurse or doctor did not influence the response.11 Elsous et al noted that “ … the relationship between physicians and nurses is complementary and nurses are partners in patient care.”11 Sterchi, in her 2007 analysis of the Jefferson Scale completed by nurses and physicians working in the day surgery unit (preoperative to postoperative), the operating room or the post-anesthesia care unit also found that the nurses’ total mean score for collaboration was significantly higher than physicians.13
However, not all prior studies have shown that nurses have more positive attitudes toward collaboration. Thomas et al showed that Critical Care physicians and nurses have “discrepant” attitudes about the teamwork they experience with each other in the Intensive Care Unit (ICU).14 Physicians in intensive care perceived higher levels of collaboration between physicians and nurses than did nurses.14 This study used a different questionnaire, the Intensive Care Unit Management Attitudes Questionnaire (ICUMAQ) to survey all ICU personnel at several Texas hospitals.14 Miller also noted on the Nurse-Physician ICU Questionnaire that physicians perceived higher levels of collaboration in an intensive care unit than did nurses, and in several cases, the differences were highly significant.15 O’Leary et al noted that physicians rated the “quality of communication and collaboration with nurses as high or very high” as compared to nurses in general medical units at an academic hospital in Chicago.16 Nurses rated the collaboration with physicians as “suboptimal.”16 In our study, however, twenty-one Intensive Care Unit nurses’ and physicians’ scores did not differ significantly from the rest of the group.
Our overall physician and nurse scores are uniform and in agreement with physicians having an overall score of 55.32, SD 4.06, and nurses having an overall score of 55.76, SD 3.33, both in the very positive range for the Jefferson Scale of Attitudes (range 15–60 with a higher score indicating higher collaboration). The one exception to the uniform agreement of our data is that the youngest age group, the 20–29-year-old age group, had a more positive response to “The physician should be the dominant authority on all health care matters”. We do not have a definitive explanation for this more positive response to this statement by the younger physicians and nurses but speculate that the younger age group may be more deferential to the authority of physicians. Unlike Weiss and Davis,17 we did not demonstrate differences in the responses of nurses with a BSN or RN degree compared to nurses with a Master’s degree or higher. Weiss and Davis noted that a nurse who identified as an administrator or educator or had a BSN or higher degree had more positive responses to collaboration than those with an Associate’s degree.17 However, we did not note any significant differences in the responses of nurses with BSN, RN, MSN or Associate’s degree.
Why do attitudes toward collaboration matter? Collaboration between nurses and physicians taking care of patients has been demonstrated to lead to better patient outcomes in ICU’s, primary care clinics and hospital inpatient floors.18–21 Baggs et al noted that nurses’ reports of collaboration were significantly (p-value = 0.02) and positively associated with patient outcomes controlling for severity of illness.18 Patient predicted risk of negative outcome decreased from 16% when the nurse reported no collaboration in decision-making to 5% when the process was fully collaborative.18 Ma et al, in 2018, reported that collaboration between nurses and doctors was associated with better patient safety outcomes of decreased hospital acquired pressure ulcers and patient falls.19 Both nurse-physician collaboration and nurse–nurse collaboration were significantly associated with patient safety outcomes.19 Capella et al showed improvement in efficiency of patient care in the trauma bay after teamwork training.20 A review of collaboration efforts in primary care clinics demonstrated improved blood pressure control, patient satisfaction and decreased number of hospitalizations.21 Other researchers have tried a variety of interventions to improve collaboration between residents in training and nurses.22–25
Why do our data contrast with results reported in prior studies using the identical validated Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration instrument? We believe the catalyst for the agreement of nurses’ and physicians’ attitudes are the stresses of the Covid-19 pandemic. During the pandemic, physicians and nurses worked long hours to provide care for many critically ill patients which required constant collaboration and communication. Before the Covid-19 pandemic, at the same teaching hospital, we collected nine days of pre-co-teaching Nurse-Doctor Co-Teaching intervention surveys and nine days of post-co-teaching Nurse-Doctor Co-Teaching intervention surveys from residents and nurses on the intervention floor units about their communication and collaboration interactions with each other.4 We analyzed these surveys for agreement of nurses’ and residents’ answers and did not find agreement or improvement after the ten-week intervention period except for one item which was the nurses’ feeling that they could more easily ask a doctor about an order in the post-intervention period compared to pre-intervention period (p-value=0.01).4
What have others reported about collaboration during the Covid-19 pandemic? Matusov et al’s data from anonymous, voluntary, and uncompensated surveys from Cedars-Sinai Medical Center in Los Angeles during the pandemic in June 2021 mirror our positive results.26 They used the Adler-Milstein survey which is made up of validated scales including Wageman’s Team Diagnostic Survey, Shortell’s communication quality scale, Schippers' coordination scale and action after planning scale and Hackman’s Job Diagnostic Survey.27 The Intensive Care Unit nurses and residents perceived collaboration similarly with no significant differences among the small group of 27 participants including 13 residents and 14 nurses in any of the “subdimensions of the questionnaire”.26 These data are similar to our results and may indicate a positive side effect of the pandemic on perceptions of nurse-physician and physician-nurse collaboration. These authors note that during the pandemic there was “more engagement of nurses on rounds”.26 In a similar vein, Hennus’s data from three academic Hospitals in Dublin, Ireland, two academic hospitals on Long Island, New York, and one academic Hospital in Utrecht, Netherlands, also indicate that during the Covid-19 pandemic in April to May of 2020, while the care may not have always been optimal, the sense of collaboration between nurse and doctors was strong and positive in the surveys they collected.28
The strengths of our study are the 415 participants with few nurses and physicians (1.6%) declining to complete the anonymous, voluntary, uncompensated survey. We had no incomplete surveys that needed to be excluded, although we had 14 out of 415 surveys (3.4%) that had one item (13 surveys) or two items (1 survey) where the Likert Scale Score was not circled. The survey was short and completed by subjects within 3–5 minutes as noted by Yildirim et al10 which made it possible to have physicians and nurses on duty readily complete it. Data was obtained from medical and surgical specialty floors in similar numbers. Intensive Care Unit data and Emergency Department data show no significant differences from the medical floors' or surgical floors’ data. Data was collected from each floor of the hospital except one floor where the nurses are employed by an affiliated cancer hospital and the two units on the floor where the innovation of Nurse-Doctor Co-Teaching had been presented. Extraordinary uniformity of statistical results with low variability was demonstrated. Gender, age (with one exception), type of nursing degree and specialization made no difference in the overall responses.
The limitations of our study are that it was conducted at one hospital that is an urban, academic teaching hospital and at one time during the year. We had three times the number of nurses compared to doctors, although Elsous et al’s study11 had a similar ratio of physicians to nurses of one physician to three nurses.11 Most physicians surveyed were residents. However, we do not know the specific number of residents compared to attendings because the Jefferson Scale survey does not ask this question. Nor do we have data on the number of years that each subject has been a physician or nurse to factor into comparisons because this question is also not asked.
Conclusions
One and a half years into the Covid-19 pandemic, physicians and nurses at an urban, academic teaching hospital demonstrated uniform and consistent agreement with their responses on the Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration. Our data may reflect a positive catalytic effect of the Covid-19 pandemic on physicians’ and nurses’ attitudes toward collaboration. Because collaboration between physicians and nurses leads to better patient outcomes,3,18–21 we view the agreement as a step in the right direction. We plan on repeating this study, with the same validated Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration, in one to two years, to see if this agreement in attitudes persists.
Acknowledgments
We are deeply grateful to Madelyn Pearson, DNP, RN, NEA-BC, Erik Alexander, MD, Emily Dehmer, MBA, Katie Fillipon, MSN, RN, and Emily Piper-Vallillo, M.Ed., who were members of the hospital-wide Nurse-Doctor Co-Teaching Initiative. Each provided encouragement for this study. We greatly appreciate Marshall Wolf, M.D.’s and Regina Mitchell, M.D.’s enthusiastic support of the Medical Education Fellowship for Internal Medicine Residents at Brigham and Women’s Hospital. Dr. Marina Zambrotta, M.D., M.Ed., was the Medical Education Fellow at Brigham and Women’s Hospital when she created and developed the pilot study of Nurse-Doctor Co-Teaching at Brigham and Women’s Hospital. We thank Paul Bain, Ph.D., MLS, Research and Instruction Librarian at the Harvard Countway Library of Medicine, Boston, MA. for his expert advice as well as his excellent and thoughtful help. We acknowledge our debt to Dr. Mohammadreza Hojat, Ph.D., Research Professor and Director, Jefferson Longitudinal Study of Medical Education, Sidney Kimmel Medical College, Philadelphia, Pennsylvania, for giving us permission to use the validated and copyrighted Jefferson Scale of Attitudes Toward Physician-Nurse Collaboration for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Morley L, Cashell A. Collaboration in health care. J Med Imaging Rad Sci. 2017;48:207–216. doi:10.1016/j.jmir.2017.02.071
2. Pike A, McHugh M, Canney K, Miller N, Reiley P, Seibert C. A new architecture for quality assurance: nurse-physician collaboration. J Nurs Care Qual. 1993;7:1–8. doi:10.1097/00001786-199304000-00007
3. Dow A, Thibault G. Interprofessional education-A foundation for a new approach to health care. N Engl J Med. 2017;377:803–805. doi:10.1056/NEJMp1705665
4. Zambrotta ME, Aylward P, Roy CL, et al. Nurse-Doctor Co-Teaching: a pilot study of the design, development, and implementation of structured interprofessional co-teaching sessions. Adv Med Educ Pract. 2021;12:339–348. doi:10.2147/AMEP.S300231
5. Hojat M, Herman MW. Developing an instrument to measure attitudes toward nurses: preliminary psychometric findings. Psychol Rep. 1985;56:571–579. doi:10.2466/pr0.1985.56.2.571
6. Hojat M, Fields SK, Veloski JJ, et al. Psychometric properties of an attitude scale measuring physician-nurse collaboration. Eval Health Prof. 1999;22(2):208–220. doi:10.1177/01632789922034275
7. Hojat M, Nasca T, Cohen M, et al. Attitudes toward Physician-Nurse Collaboration: a cross-cultural study of male and female physicians and nurses in the United States and Mexico. Nurs Res. 2001;50:123–128. doi:10.1097/00006199-200103000-00008
8. Hojat M, Gonnella JS, Nasca TJ, et al. Comparisons of American, Israeli, Italian and Mexican physicians and nurses on the total and factor scores of the Jefferson scale of attitudes toward physician-nurse collaborative relationships. Internat J Nurs Studies. 2003;40:427–435. doi:10.1016/S0020-7489(02)00108-6
9. Hojat M, Ward J, Spandorfer J, Arenson C, Van Winkle LJ, Williams B. The Jefferson scale of attitudes toward interprofessional collaboration (JeffSATIC): development and multi-institution psychometric data. J Interprof Care. 2015;29:238–244. doi:10.3109/13561820.2014.962129
10. Yildirim A, Akinci F, Ates M, et al. A Turkish version of the Jefferson scale of attitudes toward physician-nurse collaboration: a preliminary study. Contemp Nurse. 2006;23:38–45. doi:10.5172/conu.2006.23.1.38
11. Elsous A, Radwan M, Mohsen S. Nurses and physicians attitudes toward Nurse-Physician collaboration: a survey from Gaza Strip, Palestine. Nurs Res and Pract. 2017;2017:7406278.
12. Dougherty MB, Larson E. A review of instruments measuring nurse-physician collaboration. JONA. 2005;35:244–253. doi:10.1097/00005110-200505000-00008
13. Sterchi LS. Perceptions that affect physician-nurse collaboration in the perioperative setting. AORN J. 2007;86:45–57. doi:10.1016/j.aorn.2007.06.009
14. Thomas EJ, Sexton JB, Heimreich RL. Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med. 2003;31:956–959. doi:10.1097/01.CCM.0000056183.89175.76
15. Miller PA. Nurse-physician collaboration in an intensive care unit. Am J Crit Care. 2001;5:341–350. doi:10.4037/ajcc2001.10.5.341
16. O’Leary KJ, Ritter CD, Wheeler H, Szekendi MK, Brinton TS, Williams MV. Teamwork on inpatient medical units: assessing attitudes and barriers. Qual Saf Health Care. 2010;19:117–121. doi:10.1136/qshc.2008.028795
17. Weiss SJ, Davis HP. Validity and reliability of the collaborative practice scales. Nurs Res. 1985;34:299–305. doi:10.1097/00006199-198509000-00010
18. Baggs JG, Ryan SA, Phelps CE, Richeson JF, Johnson JE. The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21:18–24.
19. Ma C, Park SH, Shang J. Inter- and intra-disciplinary collaboration and patient safety outcomes in U.S. acute care hospital units: a cross-sectional study. Int J Nurs Stud. 2018;85:1–6. doi:10.1016/j.ijnurstu.2018.05.001
20. Capella J, Smith S, Philip A, et al. Teamwork training improves the clinical care of trauma patients. J Surg Educ. 2010;67:439–443. doi:10.1016/j.jsurg.2010.06.006
21. Matthys E, Remmen R, Van Bogaert P. An overview of systematic reviews on collaboration between physicians and nurses and the impact on patient outcomes: what can we learn in primary care? BMC Fam Pract. 2017;18:110–132. doi:10.1186/s12875-017-0698-x
22. O’Leary KJ, Wayne DB, Haviley C, Slade ME, Lee J, Williams MV. Improving Teamwork: impact of structured interdisciplinary rounds on a medical teaching unit. J Gen Intern Med. 2010;25:826–832. doi:10.1007/s11606-010-1345-6
23. Vazirani S, Hays RD, Shapiro MF, Cowan M. Effect of multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care. 2005;14:71–77. doi:10.4037/ajcc2005.14.1.71
24. Garth M, Millet A, Shearer E, et al. Interprofessional Collaboration: a qualitative study of non-physician perspectives on resident competency. J Gen Intern Med. 2017;33:487–492. doi:10.1007/s11606-017-4238-0
25. Zabar S, Adams J, Kurland S, et al. Charting a key competency domain: understanding resident physician interprofessional collaboration (IPC) Skills. J Gen Intern Med. 2016;31:846–853. doi:10.1007/s11606-016-3690-6
26. Matusov Y, Matthews A, Rue M, Sheffield L, Pedraza IF. Perception of interdisciplinary collaboration between ICU nurses and resident physicians during the COVID-19 pandemic. J Interprof Educ and Pract. 2022;27:1–4.
27. Adler-Milstein J, Neal K, Howell MD. Residents’ and nurses’ perceptions of team function in the medical intensive care unit. J Crit Care. 2011;26:
28. Hennus MP, Young JQ, Hennessy M, et al. Supervision, interprofessional collaboration, and patient safety in intensive care units during the COVID-19 pandemic. ATS Scholar. 2021;2:397–414. doi:10.34197/ats-scholar.2020-0165OC
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
